vanAnders2013-PsychSex-Nomenclature&knowledge-culture-WeDon'tCallSemen'PenileMucous'
advertisement

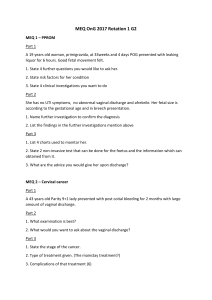
This article was downloaded by: [141.211.129.84] On: 23 October 2014, At: 11:23 Publisher: Routledge Informa Ltd Registered in England and Wales Registered Number: 1072954 Registered office: Mortimer House, 37-41 Mortimer Street, London W1T 3JH, UK Psychology & Sexuality Publication details, including instructions for authors and subscription information: http://www.tandfonline.com/loi/rpse20 Nomenclature and knowledge-culture, or, we don’t call semen ‘penile mucous’ a Sari M. van Anders a Departments of Psychology & Women’s Studies, Faculty Member of Neuroscience, Reproductive Sciences, and Science, Technology, & Society, University of Michigan, Ann Arbor, MI, USA Published online: 16 Sep 2013. To cite this article: Sari M. van Anders (2014) Nomenclature and knowledge-culture, or, we don’t call semen ‘penile mucous’, Psychology & Sexuality, 5:4, 349-356, DOI: 10.1080/19419899.2013.835743 To link to this article: http://dx.doi.org/10.1080/19419899.2013.835743 PLEASE SCROLL DOWN FOR ARTICLE Taylor & Francis makes every effort to ensure the accuracy of all the information (the “Content”) contained in the publications on our platform. However, Taylor & Francis, our agents, and our licensors make no representations or warranties whatsoever as to the accuracy, completeness, or suitability for any purpose of the Content. Any opinions and views expressed in this publication are the opinions and views of the authors, and are not the views of or endorsed by Taylor & Francis. The accuracy of the Content should not be relied upon and should be independently verified with primary sources of information. Taylor and Francis shall not be liable for any losses, actions, claims, proceedings, demands, costs, expenses, damages, and other liabilities whatsoever or howsoever caused arising directly or indirectly in connection with, in relation to or arising out of the use of the Content. This article may be used for research, teaching, and private study purposes. Any substantial or systematic reproduction, redistribution, reselling, loan, sub-licensing, systematic supply, or distribution in any form to anyone is expressly forbidden. Terms & Conditions of access and use can be found at http://www.tandfonline.com/page/termsand-conditions Psychology & Sexuality, 2014 Vol. 5, No. 4, 349–356, http://dx.doi.org/10.1080/19419899.2013.835743 ESSAY Nomenclature and knowledge-culture, or, we don’t call semen ‘penile mucous’ Sari M. van Anders* Departments of Psychology & Women’s Studies, Faculty Member of Neuroscience, Reproductive Sciences, and Science, Technology, & Society, University of Michigan, Ann Arbor, MI, USA Downloaded by [141.211.129.84] at 11:23 23 October 2014 (Received 6 November 2012; accepted 13 August 2013) Science reflects cultural practices and also occurs within them, and this ‘knowledge-culture’ is constituted by the public imaginary (general understandings and perceptions of phenomena) and the ‘scientific imaginary’ (the ability to envision scientific questions, methods, meanings and material possibilities for studying phenomena). In this feminist science laboratory case study, I argue that nomenclature contributes to epistemologies of ignorance, delimiting knowledge-culture and the scientific imaginary about vaginal fluid, which has implications for understandings of women’s bodies as well as sexual health potentials. Abject terms for vaginal fluid (vaginal mucous; vaginal discharge) preclude its existence in the scientific imaginary except as passive signs of dis-ease. I argue for a gendered abjectness of vaginal fluid’s names by situating it next to fluids that are tied to other mucosal surfaces, thus showing that even when gender is not involved in the name, gendered knowledge-culture can still affect science. I discuss how my ongoing lab research in social neuroendocrinology attends to the immune properties of vaginal fluid and positions women’s bodies as agentic, taking seriously the promise that ‘vaginal fluid’ might afford. Keywords: vaginal fluid; mucus; discharge; gender; sex; nomenclature Introduction: feminist insights and the scientific imaginary Feminist scholarship