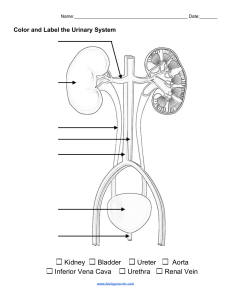
GENITO-URINARY SYSTEM DISORDER Outline Overview of the renal system Urinary tract infections (UTI) Nephrotic syndrome Renal failure (acute and chronic) Overview of anatomy and physiology – The renal and urinary systems include: the kidneys ureters bladder urethra – Urine is formed by the kidney and flows through the other structures to be eliminated from the body. – Kidneys A pair of bean-shaped, brownish-red structures located retroperitoneally on the posterior wall of the abdomen. Average adult ~113 to 170g, 10 to 12 cm long, 6 cm wide, 2.5 cm thick The right kidney is slightly lower than the left. Each kidney has 1 million nephrons responsible for urine formation – Blood Supply to the Kidneys Receive 20% to 25% of the total cardiac output. Ureters, Bladder, and Urethra – Ureters: – Urinary bladder: – Long, narrow fibromuscular tubes that receive urine form renal pelvis and pass to the bladder. It is 24 to 30 cm long, originate at the lower portion of the renal pelvis and terminate in the trigone of bladder wall. Is a muscular, hollow sac located just behind the pubic bone. Capacity of the adult bladder is 400 to 500 mL It has two inlets (the ureters) and one outlet (the urethra) Urethra: Arises from the base of the bladder Male: passes through the penis surrounded by prostate Female: it opens just anterior to the vagina – Function of the renal and urinary systems Is essential to life The primary purpose is: to maintain the body’ s state of homeostasis by: regulating fluid and electrolytes, removing wastes, providing other functions – Dysfunction of the kidneys and lower urinary tract is common and may occur at any age with varying degrees of severity. – Functions of the Kidney Urine formation Excretion of waste products Regulation of electrolytes Regulation of acid– base balance Control of water balance Control of blood pressure Renal clearance Regulation of red blood cell production Synthesis of vitamin D to active form Secretion of prostaglandins Regulates calcium and phosphorus balance Assessment of urinary system Assessment of the disorder of urinary system is performed By Subjective finding patient health history By Objective finding Physical examination: Observation; Palpation; Percussion and Auscultation 8 Physical Examination Weighing patient Look for skin turgor, Scratch, Color, Edema, Genital area for infection. Inspect and palpate bladder Palpate kidney at CVA Fist percussion at flank area for tenderness Check fluid overload on lung by auscultation 10 Diagnostic Evaluation – – – Comprehensive health history and physical – examination Urinalysis and Urine Culture: Urine color Urine clarity and odor Urine pH, Osmolality and specific gravity Tests to detect protein, glucose, and ketone bodies Microscopic examination RFT: renal concentration tests, creatinine clearance, serum creatinine, BUN, serum electrolyte levels Imaging: x-ray, Ultrasonography, CT scans, MRI, Intravenous Urography, Retrograde Pyelography, Cystography, Angiography, Urologic Endoscopic Procedures URINARY TRACT INFECTION – – – – Urinary tract infections (UTIs) are infections of the urinary tract. They are the most common outpatient infection. Escherichia coli is the most common pathogen causing a UTI. Fungal and parasitic infections sometimes cause UTIs. Classification of Urinary Tract Infection – – UTIs can be classified based on its location as an upper or lower UTI We use specific terms to describe the location of a UTI. For example, pyelonephritis implies inflammation (usually caused by infection) of the renal parenchyma and collecting system. Cystitis is an inflammation of the bladder. Urethritis is an inflammation of the urethra. – We also classify a UTI as Uncomplicated UTIs occur in an otherwise normal urinary tract. They usually only involve the bladder. Complicated UTIs occur in a person with an underlying disease or with a structural or functional problem in the urinary tract. • Examples include obstruction, stones, catheters, abnormal genitourinary (GU) tract, acute kidney injury (AKI), chronic kidney disease (CKD), kidney transplant, diabetes, or neurologic disease. Etiology and Pathophysiology – – – The urinary tract above the urethra is normally sterile. Several mechanical