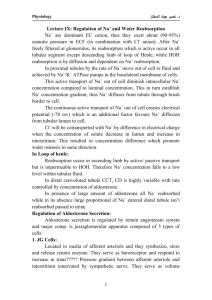
Renal Physiology II: JA; DCT; Aldosterone DCOM MS LSCI-510 Principles of Physiology L25 Renal Physiology II Distal Convoluted Tubule April 15, 2020 Dr. Stan Kunigelis Stan.Kunigelis@LMUnet.edu Office: DCOM 217 (6818) IAC Lab: Hamilton 120 (6385) Learning Objectives … 1) Describe the anatomical components of the Juxtaglomerular Apparatus and their functions. 2) Distinguish the secretions of the macula densa, mesangial cells, and juxtaglomerular cells. 3) Describe the role of juxtaglomerular cells in the activation of renin-angiotensin-aldosterone system. 4) List the actions of aldosterone on the distal convoluted tubule to regulate blood pressure. 5) Describe the mechanism of unfiltered waste secretion into the distal convoluted tubule. 2 Distal Convoluted Tubule: Renin-Angiotensin-Aldosterone System Juxtaglomerular Apparatus The Juxtaglomerular Apparatus (JA) comprises the macula densa (tubular origin) 4 and granular cells (vascular origin). JA regulates both glomerular filtration rate (local autoregulation) and secretes the enzyme renin in response to systemic hypotension. 5 Macula Densa • The macula densa is a sensor formed by the wall cells of the earliest section of the distal convoluted tubule that 1o abuts the afferent and 2o the efferent arterioles feeding the glomerulus. • Technically, it is the earliest portion of the distal convoluted tubule 6 Macula Densa • Tubular Origin • the macula densa functions as a sensor, monitoring tubular fluid flow rate through a single nephron • should the glomerular filtration rate (GFR) deviate from that expected* for a given arterial pressure, then the macula densa releases vasoactive compounds to maintain a constant GFR 7 * Recall deviations from homeostatic set points! Macula Densa: GFR • Tubular Origin • for example, if the GFR becomes too high the body risks the loss of water and ions which can cause hypotension, a drop in systemic blood pressure • therefore, the macula densa responds by releasing vasoconstrictors which decrease the GFR through that one nephron (note that this is a local autoregulatory response) 8 Macula Densa: GFR • Tubular Origin • If the macula densa detects that the GFR is too low through that one nephron, the body is at risk of accumulating wastes, experiencing water and electrolyte imbalance which could lead to systemic hypertension • therefore, the macula densa releases a vasodilator to increase GFR through that one nephron (once again, this is local autoregulation) 9 Macula Densa • these autoregulatory mechanisms allow GFR to remain constant between a MAP of 80-180 mmHg • outside of this normal range of MAP, GFR changes dramatically with blood pressure • keep in mind that this autoregulation can be easily overridden by the sympathetic nervous system and vasoactive compounds like angiotensin 10 Granular = Juxtaglomerular Cells • Vascular Origin • the macula densa (remember that this is part of the distal tubule) contacts the afferent /efferent arterioles just as they enter/leave the glomerulus • here, the wall of the afferent and efferent arterioles contains secretory granular cells (=juxtaglomerular (modified smooth muscle = myoepithelioid) cells) • There are more granular cells surrounding the afferent (input) than efferent (output) arteriole 11 Granular = Juxtaglomerular Cells • Vascular Origin • granular cells – i) are pressure sensitive, functioning as an intrarenal baroreceptor – ii) secrete the enzyme renin • activation of the renin-angiotensin-aldosterone system in response to systemic hypotension leads to vasoconstriction (angiotensin II) and the reabsorption of Na+, loss of K+ and H+ (aldosterone), which leads to a net uptake of renal water to expand the extracellular fluid volume which increases systemic blood pressure (remember that NaCl provides 90% of the osmotic force to attract and hold water) 12 Granular = Juxtaglomerular Cells As such, JA is involved in autoregulation of 1. Flow Rate: GFR through a single nephron (macula densa), and 2. BP: releases renin in response to hypotension (granular cells), to produce angiotensin II, the most potent vasoconstrictor in the body 13 Don’t confuse renin with rennin! 1) ACE-Is also block bradykinin degredation prolonging vasodilation to further decrease BP. 2) Dry cough side effect of ACE-Is. 3) ACE RBs has no influence on bradykinin. 14 • The renin-angiotensin-aldosterone system plays an important role in regulating blood volume, arterial pressure, 15 and cardiac and vascular function. 16 17 Note that ACE inhibitors or ARBs can be used in the control of hypertension. The corona virus responsible for the 2020 pandemic is believed to gain entrance via lung ACE receptors! ALDOSTERONE -aldosterone is a mineralcorticoid produced by the adrenal glands -aldosterone release can come about by one of two distinct mechanisms 1. the adrenal gland has receptors which monitor the [K+] ECF – if K levels become too high, aldosterone is released into the general circulation 2. adrenal gland release of aldosterone is stimulated by angiotensin II via JA renin -in response to hypotension, the granular/ juxtaglomerular cells of the afferent and efferent arterioles (supplying the glomerulus) release renin -renin leads to the activation of angiotensin II which stimulates the release of aldosterone from the adrenal 18 cortex • aldosterone acts upon the distal convoluted tubule of the kidney nephron to: a) activates the Na+/K+-ATPase b) increases K permeability (activation of existing channels) c) increases Na permeability (stimulates the synthesis of new Na channels) • as we saw in 1) the action of aldosterone is to cause a net reabsorption of Na and a net secretion of K and H • this results in restored blood pressure and the loss of excess K • Note: The renal corpuscle (glomerulus and Bowman's capsule) is freely permeable to both Na+ and K+. However, the body's strategies for recovering these ions is quite different. – The body reabsorbs only the Na that is needed, the rest is lost with urine. – In contrast, the body reabsorbs all filtered K, then actively secretes any excess. 