has cogently situated ‘Science’ (i.e. an epistemology) and ‘science’ (i.e. a day-to-day endeavour) as occurring within and reflecting gendered cultural processes and social interactions (e.g. Dreger, 1998; Fausto-Sterling, 2000; Haraway, 1988; Harding, 1986, 1991; Mayberry, Subramaniam, & Weasel, 2001). Accordingly, feminist scholars have carefully demonstrated that science is not very natural – in other words, that science is not a culturally neutral process, method or epistemology. Both the material of scientific phenomena and the epistemic or procedural aspects of science have also been situated within the purview of the social and cultural (e.g. JordanYoung, 2010; Oudshoorn, 1994; Traweek, 1992), or what I call here knowledge-culture. By ‘knowledge-culture’, I mean knowledge-making ventures, processes and norms that include the public imaginary and what I call here the scientific imaginary. By ‘public imaginary’, I mean culturally held ideas, perceptions, understandings and potentials of a phenomenon. The ‘scientific imaginary’ overlaps in part with the public imaginary; it *Email: smva@umich.edu © 2013 Taylor & Francis Downloaded by [141.211.129.84] at 11:23 23 October 2014 350 S.M. van Anders refers specifically to the ability to envision scientific questions, methods, meanings and material possibilities. Knowledge-culture also has a negative constituent, in terms of knowledge that does not become known. The study of why some knowledge fails to be known, becomes unlearned or is sidelined has been called agnatology or epistemologies of ignorance (e.g. Schiebinger, 2004; Tuana, 2004, 2006). Epistemologies of ignorance shape scientific imaginaries about women’s sexual and/or reproductive bodies, especially about vaginas (Braun & Kitzinger, 2001; Braun & Wilkinson, 2001). My aim is to illustrate how abject nomenclature contributes to epistemologies of ignorance about vaginal fluid, and shapes and delimits the scientific imaginary of vaginal fluid, in the brief lab-based feminist science case study. Among other intersectional locations, gender is inextricably tied to scientific imaginaries. Gender-inflected metaphors direct lines of scientific questioning and the patterns scientists are able to see and/or value in their results (Martin, 1991). Gender and sexuality are implicit, and sometimes explicit, in the language scientists use to discuss their research findings and construct scientific stories and facts (Terry, 2000). Gender also influences the terminologies scientists use to label scientific phenomenon (e.g. how oestrogen came to be named in light of specimen collections from Women’s Health Clinics,1 Oudshoorn, 1994) via gendered norms of sexuality (e.g. Dolly, the cloned sheep2 ). But nomenclature can shape the scientific imaginary in gendered ways even when these terminologies themselves do not visibly inhere gender or its metaphors (Braun & Wilkinson, 2001), as I aim to demonstrate with vaginal fluid. This article follows the tradition of ‘case studies’ in feminist science and research (e.g. Braun, 1999; Weasel, 2004), which are ways to present examples of feminist engagement with scientific laboratory practice. Feminist science case studies are especially useful because they allow practicing scientists space to be self-reflexive about scientific practice, which is more typically silenced or discouraged within scientific communities. Feminist lab case studies are one way to open up conversations about feminist science that are rooted in and relevant to scientists’ experiences. They allow for the building up of feminist science practice for scientists and other scholars interested in engaging with science. In this vaginal fluid case study, I argue that scientific terminologies not only channel the scientific imaginary into seeing certain questions as more askable, feasible or merit-worthy than others, but that nomenclature can render entire topics invisible and thus contribute to gendered epistemologies of ignorance. In other words, nomenclature can affect whether and how a question resonates within the scientific imaginary but, more than that, it can also affect whether a question even can be posed; feminist engagements can render these epistemologies of ignorance visible and extend existing