and physiologic defense mechanisms aid in maintaining sterility and preventing UTIs. These defenses include normal voiding with complete bladder emptying, ureterovesical junction (UVJ) competence, and ureteral peristaltic activity that propels urine toward the bladder. Most UTIs result from fecal organisms that ascend from the perineum to the urethra and the bladder and then adhere to the mucosa Bacterial invasion of the urinary tract by: Urethrovesical reflux, which is the reflux (backward flow) of urine from the urethra into the bladder. Vesicoureteral reflux refers to the backward flow of urine from the bladder into one or both ureters. Clinical Manifestations – Manifestations of UTIs range from painful urination in uncomplicated urethritis or cystitis to severe systemic illness with abdominal or back pain, fever, and sepsis. – – Lower urinary tract symptoms (LUTS) occur in patients who have UTIs of the upper urinary tract, as well as those confined to the lower tract. Symptoms are related to either bladder storage or bladder emptying . – – – – The urine may have grossly visible blood (hematuria) or sediment, giving it a cloudy appearance. Upper UTIs (involving the renal parenchyma, pelvis, and ureters) typically causes fever, chills, and flank pain. A UTI confined to the lower urinary tract does not usually have systemic manifestations. People with significant bacteriuria may have no symptoms or may have nonspecific symptoms, such as fatigue or anorexia – Diagnostic Assessment History and physical assessment Urinalysis (midstream, “cleancatch” voided specimen) Urine for culture and sensitivity (if indicated) Imaging studies of urinary tract (if indicated): CT scan, ultrasound, cystoscopy – Management Uncomplicated UTI Patient teaching Adequate fluid intake (8 to 9 8oz glasses/day) – Drug Therapy – Antibiotics fluconazole Recurrent UTI Repeat urinalysis Urine culture and sensitivity testing Adequate fluid intake (8 to 9 8oz glasses/day) Repeat patient teaching Imaging studies of urinary tract (if indicated) (in patients with fungal UTI) fosfomycin (Monurol) nitrofurantoin (Macrodantin, Macrobid) TMP/SMX (Bactrim, Bactrim DS) trimethoprim alone (in patients with sulfa allergy) cephalexin – Drug Therapy Antibiotic: nitrofurantoin, TMP/SMX Sensitivity-guided antibiotic therapy: ampicillin, amoxicillin, 1st- or 2nd-generation cephalosporin, fluoroquinolones 3- to 6-month trial of suppressive or prophylactic antibiotic therapy Postcoital antibiotic prophylaxis: cephalexin, nitrofurantoin, TMP/SMX, fosfomycin, trimethoprim Urethritis – – Definition: Inflammation of the urethra is usually an ascending infection and may be classified as:- Gonococcal and Non gonococci Gonococcal urethritis is caused by N. Gonorrhea and is considered as STDS. • Symptoms, in men – burning sensation on urination, purulent discharge via urethral meatus, • – in females it is asymptomatic Non gonococcal urethritis is usually caused by C-trachomitis, 27 Clinical features of all urethritis Acute dysuria, frequency, and pyuria, gross hematuria, Suprapubic or pelvic pain with abrupt onset of illness. Nocturia Incontinence Back pain Urine discoloration, dribbling, Burning sensation Pusy or foamy discharge In patients with complicated UTIs manifestations can range to sepsis with shock 28 Diagnostic tests – Urine analysis – CBC – Urine culture and sensitivity – Wet smear – Digital finger examination – Gram stain 29 Medical management 1. Based on the cause For gonococal case of STD Rx :- Ceftriaxone 250 mg IM stat OR spectinomycin 2gm IM stat plus Azythromycin 1gm po stat For fungal case : Clotrimazole 200 mg vaginal tab at bed time for 3 days For herpus simplex type 2, Acyclovir 800mg bid For trichomonas vaginalis, metronidazole 2 gm po stat 30 31 2. Based on severity For simple or uncomplicated UTI: 1. 2. 3. 