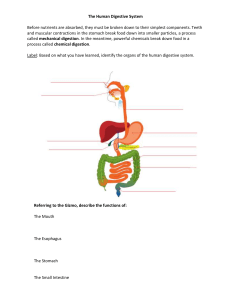
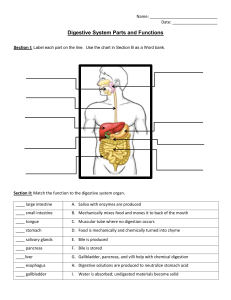
Omental bursa – a long, double fold of mesentery that extends inferiorly from the stomach before looping back to the transverse colon to create a cavity/pocket Mesentery proper – attaches the small intestine to the posterior abdominal wall DIGESTIVE SYSTEM With the help of the circulatory system, is like a gigantic ‘meals on wheels’, serving 100 T customers the nutrients they need Has its own quality control and waste disposal methods Retroperitoneal – abdominal organs that have no mesenteries; duodenum, pancreas, ascending + descending colon, rectum, kidneys, adrenal glands, urinary bladder FUNCTIONS (IDEA) 1. Ingestion of food. 2. Digestion of food. 3. Elimination of wastes. 4. Absorption of nutrients. ANATOMY AND HISTOLOGY Digestive Tract / Gastrointestinal Tract Oral cavity, pharynx, esophagus, stomach, small intestine, large intestine, anus Four Tunics 1. Mucosa Innermost tunic Consists of mucous epithelium, lamina propria (loose CT), muscularis mucosae (thins SM layer) Mouth, esophagus, anus; resists abrasion Stomach, intestine; absorbs and secrets 2. 3. 4. Submucosa Thick layer of loose CT, consists of nerves, blood vessels, small glands Plexus – extensive network of nerve cell processes (innervated by the autonomic nerves) Muscularis Consists of circular SM (inner), longitudinal SM (outer) Enteric nervous system – composed of the nerve plexuses of the submucosa and muscularis; controls movement and secretion within the tract Serosa Outermost layer Consists of the peritoneum (smooth epithelial layer + underlying CT) Adventitia – connective tissue; regions of the DT not covered by the peritoneum Peritoneum 1. Visceral Peritoneum / Serosa membrane that covers the organs 2. – serous Parietal Peritoneum – serous membrance that covers the wall of the abdominal cavity Mesenteries – CT sheets that hold the abdominal cavity organs in place a. Lesser omentum – connects the lesser curvature of the stomack to the liver and diaphragm b. Greater omentum – connects the greater curvature of the stomach to the transverse colon and posterior body wall ORAL CAVITY, PHARYNX, AND ESOPHAGUS Anatomy of Oral Cavity Bounded by the lips and cheeks ++ contains the teeth and tongue Lips – muscular structures formed by the orbicularis oris muscle Cheeks – buccinators muscles flatten the cheeks against teeth Mastification – begins the process of mechanical digestion Tongue – plays a major role in the process of swallowing; major sensory organ for taste; one of the major organs of speech Frenulum – thin fold of tissue inferior to the tongue Teeth 1. 2. 3. 4. 5. 32 teeth in normal adult mouth Located in the mandible and maxillae Incisor – to cut Canine – to tear Premolars Molars Wisdom teeth – third molars Permanent teeth – secondary teeth Primary teeth – deciduous teeth; milk or baby teeth Parts a. b. c. d. Crown Cusps Neck Root Pulp cavity – center of the tooth; contains blood vessels nerves, and pulp (connective tissue) Dentin – bonelike tissue that surrounds the pulp cavity Enamel – extremely hard, acellular substance that covers the dentin of the tooth drown Cementum – covers the surface of the dentin in the root; anchors the tooth in the jaw Alveoli (along the alveolar process of mandible x maxillae) – where the teeth are rooted Gingiva – dense fibrous CT and most stratified squamous epithelium that covers the alveolar processes Periodontal ligaments – CT fibers that extend from the alveolar walls that hold the teeth in place Dental caries / Tooth decay – result of the breakdown of enamel by acids produced by bacteria on tooth surface Periodontal disease – inflammation x degeneration of the periodontal ligaments, gingiva, alveolar bone Palate and Tonsils Palate – roof of the oral cavity; prevents food from passing into the nasal cavity during chewing and swallowing a. Hard palate – anterior