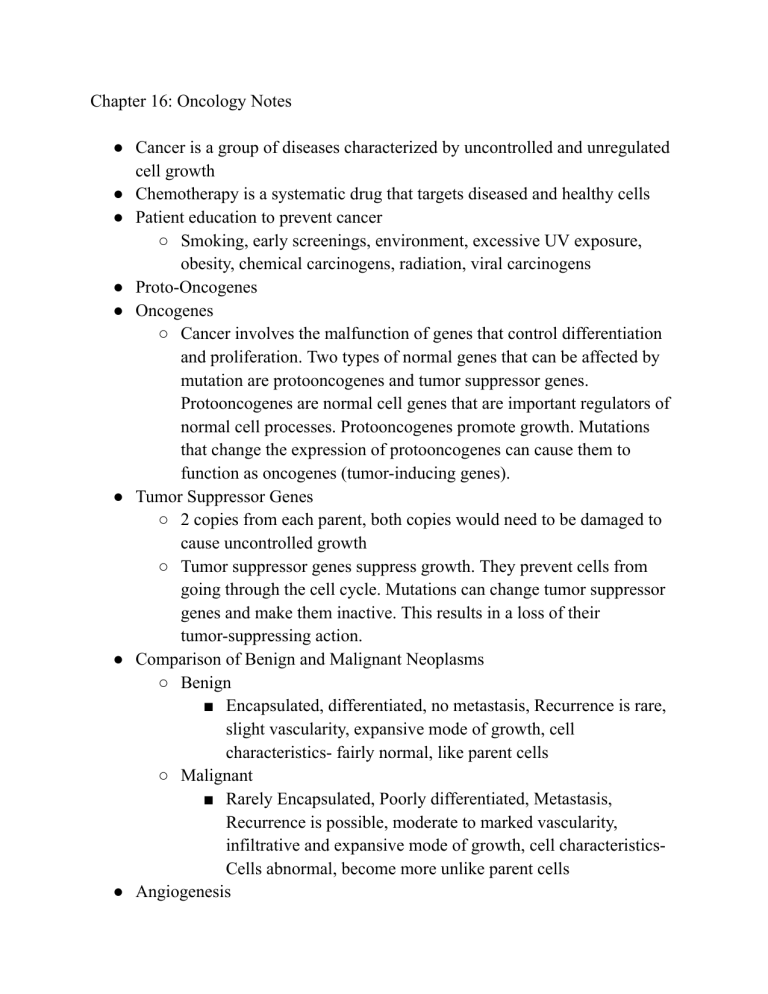
Chapter 16: Oncology Notes ● Cancer is a group of diseases characterized by uncontrolled and unregulated cell growth ● Chemotherapy is a systematic drug that targets diseased and healthy cells ● Patient education to prevent cancer ○ Smoking, early screenings, environment, excessive UV exposure, obesity, chemical carcinogens, radiation, viral carcinogens ● Proto-Oncogenes ● Oncogenes ○ Cancer involves the malfunction of genes that control differentiation and proliferation. Two types of normal genes that can be affected by mutation are protooncogenes and tumor suppressor genes. Protooncogenes are normal cell genes that are important regulators of normal cell processes. Protooncogenes promote growth. Mutations that change the expression of protooncogenes can cause them to function as oncogenes (tumor-inducing genes). ● Tumor Suppressor Genes ○ 2 copies from each parent, both copies would need to be damaged to cause uncontrolled growth ○ Tumor suppressor genes suppress growth. They prevent cells from going through the cell cycle. Mutations can change tumor suppressor genes and make them inactive. This results in a loss of their tumor-suppressing action. ● Comparison of Benign and Malignant Neoplasms ○ Benign ■ Encapsulated, differentiated, no metastasis, Recurrence is rare, slight vascularity, expansive mode of growth, cell characteristics- fairly normal, like parent cells ○ Malignant ■ Rarely Encapsulated, Poorly differentiated, Metastasis, Recurrence is possible, moderate to marked vascularity, infiltrative and expansive mode of growth, cell characteristicsCells abnormal, become more unlike parent cells ● Angiogenesis ● Anatomic Classification of Tumors- based upon the type of cells and/or anatomical location ● Metastasis- spread of cancer cells from original location to new locations ● Cancer Staging ○ Stage 0: Cancer in situ. Abnormal cells are present but have not spread to nearby tissue. Also called, carcinoma in situ, or CIS. CIS is not cancer, but it may become cancer. ○ Stage I: Tumor limited to the tissue of origin; localized tumor growth ○ Stage II: Limited local spread ○ Stage III: Extensive local and regional spread ○ Stage IV: Metastasis ● Pathology, biopsy: In histologic grading of tumors, the appearance of cells and degree of differentiation are evaluated pathologically. ● Histological grading ○ Grade I: Cells differ slightly from normal cells (mild dysplasia) and are well-differentiated (low grade). ○ Grade II: Cells are more abnormal (moderate dysplasia) and moderately differentiated (intermediate grade). ○ Grade III: Cells are very abnormal (severe dysplasia) and poorly differentiated (high grade). ○ Grade IV: Cells are immature, primitive (anaplasia), and undifferentiated. Cell origin is hard to determine (high grade). ○ Grade X: Grade cannot be assessed. ● TNM Classification System ○ We use the TNM classification system (Table 16.5) to determine the anatomic extent of cancer involvement. There are 3 parameters: tumor size and invasiveness (T), presence or absence of regional spread to the lymph nodes (N), and metastasis to distant organ sites (M). Examples of the TNM classification system are shown in Tables 30.26 and 56.7. We do not