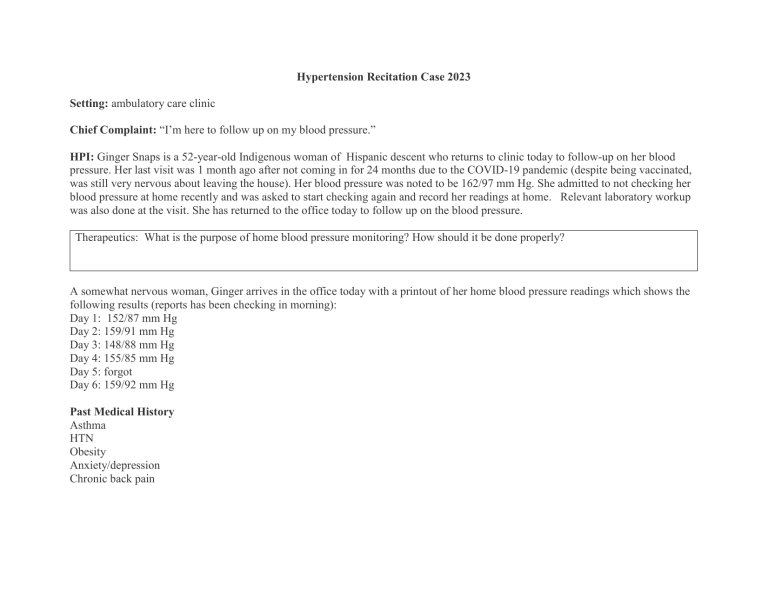
Hypertension Recitation Case 2023 Setting: ambulatory care clinic Chief Complaint: “I’m here to follow up on my blood pressure.” HPI: Ginger Snaps is a 52-year-old Indigenous woman of Hispanic descent who returns to clinic today to follow-up on her blood pressure. Her last visit was 1 month ago after not coming in for 24 months due to the COVID-19 pandemic (despite being vaccinated, was still very nervous about leaving the house). Her blood pressure was noted to be 162/97 mm Hg. She admitted to not checking her blood pressure at home recently and was asked to start checking again and record her readings at home. Relevant laboratory workup was also done at the visit. She has returned to the office today to follow up on the blood pressure. Therapeutics: What is the purpose of home blood pressure monitoring? How should it be done properly? A somewhat nervous woman, Ginger arrives in the office today with a printout of her home blood pressure readings which shows the following results (reports has been checking in morning): Day 1: 152/87 mm Hg Day 2: 159/91 mm Hg Day 3: 148/88 mm Hg Day 4: 155/85 mm Hg Day 5: forgot Day 6: 159/92 mm Hg Past Medical History Asthma HTN Obesity Anxiety/depression Chronic back pain Pathophysiology: What are the 2 factors that determine BP? What causes hypertension? Therapeutics: Could this patient be having white coat hypertension? Why/why not? What stage hypertension does this patient have? What are the implications for the treatment of her hypertension? Family History Father had a stroke at age 61; mother passed away due to complications related to diabetes. Sister (age 55) also has hypertension and diabetes. Social History Lives with husband Works for an insurance company – has been allowed to work from home since start of COVID Admits to not being as active since quarantine began and “munching” on food throughout the day (i.e. chips, pretzels). Has been ordering food more than cooking at home. When cooks, likes to make foods from her culture (empanadas, chicken fajitas, etc) Smokes ½ pack/day Alcohol consumption: 1-2 glasses of wine with dinner Caffeine consumption: 2-3 cups/day Therapeutics: Which lifestyle modifications should this patient implement to help lower her blood pressure? List them in order from most effective to least effective for lowering BP. Allergies: none Meds Chlorthalidone 25 mg po daily Venlafaxine XR 150 mg daily Albuterol inhaler PRN shortness of breath Symbicort 80/4.5 twice daily Ibuprofen 600 mg twice daily for pain Pharmacology: Which of her medications might be contributing to her increased BP and explain how? Medicinal chemistry: What class of diuretics do hydrochlorothiazide, chlorthalidone and amiloride belong to? Compare and contrast the SAR of these drug classes. ROS: Occasional back pain, happening at random times; no c/o sensory loss, or visual changes No dysuria, flank pain, hematuria, pedal edema, chest pain. SOB occurs 1-2 times/week, needing to use rescue inhaler Physical Examination Gen: The patient is an obese Indigenous woman of Hispanic descent (Birth sex: female; Gender identity: woman) VS: BP 164/94 mm Hg, HR 92, RR 18, T 37.5°C; Wt 185, Ht 5′3″ BMI 32.8 Lungs/Thorax: Clear, breath sounds normal CV: Heart sounds normal, no murmurs, no bruits Abd: Soft NT/ND Neuro: A & O × 3 Labs (1 month ago, Fasting) Urea Nitrogen (BUN) Serum creatinine (SCr) Sodium Potassium Chloride CO2 Glucose Calcium Hemoglobin A1C Total cholesterol HDL LDL (direct) Triglycerides Reference Range 6-23 mg/dL 0.5-1.1 mg/dL 135-145 mmol/L 3.5-5.2 mmol/L 96-108 mmol/L 22-30 mmol/L <100 8.5-10.5 mg/dL < 5.7 (preDM) 6.5% (DM) < 200 mg/dL > 45 mg/dL Individualized < 150 mg/dL Result 24 1.1 140 4 102 24 120 9.9 5.7 % 204 27 145 157 Urinary albumin/creatinine ratio (UACR) TSH < 30 mg/g creatinine 25 0.5-5 mcg/dL 1.1 Pathophysiology: What is the relationship between Type II DM and hypertension? Therapeutics: Which drug class(es) would be reasonable to add to her regimen and why? Assessment: 1. Uncontrolled hypertension 2. Obesity 3. Anxiety 4. Asthma Use the table below to guide you in identifying the subjective and objective findings, creating an assessment with rationale, making an appropriate recommendation/intervention, describing the goal of therapy/therapeutic endpoint and determining monitoring parameters for each of the health-related problems. (Remember to Use the Pharmacist Patient Care Process: 1) Collect and Assess Information (Pertinent findings); 2) Develop and implement Care Plan (Recommendations/Interventions & Goal of Therapy/Therapeutic Endpoint); 3) Follow-up: Monitor and Evaluate (Efficacy& Safety/Toxicity) Healthrelated problems Subjective or objective findings What evidence from the case support the therapeutic problem? Goal of Therapy/ Therapeutic Endpoint Recommendation / Intervention Efficacy Safety / Toxicity Health-related problems Hypertension Monitor BP in one month The following are prescriptions that you, as the pharmacist, must assess and determine whether the patient should continue or stop the medication, or adjust the medication dose. For this part of the table, identify if you would dispense each medication, your justification, and what recommendation / intervention should be made / taken. Medication Orders Continue? Stop? Adjust? Justification and/or Recommendation / Dispense or not dispense Intervention Chlorthalidone 25 mg po daily Venlafaxine XR 150 mg daily Albuterol inhaler PRN shortness of breath Symbicort 80/4.5 twice daily Ibuprofen 600 mg twice daily for pain Therapeutics: Recommend a drug and dose that would be acceptable to add to her regimen and state why? Olmesartan 20 mg daily was added to her regimen. Medicinal chemistry: Discuss the SAR of Olmesartan compared to ACEIs. Pharmacology: Compare Olmesartan to Lisinopril in mechanism and ADEs. Therapeutics: In whom might a DHP CCB be recommended to manage HTN?





