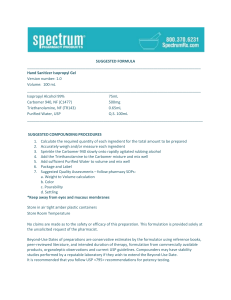
ASK ASKTHE THEEXPERT EXPERT By TK TK With Patricia C. Kienle RPh, MPA, BCSCP, FASHP Director of Accreditation and Medication Safety Cardinal Health Identify Gaps in USP <800> Compliance In addition, the qualitative method can be used to monitor HD residue from commonly used products on nursing units, patient care units, ambulatory infusion centers, etc. In short, both systems offer pharmacy significant utility for monitoring HD residue. Pharmacy Purchasing & Products recently held a webinar entitled: Identify Gaps to Achieving USP <800> Compliance presented by Patricia C. Kienle, RPh, MPA, BCSCP, FASHP A SERIES OF 20-MINUTE WEBINARS The following questions were submitted by attendees. The webinar slides and full presentation can be downloaded at pppmag.com/webinars. Q Do you have recommendations for non-pharmacy staff who are responsible for preparing their facility’s hazardous injectables? A: It is not uncommon in small facilities, particularly Q Should soiled gloves and wipes used in hazardous drug receiving be wasted in the trace chemotherapy waste bin or a black RCRA bin? A: At a minimum, anything that has had contact with hazardous drugs (HDs) should be treated as contaminated and disposed of as trace waste. If any products or PPE are used to address an HD spill, they should be disposed of as RCRA waste. There are three reference points to determine what additional waste should be classified as RCRA waste. First, check with your organization’s waste hauler for guidance. Secondly, review your state regulations as these may be more stringent or more detailed than the federal regulations. Finally, look to the pharmacy literature on this topic. Charlotte Smith has published several informative articles outlining how to manage HD disposal by matching the type and quantity of waste to the correct waste stream (see Charlotte Smith’s latest article on page 6 in this issue, “Demystify New Regulations for Hazardous Waste”). Q Now that NIOSH has removed biologics from the draft List of Antineoplastic and Other Hazardous Drugs, how can pharmacy ensure that their organization’s HD list is complete and accurate? A: The possibility for biologics to fall through the cracks since being removed from the NIOSH list is quite concerning. I understand why NIOSH took this approach, as there is more rigorous direction in the literature for the safe handling of drugs versus the safe handling of biologics. However, there is now a risk that as new agents enter the market, most of which are biologics, the companies may not 2 ■ May 2021 ■ pppmag.com include manufacturer’s safe-handling guidance in the package insert (PI) as that would automatically place that drug into Table 1. There have been requests for other organizations, such as ASHP, to establish and maintain a list of hazardous biologics. In the interim, pharmacists are going to have to take a rigorous approach to identify risks associated with biologics and then share this information through the pharmacy literature. This is a great opportunity for residency projects or for facilities that have sufficient resources to research biologics and then provide that information to the pharmacy community. Q Regarding wipe sampling, what are the benefits of the quick qualitative test versus the quantitative test? A: I like both the quantitative and the quick qualitative wipe sampling tests for different reasons. The quantitative wipe sampling approach has been around for a number of years: wipe the designated surface, send that sample to the vendor’s lab, and receive the results on a panel of drugs within a week or so. Some vendors in this area allow you to test specifically for the HDs that are most prevalent in your practice, which I think is a great option. The results from these sampling kits provide a quantitative picture of the exposure risk in your facility based on a wide variety of HDs. The quick, qualitative test method for wipe sampling has become available more recently. This approach offers testing for three drugs and delivers the results in 30 minutes. Because this method provides targeted information, the qualitative method is an excellent resource for training, checking for correct technique, and evaluating spill response efforts. in offsite physician offices, for a non-pharmacist to prepare HDs. While the staff member preparing HDs does not have to be a pharmacist or pharmacy technician, they do need to follow all the same procedures a pharmacist or pharmacy technician would follow under USP <800>. Regardless of job title, the person mixing HDs must have the appropriate facilities and documented competency to do so. HD compounding must take place in a separate room that is under negative pressure, vents to the outside, and has the appropriate number of air changes per hour. In addition, compounding must take place in the appropriate containment primary engineering control (C-PEC), either a biological safety cabinet or compounding aseptic containment isolator. These requirements serve to evacuate the hazard and control the risk of exposure. It is important to note that rather than use the word pharmacy, USP <800> uses the term entity. Just as compounding activities are not limited by job title, compounding locations are not limited to the pharmacy only. An entity could be a remote hospital where nursing is doing all of the compounding, a physicians’ office, a clinic, etc. The key requirement is that all of the criteria in USP <800> be followed regardless of location as those rules exist for the protection of the compounder. Q Could you expand on the use of pass-throughs from uncontrolled areas into an ISO-7 cleanroom? A: Properly designed and well controlled pass- throughs can significantly improve the efficiency of a cleanroom operation. From a workflow