boundaries of the scientific imaginary. Social neuroendocrine research on sexuality: how I got into vaginas My research programme focuses on hormones and intimacy in social context. In one line of research, my lab’s work has shown that some forms of sexuality (penis–vagina intercourse; sexual cognitions) increase testosterone in women (Goldey & van Anders, 2011; van Anders, Hamilton, Schmidt, & Watson, 2007). I am particularly interested in what we call the ‘reverse relationship’ (van Anders & Watson, 2006) of how social experiences and contexts influence hormone levels, in part because it expands and plays with traditional notions of nature/nurture dichotomies. It is exciting to be doing scholarly work that simultaneously contributes to bioknowledge and troubles biological determinism by highlighting the malleability and social situatedness of hormones and bioprocesses. Psychology & Sexuality 351 Hormones and social processes are intertwined, but so are hormones and other physiological parameters like the immune system. So, I am interested both in sexual modulation of hormones like testosterone (i.e. how sexuality affects testosterone, with sexuality including sexual activity or thoughts) but also in the physiological sequelae3 of these sexuallyinduced changes in testosterone (i.e. how the changes in testosterone from sexual activity affect immune processes). Accordingly, in addition to social modulation of hormones, my lab examines the social modulation of immune function in relation to sexuality. And this is where vaginas come in. Like the mouth, the vaginal surface is a mucosal membrane through which pathogens easily pass, necessitating immune defences. Downloaded by [141.211.129.84] at 11:23 23 October 2014 Enter vaginal fluid Vaginal fluid is largely understood to be, in scientific terms, ‘all kinds of awesome’. Vaginal fluid makes vulvas and vaginas slick, making penetration more comfortable and enjoyable for many folks.4 Much more surprising, however, are some quite amazing properties of vaginal fluid. It fights against sexually transmitted infections (STIs) or – more accurately – contains numerous immune parameters that defend against pathogens (Anderson et al., 2009; Weissenbacher et al., 2009). Vaginal fluid fights herpes (John et al., 2005). It fights HIV (Kaushic, Ferreira, Kafka, & Nazli, 2010; Mestecky, Kutteh, & Jackson, 1994). It will chase after burglars and rescue treed kittens. I like to think of vaginal fluid as wearing a cape and tights, because it is just that super. But I became thoughtful about how surprising these super powers were to me, a feminist scientist who already studied sexuality, gender/sex5 and bodily fluids. I wondered ‘Why are the STI-fighting abilities of vaginal fluids a part of its secret identity rather than a known aspect of its day job?’ I’ll come back to this. In my lab, we have become interested in sexuality and vaginal immunity, which we test via – no surprise here – vaginal fluid. Traditionally, researchers have measured vaginal immune parameters using a vaginal lavage (wash). A vaginal lavage is like a vagina gargle . . . if you gargled by having a health professional squirt fluid into your orifice with a glorified turkey baster while you were lying on your back in a clinic with your knickers off, then had it sucked it up with said baster by said professional to have your orifice flushed again, and then did a ‘rinse and repeat’ a few more times. In my research, we collect vaginal fluid by asking women to wear slender tampons for brief periods of time in their own homes without us present.6 We see this as relatively noninvasive, though I realise you might be thinking that the tampons go into vaginas and that ‘noninvasive’ is a sleight of hand term to use here . . . but consider the vagina gargle alternative above. And you know, after decades of putting tampons in my own vagina, they seem pretty ho-hum to me, especially compared to vaginal lavages or blood draws or other methods of sampling bodily fluids. In fact, I am going to put myself on the line and speculate that large numbers of women who have previously used tampons are probably more comfortable putting and taking out a slender tampon than they are spitting into our saliva tubes. To use tampons for