part that contains bone b. Soft palate – posterior portion that consists of skeletal muscle _ CT Uvula – grape-like; posterior extension of the soft palate Tonsils – protect against pathogens from entering the nose and mouth Salivary Glands Produce saliva (serous + mucous fluids) 3 Pairs of SG 1. Parotid glands – largest; serous glands located anterior to each ear 2. Submandibular glands – produce more serous than mucous secretions 3. Sublingual glands – smallest; produce primarily mucous secretions Esophagus Muscular tube that ransports food from the pharynx to the stomach Esophageal sphincters – regulate the movement of food into and out of the esophagus Cardiac sphincter – lower ES Swallowing / Deglutition 1. Voluntary Phase Bolus (mass of food) us formed in the mouth Bolus is pushed by the tongue forcing in into the oropharynx 2. 3. Pharyngeal Phase A reflex initiated when a bolus of food stimulates receptors in the oropharynx Epiglottis – tipped posteriorly to cover the larynx Esophageal Phase Responsible for moving food form the pharynx to the stomach Peristaltic waves – muscular contractions of the esophagus STOMACH Functions primarily as a storage and mixing chamber for ingested food Anatomy Gastroesophageal opening esophagus ino the stomach – opening Cardiac region – region of t gastroesophageal opening; near the heart from the around the Fundus – most superior part of the stomach Mumps – inflammation of the parotid gland caused by viral infection Body – largest part of the stomach Greater curvature Lesser curvature Saliva Helps keep the oral cavity moist Contains enzymes that begin the process of digestion Pyloric opening – opening from the stomach into the small intestine Salivary amylase – a digestive enzyme that breaks the covalent bonds bet. glucose molecules (starch) and other polysaccharides; enhances the sweet taste of food Lysozyme – enzyme that has weak antibacterial action Mastification Breaks large food particles into many small ones Increases the efficiency of digestion Pharynx Throat Connects the mouth with the esophagus Oropharynx + laryngopharynx – transmit food Contains pharyngeal constrictor muscles Pyloric sphincter – thick ring of smooth muscle Pyloric region – region near the pyloric opening Outer longitudinal, middle circular, and inner obique layer – produce a churning action in the stomach Rugae – large folds where the submucosa and mucosa are thrown into when the stomach is empty Gastric pits – openings for the gastric glands; formed by simple columnar epithelium Epithelial cells of the Stomach 1. Surface mucous cells – inner surface of stomach & lining the gastric pits; coats and protects the stomach lining 2. Mucous neck cells – produce mucus 3. 4. 5. Parietal cells – produce hydrochloric acid & intrinsic factor Endocrine cells – produce regulatory chemicals Chief cells – produce pepsinogen (precursor of the protein digesting enzyme pepsin) Secretions of the Stomach Chyme – semifluid mixture (food + stomach secretions) 1. 2. 3. 4. Hydrochloric acid kills microorganisms and activates pepsin Pepsin breaks covalent bond of proteins to form smaller peptide chains. Mucus lubricates and protects epithelial cells from the damaging effect of acidic chime + pepsin Intrinsic factor binds with vit. B12 (DNA synthesis and RBC prod.) and makes it more readily absorbed in the small intestine Regulation of Stomach Secretions 1. Cephalic phase – stomach secretions are initiated by the sight, smell, taste, or thought of food 2. Gastric phase – partially digested proteins and distention of the stomach promote secretion Gastrin – hormone that enters the circulation and is carried back to the stomach 3. Intestinal phase – acidic chime in the duodenum stimulates neuronal reflexes and the secretion of hormones that inhibit gastric secretions by negative feedback loops Secretin – hormone that inhibits gastric secretions; released from the