design perspective, pass-throughs between a negativepressure room and an unclassified area allow for Don’t miss out on premium content pppmag.com/subscribe P HARMACY Purchasing&Products ASK THE EXPERT the movement of supplies and finished product without having to don full PPE and walk into a positive pressure area. However, the FDA November 2020 Guidance Document “Insanitary Conditions at Compounding Facilities” weighs in on the use of pass-throughs between negative pressure and unclassified areas and requires that pass-throughs in these locations are classified.1 Thus, it is important that this workflow improvement be properly designed and implemented with care. Q How can health care facilities ensure that the crushing of HD medications in both pharmacy and at the bedside is safe? A: The first step to prevent incorrect HD handling is to ensure that everyone in your organization who may encounter these products is familiar with the organization’s HD list as it applies to them. That information should not be a secret in your organization. When crushing HDs, every effort should be made to conduct this process in the pharmacy. It is best practice to do this in the controlled environment of the pharmacy, within a C-PEC, using the applicable tools, and ensuring the use of appropriate packaging and labeling. Nevertheless, this is not always possible. When it is necessary to crush an HD outside of the pharmacy, that staff person must recognize that this is a hazardous practice, and they must understand what protection is required. In USP <800>, the use of a plastic pouch is discussed as a minimum measure of protection. A few companies produce these plastic pouches which serve to contain any dust and particles that might be generated during the crushing process. However, additional controls are still needed to get the product out of the plastic pouch safely. Although it is not a requirement, I would suggest the use chemo gloves, and depending on the HD being crushed, respiratory protection should also be considered. WHERE TO FIND Q Could you talk about the design of the negative storage room for hazardous drugs and the process to follow for unpacking HDs? A: When designing a negative storage room, keep in mind that receiving, unpacking, and storing the drugs are three separate processes and must be addressed as such. The current wording in USP <800> presents these three processes in a single section, but they are distinct steps. It is important to note that rather than use the word pharmacy, USP <800> uses the term entity. Just as compounding activities are not limited by job title, compounding locations are not limited to the pharmacy only. When you receive a delivery, you should be able to tell from the outside of the container that it contains a hazardous drug. While there is no requirement for the outside labeling to denote that HDs are contained within, USP <800> does encourage that any containers with Table 1 antineoplastic HDs indicate this on the exterior of the container. This is something you should discuss with your supplier. Next, you need to establish a receiving area to review incoming shipments. This area does not need to be under negative pressure, so you can use your regular receiving area. Note that the receiving area cannot be positive pressure, so neither the anteroom nor regular buffer room can serve this purpose. Wipe Sampling Kits For a full list of vendors offering wipe sampling go to: .com Key Wipe Sampling Suppliers .com American Analytics, Inc Bio-Med QC LLC ChemoGLO, LLC pppmag.com/findit/vendor/1464 pppmag.com/findit/vendor/974 pppmag.com/findit/vendor/1147 2finditnow.com 4 ■ BD Bureau Veritas Laboratories Cleanroom Connection pppmag.com/findit/vendor/307 pppmag.com/findit/vendor/1496 pppmag.com/findit/vendor/1308 May 2021 ■ pppmag.com Then, identify your storage site. Certain drugs must be stored in a negative-pressure room, such as Table 1 antineoplastics, any active pharmaceutical ingredients (raw powder), and anything else determined in your assessment of risk that must be handled under USP <800>. These drugs can be stored in a separate negative-pressure storage room. If that is not an option, consider using your negative-pressure buffer room as the storage site if space permits. .com The process for transporting the HDs from the unpacking area into the storage area will be dictated largely by your facility’s design. Ideally, the plastic-bagged HDs would be removed from the wholesaler’s tote without opening the plastic bags, and the outside of the plastic bag would be thoroughly wiped to remove any potential contamination. If your facility has a pass-through into the storage area, place the bags in the pass-through for the staff in the storage area to complete the unpacking and storing process. If you do not have a pass-through, another option is to designate a cleanable plastic tote, and use that to move products in and out of the storage area. In short, you must determine where HDs will be received, unpacked, and stored, based on your facility’s design. Then, put the appropriate policies and procedures in place to ensure safety. n References 1. United States Department of Health and Human Services, Food and Drug Administration Center for Drug Evaluation and Research, Office of Compliance. Compounding and Related Documents, Insanitary Conditions at Compounding Facilities Guidance for Industry, Guidance for Industry. https://www.fda.gov/media/124948/download. Accessed March 16, 2021. Patricia C. Kienle, RPh, MPA, BCSCP, FASHP, is director of accreditation and medication safety for Cardinal Health and is a member of the USP Compounding Expert Committee. Her comments herein are her own and not official information from USP. .com content Don’t miss out on premium pppmag.com/subscribe P HARMACY Purchasing&Products