collecting vaginal fluid, we had to validate the tampon method against the vagina gargle method, and – if recruitment is any indication – few women are interested in the vagina gargle7 (surprise!). We had to do this cross-validation even though others had published about their use of tampons in this way (e.g. Johansson, Wassen, Holmgren, Jertborn, & Rudin, 2001), which means that the tampon method had already been validated in most senses. Really, a tampon is like a swab of sorts, and swabs are routinely used to soak up other bodily fluids like saliva. But women insert tampons into their own bodies, and I suspect that this self-use (and perhaps ease of use) is what makes them suspect (the tampons! not the women . . . or is it the other way around?). For tampons Downloaded by [141.211.129.84] at 11:23 23 October 2014 352 S.M. van Anders to exist in the scientific imaginary as a valid method of sample collection, the following conditions need to be met: we have to trust that women are capable of using tampons; we have to trust that women are capable of using tampons by themselves, with no scientists or health professional to monitor them; we have to conceive of the possibility that something only women are perceived to do8 could be scientifically valuable and, of course, we have to think of tampons themselves outside an androcentric context of menstrual disgust and discomfort. Now might be a good time to recap: vaginal fluid is a critical agent in fighting STIs and reducing initial HIV infection, it has measurable immune properties and it’s easily and noninvasively self-collected by women without any special training or health professionals. Yet, one might easily think that vaginas are passive receptacles for disease resulting from penile penetration (Braun & Kitzinger, 2001; Braun & Wilkinson, 2001), despite the very agentic role vaginal fluid can play. So, why don’t we know more about vaginal fluid? Scratch that. The question is, actually, why do not most of us know much of anything about vaginal fluid? Nomenclature constitutes knowledge-culture The absence of vaginal fluid parallels what Braun and Wilkinson have identified as the ‘absence of vaginas’ alongside other cultural vaginal representations (Braun & Wilkinson, 2001). I think of vaginal fluid as vaginal fluid and so I don’t mind collecting, storing and measuring it. A large number of folks9 (scientists, laypeople, etc.), however, use terms like vaginal mucous or vaginal discharge. For example, the online biomedical search engine PubMed (U.S. National Library of Medicine & National Institutes of Health, 2013) returns 697 results for a search on ‘vaginal fluid’ but 2498 results for ‘vaginal discharge’. A Google Trends search (Google, 2013) shows that ‘vaginal discharge’ is searched for orders of magnitude more frequently than ‘vaginal fluid’ (or ‘vaginal mucus’, for that matter). I think these terms directly contribute to epistemologies of ignorance. They limit our ability to think seriously about vaginal fluid as something valuable or scientifically meaningful. As Whitford notes, mucus is uncomfortably close to the abject (Whitford, 1991). This abject nomenclature has contributed to an epistemology of ignorance around vaginal fluid that restrains the desire to think about it, much less conduct research on vaginal immunity. This nomenclature precludes our ability to incorporate vaginal fluid or immunity into the scientific imaginary. You know what mucous is? My personal definition of mucous is a lumpy, clumpy, glutinous, semi-adhering mystery substance that is neither fully liquid nor solid. Mucous is what you pick or blow from your nose, or what embarrasses you after you surface from jumping into a pool. Mucous seeps from healing or infected sores and – if you’re lucky – mucous is clear or white, but it could be yellow, neon green (the horror!) or tinged red with blood. Mucous is, in a word, evocative of all things disgustful. And what about discharge? Discharge is definitionally unneeded/unwanted, a waste product, a sign that something is not right. Discharge is dairy-free cottage cheese, a yeast infection. Discharge itches. Vaginal mucous and vaginal discharge are passive – or passive aggressive – in their existence, a very unwelcome signal of other