Uploaded by
sivaneasan.nadarajah
Immunity: Immune Response, Antibodies, and Lymphocytes
advertisement
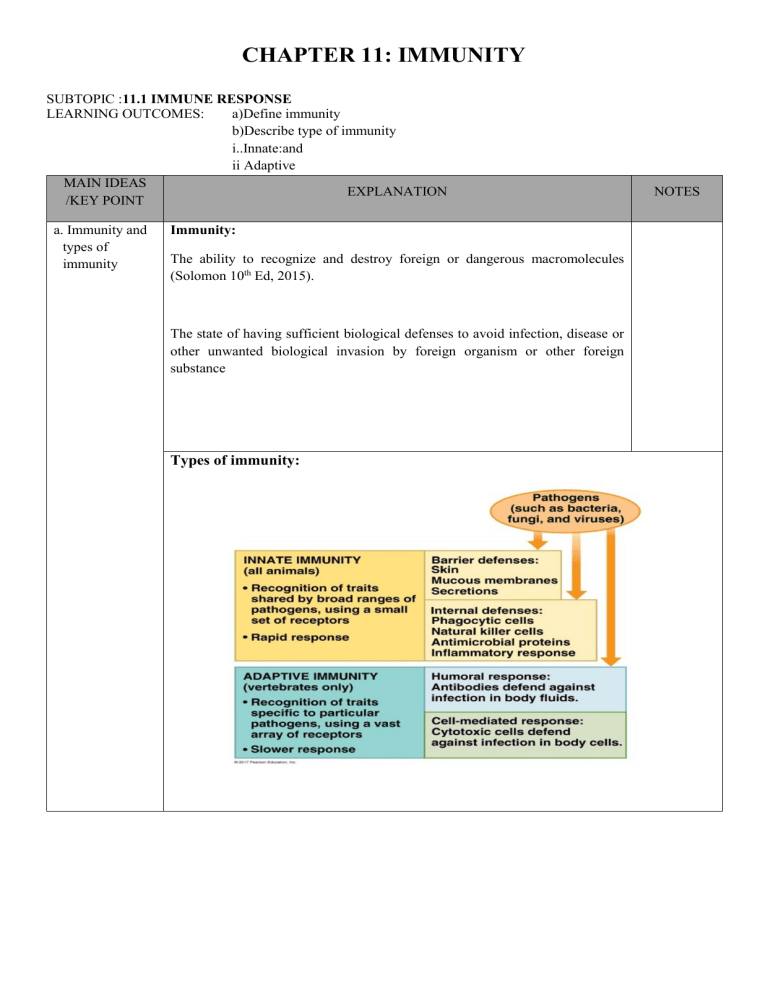
CHAPTER 11: IMMUNITY SUBTOPIC :11.1 IMMUNE RESPONSE LEARNING OUTCOMES: a)Define immunity b)Describe type of immunity i..Innate:and ii Adaptive MAIN IDEAS EXPLANATION /KEY POINT a. Immunity and types of immunity Immunity: The ability to recognize and destroy foreign or dangerous macromolecules (Solomon 10th Ed, 2015). The state of having sufficient biological defenses to avoid infection, disease or other unwanted biological invasion by foreign organism or other foreign substance Types of immunity: NOTES MAIN IDEAS /KEY POINT EXPLANATION NOTES SUBTOPIC :11.2 ANTIBODY LEARNING OUTCOMES: a) Describe the general structure of antibody b) State the classes of antibody based on its structure MAIN IDEAS /KEY POINT General structure of antibodies and classes based on its structure. EXPLANATION Antibody: A specific protein (immunoglobulin) that recognizes and binds to specific antigen which produced by plasma cells. Structure of antibodies: Basic shape of antibody • • • • • • Y shaped 4 polypeptide chains: 2 identical light chains 2 identical heavy chains Linked by disulphide bridge Each chain contains: variable region (V) constant region (C) The constant region of heavy chains: form the base of antibody molecules determines the way antibody is secreted & how it is distributed in body fluid ✓ Eg: circulate in body fluid or bind to membranes of mast cells (mast cells are cells found in connective tissue that store histamine, inflammatory signaling molecule) The variable region of the light and heavy chain: determine the specificity of an antibody molecules amino acid sequence varies extensively from one B cell to another. part of heavy-chain V region and a light-chain V region form as asymmetric binding site for an antigen. • Each antibody has 2 antigen-binding sites Form by the free tips end of both variable region Classes of antibody: i. IgD • Found in blood and lymph and on surfaces of B cells • Single monomer • Function: act as antigen receptors on the surfaces of B cells Stimulating the differentiation of B cells into plasma cells and memory cells ii. IgE • Bind to mast cells and basophil and stimulate them to produce histamines • Single monomer • Function: responsible for allergic reaction but useful against parasitic worms iii. • • • • IgG Temporary protection to newborn. single monomer Easily cross the walls of blood vessel and enter tissue fluid e.g.: maternal IgG antibodies can cross the placenta and confer passive immunity to fetus iv. IgM • Primary antibody response. • Pentamer: Large size 5 monomers held together by polypeptide called J (joining) chain • First antibodies to appear in response to initial exposure to an antigen v. IgA • Common in mucous membranes and in body secretions: mucus, saliva, tears, breast milk • Most abundant in body (IgG most abundant in serum) • Dimer: 2 monomers held by J chain • Functions: prevent the attachment of pathogens to mucosal surfaces SUBTOPIC :11.3 LYMPHOCYTE DEVELOPMENT LEARNING OUTCOMES: a) Describe B cell and T cell MAIN IDEAS /KEY POINT EXPLANATION Lymphocytes originate from stem cell in the bone marrow. Early lymphocytes are all a like. Later they develop into T and B lymphocytes/cell – depending on where they continue their maturation. Lymphocytes that migrate from the bone marrow to thymus develop into T cells Lymphocytes that remain in the bone marrow and continue their maturation there become B cells i. Lymphocytes Account for 20 – 30 % of circulating leukocytes (a) B cells Make up 10-15% of circulating lymphocytes,B cell can be further divided into: • Plasma cells when stimulated, B cells can differentiate into plasma cells which produce and secrete antibodies • Memory B cells Subset of B cells that respond to a previously encountered antigen (b) T cells Approximately 80% of circulating lymphocytes are classified as T cells • Cytotoxic T cells Attack foreign cells or body cells infected by viruses. • Helper T cells Stimulate the activation and function of both T cells and B cells. • Suppressor T cells Inhibit the activation