duodenum in response to low pH Cholecystokinin – major inhibitor of gastric motility; released from the duodenum initiated by fatty acids and peptides Movement in the Stomach Increased motility = increases emptying Distention of stomach = increases gastric motility A. Mixing waves – thoroughly mix ingested food with stomach secretions to form chime Fluid part of chime – pushed toward the pyloric sphincter Solid center – moves back toward the body of the stomach B. Peristaltic waves – force the chime toward and through the pyloric sphincter SMALL INTESTINE Major site of digestion and absorption of food Major function is the absorption of nutrients Anatomy 1. Duodenum – 12 in. long 2. Jejunum – 2.5 m long; makes up 2/5 3. Ileum – 3.5 m long; makes up 3/5 Common bile duct (liver) and pancreatic (pancreas) – join and empty into the duodenum duct Increased surface area 1. Circular folds – formed by mucosa and submucosa that run perpendicular to the long axis of the digestive tract 2. Villi – formed by tiny, fingerlike projections of the mucosa 3. Microvilli – numerous cytoplasmic extensions on the surface of the villi Lacteal – lymphatic capillary Simple Columnar Epithelium 1. Absorptive cells – have microvilli, produce digestive enzymes, absorb digested food 2. Goblet cells – produce a protective mucus 3. Granular cells – help protect the intestinal epithelium from bacteria 4. Endocrine cells – produce regulatory hormones Intestinal glands – epithelial cells produced within tubular galnds of mucosa Duodenal glands – mucous glands in the submucosa of the duodenum Peyer patches – clusters of lymphatic nodules along the digestive tract Ileocecal junction – where the ileum connects to the large intestine Ileocecal sphincter – ring of smooth muscle Ileocecal valve – allow intestinal contents to move from the ileum to the large intestine; but not in opposite direction Secretions of the Small Intestine 1. Peptidases – break peptide bonds in proteins to form amino acids 2. Disaccharidases – break down disaccharides (maltose) into monosaccharides (glucose) Movement of the Small Intestine A. Peristaltic contractions – proceed along the length of the intestine for variable distances; causes the chime to move along the small intestine B. Segmental contractions – propagate for shot distances; mix intestinal contents LIVER AND PANCREAS Anatomy of Liver Major Lobes 1. Right lobe 2. Left lobe Falciform ligament – CT septum that separates the right and left lobe of the liver Smaller Lobes 1. Caudate lobe 2. Quadrate lobe Pancreatic islet / Islets of Langerhans – endocrine part; produce insulin and glucagon Porta – gate through which blood vessels, ducts, and nerves enter and exit the liver Sources of Blood in the Liver 1. Hepatic artery – takes oxygen-rich blood to the liver; supplies liver with oxygen 2. Hepatic portal vein – oxygen-poor blood but rich in nutrients Hepatic veins – where blood exits the liver and empty into the inferior vena cava Portal Triads 1. Hepatic artery 2. Hepatic portal vein 3. Hepatic duct Acini – produce digestive enymes Pancreatic duct – formed by larger ducts from clusters of acini Functions of the Pancreas Major Proteolytic enzymes – continue protein digestion that began in the stomach 4. Trypsin 5. Chymotrypsin 6. Carboxypeptidase Pancreatic amylase – continues polysaccharide digestion that began in the oral cavity Hepatic cords – located bet. the center and margins of each lobule Hepatocytes – platelike groups that form the hepatic cords Hepatic sinusoids – blood channels that separates the hepatic cords from one another Central vein – where mixed blood flows toward the center of each lobule Bile canaliculus – a cleftlike lumen bet. the cells of each hepatic cord Common hepatic duct – right + left hepatic ducts Common bile duct – common hepatic duct + cystic duct Gallbladder – stores and concentrates bile Duodenal papilla – where the common bile duct joind the pancreatic duct and opens into the duodenum Functions of the Liver 1. Digestion 2. Excretion 3. Nutrient storage 4. Nutrient conversion 5. Detoxification of harmful chemicals 6. Synthesis of new molecules Bile salts – emulsify fats that results Anatomy of Pancreas 1. Head – near the midline of the body 2. Tail – extends to the left Lipase – lipid-digesting enzyme Nucleases – enzymes that degrade DNA and RNA to their component nucleotides LARGE INTESTINE Anatomy Cecum Proximal end of the large intestine Appendix – 9 cm tube attached to the cecum Colon 5. 