things gone wrong, of dis-ease. Vaginal mucous and vaginal discharge claim our attention only because of their abjectness. We’d rather they didn’t exist, really. But semen! Semen is an autobiography of what a penis can do. Semen is autonomous in that it evokes nothing but itself. Semen carries baggage, of course – like warnings, power, fertility, embarrassment – but is almost the opposite of abject as evidenced by the title of Lisa Jean Moore’s book on sperm and semen ‘Sperm Counts: Overcome by Downloaded by [141.211.129.84] at 11:23 23 October 2014 Psychology & Sexuality 353 Man’s Most Precious Fluid’ (Moore, 2007). In this book, Moore describes how semen and sperm are accorded social value as proxies for (valued) masculinity. And, though semen is described as gelatinous by Moore and the authors she cites, the terms ‘mucus’ and ‘discharge’ are used only to refer to vaginal fluid, never to semen. Given that the vagina is seen as inferior to the penis, it is far from surprising that vaginal fluid should be seen so pejoratively in comparison with ‘penile fluid’ (or semen) (Braun & Wilkinson, 2001). In general parlance, semen is rhetorically seminal, whereas vaginal mucous and discharge are semantically derivative. That semen is often mucusy, clumpy, odorous and not entirely lacking in hue seems irrelevant. Yet, vaginal mucous and discharge have no fighting chance in the arena of cultural value because of their very names, in part. Which is odd, when you consider how much of a fight they do put up, immunologically speaking, and how often they win.10 But, you might moan, the vagina’s surface IS a mucous membrane. And therefore why not vaginal mucous? Yes, the vagina’s surface is a mucous membrane. The mouth’s surface is a mucus membrane too. As is the lining of the nose, the eyes and the penile urethra. But we give names to the fluids that are associated with these other mucous membranes. We do not call saliva ‘mouth discharge’. And, we do not call semen ‘penile mucous’. This case study, however, is not a call to outlaw the terms ‘mucus’ or ‘discharge’, which clearly have their health-related and biomedical utility. Instead, I aim to make the point that a term like ‘vaginal fluid’ is less likely to contribute to the very epistemologies of ignorance surrounding women’s bodies. Accordingly, vaginal fluid may be useful for, well, fluid from and in vaginas. Discharge and/or mucus may be appropriately retained for use in contexts of illness, disease or health issues. The use of terms that indicate disease as normative terms for women’s bodies pose, however, serious challenges to a more comprehensive scientific imaginary that takes women’s bodies and/or vaginas seriously. You might argue, people DO use the term penile mucous. And therefore Equality! Yes, penile mucous is a term that is used. But it is used very infrequently, and then only by clinicians, health professionals, and basically no one else. Penile mucous refers to fluids that seep from the penis and signify something gone wrong. That the use of the term ‘penile mucous’ is limited to illness and the health/biomedical community, whereas vaginal mucus/discharge is used widely and normatively to refer to even healthy bodily functions in women supports the point I am making. In other words, language around vaginal fluid is abject in a particularly gendered way. So, why don’t we know much about vaginal fluid? Where is vaginal fluid in the public or scientific imaginary? Why does the study of vaginal fluid necessitate discussing epistemologies of ignorance? Well, who the fuck wants to study mucous and discharge? They are fucking gross. And I am not talking gross by dint of vaginal source; I mean, mucous and discharge are gross regardless of where they originate. Who wants to collect glumpy mucous? Store abject discharge in their lab? Train undergraduates and graduate students to handle tubes filled with signs of dis-ease? Who wants to tell people that they study glutinous vagina output unless the rationale is to solve said glutinousness? Vaginal mucus and discharge cannot really exist in the scientific imaginary except on those occasions when they do as clinical problems. They sometimes are clinical problems, so it is important that they are studied in this