Physica A: Statistical Mechanics and its Applications
Agent-Based Model for COVID-19: The Impact of Social Distancing and Vaccination
Strategies
--Manuscript Draft-Manuscript Number:
PHYSA-222618
Article Type:
Research Paper
Section/Category:
Concepts or methods of statistical mechanics in Complex Systems and Complex
Networks
Keywords:
COVID-19; COVID-19 vaccines; social distancing; agent-based modeling
Corresponding Author:
Aquino L. Espindola, Dr
Universidade Federal Fluminense
Volta Redonda, Rio de Janeiro BRAZIL
First Author:
Bruno S. de Andrade, BSC
Order of Authors:
Bruno S. de Andrade, BSC
Aquino L. Espindola, Dr
Aydamari Faria Junior, Dr.
Thadeu J. P. Penna, Dr.
Abstract:
In this work we study the transmission of the new coronavirus, SARS-CoV-2, which
causes COVID-19. Our main aim is to analyze the disease prevalence when
vaccination and social distancing strategies are used. Simulations are implemented
using an agent-based model (ABM) adapted from a SEIR type (Susceptible-ExposedInfectious-Recovered) compartmental model. Several scenarios are simulated using
the most common vaccines available in Brazil. On each scenario, different fractions of
the population are affected by vaccination and social distancing measures. Results
show the importance to start public health interventions to reduce the size of the
epidemic. Besides, simulations show that vaccination only is not capable to control the
disease spread.
Suggested Reviewers:
Suani Tavares Rubim de Pinho, Dr.
Professor, Federal University of Bahia
suani@ufba.br
Professor de Pinho has experience in mathematical modeling and recently has
published several papers about covid models.
Suzana Mossa de Oliveira, Dr.
Federal Fluminense University
mosssuzana@gmail.com
Professor has a large experience on computer simulations
Sílvio da Costa Ferreira Junior, Dr.
Professor, Federal University of Vicosa Department of Physics
silviojr@ufv.br
Professor has a large experience on biological computer simulations
Mary Pugh, PhD
Professor, University of Toronto Department of Mathematics
mpugh@math.utoronto.ca
Experience on mathematical modelling
Troy Day, PhD
Queen's University
day@queensu.ca
Professor Day is an applied mathematician working in the area of mathematical
biology.
Powered by Editorial Manager® and ProduXion Manager® from Aries Systems Corporation
Cover letter and Highlights
Cover Letter
Agent-Based Model for COVID-19: The Impact of
Social Distancing and Vaccination Strategies
Bruno S. de Andrade, Aquino L. Espı́ndola, Aydamari Faria Junior, Thadeu J.
P. Penna
October 18, 2022
Dear Editor,
In this study we propose an agent-based model (ABM) to understand how different vaccination and social distancing strategies may impact in the transmission
of the new coronavirus. All data used in the simulated scenarios are obtained
from Brazil, i.e., we have used information about the most common vaccines
available in Brazil. Results clearly show the importance of vaccination and
social distancing combination to avoid the collapse of the health system.
Because of the characteristics of the model such its computational implementation based on a agent-based model in a square lattice and the statistical analysis
of the results, we believe that this paper could interest and reach the audience
of Physica A.
If you need any additional information, please, do not hesitate to contact me.
Sincerely,
Aquino L. Espı́ndola
1
Highlights
Different types of vaccines require different percentage of people under
social distancing.
Any delay to start health care interventions also raises the risk of overburdening hospitals.
Vaccination only is not capable to control the disease COVID-19 spread.