6. 7. 8. Ascending colon Transverse colon Descending colon Sigmoid colon Crypts – straight, tubular glands in the mucosal lining of the colon Teniae coli – three bands Rectum Straight, muscular tube that begins at the termination of sigmoid colon & ends at the anal canal Anal Canal Begins at the inferior end of the rectum and ends at the anus (external digestive tract opening) Bile – dilutes and neutralizes stomach acid; dramatically increases the efficiency of fat digestion and absorption; stimulated by secretin Bilirubin – bile pigment breakdown of hemoglobin Compound acinar gland – exocrine part from the Internal anal sphincter – smooth muscle layer at superior end External anal sphincter – skeletal muscle at inferior end Hemorrhoids – enlarged or inflamed rectal or hemorrhoidal, veins that supply the anal canal; may cause pain, itching, bleeding around anus Functions of Large Intestine 3. Feces production 4. Water absorption Feces – converted chyme Lipase – secreted by pancreas; digests lipid molecules Defecation – elimination of feces from the colon Micelles – aggregated bile salts around small droplets of digested lipids Mass movements – strong contractions in the large parts of the colon; propel the colon contents a considerable distance towards the anys Defecation reflex – local (weak contractions) parasympathetic (strong contractions) reflexes + DIGESTION, ABSORPTION, AND TRANSPORT Digestion – breakdown of food to molecules tha are small enough to be absorbed into the circulation a. Mechanical digestion – breaks large good particles into smaller ones b. Chemical digestion – breaking of covalent chemical bonds in organic molecules by digestive enzymes Absorption – begin in stomach; lipid-soluble molecules diffuse through the stomach epithelium into the circulation Transport – requires carrier molecules and includes facilitated diffusion, cotransport, and active transport Carbohydrates Consist primarily of starches, cellulose, sucrose (table sugar), small amounts of fructose (fruit sugar), and lactose (milk sugar) Polysaccharides – large carbohydrates that consist of many sugars linked by chemical bonds Salivary amylase – begins carbohydrates in the mouth Pancreatic amylase carbohydrates Disaccharides polysaccharide – – two the digestion of continues digestion of sugars; broken down Disaccharidase – group of enzymes that break the disaccharides to monosaccharides Monosaccharides – single sugars; glucose, galactose, and fructose Lipids Molecules which are insoluble or slightly soluble in water Triglycerides – most common type of lipid; 3 fatty acids bound to glycerol Saturated – fatty acids have only single bonds Unsaturated – fatty acids have one or more double bonds Emulsification – large lipid droplets are transformed into much smaller droplets Chylomicrons (lipoproteins) – packaged lipid-protein complexes Chyle – lymph containing late amounts of absorbed lipid Proteins Chains of amino acids Pepsin – enzyme secreted by stomach that breaks down proteins Polypeptides – shorter amino acid chains Trypsin, Chymotrypsin, Carboxypeptidase – enzymes produced by pancreas that continue the digestive process Peptidases – small peptides Water and Minerals Approximately 9 L of water enters the digestive tract Approximately 2 L from food & drink & remaining 7 liters is from digestive secretions