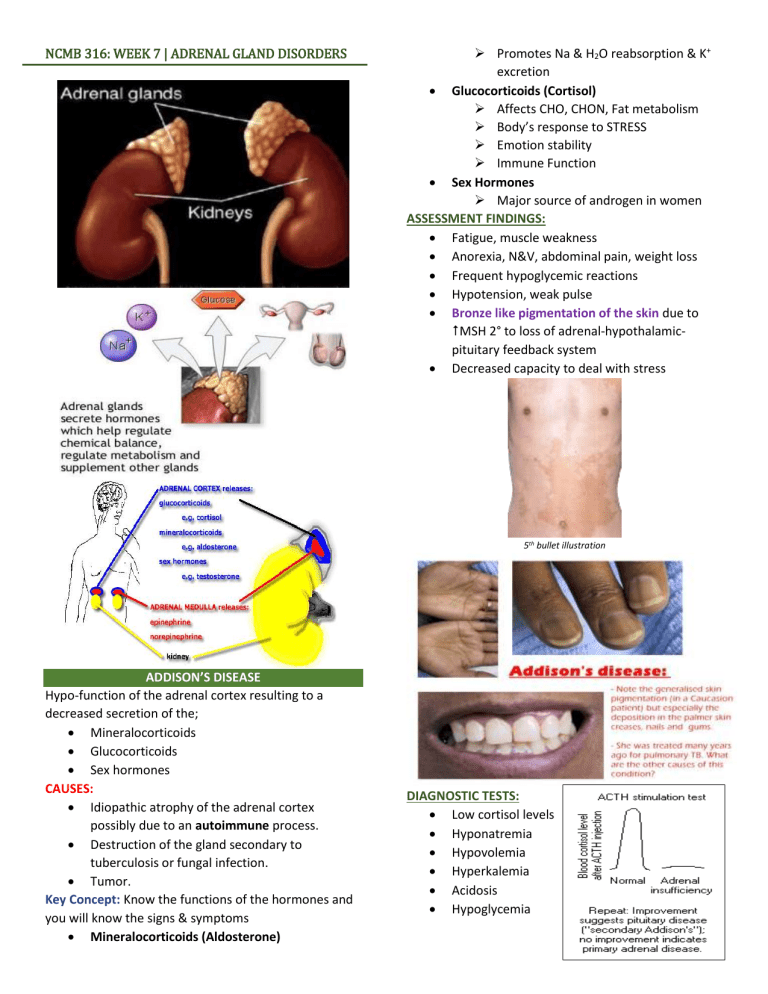
NCMB 316: WEEK 7 | ADRENAL GLAND DISORDERS Promotes Na & H2O reabsorption & K+ excretion Glucocorticoids (Cortisol) Affects CHO, CHON, Fat metabolism Body’s response to STRESS Emotion stability Immune Function Sex Hormones Major source of androgen in women ASSESSMENT FINDINGS: Fatigue, muscle weakness Anorexia, N&V, abdominal pain, weight loss Frequent hypoglycemic reactions Hypotension, weak pulse Bronze like pigmentation of the skin due to MSH 2° to loss of adrenal-hypothalamicpituitary feedback system Decreased capacity to deal with stress 5th bullet illustration ADDISON’S DISEASE Hypo-function of the adrenal cortex resulting to a decreased secretion of the; Mineralocorticoids Glucocorticoids Sex hormones CAUSES: Idiopathic atrophy of the adrenal cortex possibly due to an autoimmune process. Destruction of the gland secondary to tuberculosis or fungal infection. Tumor. Key Concept: Know the functions of the hormones and you will know the signs & symptoms Mineralocorticoids (Aldosterone) DIAGNOSTIC TESTS: Low cortisol levels Hyponatremia Hypovolemia Hyperkalemia Acidosis Hypoglycemia NURSING INTERVENTION: Administer HRT as ordered. Glucocorticoids (Cortisone, Hydrocortisone) - simulate diurnal rhythm of cortisol release, give 2/3 of dose in early morning and 1/3 of dose in afternoon Mineralocorticoids (Fludrocortisone acetate) Monitor VS Decrease stress in the environment Provide rest periods; prevent fatigue Prevent exposure to infection Monitor I&O, weigh daily Provide proper nutrition in small, frequent feedings of diet high in Sugar (carbohydrate), Salt (sodium) and Protein. Provide client teaching and D/C planning concerning: o Use of prescribed medications for lifelong replacement therapy; never omit medications o Need to avoid stress, trauma, and infections, and to notify physician if these occur as medication dosage may need to be adjusted o Stress management techniques o Diet modification o Use of salt tablets (if prescribed) or ingestion of salty foods (potato chips) if experiencing increased sweating o Importance of alternating regular exercise with rest periods, avoidance of strenuous exercise especially in hot weather. CUSHING’S SYNDROME Hyper-function of the adrenal cortex resulting to an excessive secretion of the; Mineralocorticoids Glucocorticoids Sex hormones CAUSES: Overproduction of ACTH Benign or malignant tumors Prolonged corticosteroids therapy Key Concept: Know the functions of the hormones and you will know the signs & symptoms Mineralocorticoids (Aldosterone) Promotes Na & H2O reabsorption & K+ excretion Glucocorticoids (Cortisol) Affects CHO, CHON, Fat metabolism Body’s response to STRESS Emotion stability Immune Function Sex Hormones Major source of androgen in women ASSESSMENT FINDINGS: Muscle weakness, fatigue Obese trunk with thin arms and legs, muscle wasting (pendulous abdomen) Irritability, depression, frequent mood swings Moon face, buffalo hump Purple striae on trunk, acne, thin skin Signs of masculinization in women; menstrual dysfunction, decreased libido Osteoporosis, decreased resistance to infection Hypertension, edema DIAGNOSTIC TEST: cortisol levels slight hypernatremia hypokalemia hyperglycemia NURSING INTERVENTION: Maintain muscle tone (Provide ROM exercises, Assist with ambulation) Prevent accidents or falls and provide adequate rest Protect client from exposure to infection Maintain skin integrity Provide meticulous skin care. Prevent tearing of skin: use paper tape if necessary. Minimize stress in the environment. Monitor VS: observe for hypertension, edema Measure I&O and daily weights Provide diet that is low in calories and sodium high in protein, K+, Ca++ vitamin supplements Monitor urine for glucose and acetone; administer insulin if ordered Provide psychological support and acceptance. Prepare client for hypophysectomy or radiation if condition is caused by a pituitary tumor Prepare client for an adrenalectomy if condition is caused by an adrenal tumor or hyperplasia Provide client teaching D/C planning concerning: Diet