way. But calling vaginal fluid ‘vaginal discharge’ or ‘vaginal mucous’ makes vaginal fluid an unlikely topic or medium for science outside of this specific sphere. Language choice constrains what is knowable, and therefore what can be interesting or worth examining. Nomenclature directly contributes to epistemologies of ignorance. We cannot know how ‘awesome’ (in scientific terms) vaginal fluid is when we think of Downloaded by [141.211.129.84] at 11:23 23 October 2014 354 S.M. van Anders vaginal mucous and discharge as the physical embodiment of abject. We cannot think of vaginas as agents of change – or, really, as agentic at all – when our terminologies position vaginas and their output as passive indicators of dis-ease. We cannot study how vaginal mucous or discharge might be part of the solution for engaging with STIs and stemming the tide of vaginally-acquired HIV when we cannot even conceptualise why anyone would want to collect such a disgustful substance. Language choice, as with this example of vaginal fluid, matters for the scientific imaginary because of its social location and the social location of scientists. To be clear, I am far from the first to suggest that scientific terminologies are inflected by culture and that these cultural blinders delimit scientific questions and research (e.g. Dreger, 1998; Fausto-Sterling, 2000; Harding, 1991; Mayberry et al., 2001). I am also not the first to study the powerful qualities and actions of vaginal fluid. And, (a very few) feminist scholars like Luce Irigaray have pointed to alternative views of vaginal mucus, albeit ones potentially located in difference feminism (Whitford, 1991). Instead, my point is to provide an additional and specific feminist science case study about how the naming of women’s bodies, sexualities and outputs has foreclosed the possibilities that research starting from agentic women’s bodies might afford. But only in so much as we use this hegemonic language. So, our language matters, because terminology delimits what methods we use. Our scientific nomenclature creates a knowledge culture, a culture of what is knowable, and this affects the scientific imaginary. Nomenclature affects how we know things, and also how we do not. In other words, vaginal mucus and vaginal discharge contribute to vaginal epistemologies of ignorance. Vaginal fluid, instead, might contribute to epistemologies, to an opening up of scientific imaginaries. Who chooses names? Who asserts nomenclatures? The scientific imaginary is both a reflection and a result of cultural forces. Vaginal fluid is obviously a biological and physiological entity even as it simultaneously is a cultural one. I have argued that its location in knowledge-culture affects its location in the scientific imaginary; this procession directly affects the biological and physiological properties of vaginal fluid, in so far as we are able to understand them. In this way, the terms we use to refer to vaginal fluid in our everyday science ends up constituting its very biological, physiological and immunological potentials and properties. So what would happen if increasing numbers of scientists, lay people and scholars used vaginal fluid rather than its more abject terms? Even health professionals could use the term ‘vaginal fluid’ in context-specific ways, for example, when talking about taking samples for testing, or checking fluids for signs of menstrual phase rather than using language that implicitly positions vaginal output as symptom. Nomenclature seems to be a strictly scientific endeavour but is, after all, the decision of scientists and practitioners, a property of science (day-to-day lab work) rather than Science (epistemological decisions). So, rather than contributing to vaginal epistemologies of ignorance that may have implications for research on STIs in addition to ‘merely’ diseasing women’s bodily functions in general, why not a quiet change? Why not attend to women’s bodies and/or vaginas in less stigmatised ways (Chrisler, 2011)? Vaginal fluid is, after all, only what we actually call it. And what we call vaginal fluid seems intimately tied to whether we see scientific value in it. Notes 1. Oestrogens were first measured from fluid samples collected from women at Women’s Health Clinics, which were largely organised around reproductive issues (e.g. related to menstrual cycles, fertility, menopause, pregnancy) (Oudshoorn, 1994). ‘Oestrogen’ comes from creating Psychology & Sexuality 2. 