Pharmacology Study Guide: Drug Administration & Calculations
advertisement

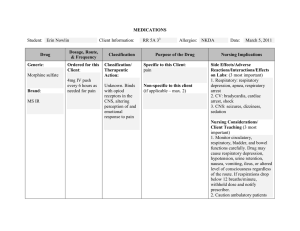
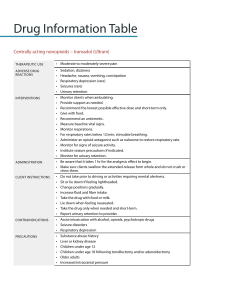
PHARMACO OGY What is Pharmacology? Pharmacology is the scientific study of the origin, nature, chemistry, effects, and uses of drugs. This knowledge is essential to providing safe and accurate medication administration to your patients. Three basic concepts of pharmacology: Pharmacokinetics the absorption, distribution, metabolism, and excretion of drugs by the body. PHARMACOKINETICS PHASES Absorbtion how does the drug enter the body? Pharmacodynamics the biochemical and physical effects of drugs and the mechanisms of drug actions. Pharmacotherapeutics the use of drugs to prevent and treat diseases. Distribution how does the drug get where it needs to go? Metabolization how does the drug is broken down? Excretion how does the drug leave the body? ABBREV AT ONS ROUTES OF ADMINISTRATION PO by mouth IM intramuscularly PR per rectum SubQ subcutaneously SL sublingual ID intradermal GT gastrostomy tube IV intravenous IVP intravenous push IVPB intravenous piggyback NG nasogastric tube TIMES OF MEDICATIONS ac pc daily bid tid qid qh ad lib stat q2h q4h q6h prn hs before meals after meals every day 2x a day 3x a day 4x a day every hour as desired immediately every 2 hours every 4 hours every 6 hours as needed at bedtime ABBREV AT ONS DRUG PREPARATION tab, tabs caps gtt EC CR susp tablet capsule drop enteric coated controlled release suspension el, elix sup, supp suppository SR sustained release elixir DOSAGE CALCULATION Basic Dosage Calculation D ________ xV desired dose H amount on hand / available dosage of the medication volume = IV Flow Rates mL of solution = mL/hr ________ total no. of hours dose IV Flow Rates mL of solution ________ x drop factor = total no. of minutes gtt/min sample: 1. Administer digoxin 0.5 mg IV daily. The drug concentration available from the pharmacy is digoxin 0.25 mg/mL. How many ML will you need to administer a 0.5 mg dose? D / H x V = Dose 0.5 / 0.25 x 1 = 2mL 2. Nurse A will infuse 1 1/2 L of NS in over 7 hours; drop factor is 15 gtt/mL. What flow rate (mL/hr) will the nurse set on the IV infusion pump? 3. A patient is receiving 250 mL normal saline IV over 4 hours, using tubing with a drip factor of 10 drops/mL. How many drops per minute should be delivered? mL of solution / total hours = mL/hr 1,500mL / 7hrs = 214.3 mL/hr mL of solution / total minutes x drop factor = gtt/min 250 mL x 10gtts per mL / 240 mins = 10.42 gtts/min Dosage Calculation Conversions 1 kg 1,000 grams 2.2 pounds 1 pound 1 gram 1 mg 1 grain 1 liter 0.45 kg 1,000 mg 1,000 mcg 60 mg 1,000 mL 16 ounces 15-16 grains 1 quart 1 teaspoon 5 mL 60 drops 1 tablespoon 3 teaspoons 15 mL 30 mL 1 ounce 1 cup 1 pint 1 quart 1 gallon 2 tablespoons 1/2 pint 2 cups 2 pints 4 quarts 8 ounces 16 ounces 4 cups 8 pints 2 pints 4 cups 240-250 mL 480 mL 1 liter 32 ounces 16 cups 128 ounces 32 ounces 1,000 mL 3, 785 mL DRUG ADMINISTRATION Buccal, sublingual, and translingual Buccal (in the pouch between the cheek and teeth), Sublingual (under the tongue), or Translingual (on the tongue) This is to prevent their destruction or transformation in the stomach or small intestine. Gastric Rectal and vaginal Suppositories, ointments, creams, or gels may be instilled into the rectum or vagina to treat local irritation or infection. Some drugs applied to the mucosa of the rectum or vagina can also be absorbed systemically. Respiratory The gastric route allows direct administration of a drug into the GI system. Drugs that are available as gases can be administered into the respiratory system through inhalation. This route is used when patients can’t ingest the drug orally. This route is accessed through a tube placed directly into the GI system, such as a “G-tube.” These drugs are rapidly absorbed. In addition, some of these drugs can be self-administered by devices such as the metered-dose inhaler. Oral Oral administration is usually the safest, most convenient, and least expensive route. Oral drugs are administered to patients who are conscious and able to swallow. Topical The topical