and function of both T and B cells. • Memory T cells Subset of T cells that respond to a previously encountered antigen NOTES SUBTOPIC :11.4 DEVELOPMENT OF ADAPTIVE IMMUNITY LEARNING OUTCOMES: a) Explain cell mediated immune response b) Explain Hummoral (Antibody mediated) Immune response. c) Explain various type of antigen and antibody interactions: i. neutralization ii. opsonization iii. activation of complement system and pore formation. d) Explain the primary and secondary immune responses. MAIN IDEAS /KEY POINT Two types of immune response. EXPLANATION Types of immune response: i. Cell mediated immune response The branch of adaptive immunity that involves the activation of cytotoxic T cells, which defend against infected cells. ii. Humoral (Antibody mediated) immune response The branch of adaptive immunity that involves the activation of B cells and that leads to the production of antibodies, which defend against bacteria and viruses in body fluids. Components of humoral and cell mediated immune response: ii. Lymphocytes Account for 20 – 30 % of circulating leukocytes. B cells and T cells are the major lymphocytes involved in both immune response. iii. Major histocompatibility complex (MHC) molecule A host protein that functions in antigen presentation. • Glycoprotein and antigen that appears in plasma membrane is capable to activate T cells. • Membrane glycoproteins are called MHC proteins/human leukocyte antigens (HLAs). • Amino acid sequences and shapes of MHC proteins differs among individuals. • For T cell to recognize an antigen, the antigen must be bound to glycoproteins in the plasma membranes of another cell. NOTES MAIN IDEAS /KEY POINT EXPLANATION (a) MHC class I molecule • Present in plasma membrane of all nucleated cell • Pick up small peptides from the surrounding cytoplasm and carry them to the cell surface • If the cytoplasm contains abnormal peptides or viral proteins, they soon appear in the plasma membrane • T cells will recognize them as foreign and be activated (b) MHC class II molecule • Present only in the plasma membranes of antigen presenting cell (APC) and lymphocytes • APCs are specialized cells responsible for activating T cell defenses against foreign cells (including bacteria) and foreign proteins iv. Cytokines Signaling proteins that regulate interaction between cells in the immune system (a) Interleukin I (IL-1) • Primary source: macrophages • Activates helper T cells (b) Interleukin 2 (IL-2) • Source: Helper T cells. • Activates B cells and cytotoxic T cells Helper T (TH) cells stimulate the humoral and cell-mediated immune response 1. The macrophage ingest a microbe or other foreign particle and breaks it into fragments (foreign antigens) 2. MHC class II (self protein) bind to foreign antigens 3. Display them on the cell surface NOTES MAIN IDEAS /KEY POINT EXPLANATION 4. Helper T cell recognize and bind to the MHC-antigen complex caused APC release IL-1; and diffuse to the TH cell and stimulate it. 5. Activated TH cell release IL-2. IL-2 makes TH cell itself grow and divide producing memory cells and additional active TH cells. 6. IL-2 activate B cells and stimulating the humoral immune response 7. IL-2 activate TC cells stimulating the cell mediated immune response NOTES MAIN IDEAS /KEY POINT EXPLANATION NOTES Cell Mediated Immune Response a)Cell mediated immune response i. Pathogens bearing foreign antigens invade body ii. Antigen presenting cell @ APC (dendritic cell / macrophage) phagocytizes pathogen iii. Foreign antigen binds to the class II MHC protein form MHC- antigen complex and displayed on surface of APC iv. TH cell with its antigen receptor and accessory protein, CD4 binds with APC v. APC releases interleukin 1 (IL-1) to activate TH cell vi. Activated TH cell release IL-2 vii. TH cell proliferate producing activated TH cells and memory TH cells viii. Activated helper T cell will release IL-2 and the cytotoxic T (TC) cell ix. TC cell also becomes active when encounters an appropriate antigens bound to class I MHC molecule of infected cell. x. Activated TC undergoes mitotic division producing active TC cells (effector cells) and memory TC cells. xi. Activated