2
Manuscript (New submissions only)
Click here to view linked References
Agent-Based Model for COVID-19: The Impact of
Social Distancing and Vaccination Strategies
Bruno S. de Andradea , Aquino L. Espı́ndolaa,∗ , Aydamari Faria Juniorb ,
Thadeu J. P. Pennaa
a
Departamento de Fı́sica, Instituto de Ciências Exatas - ICEx, Universidade Federal
Fluminense, Rua Des. Ellis Hermydio Figueira, 783, 27.213-145, Volta Redonda, Rio de
Janeiro, Brazil
b
Departamento de Psicologia, Instituto de Ciências Humanas e Sociais - ICHS,
Universidade Federal Fluminense, Rua Des. Ellis Hermydio Figueira, 783, 27.213-145,
Volta Redonda, Rio de Janeiro, Brazil
Abstract
In this work we study the transmission of the new coronavirus, SARS-CoV-2,
which causes COVID-19. Our main aim is to analyze the disease prevalence
when vaccination and social distancing strategies are used. Simulations are
implemented using an agent-based model (ABM) adapted from a SEIR type
(Susceptible-Exposed-Infectious-Recovered) compartmental model. Several
scenarios are simulated using the most common vaccines available in Brazil.
On each scenario, different fractions of the population are affected by vaccination and social distancing measures. Results show the importance to
start public health interventions to reduce the size of the epidemic. Besides,
simulations show that vaccination only is not capable to control the disease
spread.
Key words: COVID-19, COVID-19 vaccines, social distancing, agent-based
modeling
1
2
3
4
1. Introduction
Coronaviruses are pathogens that can affect humans and animals, causing
respiratory illnesses ranging from mild colds to life-threatening respiratory
problems [1]. To date, among all coronaviruses that can cause disease in
∗
Corresponding author
Preprint submitted to Physica A
October 19, 2022
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
humans, three were responsible for respiratory disease outbreaks that led to
a large number of deaths [2].
The first recent coronavirus human outbreak was detected in China, in
2002, spread to more than 30 countries, causing Severe Acute Respiratory
Syndrome (SARS-CoV). The second outbreak was identified in Saudi Arabia,
in 2012, known as Middle East Respiratory Syndrome (MERS-CoV), with
cases reported in 27 countries. The newest coronavirus outbreak was detected
in the province of Wuhan, China, in the end of 2019. The virus SARS-CoV-2,
as it have been named, is responsible for COVID-19 (Coronavirus Disease
2019 ) and spread throughout the world at a high transmission rate [2, 3].
In the end of January, 2020, the fast spread of the virus caused it to
be considered as an international public health emergency. Less than two
months later, the disease was declared as a pandemic by the World Health
Organization (WHO). So far, more than 6 million deaths have been confirmed
due to COVID-19, more than 650,000 in Brazil, according to official data.
More than two years after the pandemic beginning, new virus strains continue
to arise and infect people around the world [4].
SARS-CoV-2 can be transmitted via airborne droplets and particles through
speech, coughs or sneezes. Fomite-mediated transmission (handling objects
previously contaminated by the virus) was also reported. Therefore, this
virus can easily spread, specially in crowded places without adequate ventilation [5, 6].
To reduce the risk to be infected or infect others with the new coronavirus,
WHO recommendations are [5]: when leaving home, wear a face mask properly; keep at least one meter from other people; avoid closed, crowded places
without adequate ventilation for long periods of time; refrain from touching
objects and surfaces that may be contaminated with the virus; wash hands
with soap and water frequently or sanitize with gel alcohol; get vaccinated,
following local recommendations on vaccination. In addition to those measures, to prevent the overburdening of hospitals due to an expeditious spread
of the disease, social distancing practices had to taken by many countries [7].
Immune response to the virus infection varies in each infected person.
Some factors can make an individual more vulnerable to infection, namely:
age, health conditions, immune system status and possible pre-existing diseases, such as diabetes, high blood pressure and obesity [8].
About one third of infected individuals do not develop symptoms and
the majority of those infected with COVID-19 only suffer mild to moderate
symptoms [9]. Main symptoms include fever, dry cough, fatigue and loss
2
43
44
45
46
47
48
49
50
51
52
53
54
55
56
57
58
59
60
61
62
63
64
65
66
67
68
69
70
71
72
73
74
75
76
77
78
79
80
of smell and taste, although it may differ depending on the SARS-CoV-2
variant. In general, recovery usually takes up to two weeks from the onset of
the infection [10]. However, severe forms of COVID-19 may include shortness
of breath, difficulty breathing, chest pain, extreme tiredness or confusion. In
those cases emergency medical attention should be sought and recovery from
the disease can take up to six weeks, on average [8, 10].