4. Ciprofloxacin 500 mg bid for 05 days or Norfloxacin 400mg bid for 710 days or Doxycycline 100 mg bid for 710 days or Amoxicillin 500mg tid for 5-7 days For complicated and recurrent UTI:1. Ceftriaxone 1gm IV/IM bid for 03 days or 2. Gentamycin 80 IM/IV TID for 5-7 days 3. Cefix 200mg po daily for 05 days Nursing management – – – – – – – A high (2 L daily) fluid intake should be encouraged during treatment and for some subsequent weeks. Safe sexual intercourse Appropriate taking of prescribed drugs Frequent voiding Frequent personal hygiene Use appropriate sanitary pad Circumcision for male patients 32 Cystitis 33 – – Definition: Is inflammation of the urinary bladder Cause: ascending infection from the urethra, urethrovesical reflux, fecal contamination, Use of catheter or cyst scope Risk factors Inability or failure to empty the bladder completely Obstructed urinary flow Immuno-suppression Instrumentation Contributing conditions including DM, pregnancy, gout neurologic disorders Anal sex Clinical manifestations – Frequency and urgency of urination – Burning and pain on urination, – Suprapubic pain or spasm and urine retention ,hesitancy, – Nocturia, dysuria and Foul smelling urine, – In some clients hematuria and pyuria (WBC or pus in urine), – There may be fever, nausea, vomiting malaise, dizziness and flank tenderness 34 Diagnostic tests – Urine analysis – Urine culture – Ultrasound – Gram stain – Antibody – coated bacterial test – Complete blood cell count 35 Medical management – Ciprofloxacin 500mg bid for 05 days or – Cotrimoxazole 960 mg bid for 7-10 days or – Cefix 200mg daily for 5-7 days or – Cephalexin 500mg bid for 5-7 days or – Ceftriaxone 1 gm IV/IM bid for 3-5 days or – Gentamycin 80 mg IV/IM tid 5-7 days 36 Nursing management – – – – – – – – – Encourage high fluid intake Voiding after sexual intercourse Circumcision for male Keep personal hygiene Encourage shower bath rather tub bath Keep the dryness of perineal area Follow strict sterility during instrumentation Avoid taking of very irritant drinks and foods to bladder Encourage frequent urine voiding 37 Upper Urinary Tract Infection An infection of ureter (ureteritis) and kidney (pyelonephritis) Pyelonephritis is a bacterial infection of the renal pelvis, tubules, and interstitial tissue of one or both kidneys, by bacteria that come from bladder and rarely from blood Pyelonephritis can be acute or chronic Chronic pyelonephritis usually has no symptoms of infection unless an acute exacerbation occurs 38 Pyelonephritis – Inflammation of the renal pelvis, and kidney tissues Acute----Bacterial ”ascending infection”. Chronic----Non bacterial and inflammatory processes. Acute pyelonephritis: Active infection manifested by Fever, Chills, CVA tenderness, N/V, Tachycardia, symptoms of lower UTI such as dysuria and frequency; Upper UTI is associated with antibody coating of the bacteria in the urine. Chronic Pyelonephritis: May be due to repeated bouts of acute pyelonephritis Pts have usually no symptoms of infection unless acute exacerbation occurs. Noticeable signs include Fatigue, Head Ache, Poor Appetite, Polyuria, Excessive thirst, and Weight loss. Its complication include end - stage renal disease 39 Acute pyelonephritis – Acute Pyelonephritis is a bacterial infection of the renal pelvis, tubules, and interstitial tissue of one or both kidneys, by bacteria – Pt with acute pyelonephritis usually has enlarged kidneys with interstial infestation of inflammatory cells. – Abscess may be noted, eventually atrophy and destruction of tubules and the glomeruli will be occur 40 Risk factors It is usually seen in association with pregnancy, chronic health problems, such as diabetes mellitus or hypertensive kidney disease Sexually active women ages 20 to 50 but may also occur in those who are not sexually active or in young girls. Perineal colonization by Escherichia coli [E.cloli] Sexual intercourse Insertion of instruments into the urinary tract Obstruction of the bladder or urethral with resultant stagnant of urine. 41 Pathophysiology Pyelonephritis is frequently secondary to ureterovesical reflux into the ureters Urinary tract obstruction Bladder tumors, strictures, benign prostatic hyperplasia, and urinary stones Interstitial infiltrations of inflammatory cells Abscesses Atrophy and destruction of tubules and the glomeruli When pyelonephritis becomes chronic, the kidneys become scarred, contracted, and nonfunctioning 42 Clinical Manifestations Enlarged kidneys Appears acutely ill Chills and fever Leukocytosis, bacteriuria and pyuria, Flank pain CVA tenderness Symptoms of lower urinary tract involvement such as dysuria and frequency. 