19 Let’s Look At This in Greater Detail • aldosterone acts on the distal convoluted tubule to carry out the following: a) activate a Na+/K+-ATPase (serosal (blood) surface) which secretes K+ to the tubular fluid (urine) and reabsorbs Na+ – – – – this provides net Na reabsorption and K secretion since the ATPase is electrogenic, 3Na+ are reabsorbed for every 2K+ secreted in order to maintain charge neutrality H+ is also secreted (3Na/2K, 1H) as such, aldosterone leads to the loss of H+ which acidifies the urine 20 Let’s Look At This in Greater Detail • aldosterone acts on the distal convoluted tubule to carry out the following: b) increased K permeability (lumenal surface) of the distal convoluted tubule wall (aldosterone activated, ATP dependent K channels) which makes it easier to lose excess K 21 Let’s Look At This in Greater Detail • aldosterone acts on the distal convoluted tubule to carry out the following: c) stimulates the de novo synthesis of Na channel proteins (i.e., subunits) which are inserted into the lumenal surface of the distal convoluted tubule to facilitate the uptake of Na 22 Remember that the body filters all Na and reabsorbs only what is needed. • remember that only 8% of the filtered Na is actively reabsorbed in the distal convoluted tubule – 67% in proximal convoluted tubule – 25% in loop of Henle • however, this 8% of total Na has the greatest influence on systemic MAP 23 Aldosterone 1. activates Na/K-ATPase, 2. ρK (existing channels), 3. ρNa (new channel formation). Na+ Serosal Surface K+ K+ Na+ Tubular Surface DCT Wall Tubular Fluid DCT Wall Cell 3Na reabsorbed for every 2K and 1H secreted 24 Juxtaglomerular Apparatus Macula Densa Granular Cells • Tubular origin • Earliest region of DCT monitors tubular fluid flow rate through a single nephron • Releases vasodilators if GFR • Releases vasoconstrictors if GFR • Vasoactive compounds diffuse to afferent arterial to alter GFR to that one nephron local • Vascular origin • Pressure sensitive intrarenal baroreceptors • Secretory cells present in the wall of the afferent and efferent arterioles release renin in response to hypotension • Activates the reninangiotensin-aldosterone system global response autoregulatory response 25 Diuretics Diuretics are drugs that increase urine production, relieving excess fluid buildup in body tissues. Diuretics are used to treat high blood pressure, lung disease, premenstrual syndrome, and other conditions. 1. Loop diuretics exert their action on the sodium reabsorption mechanism of the thick ascending limb of the loop of Henle, resulting in excretion of urine isotonic with plasma. 2. Thiazides a group of synthetic compounds that decrease reabsorption of sodium by the kidney and thereby increase loss of water and sodium; they enhance excretion of sodium and chloride equally 3. Osmotic diuretics are a group of low molecular weight substances that can remain in high concentrations in renal tubules contributing to osmolality of glomerular filtrate. 4. Potassium-sparing diuretics those block the exchange of sodium for potassium and hydrogen ions in the distal tubule, increasing sodium 26 and chloride excretion without increasing potassium excretion. FYI Examples Mechanism - Ethanol, Water inhibits vasopressin secretion ACIDIFYING SALTS CaCl2, NH4Cl ARGININE VASOPRESSIN amphotericin B, lithium citrate inhibit vasopressin's action AQUARETICS Goldenrod, Juniper Increases blood flow in kidneys NA-H EXCHANGER ANTAGONISTS dopamine promote Na+ excretion proximal tubule CARBONIC ANHYDRASE INHIBITORS Acetazolamide, dorzolamide inhibit H+ secretion, resultant promotion of Na+ and K+ excretion proximal tubule LOOP DIURETICS Bumetanide, ethacrynic acid, furosemide,, torsemide inhibit the Na-K-2Cl symporter medullary thick ascending limb OSMOTIC DIURETICS glucose (especially in uncontrolled diabetes), mannitol promote osmotic diuresis proximal tubule, descending limb POTASSIUM-SPARING DIURETICS amiloride, spironolactone, triamterene, potassium canrenoate. inhibition of Na+/K+ exchanger: Spironolactone inhibits aldosterone action, Amiloride inhibits epithelial sodium channels cortical collecting ducts THIAZIDES bendroflumethiazide, hydrochlorothiazide inhibit reabsorption by Na+/Clsymporter distal convoluted tubules XANTHINES Caffeine, theophylline, theobromine inhibit reabsorption of Na+, increase glomerular filtration rate tubules RECEPTOR 2 ANTAGONISTS Location collecting duct 27 Kidney Disease • Hereditary Disorders – polycystic kidney disease*, – Alport's syndrome, • • • • • glomerulonephritis, endstage kidney disease, hearing loss, may affect the eyes. blood in the urine (hematuria). – hereditary nephritis, – primary hyperoxaluria and – cystinuria. • Congenital Disease – malformation of the genitourinary tract, leading to obstruction, infection, and/or destruction of kidney tissue. • Acquired Kidney Disease – Kidney Stones – Nephrotic Syndrome • large protein loss in the urine [frequently in association with low blood protein (albumin) levels, an elevated blood cholesterol and severe retention of body fluid, causing swelling (edema)]. – Long-standing High Blood Pressure (hypertension) – Diabetes – Drugs and Toxins • Certain medications, toxins, pesticides and "street" drugs (i.e., heroin) can also produce kidney damage. 28 *PCKD is associated with increased risk of intracranial aneurysms. 53-70yo life expectancy. 1/1K incidence. 29