Using previous data from MERS-CoV, SARS-CoV and ongoing research
of SARS-CoV-2, scientists around the world quickly started the process of
sequencing SARS-CoV-2 RNA and identified the spike protein [11], which
allows the virus to enter human cells [12]. Thus, in December 11th, 2020, a
mRNA spike-based vaccine, from pharmaceutical Pfizer-BioNTech, has been
approved and authorized for emergency use [13].
Despite the efforts (and success) of developing a vaccine, it took almost
a year to develop and distribute it (unevenly) throughout the world. Consequently, the aforementioned caveats entailed non pharmaceutical interventions, such as social distancing, to be the sole measures available for at least
the first year of pandemic [14]. Even after vaccine availability, most governments were obliged to combine vaccination campaigns with non pharmaceutical interventions to control the number of COVID-19 cases and hospitals
sufficiency.
In Brazil, the first batches of immunizations against COVID-19 arrived
on January, 19th, 2021. From that date up until now, millions of doses were
distributed all over the country by the Ministry of Health [15]. Initially, in
Brazil, health professionals and people aged over 80 were the first to receive
the vaccine, followed by younger individuals, until all population was eligible
[16].
Therefore, since the beginning of the pandemic, from the virus emergence
to the creation of new vaccines, some epidemiological questions have not
been answered yet. As a result, in this work we developed an agent-based
model (ABM) to simulate the impact of vaccines and social distancing on the
epidemic prevalence. This model allows us to analyze different vaccination
scenarios in combination with social distancing practices. In all simulations,
data from Brazil are used as parameters so we can identify the impact of
these public health interventions on the population.
This paper is organized as follows. In Section 2 we describe the disease
dynamics and how it is implemented using the agent-based modeling approach. In Section 3 different scenarios are simulated and the results are
discussed. Finally, concluding remarks are done in Section 4.
3
81
82
83
84
85
86
87
88
89
90
91
92
93
2. The Model
A SEIR type model was adapted to develop an agent-based model to simulate the transmission of the SARS-CoV-2 original strain. The model was
implemented on a square lattice of size N = L × L, with periodic boundary
conditions, where each site contains one individual with particular characteristics (health status, gender, age, vaccination status (vaccinated or not) and
social distancing status (isolated or not)). Besides, each individual may die
due natural causes which data were obtained from the Brazilian mortality
table (see Table S1). Finally, the period of time that an individual may stay
in a certain health state is randomly determined, according to the maximum
and minimum time limits of that particular COVID-19 health state [8, 17].
Other epidemiological parameters were obtained from the first COVID-19
wave in Brazil.
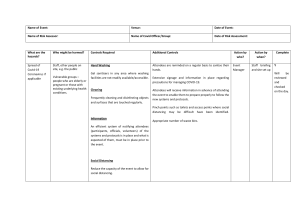
Figure 1: Flowchart presenting progression between COVID-19 health states. Model
compartments are: X, susceptible; E, exposed; P , pre-symptomatic; A, asymptomatic;
Sm , mild symptomatic; SM , mild symptomatic; SS , severe symptomatic; H, hospitalized
patient; ICU , patient admitted to the intensive care unit; D, killed due to COVID-19; R,
recovered.
94
95
96
97
The transition dynamics between agents’ health states is shown in Figure 1. In this figure, each compartment represents an individual health state,
namely: X, susceptible to infection; E, exposed to the virus (latency period)
and; P , pre-symptomatic, individual who does not present symptoms, but
4
98
99
100
101
102
103
104
105
106
107
108
109
110
111
112
113
114
115
116
117
118
119
120
may infect other ones. During the viral replication, a pre-symptomatic individual may progress to: A, asymptomatic; symptomatic Si , where the
subscript i = {m, M, S} represent the mild, moderate, and severe states,
respectively. Most of individuals with severe cases, SS , may be hospitalized,
H. If the health conditions worsens and, only if there are beds available, this
individual may be admitted to the Intensive Care Unit, ICU .