43 Assessment and Diagnostic Findings Ultrasound CT scan Urine culture and sensitivity Complete blood cell count Digital finger examination Cystoscopy Antibody coated bacterial test 44 Management Patients with acute uncomplicated pyelonephritis are usually treated as outpatients if they are not dehydrated, not experiencing nausea or vomiting, and not showing signs or symptoms of sepsis. Drug therapy is almost similar with lower UTI cotrimoxazole, ciprofloxacin, gentamicin with or without amoxaccilin, ampicillin, or a third-generation cephalosporin.) 45 Nursing Management – – – – – – – Unless contraindicated fluid intake is encouraged Urine output are carefully measured and recorded,, Teach emptying the bladder regularly and performing recommended perineal hygiene. Frequent voiding Avoidance of sugars and sugary foods Avoid caffeinated drinks Drinking unsweetened cranberry juice as well as taking vitamin C with that last meal of a day 46 Prevention:– – – – – – Cleaning the urethral meatus after intercourse Urination within 15 min of sexual intercourse to allow flow of urine to expel the bacteria before specialized extensions anchor the bacteria to the walls of the urethra Having adequate fluid intake, especially water Not resting the urge to urinate Bathing in warm water without soap, bath foams etc Practicing good hygiene including wiping from the front to back to avoid contamination of the urinary tact by fecal pathogens 47 Chronic pyelonephritis – – – Repeated bouts of acute pyelonephritis may lead to chronic pyelonephritis. The infection commonly starts in the adrenal medulla and then spread adjacent cortex. The infected portion of the kidney heals, resulting in fibrosis and scarring and the kidney may become contracted and become non functional. Clinical Manifestation; Have no symptoms, unless pt has acute exacerbation Noticeable s/s may include; Fatigue, Poor appetite, Headache, Excessive thirst, Wt loss & Persistent and recurrent infection may produce progressive scarring of the kidneys with renal failure the end result 48 Diagnosis is the same to acute type Medical management – For mild case like that of acute pyelonephritis For sever and complicated form needs hospitalization and treated with: Gentamycin 80 mg IV Tid for 7-10 days or Ceftriaxone 1gm Iv Bid for 5-7 days or Ciprofloxacin 200mg IV bid for 5-7 days or Ceftazidim 2 gm IV tid for 5-7 days plus Vancomycin 1 gm Iv bid for 5-7 days 49 Nursing management – – – – – – – Monitor vital sign Q2-4 hrs, monitor urine by catheter and malodor Administer antipyretic and antibiotic Encourage adequate hydration Avoid fluid that may irritate the bladder (Eg Coffee, tea, alcohols, cola) Encourage voiding frequently Encourage perineal hygiene Educate to avoid sexual intercourse until urethritis is cured, and instruct the sexual partner to be evaluated for urethritis 50 Nephrotic syndrome – – – Type of renal failure characterized by increased glomerular permeability and massive proteinuria Seriously damaged glomerular capillary membrane Clinical findings: – proteinuria, hypoalbuminemia, diffuse edema, high serum cholesterol, hyperlipidemia Although the liver is capable of increasing the production of albumin, it cannot keep up with the daily loss of albumin through the kidneys. Pathophysiology – – Nephrotic syndrome occurs with many intrinsic renal diseases and systemic diseases that cause glomerular damage. It is not a specific glomerular disease but a constellation of clinical findings that result from the glomerular damage. Clinical Manifestations – Edema soft and pitting Periorbital dependent areas (sacrum, ankles, and hands), in the abdomen (ascites). – – – Irritability Headache Malaise Assessment and Diagnostic Findings – – – – – History Physical examination Proteinuria (albumin) exceeding 3.5 g/day is the hallmark of the diagnosis of nephrotic syndrome Increased WBCs, granular and epithelial casts in urine Needle biopsy of the kidney for histologic examination. – Medical Management Treatment is focused on: treating the underlying disease slowing progression of CKD, relieving symptoms. Typical treatment includes: Diuretics for edema, ACE inhibitors to reduce proteinuria, Lipid lowering agents for hyperlipidemia Antibiotics for infections – Nursing Management Similar to care for patient with acute