use TNM staging with all cancers. For example, we do not stage leukemias with TNM since they are not solid tumors. CIS has its own designation in the system (Tis). CIS has all the histologic characteristics of cancer except invasion, a key feature of the TNM staging system. ○ T-Primary Tumor (Tumor size and invasiveness), N-Regional Lymph Nodes, M- Distant Metastases ○ The original description of the extent of the tumor stays part of the record. If the patient needs more treatment, or if treatment fails, retreatment staging is done to determine the extent of the disease before retreatment. “Restaging” classification (rTNM) is distinguished from the stage at diagnosis since the clinical significance may be different. Staging cannot decrease, but the stage can increase. ● Prevention and Early Detection of Cancer ○ Limit alcohol use. ○ Get regular physical activity (e.g., 30 min or more of moderate physical activity 5 times weekly). ○ Maintain a normal weight. ○ Have regular physical examinations. ○ Obtain regular colorectal screenings. ○ Avoid cigarette smoking and other tobacco use. ○ Get regular mammography screening and Pap tests. ○ Be familiar with your own family history and risk factors for cancer. ○ Obtain adequate rest of at least 6–8 hours per night. ○ Use sunscreen with a sun protection factor of 15 or higher. Avoid tanning beds. ○ Eliminate, reduce, or change the perception of stressors and enhance the ability to effectively cope with stress (see Chapter 7). ○ Eat a balanced diet that includes vegetables and fresh fruits, whole grains, and fiber. Reduce dietary fat and preservatives. Limit smoked and salt-cured meats with high nitrite concentrations. ● Warning Signs of Cancer (Vague Warning Signs) ○ Change in bowel or bladder habits ○ A sore that does not heal ○ Unusual bleeding or discharge from any body orifice ○ Thickening or a lump in the breast or elsewhere ○ Indigestion or difficulty in swallowing ○ Obvious change in a wart or mole ○ Nagging cough or hoarseness ● Diagnostic studies depend on the suspected primary or metastatic site(s) of the cancer. Examples include: ○ Cytology studies (e.g., Pap test, bronchial washings) ○ Chest x-ray ○ Complete blood count (CBC), chemistry profile ○ Liver function studies (e.g., aspartate aminotransferase [AST]) ○ Endoscopic examination: upper GI, sigmoidoscopy, or colonoscopy (including guaiac test for occult blood) ○ Radiographic studies (e.g., mammography, ultrasound, CT scan, MRI) ○ Radioisotope scans (e.g., bone, lung, liver, brain) ○ PET scan (Fig. 16.7) ○ Tumor markers (e.g., CEA, AFP, PSA, CA-125) ○ Genetic markers (e.g., BRCA1, BRCA2) ○ Molecular receptor status (e.g., estrogen and progesterone receptors) ○ Bone marrow examination ● Sentinel node biopsy- biopsy the nearest draining biopsy to the cancer site ● The goals of cancer treatment are cure, control, and palliation ○ When cure is the goal, we expect treatment to have the greatest chance of eradicating the cancer. Curative cancer therapy differs by the type of cancer. It may involve local therapies (e.g., surgery or radiation) alone or in combination, with or without adjunctive systemic therapy (e.g., chemotherapy). ○ Control is the goal of treatment for cancers that we cannot