route is used to deliver a drug via the skin or a mucous membrane. This route is used for most dermatologic, ophthalmic, otic, and nasal preparations. The respiratory route is also used in emergencies—for example, to administer some injectable drugs directly into the lungs via an endotracheal tube. Specialized infusions epidural—injected into the epidural space intrapleural—injected into the pleural cavity intraperitoneal—injected into the peritoneal cavity intraosseous—injected into the rich vascular network of a long bone intra-articular—injected into a joint intrathecal—injected into the spinal canal. Parenteral Administration Intramuscular Subcutaneous ·The IM route allows drugs to be injected directly into various muscle groups at varying tissue depths. ·small amounts of a drug are injected beneath the dermis and into the subcutaneous tissue, usually in the patient’s upper arm, thigh, or abdomen. This form of administration provides rapid systemic action and allows for absorption of relatively large doses (up to 3 mL). This allows the drug to move into the bloodstream more rapidly than if given by mouth. Aqueous suspensions and solutions in oil as well as drugs that aren’t available in oral forms are given IM. Drugs given by the subcutaneous route include nonirritating aqueous solutions and suspensions contained in up to 1 mL of fluid, such as heparin and insulin. Needle size: 18-27 gauge Uses Z-track method Intramuscular Needle size: 25-18 gauge Note: Do not inject more than 15mL of solution Subcutaneous Intravenous Intradermal Parenteral Administration Intravenous Intradermal The IV route allows injection of drugs and other substances directly into the bloodstream through a vein. Appropriate substances to administer IV include drugs, fluids, blood or blood products, and diagnostic contrast agents. Administration can range from a single dose to an ongoing infusion that’s delivered with great precision. Needle size: 16 gauge- patients who have trauma 18 gauge- surgery and blood administration 22 to 24 gauge- children. older adults and clients who have medical issues or are stable post-op Intramuscular Drugs are injected into the skin. A needle is inserted at a 10- to 15-degree angle so that it punctures only the skin’s surface. Used mainly for diagnostic purposes, such as testing for allergies or tuberculosis. Should form a "BLEB" Needle size: 26-27 gauge Subcutaneous Intravenous Intradermal Intravenous Therapy TYPES OF SOLUTIONS Hypertonic Solution Hypotonic Solution D5N5 0.45% NS Low levels of sodium or chloride; metabolic alkalosis 5% Dextrose in 0.45% Saline 5% Dextrose in LR Maintenance Fluid Replaces fluids Used for burns, bleeding, dehydration 2.5% Dextrose 0.33% NS Causes cell to shrink Ringer's Solution Treats intracellular dehydration (DKA) Never give to patients with burns or liver disease Causes cell to swell Isotonic Solution 0.9% saline (NS) Helps kidneys excrete excess fluids Sodium or chloride replacement Used with blood products Replaces fluids Used for burns, bleeding, dehydration 5% Dextrose in Water No effect w/ same concentration Replaces deficits of total body water Not used alone: dilution of electrolytes can occur Intravenous Therapy COMPLICATIONS Air Embolism air enters the vein through the IV tubing Infiltration IV fluid leaks into the surrounding tissues Infection entry of microorganism into the body via IV Symptoms Treatment Tachycardia Chest pain Hypotension Decreased LOC Cyanosis Clamp the tubing Turn the patient on their left side & place in Trendelenburg position Notify the HCP Pain Swelling Coolness Numbness in the site No blood return Remove the IV Elevate the extremity Apply warm or cool compress Do not rub the area Tachycardia Redness Swelling Chills & fever Malaise Nausea & Vomiting Remove the IV Obtain cultures Possible administration antibiotics Intravenous Therapy COMPLICATIONS Circulatory Overload administration of fluids too rapidly (FLUID VOLUME OVERLOAD) Phlebitis inflammation of the veins that can lead to thrombophlebitis Hematoma collection of blood in the tissues Symptoms Treatment Increase blood pressure Distended neck veins Dyspnea Wet cough and crackles