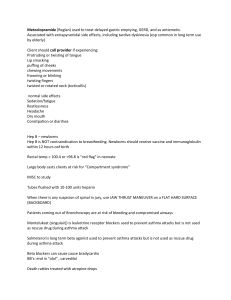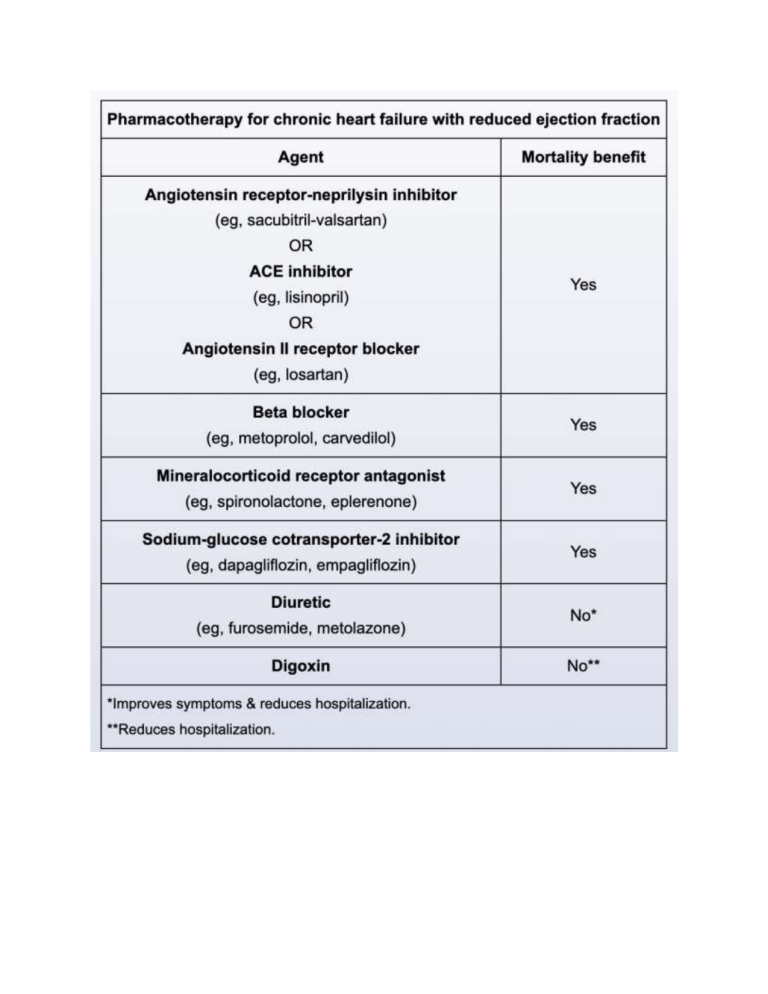
HCM is inherited in an autosomal dominant fashion, resulting from mutation in genes encoding for myocardial contractile proteins of the cardiac sarcomere. Cardiac myosin-binding protein C and cardiac beta-myosin heavy chain are most commonly affected, accounting for approximately 40% and 30% of identifiable mutations, respectively. Affected patients often have a recognizable family history of HCM but not always because sporadic mutations can occur Mechanical prosthetic aortic valve can present with prosthetic valve dysfunction (PVD), which most commonly occurs in the following forms: Paravalvular leak (regurgitation around the valve): more commonly with mechanical (rather than bioprosthetic) valves and results from dehiscence of the valve from the aortic or mitral annulus, often due to annular degeneration or underlying infective endocarditis. Transvalvular regurgitation (regurgitation through the valve): more commonly affects bioprosthetic (rather than mechanical) valves and can result from cusp degeneration or occasionally valvular thrombus that impairs valve closure. Patients are often initially asymptomatic but can develop severe heart failure; those with significant regurgitation generally have a poor prognosis. Diagnosis of exclusion Ventricular aneurysm Pulsus paradoxus can be seen in COPD and asthma Nitrates cause vasodilation decreasing systemic vascular resistance Coronary stent thrombosis is a serious complication of coronary stent placement that can occur acutely (within 24 hours) or subacutely (within 30 days) or be delayed up to a year or more. The risk is greatest prior to reendothelialization because exposed stent material is thrombogenic Sarcoidosis cardiac manifestations Aspirin is a common trigger for bronchoconstriction in patients with asthma, especially those with concurrent chronic rhinitis and nasal polyps. Nonselective beta blockers (eg, propranolol, nadolol, sotalol, timolol) act on β1 and β2 receptors and often trigger bronchoconstriction in patients with underlying asthma. Cardioselective beta blockers (eg, metoprolol, atenolol, bisoprolol, nebivolol) act predominantly on β1 receptors and are generally considered safe in patients with mild-to-moderate asthma. However, all beta blockers can trigger bronchoconstriction, especially when administered in large doses. This medication-triggered bronchoconstriction can lead to a cough. In addition, ACE inhibitors (eg, lisinopril) can cause dry cough through increased levels of circulating bradykinin and resultant bronchial irritation. Onset of the cough can occur soon after ACE inhibitor initiation (as is likely the case in this patient) or can be delayed (eg, months); it is not affected by underlying asthma.