TC cell migrates to the area of infection and eliminate cells that are infected by viruses or other intracellular pathogen. MAIN IDEAS /KEY POINT EXPLANATION xii. Fragments of foreign proteins inside of the cell bind with class I MHC molecules and then displayed on the cell surface. The MHC-antigen complex is recognized by TC cells. xiii. TC cells with accessory protein CD8 binds to the MHC molecule, helping keep the two cells in contact. xiv. TC cell may: release perforin to destroy the target cell’s plasma membrane and form pores. Secrete a poisonous lymphotoxin, granzymes to kill the target cell. It activates genes in the target cell’s nucleus that program the cell to die (apoptosis). Humoral immune response b)Humoral (Antiody mediated)im mune response i. Antigen presenting cell @ APC (dendritic cell / macrophage / B cell) phagocytizes pathogen and degrades it. ii. Fragment of foreign antigen binds to the class II MHC protein forming MHC-antigen complex and displayed on the surface of APC iii. TH cell with its antigen receptor and accessory protein, CD4 binds to the complex of APC iv. APC releases interleukin 1 (IL-1) to activate TH cell NOTES MAIN IDEAS /KEY POINT EXPLANATION v. Activated TH cell releases IL-2 vi. TH cell proliferates producing activated TH cells and memory TH cells vii. Once antigens are bound to B cell receptor (antibody) in the B cell membrane, the B cell displays those antigens that bound to class II MHC molecule on the surface of its plasma membrane viii. Activated TH bind to the sensitized B cell. ix. Activated TH cell will release IL-2 that co-stimulate the sensitized B cell and trigger its activation. x. The activated B cell then proliferates or divides mitotically, producing memory B cells and plasma cells (effector cells). xi. Plasma cells secretes antibodies. xii. Antibody-antigen interaction occurs. xiii. Triggers processes leading to pathogen destruction xiv. Memory B cells are long-lived cells that can give rise to effector cells if the same antigen is encountered later in life NOTES MAIN IDEAS /KEY POINT c) Various types of antigen and antibody interactions: EXPLANATION NOTES Antigen: • Any foreign molecule that elicits an immune response by binding to receptors of B cells or T cells. • Usually protein, glycoprotein or polysaccharide • Epitope/antigenic determinant sites: a small, accessible region of an antigen to which an antigen receptor or antibody binds • An antigen may have several different epitopes • Each epitope is recognized by a different antibody • Different antibodies can recognize distinct epitopes on the same antigen MAIN IDEAS /KEY POINT EXPLANATION NOTES Antigen and antibody interactions: • An antigen-antibody complex forms when an antibody molecule binds to its corresponding antigen molecule • Once the two molecules are in position, hydrogen bonding and other weak chemical forces lock them together • Antigen covered with antibodies attract eosinophils, neutrophils and macrophages • These cells then phagocytize the pathogens i. Neutralization • A process in which antibodies bind to proteins on the surface of a virus. • Viruses and bacterial toxins have specific sites that must bind to target regions on body cells before they can enter or injure those cells. • Antibodies bind to those sites, making the virus or toxin incapable of attaching itself to cell. • Thus, neutralizing the virus/toxins. ii. Opsonization • A process by which a particulate antigen becomes more susceptible to phagocytosis by macrophages and neutrophils. • A coating of antibodies and complement proteins increase the effectiveness of phagocytosis. • Some bacteria have slick plasma membranes or capsules, but opsonization makes it easier for phagocytes to hang on onto their prey before they engulf it. MAIN IDEAS /KEY POINT EXPLANATION • NOTES Phagocytes can bind more easily to antibodies and complement proteins than they can to the bare surface of a pathogen. iii. Activation of complement system and pore formation • When an antibody molecule binds to an antigen, it forms antigen-antibody complex. • Portion of the antibody change shape exposing areas that bind complement protein. • This binding