Decrease flow rate (keep vein-open rate) Elevate head of the bed Keep the patient warm Notify the physician Heat Redness Tenderness at the site Decrease flow of IV Remove the IV Notify the physician Restart the IV on the opposite side Ecchymosis Blood Hard painful lump at the site Elevate the extremity Apply pressure and ice 6 RIGHTS OF MEDICATION ADMINISTRATION RIGHT PATIENT RIGHT TIME RIGHT DOSE RIGHT MEDICATION RIGHT ROUTE RIGHT DOCUMENTATION DRUGS ANTIBIOTICS/ANTIBACTERIALS BROAD SPECTRUM ANTIBIOTICS –oxacin PENICILLINS TETRACYCLINES -cycline AMINOGLYCOSIDES SULFONAMIDES sulf- CEPHALOSPORINS –cef ceph- & MACROLIDES -cillin -mycin FLUOROQUINOLONES –floxacin ANTIVIRALS Antiviral (disrupts viral mutation) –virimat Antiviral (undefined group) vir- -vir- -vir Antiviral (neuraminidase inhibitors) –cyclovir HIV Protease Inhibitors -navir HIV/AIDS –vudine ANTIFUNGAL Antifungal –azole ANTIHYPERTENSIVES ACE Inhibitors -pril Beta Blockers -olol Angiotensin II receptor antagonists Calcium channel blockers –sartan –pine -amill Vasopressin receptor antagonist Alpha-1 blockers -osin Loop diuretics –ide -semide -vaptan Thiazide diuretics -thiazide Potassium sparing diuretics –actone ANTIHYPERLIPIDEMICS HMG-CoA reductase inhibitors –statin OTHERS Anticoagulants (Factor Xa inhibitors) –xaban Anticoagulants (Dicumarol type) –arol Anticoagulants (Hirudin type) –irudin Low-molecular-weight heparin (LMWH) –parin Thrombolytics (clot-buster) –teplase –ase Antiarrhythmics –arone UPPER RESPIRATORY Second-gen antihistamines (H1-antagonist) Nasal decongestants –adine; -trizine; -ticine –ephrine –zoline LOWER RESPIRATORY Beta2-agonists (Bronchodilator) –terol Xanthine derivatives –phylline Cholinergic blockers –tropium; -clindidiun Immunomodulators & leukotriene modifiers –zumab; –lukast histamines (H1-antagonist) ANESTHETICS Local Anesthetics –caine ANTIANXIETY Barbiturates (CNS depressant) Barbiturates (used for anxiety/sedation) –barbital –zolam; -zepam ANTIDEPRESSANTS Serotonin Reuptake Inhibitors (SSRIs) –oxetine; -talopram; -zodone Serotonin- Norepinephrine Reuptake –faxine; -zodone; -nacipram Inhibitors (SNRI/DNRI) Tricyclic antidepressants (TCAs ) –triptyline; -pramine ANALGESICS/OPIODS Opiods –done; -one NSAIDs –olac; -profen Salicylates Aspirin (ASA) Nonsalicylates Acetaminophen GASTROINTESTINAL Histamine H2 Antagonist (H2-Blockers) –tidine; dine Proton Pump Inhibitors (PPIs) -prazole Laxative -lax ANTIDIABETIC Oral hypoglycemic –ide –tide –linide Inhibitor of the DPP-4 enzyme –gliptin Thiazolidinedione –glitazone OTHERS Corticosteroids –asone; -olone; -inide Triptans (anti-migraine) –triptan Ergotamines (anti-migraine) –ergot- Antiseptics –chloro Antituberculars (TB) rifa- Bisphosphonates –dronate OTHERS Neuromuscular blockers –nuim Retinoids (anti-acne) tretin- Phosphodiesterase 5 inhibitors –afil Carbonic anhydrase inhibitors –lamide Progestin (female hormone) –trel Atypical antipsychotics -ridone Common Meds & their drug classification ANTIBIOTICS ANTIFUNGAL AGENTS Penicillin Ampicillin Oxacillin Cefuroxime Sodium Cefotaxime Sodium Co-amoxiclav Piperacillin + Tazobactam Ciprofloxacin Clindamycin Erythromycin ANTIVIRAL DRUGS Acyclovir Zidovudine Oseltamivir Ribavirin Ganciclovir Indinavir Amantadine Zanamivir Trifluridine Penciclovir Fluconazole Ketoconazole Itraconazole Amphotericin-B Flucytosine Cystatin Griseofulvin ANTIHELMINTIC Albendazole Ivermectin Mebendazole Praziquantel Pyrantel ANTIPROTOZOAL AGENTS Metronidazole Pentamidine Tinidazole Nitazoxanide Atovaquone ANTINEOPLASTIC Cisplatin Cyclophosphamide Carboplatin Dacarbazine Chlorambucil Opiods/narcotics Warfarin Heparin Digoxin Anticholinergics Benzodiazepines Cholinergic crisis Acetaminophen (Tylenol) Magnesium sulfate Iron Lead Alcohol withdrawal Beta blockers Calcium channel blockers Aspirin Insulin Pyridoxine Tricyclic antidepressants Cyanide ANTIDOTES Naloxone (Narcan) Vitamin K Protamine sulfate Digibind Physostigmine Flumazenil (Romazicon) Atropine (Atropen) Acetylcysteine Calcium gluconate Deferoxamine Chelation agents; Dimercaprol &disodium chlordiazepoxide Glucagon Glucagon, insulin, calcium Sodium bicarbonate Glucose Deferoxamine Sodium bicarbonate