glomerulonephritis and ESRD. adequate medication and dietary instructions Patients must be made aware about communicating any health related change to their health care providers as soon as possible – Complications Infection (due to a deficient immune response), Thromboembolism (renal vein, pulmonary emboli) ARF (due to hypovolemia) Atherosclerosis (due to hyperlipidemia) Renal Failure – Sever impairment or total lack of kidney function, resulting in an inability to: remove metabolic end products from the blood regulate the fluid, electrolyte, and pH balance respond to functional disturbances of all body system – can be acute or chronic Acute Renal failure /ARF/ – ARF is a sudden and almost complete loss of kidney function (ed GFR), over a period of hours or days, with progressive azotemia. – I. Prerenal Failure (hypo-perfusion of kidney) 50-70% of causes factors out side the kidneys impair renal blood flow lead to decreased glomerular perfusion and filtration – I. II. Pre-renal causes may include: Hypovolemia due to: hemorrhage dehydration burns GI losses Vasodilatation b/c of: sepsis anaphylaxis Vasodilator drugs ed CO caused by: III. myocardial infraction HF dysrhythmias cardiac shock II. Intra-renal Failure (actual damage to kidney tissue) 20-30% of causes Include conditions that lead to actual damage to the renal tissues-Acute Tubular Necrosis/ATN Nephrotoxic injury (30%) caused by drugs like: aminoglycosides, heavy metals (lead, mercury) radiocontrast agents NSAIDs ACE inhibitors – Intra-renal Failure cause… Ischemia due to renal hypo-perfusion (>50%) Medical conditions: CKD, diabetes, heart failure, hypertension, and cirrhosis can lead to ATN Myoglobinuria: trauma, crush injuries, burns Hemoglobinuria: transfusion reaction, hemolytic anemia Primary renal disorders (APN, AGN) Toxemia of pregnancy /eclampsia Systemic lupus erythematosus III. Post renal Failure (obstruction to urine flow) 1-10% of causes Involve mechanical obstruction of urinary out flow some where distal to the kidney The most common causes are: Prostate cancer Benign prostatic hyperplasia\BPH Calculi Stricture Tumors Blood clots ARF: Clinical Courses – Clinically ARF may progress through 4 phases of: A. B. C. D. Initiation Oliguria Diuresis, and Recovery I. Initiation period Begins with the initial insult Ends when oliguria develops II. Oliguric phase The most common initial manifestation Caused by a reduction in the GFR Usually occurs with in 1 to 7 days of causative event Accompanied by a rise in urea, creatinine, uric acid, organic acid & intracellular cations like K+, Mg2+ The average duration is about 10-14 days but, rarely exceeds 4 weeks the longer the oliguric phase lasts the poorer for the prognosis of renal function – Common changes that occur during oliguric phase decreased urine output fluid volume excess metabolic acidosis potassium excess waste product accumulation neurologic disorders III. Diuresis phase (high output phase) Begins with a gradual increase in the daily urine output of 1-3 liter/day, but may reach >3-5L/day Caused by osmotic diuresis due to: the high urea concentration in the glomerular filtrate the inadequate concentrating ability of the tubules Signals that glomerulus has started to recover Lab values stop to increase and eventually decrease – Because of the large losses of fluid and electrolytes, the patient must be monitored for: hyponatremia, hypokalemia dehydration – The phase may last for 1 to 3 weeks. IV. Recovery phase (convalescent phase) begins when the GFR increases so that BUN and serum creatinine levels start to stabilize and then decrease. major improvements occur in the first 1 to 2 weeks of this phase but, renal function can continue to improve for up to 12 months after ARF Some patients may experience slight reduction in kidney function for the rest of their life, so they will still be at risk for fluid and electrolyte imbalances. some patients may progress to CRF Comparing Clinical Characteristics of ARF Clinical Manifestations – – Almost every system of the body is affected Clinical manifestations are related to azotemia, as well as the underlying cause acute renal failure does not produce a classic set of symptoms. decreased urine output (70% of patients). initially, weight gain peripheral