activates the complement system. • The activated bound complement molecule then forms membrane attack complex. • Pores formed in plasma membrane, allowing water and ions to rush in. • The cell swells and lyses, destroy the pathogen. MAIN IDEAS /KEY POINT d.Primary and secondary immune responses. EXPLANATION • • • • • • NOTES Results from exposure of B cell to an antigen Includes series of cell division, differentiation and antibody production. Before stimulation by an antigen, B cells are small lymphocyte. After activation, B cell undergoes a series of divisions to produce large lymphocyte. Some enlarge cells become plasma cells to produce antibody. Others revert back to small lymphocytes become memory B cells. Primary immune response • Low concentration of antibodies produced at early stage and peak up one to two weeks after exposure (test on antibody titer). • Has lag time: slow reaction during 3- 6 days after the exposure. • B cells specific for that antigen multiply and develop into plasma cells • Takes 3-14 days to produce enough antibodies to be effective against antigen. • Meantime, individual usually develops disease symptoms because the antigen has had time to cause tissue damage. MAIN IDEAS /KEY POINT EXPLANATION • • • • • • NOTES Plasma cells secrete antibody. Antibody concentration rise and reach the peak in 10 -12 days. IgM is the first antibody produced and later other classes of antibodies are produced as well. Primary response lasts several days or weeks. Concentration of antibodies decrease because plasma cell dies. Memory B cell left in the body. Secondary immune response • • • • • • • The response of immune system to the second infection for same antigen Memory cell recognize the same antigen faster. Within hours after second exposure: memory B cells proliferate & differentiate rapidly into plasma cells to produce antibody. IgG mainly antibody produced. Within 2-3 days, antibody rises steeply, higher than in primary response and remain high for weeks to months. Plasma cells functioning for much longer than in primary response. Memory B cell able to recognize antigen for longer period; may persist for many years and probably for life or the immunity is long lasting. SUBTOPIC :11.5 IMMUNIZATION LEARNING OUTCOMES: a) Define Vaccine b) State the sources of antigen to make vaccine: i)Inactivated bacterial toxins: ii)Killed or weaken pathogens iii)Genes encoding microbial protein (DNA,RNA and protein) c)State the importance of vaccination MAIN IDEAS /KEY POINT a)What is vaccine EXPLANATION A commercially produced, weakened or killed antigen associated with a particular disease that stimulates the body to make antibodies. Solomon. E.P. Martin, C.E. Martin, D.W., Berg, L.R. (2015) Biology. Cencage Learning. Pg G-46 Inactivated Bacterial toxin Some bacteria causes disease by making a harmful protein called a toxin. The toxin is taken out and inactivated by using chemical . The inactivated toxin is called toxoid. By inactivating the toxin, it no longer causes diseases but triggers immune response to produce antibodies. Sources of antigen to make vaccine. Examples: Vaccines for Tetanus,Diphteria,Pertussis Killed or weaken pathogen Pathogens are microbes that causes diseases such as bacteria,viruses,fungi and parasites. By weakening a pathogen,the ability of the pathogen to reproduce is limited.Therefore,they does not cause diseases. A weakened virus vaccine reproduces 20 times lesser than a normal virus infection. NOTES However,it is able to reproduce minimaly to induce the production of memory B cells.This protects the body against the infection in the future. Examples:Vaccine for measless,mumps,rubella (MMR) and chickenpox The benefits of producing vaccine through weakened pathogens is, it provides lifelong protections. The limitation is, this type of vaccine cannot be given to people with weak immune system .For instance,people with AIDS or cancer.. By killing a pathogen, the pathogen (viruses) are being inactivated. Inactivated viruses cannot reproduce or cause diseases. However, the antigens on the viruses are still recognized by the immune system and triggers immune response by producing