Hydroxocobalamin Emergency drugs "LEAN" L -Lidocaine E -Epinephrine Used for Ventricular arrhythmias, topical/local anesthetic Used for Bronchodilation; anaphylaxis; hypersensitivity reaction; Acute asthma attack; Chronic simple glaucoma A -Atropine Sulfate N -Narcan Used to decrease respiratory secretions; treats sinus bradycardia; reverses effects of anticholinesterase medication Used for Opioid-induced toxicity; opioid-induced respiratory depression; used in neonates to counteract or treat effects from narcotics given to mother during labor Non-Opiate Analgesics Tylenol acetaminophen also an antipyretic should not exceed 4g within 24 hours no anti-inflammatory properties or GI irritation Hepatotoxicity Nausea/vomiting and gastric irritation Monitor liver function, assess for jaundice and increase LFT Educate the patient to avoid alcohol while taking acetaminophen Aspirin Acetylsalicylic acid antipyretic, anti-inflammatory, anti-platelet side effects GI irritation is expected NOTE: if GI bleeding develops, report immediately Decreased platelets count and has higher risk of bleeding nursing considerations Watch for signs of salicylism (aspirin overdose) which includes: -Tinnitus Impaired hearing and vision -Fever _Dizziness -Confusion -Nausea and vomiting -Sweating Non-Opiate Analgesics NSAIDs COX-1 inhibitors COX-2 inhibitors ibuprofen vioxx celebrex NSAIDs should be avoided in those patients with IBS or ulcer disease because of possible GI bleeding Dizziness, drowsiness and possible risk of stroke is associated with the use of NSAIDs Educate patient to report for any rashes, itching and vision changes as this could be Stevens-Johnsons Syndrome. Take note that NSAIDs can also impair kidney function. Opiate Analgesics Morphine Fentanyl (Duragesic) Methadone (Dolophine) Codeine Sulfate Oxycodone (Oxycontin) Hydromorphone (Dilaudid) Ultram (Tramadol) Meperidine (Demerol) Use for relieving pain w/o producing loss of consciousness or reflex activity. Respiratory Depression Opiates act on opioid receptor by altering perception of, and reducing severe pain. Constipation nursing considerations Frequently assess pain level and document its effectiveness. Take VS before administering the medication. Hold if RR drops to below 12 breaths per min. Administer IV opioids SLOWLY. Educate patient on long-term use of high dosage of opioids to wean off slowly. side effects Monitor VS and have naloxone available. Avoid administering w/other CNS depressants. Ensure that patient is well-hydrated. Encourage mobility Administer stool softeners or stimulant laxatives to avoid constipation Urinary Retention Encourage patient to void at least 4 hours. Monitor I&O, and obtain an order to bladder scan if needed. CNS depression & sedation Advise patient to avoid hazardous activities like driving. Morphine Side Effects "MORPHINE" M -Myosis O -Out of it (sedation) R -Respiratory depression P -Pneumonia (aspiration) H -Hypotension I -Infrequency (constipation, urinary retention) N -Nausea E -Emesis I can do all things through Christ who strengthens me. PHILIPPIANS 4:13 Good luck future RN! References Chelsea (2020). Complete Nursing School Bundle. CeceStudyGuides. Koharchik, L.S. & Hardy, E.C. (2013). As easy 1,2,3! Dosage calculations. Nursing Made Incredibly Easy!, 11(1), 25-29. https://www.doi.org/10/.1097/01.NME.0000424170.34092.7a Tuttle, K. (2020). The Complete Nursing School Bundle. NurseInTheMaking LLC. Vera, M. (2019). Pharmacology Nursing Mnemonics & Tips. Nurses Labs. Retrieved from https://nurseslabs.com/pharmacology-nursing-mnemonics-tips/ Wilson, K.M. (2013). The nurse's quick guide to I.V. drug calculations. Nursing Made Incredibly Easy! 11(2), 1-2. https://www.doi.org/10.1097/01.NME.0000426306.10980.65 By purchasing, you agree with the following terms and conditions: 1. You agree that this study guide are simply guides and should not be used over and above your course material and teacher instruction in nursing school. 2. These study guides are not intended to be used as medical advice or clinical practice, they are for educational use only. 3. You also agree NOT to distribute or share the materials under any circumstances.