modifications Importance of adequate rest Need to avoid stress and infection Change in medication regimen (alternate day therapy or reduced dosage) if cause of the condition is prolonged corticosteroid therapy. PHEOCHROMOCYTOMA A condition of hyper-functioning tumor of the adrenal medulla resulting to excessive secretion of epinephrine & norepinephrine. Occurs most commonly between ages 25-50, hereditary in some cases. ASSESSMENT FINDINGS: Severe headache, apprehension, palpitations, profuse sweating, nausea Hypertension, tachycardia, vomiting, hyperglycemia, dilation of pupils, cold extremities. DIAGNOSTIC TESTS: Increased plasma levels of catecholamines Elevated blood sugar Glycosuria Elevated urinary catecholamines and urinary vanillylmandelic acid (VMA) levels Presence of tumor on x-ray. NURSING INTERVENTIONS: Monitor vital signs, especially blood pressure. Administer medications as ordered to control hypertension. Promote rest; decrease stressful stimuli. Monitor urine tests for glucose and acetone Provide high-calorie, well-balanced diet; avoid stimulants such as coffee, tea. Provide care for the client with an adrenalectomy as ordered; observe postadrenelectomy client carefully for shock due to drastic drop in catecholamine level. Provide client teaching and discharge planning: same as for adrenalectomy. ENDOCRINE PHARMACOLOGY Anti-diuretic hormones (ADH) Enhance re-absorption of H2O in the kidneys Used in Diabetes Insipidus (DI) Desmopressin and Lypressin intranasally. Pitressin IM. SIDE-EFFECTS: Flushing and headache Water intoxication. THYROID HORMONES Levothyroxine (Synthroid) and Liothyroxine (Cytomel). Used to replace hormonal deficit in HYPOTHYROIDSM. SIDE-EFFECTS: Nausea and Vomiting Signs of metabolism (tachycardia, hypertension, etc..) NURSING RESPONSIBILITY: Monitor weight, VS Instruct client to take daily medication the same time each morning WITHOUT FOOD Advise to report palpitation, tachycardia, and chest pain Instruct to avoid foods that inhibit thyroid secretions like cabbage, spinach and radishes. ANTI-THYROID MEDICATIONS Inhibit the synthesis of thyroid hormones Methimazole (Tapazole) PTU (Prophylthiouracil) Iodine solution (SSKI) and Lugol’s solution SIDE-EFFECTS: N/V Diarrhea AGRANULOCYTOSIS (WBC) Most important to monitor. NURSING RESPONSIBILITIES: Monitor VS, T3 and T4, weight Take medications WITH MEALS to avoid gastric upset Instruct to report SORE THROAT or unexplained FEVER Monitor for signs of hypothyroidism. Instruct not to stop medication abruptly. LUGOL’S SOLUTION Used to decrease the vascularity of the thyroid Diminishes T3 and T4 production Given per orem, can be diluted with juice, Use straw. STEROIDS Used to replace the steroids in the body if there is deficiency Cortisol, cortisone, betamethasone, and hydrocortisone SIDE-EFFECTS: Hyperglycemia Increased susceptibility to infection Hypokalemia Edema If high doses: osteoporosis, growth retardation, peptic ulcer, hypertension, cataract, mood changes, hirsutism, and fragile skin NURSING RESPONSIBILITIES: Monitor VS, electrolytes, glucose Monitor I&O, weight, edema Protect patient from infection Handle patient gently Instruct to take meds WITH MEALS to prevent gastric ulcer formation. Caution the patient NOT to abruptly stop the drug. Drug is tapered to allow the adrenal gland to secrete endogenous hormones. HYPOTHYROIDISM Hypo-secretion of thyroid hormones Common causes: Iodine deficiency, Hashimoto’s disease MANIFESTATIONS: Related to hypo-metabolic state: constipation weight gain cold intolerance poor appetite mental slowness NURSING MANAGEMENT: Provide warm environment LOW calorie diet HIGH fiber diet Avoid sedatives Medications: Hormone replacement. HYPERTHYROIDISM Hyper-secretion of thyroid hormones. COMMON CAUSE: Grave’s disease, Toxic goiter MANIFESTATIONS: Related to hyper-metabolic state: diarrhea weight loss heat intolerance hypertension NURSING MANAGEMENT: Adequate rest and sleep Cool environment HIGH calorie foods Eye care Drugs: anti-thyroid: PTU and methimazole, propranolol Care of patients after thyroidectomy.