antibody. Examples;Vaccines for polio,Hepatitis A and rabies are produced using inactivated viruses. The advantages of this method is that vaccine cannot cause even a mild form of the disease that it prevents. Also, the vaccine can be given to people with weakened immune systems The limitation is it typically requires several doses to achieve immunity. Genes encoding microbial protein (DNA,RNA and protein) By injecting and individual with DNA vaccines or RNA vaccines, The DNA or RNA provides the information to make the viruses from inside the body. Vaccinated person use the information to make the spike protein from the surface of the virus. Immune system detects the protein as foreign substances and triggers the immune system. The RNA vaccine uses mRNA of the the viruses to trigger immune response. Example: Pfizer and Moderna COVID-19 vaccines are made this way. Vaccination is the most effective way to prevent diseases that is caused by pathogens as it : Importance of vaccination Prevents outbreak of a infectious diseases by forming a herd immunity when majority of the population is vaccinated. Protects the body from severe illness and reduce the mortality rate due to illness. Reduces economical and social impact of pandemic. SUBTOPIC :11.6 Health issue related to Immune response LEARNING OUTCOMES: a)Explain the immune suppression by HIV infection b)State autoimmune diseases: i. Systemic Lupus Erythematosus (SLE); ii. Multiple Sclerosis; and iii. Diabetes Type I MAIN IDEAS /KEY POINT EXPLANATION Immune suppression by HIV The human immunodeficiency virus (HIV) is the pathogen that causes AIDS. The pathogen attack humoral and cell mediated immune response. HIV infects helper T cells with high efficiency by binding specifically to CD4 accessory protein. HIV also infects cells with low level of CD4.Such as macrophages and brain cells. Inside the infected cell the HIV’s RNA genome is reverse- transcribed to produce DNA which is integrated to host cell’s genome. By doing this, the viral genome can direct the production of new viruses. Although body responds to HIV by immune system but some HIV may still escape. HIV has a very high mutation rate. Hence it persists inside body. Altered proteins on the surface of mutated viruses reduces interaction with antibodies and cytotoxic T cells. Therefore, the viruses replicates, mutates and evolves within the body. Over time, an untreated HIV infection not only avoids the adaptive immune response but also abolishes it Viral replication and cell death triggered by the virus lead to loss of helper T cells, impairing both humoral and cell-mediated immune responses. NOTES Autoimmune disease: A disease in which the body produces antibodies against its own cells or tissue. Also called autoimmunity. Solomon. E.P. Martin, C.E. Martin, D.W., Berg, L.R. (2015) Biology. Cencage Learning. Pg G-4 In autoimmune diseases, antibodies and T cells attack the body’s own tissue Systemic Lupus Erythematosus (SLE) In systemic lupus erythematosus (SLE) commonly called lupus, the immune system generates antibodies against histones and DNA released by the normal breakdown of body cells. Symptoms include: skin rashes fever arthritis kidney dysfunction Other symptoms depend on the part of the body being attacked by the disease. Multiple sclerosis Multiple sclerosis (MS) is a chronic disease affecting the central nervous system (the brain and spinal cord). It also known as rheumatoid arthritis. MS occurs when the immune system attacks nerve fibers and myelin sheathing in the brain and spinal cord. This attack causes inflammation, which destroys nerve cell processes and myelin – altering electrical messages in the brain. Diabetes Type I Diabetes Type 1 (T1D) results from the destruction of beta cells in the pancreas which produce insulin that are wrongfully targeted and killed off by specific antibodies created by the adaptive immune system. Therefore, it is known as insulin-dependent diabetes Symptoms include: excessive hunger excessive thirst blurred vision fatigue frequent urination dramatic weight loss in a short period of time It is caused by: Genetics Exposure to viruses and other environmental factors.