3. 4. Downloaded by [141.211.129.84] at 11:23 23 October 2014 5. 6. 7. 8. 9. 10. 355 ‘oestrus’, which is the reproductive phase of female non-human animal cycles. ‘Oestrus’ itself linguistically means ‘possessed by the gadfly’, referring to the ‘madness’ that was said to characterise non-human female sexual behaviour during their fertile phases (Fausto-Sterling, 2000). Because there were no comparable Men’s Health clinics, androgens were not first measured in relation to reproductive or clinical issues per se, and ‘androgen’ simply refers to creating man; the parallel term for oestrogens would have been gynogen. As the lead scientist on the project is widely reported to have said (CBC News & Morales, 2007): ‘Dolly is derived from a mammary gland cell and we couldn’t think of a more impressive pair of glands than Dolly Parton’s’. A term used in behavioural neuroendocrinology to denote effects, or downstream events in a chain. But see (Mbikusita-Lewanika, Stephen, & Thomas, 2009) for interesting discussions on dry sex. I use ‘gender/sex’ in most of my studies (at least when editors will allow it) because I study adults and typically cannot know whether any given phenomenon I am studying is related to gender (i.e. social, historical, contextual) or sex (i.e. innate, inborn, evolved, fixed). This is true even when I am studying biological processes, because social context can influence biology. And, we only enrol women who are comfortable using tampons and have a history of using them. At least, its clinical version. I say ‘perceived’ because people with menstruating vaginas, including transmen, also use tampons. I would like to be clear that I do not mean to imply all folks here. If you are a health professional or scientist or generally awesome person that uses ‘vaginal fluid’, I congratulate you and do not mean you here. In fact, I do not mean any one person in this article; I’m talking about cultural norms that influence how each of us think and act, even the most progressive and feminist of us (who hopefully would be interested in reflecting upon practices that may contain hegemonic norms, and changing them). I want to briefly mention that vaginal fluid alone will not prevent STIs and that use of barrier methods like condoms or dams are the only known methods for reducing the risk of STIs. Notes on contributor Sari van Anders is an Assistant Professor of Psychology and Women’s Studies. The lab’s research focuses on hormones and intimacy in social and evolutionary context, with attention to gender/sex, sexual diversity and feminist science practice, as well as the health implications of dynamic social (and socially situated) endocrinology. References Anderson, D. J., Williams, D. L., Ballagh, S. A., Barnhart, K., Creinin, M. D., Newman, D. R., . . . Jamieson, D. J. (2009). Safety analysis of the diaphragm in combination with lubricant or acidifying microbicide gels: Effects on markers of inflammation and innate immunity in cervicovaginal fluid. American Journal of Reproductive Immunology (New York, NY: 1989), 61(2), 121–129. doi:10.1111/j.1600–0897.2008.00670.x Braun, V. (1999). Breaking a taboo? Talking (and laughing) about the vagina. Feminism and Psychology, 9, 367–372. Braun, V., & Kitzinger, C. (2001). Telling it straight? Dictionary definitions of women’s genitals. Journal of Sociolinguistics, 5, 214–232. Braun, V., & Wilkinson, S. (2001). Socio-cultural representations of the vagina. Journal of Reproductive and Infant Psychology, 19, 17–32. CBC News & Morales, S. (2007). Send in the clones: The science of cloning, a decade after dolly. Retrieved from http://www.cbc.ca/news/background/genetics_reproduction/sciencecloning.html Chrisler, J. C. (2011). Leaks, lumps, and lines: Stigma and women’s bodies. Psychology of Women Q, 3(5), 202–214. Dreger, A. D. (1998). Hermaphrodites and the medical invention of sex. Cambridge, MA: Harvard University Press. Downloaded by [141.211.129.84] at 11:23 23 October 2014 356 S.M. van Anders Fausto-Sterling, A. (2000). Sexing the body: Gender politics and the