completely eradicate but are responsive to anticancer therapies. As with other chronic illnesses (e.g., diabetes, heart failure), cancer can be controlled for long periods with therapy. ○ Palliation is the goal of treatment when the goals are symptom control or relief and maintaining a satisfactory quality of life. Palliative care and treatment are not mutually exclusive and can take place concurrently. An example of treatment in which palliation is the goal includes using radiation therapy to reduce tumor size and relieve subsequent symptoms, like the pain of bone metastasis. ● Cancer Treatments ○ Surgery ○ Chemotherapy ○ ○ ○ ○ ○ ○ ● ● ● ● Radiation therapy Immunotherapy Targeted therapy Nursing Management for treatments Nurses do not give chemotherapy Table 16.11: Problems Caused by Chemotherapy and Radiation Therapy ■ Myelosuppression ■ Tissue Vesicant ■ Weakness, hair loss, nausea/vomiting ■ High risk of infection due to immunocompromised status, bone marrow suppression ■ Diarrhea, mucositis, anemia ■ Skin issues Different routes of Chemotherapy ■ Oral ■ Intraarterial ■ Intracavitary (pleural, peritoneal) ■ Intramuscular ■ Intrathecal ■ Intravenous ■ Perfusion ■ Subcutaneous ■ Topical Only persons specifically trained in chemotherapy handling techniques should be involved with the preparation and administration of cancer drugs.10 Cancer drugs may pose a hazard to health care persons who do not follow safe handling guidelines. A person preparing, transporting, or giving chemotherapy may absorb the drug through inhalation of particles when reconstituting a powder or through skin contact from exposure to droplets or powder. Patients experience systemic symptoms What will you teach the patient about these? ○ Wigs for hair loss ○ Diet for n/v ○ Small frequent meals ● How will you help the patient manage the side effects? ● Radiation ○ Targeted at specific area ○ External beam-skin care is important ○ Internal radiation (brachytherapy) ■ Insertion of radioactive materials into or near the tumor ○ Principles of ALARA ■ The principles of ALARA (as low as reasonably achievable) and time, distance, and shielding are vital to our safety when caring for the person with a source of internal radiation. Organize care to limit the time spent in direct contact with the patient. To lessen anxiety and confusion, tell the patient the reason for time and distance limitations before the treatment. ● Immunotherapy and Targeted Therapy ○ Boost and manipulates environment to inhibit or attack cancer cells ■ Flu like symptoms ■ Orthostatic Hypotension ○ Myelosuppression ■ Nadir-lowest blood counts between 7-10 days after starting therapy ● What does this mean to you? ● What might be given to stimulate counts? ■ Fatigue ■ GI Issues ■ Skin issues ■ Pneumonitis ● Delayed acute inflammatory reaction that may occur within 1 to 3 months after completing thoracic radiation. This reaction is often asymptomatic. An increase in cough, fever and night sweats may occur. Some patients may develop pulmonary fibrosis (with or without pneumonitis), a late effect of therapy. ○ Table 16.19: Oncologic Emergencies ■ Tumor lysis syndrome ■ SIADH ■ Metabolic emergencies ● Hypercalcemia ■ SUperior vena cava syndrome ○ Read Page 284-288