edema – Later, as nitrogenous products accumulate, symptoms of uremia may develop, including: – – Dry skin and mucous membrane If uremic pericarditis is present – – persistent nausea, vomiting and diarrhea drowsiness, headache, muscle twitching, and seizures the breath may have the odor of urine patients may appear critically ill and lethargic chest pain, a pericardial friction rub, and findings of pericardial tamponade may occur Fluid accumulation in the lungs may cause dyspnea and crackles on auscultation. Other findings depend on the underlying cause Diagnosis – – – – – – – History Physical examination RFT Serum electrolytes U/A X-ray Renal ultra sound/MRI/CT Scan ARF: Medical Management – Goal: Restore normal chemical balance Prevent complications until repair of renal tissue Restoration of renal function – Management includes: Eliminating the underlying cause Maintaining fluid balance: avoiding fluid excesses Providing renal replacement therapy (as indicated) Controlling symptoms Correcting hypovolemia (prerenal) – – – – – – Maintaining cardiac out put to ensure adequate perfusion of the kidneys Loop diuretics like furosimide /lasix/ Osmotic diuretic (manitol) to prevent volume over load Monitoring fluid intake during the oliguric phase Treat hyperkalemia Phosphate binding agents (e.g. aluminum hydroxide) to treat elevated phosphorus. – Nutritional management – phosphate restriction sodium restriction protein limited to about 1g/kg/day during oliguric phase to minimize protein breakdown. Dialysis (if indicated) Preventing Acute Renal Failure – Provide adequate hydration to patients at risk for dehydration including: before, during, and after surgery patients undergoing intensive diagnostic studies requiring fluid restriction and contrast agents patients with neoplastic disorders or disorders of metabolism (eg, gout) and those receiving chemotherapy Prevent and treat shock promptly with blood and fluid replacement Monitor central venous and arterial pressures – – – – – – – – – Hourly monitor urine output of critically ill patients Treat hypotension promptly Continually assess renal function Take precautions to ensure that the appropriate blood is administered to the correct patient Prevent and treat infections promptly Pay special attention to wounds, burns, and other precursors of sepsis. Give meticulous care to patients with indwelling catheters. Remove catheters as soon as possible. Closely monitor dosage, duration, and blood levels of all medications metabolized or excreted by the kidneys Chronic Renal Failure (End-Stage Renal Disease) – – Kidney damage that require renal replacement therapy on a permanent basis, Final (5th) stage of CKD, referred to as chronic renal failure (CRF) or ESRD Pathophysiology – – – – As renal function declines, the end products of protein metabolism accumulate in the blood. Uremia develops and adversely affects every system. The greater the buildup of waste products, the more pronounced the symptoms are. The rate of decline in renal function and progression of ESRD is related: underlying disorder, the urinary excretion of protein, the presence of hypertension. Clinical Manifestations – – Patients exhibit a number of signs and symptoms The severity of these signs and symptoms depends: the degree of renal impairment, other underlying conditions, the patient’ s age – CVD is the predominant cause of death in ESRD Assessment and Diagnostic Findings – – – – – History Physical examination Glomerular Filtration Rate Sodium and Water Retention Blood tests: Acidosis BUN, Creatinine Anemia/Hgb Calcium and Phosphorus Imbalance Medical Management – – – Goal: to maintain kidney function and homeostasis for as long as possible. All factors that contribute to ESRD that are reversible are identified and treated. Management is accomplished primarily with: Dietary therapy Medications (Calcium and Phosphorus Binders like alciumcarbonate or calcium acetate), Antihypertensive and Cardiovascular Agents (diuretic, inotropic agents), sodium bicarbonate supplements, Antiseizure (diazepam or phenytoin), erythropoietin) Dialysis KIDNEY TRANSPLANTATION – Nutritional Therapy Careful regulation of protein intake, fluid intake to balance fluid losses, sodium intake to balance sodium losses, and some