construction of sexuality. New York, NY: Basic Books. Goldey, K. L., & van Anders, S. M. (2011). Sexy thoughts: Effects of sexual cognitions on testosterone, cortisol, and arousal in women. Hormones and Behavior, 59(5), 754–764. doi:10.1016/j.yhbeh.2010.12.005 Google. (2013). Google trends. Retrieved from http://www.google.com/trends/ Haraway, D. (1988). Situated knowledges: The science question in feminism and the privilege of partial perspective. Feminist Studies, 14(3), 575–599. Harding, S. G. (1986). The science question in feminism. Ithaca, NY: Cornell University Press. Harding, S. G. (1991). Whose science? Whose knowledge? Thinking from women’s lives. Ithaca, NY: Cornell University Press. Johansson, E. L., Wassen, L., Holmgren, J., Jertborn, M., & Rudin, A. (2001). Nasal and vaginal vaccinations have differential effects on antibody responses in vaginal and cervical secretions in humans. Infection and immunity, 69(12), 7481–7486. doi:10.1128/IAI.69.12.7481–7486.2001 John, M., Keller, M. J., Fam, E. H., Cheshenko, N., Hogarty, K., Kasowitz, A., & Herold, B. C. (2005). Cervicovaginal secretions contribute to innate resistance to herpes simplex virus infection. The Journal of Infectious Diseases, 192(10), 1731–1740. doi:10.1086/497168 Jordan-Young, R. M. (2010). Brain storm: The flaws in the science of sex differences. Cambridge, MA: Harvard University Press. Kaushic, C., Ferreira, V. H., Kafka, J. K., & Nazli, A. (2010). HIV infection in the female genital tract: Discrete influence of the local mucosal microenvironment. American Journal of Reproductive Immunology (New York, N.Y.: 1989), 63(6), 566–575. doi:10.1111/j.1600–0897.2010.00843.x Martin, E. (1991). The egg and the sperm: How science has constructed a romance based on stereotypical male-female roles. Signs: Journal of Women in Culture & Society, 16(3), 485–501. Mayberry, M., Subramaniam, B., & Weasel, L. (Eds.). (2001). Feminist science studies: A new generation. New York, NY: Routledge. Mbikusita-Lewanika, M. F., Stephen, H. F., & Thomas, J. (2009). The prevalence of the use of ‘dry sex’ traditional medicines, among zambian women, and the profile of the users. Psychology Health & Medicine, 1(4), 227–238. Mestecky, J., Kutteh, W. H., & Jackson, S. (1994). Mucosal immunity in the female genital tract: Relevance to vaccination efforts against the human immunodeficiency virus. AIDS Research and Human Retroviruses, 10(Suppl. 2), 11–20. Moore, L. J. (2007). Sperm counts: Overcome by man’s most precious fluid. New York, NY: New York University Press. Oudshoorn, N. (1994). Beyond the natural body: An archaeology of sex hormones. Abingdon: Routledge. Schiebinger, L. (2004). Feminist history of colonial science. Hypatia, 19, 233–254. Terry, J. (2000). ‘Unnatural acts’ in nature: The scientific fascination with queer animals. GLQ: A Journal of Lesbian and Gay Studies, 6(2), 151–193. Traweek, S. (1992). Beamtimes and lifetimes: The world of high energy physicists. Cambridge, MA: Harvard University Press. Tuana, N. (2004). Coming to understand: Orgasm and the epistemology of ignorance. Hypatia, 19(1), 194–232. Tuana, N. (2006). The speculum of ignorance: The women’s health movement and epistemologies of ignorance. Hypatia, 21(3), 1–19. U.S. National Library of Medicine, & National Institutes of Health. (2013). PubMed.gov. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/ Weasel, L. (2004). Feminist intersections in science: Race, gender and sexuality through the microscope. Hypatia, 19(1), 183–193. Weissenbacher, T. M., Witkin, S. S., Gingelmaier, A., Scholz, C., Friese, K., & Mylonas, I. (2009). Relationship between recurrent vulvovaginal candidosis and immune mediators in vaginal fluid. European Journal of Obstetrics, Gynecology, and Reproductive Biology, 144(1), 59–63. doi:10.1016/j.ejogrb.2009.01.010 Whitford, M. (1991). Irigaray’s body symbolic. Hypatia, 6(3), 97–110. van Anders, S. M., Hamilton, L. D., Schmidt, N., & Watson, N. V. (2007). Associations between testosterone secretion and sexual activity in women. Hormones and Behavior, 51(4), 477–482. doi:10.1016/j.yhbeh.2007.01.003 van Anders, S. M., & Watson, N. V. (2006). Social neuroendocrinology: Effects of social contexts and behaviors on sex steroids in humans. Human Nature, 17(2), 212–237.