restriction of potassium. Adequate caloric intake and vitamin supplementation The allowed protein must be of high biologic value (dairy products, eggs, meats). Calories are supplied by carbohydrates and fat to prevent wasting Vitamin supplementation (for protein restriction and dialysis patients) Nursing Diagnosis – – – – – – Excess fluid volume related to decreased urine output, dietary excesses, and retention of sodium and water Imbalanced nutrition: less than body requirements related to anorexia, nausea, vomiting, dietary restrictions, and altered oral mucous membranes Deficient knowledge regarding the condition and treatment Activity intolerance related to fatigue, anemia, retention of waste products, and dialysis procedure Risk for situational low self-esteem related to dependency, role changes, change in body image, and change in sexual function Hyperkalemia; pericarditis, pericardial effusion, and pericardial tamponade; hypertension; anemia; bone disease and metastatic calcifications (collaborative nursing diagnosis) Nursing intervention – Nursing care is directed toward: – assessing fluid status and identifying potential sources of imbalance, implementing a dietary program to ensure proper nutritional intake within the limits of the treatment regimen, promoting positive feelings by encouraging increased selfcare and greater independence. emotional support for the patient and family Provide explanations and information concerning: ESRD, treatment options potential complications – Assess fluid status: Daily weight Intake and output balance Skin turgor and edema Distention of neck veins Bp, pulse rate, and rhythm Respiratory rate and effort – – Limit fluid intake Identify potential sources of fluid: – – – Medications and fluids: oral and intravenous Foods Explain to patient and family rationale for fluid/food restriction. Assist patient to cope with the discomforts resulting from fluid restriction. Provide or encourage frequent oral hygiene – – – – Encourage high-calorie, low-protein, low-sodium, and low potassium snacks between meals. Provide written lists of foods allowed. Provide pleasant surroundings at meal-times. Assess for evidence of inadequate protein intake: Edema formation Delayed wound healing Decreased serum albumin levels Complications – Potential complications of chronic renal failure: Hyperkalemia Pericarditis, pericardial effusion, pericardial tamponade Hypertension Anemia Bone disease Nursing intervention – Pericarditis, Pericardial Effusion, and Pericardial Tamponade Assess patient for fever, chest pain, pericardial friction rub (if present), notify physician. If patient has pericarditis, assess for the following every 4 hrs: Paradoxical pulse 10 mm Hg Extreme hypotension Weak or absent peripheral pulses Altered level of consciousness Bulging neck veins Prepare patient for cardiac ultrasound. Prepare patient for emergency pericardiocentesis Nursing intervention …cont’ed – Hypertension Monitor and record blood pressure as indicated. Administer antihypertensive medications as prescribed. Encourage compliance with dietary and fluid restriction therapy. Teach patient to report signs of fluid overload, vision changes, headaches, edema, or seizures. Hyperkalemia Monitor serum potassium levels; Notify physician if greater than 5.5 mEq/L, and prepare to treat hyperkalemia. Assess patient for muscle weakness, diarrhea, ECG changes Nursing intervention …cont’ed – Anemia Monitor RBC count, Hgb, and hematocrit levels. Administer medications as prescribed, including: Iron Folic acid supplements, Epogen, Multivitamins Avoid drawing unnecessary blood specimens. Teach patient to prevent bleeding Administer blood component therapy as indicated. Nursing intervention …cont’ed – Bone Disease and Metastatic Calcifications Administer: phosphate binders, calcium supplements, vitamin D supplements as prescribed. Monitor serum lab values as indicated (calcium, phosphorus, aluminum levels) and report abnormal findings to physician. Assist patient with an exercise program References 1. 2. 3. Brunner & Suddarth’s Textbook of Medical-Surgical Nursing, 14th edition Focus on Adult Health_ Medical-Surgical Nursing-2nd edition Lewiss Medical-Surgical Nursing Assessment and Management of Clinical Problems-11th EDITION