In the model, vaccines are applied to susceptible, S, and exposed, E, individuals, as long as people identified as infected have to wait until their symptoms subside [18]. Vaccination follows an immunization schedule that prioritizes advanced ages, starting with individuals over 90. Then, this threshold
age is reduced by 3 years each day, until vaccination reaches age 3, which is
the minimum [19].1
The four most used COVID-19 vaccines in Brazil were analyzed separately, taking into account their effectiveness against the most severe forms
of the disease. Despite the fact that vaccines were not developed to prevent
infection, this “secondary” goal has been considered and evaluated by researchers as well as governments around the world. Therefore, we also chose
to include effectiveness in our data.
For scenarios where all four vaccines were applied, we followed the percentage of doses used in Brazil. In addition, to compare results, we also
performed simulations in which vaccination does not occur. Effectiveness
data of each vaccine are shown in Table 1, as well as the percentage of doses
received by Brazil in 2021.
Efficacy [20]
Symptoms
Doses Received [21]
Vaccine
Infection
Severe
AstraZeneca
35.3%
94%
63%
Sinovac-CoronaVac
20.2%
50%
47%
Janssen
0.80%
86%
72%
Pfizer
36.0%
95%
86%
Table 1: Vaccines used in Brazil on 2021 and the percentage of doses received (column 2).
Columns 3 and 4 show the efficacy in case of severe symptoms or infection, respectively.
1
By June 2022, Moderna and Pfizer’s vaccines have been authorized for use in children
6 months or older.
5
121
122
123
124
125
126
127
In any infection stage an individual may recover, R, or; for the most severe
symptomatic cases, die, due to COVID-19 complications D [22]. Besides, in
the model, individuals also may die of natural death, according to the age
group mortality rate. This is obtained from the mortality table in Brazil, in
2020 (see Table S1, ??) [23].
Susceptible individuals may be infected by the virus as aforementioned
and the probability of infection is given by the equation:
pc = (1 − evac )[1 − (1 − β)n ],
128
129
130
131
132
133
134
135
136
137
138
where n is the total number of infectious agents with which the individual
had contact; β is the disease infectivity (R0 dependent) and; evac , acquired
immunity against infection if vaccination occurred.
The value of n is obtained counting the interaction of each agent with
its eight neighbors (Moore neighborhood), plus the possible random contacts
in the lattice, if the individual is not isolated. Then, a random number,
rn ∈ [0, 1], obtained from an uniform distribution, is generated and compared
to the pc value. If rn ≤ Pc , contagion takes place and the individual progress
to exposed, E, state; otherwise, he/she remains susceptible to COVID-19.
Exposed individuals are infected by the virus and enter in the incubation
(latency) period. In the model, incubation period is determined by:
Lt = rn(Lmax − Lmin ) + Lmin ,
139
140
141
142
143
144
145
146
147
148
149
150
(1)
(2)
where Lmin = 2 days and Lmax = 14 days are the minimum and maximum latency periods of SARS-CoV-2 virus, respectively. Again, a random
number, rn ∈ [0, 1], obtained from an uniform distribution, is multiplied by
latency time interval to obtain Lt .2 When latency period ends, the individual
becomes infectious and progress to the pre-symptomatic state, P ,.
Even in this state pre-symptomatic individuals may infect others in the
lattice. Thereafter, they may: present COVID-19 symptoms if they progress
to one of the symptomatic states ,Si , with i = {m, M, S} or; do not present
symptoms and pass to asymptomatic state, A. About 33% of individuals
infected with the new coronavirus progress to the asymptomatic state. The
remaining ones present symptoms in different degrees: mild, 81%; moderate,
14% and; severe, 5% [8].
2
This procedure is the same to determine all time intervals to other disease states.
6
The period of time that an individual stays in an infectious stage is given
151
152
by:
It = rn(Imax − Imin ) + Imin ,
153
154
155
156
157
158
159
160
161
162
163
164
165
166
167
168
169
170
171
172
where Imin = 2 days and Imax = 14 days are the minimum and maximum
time spent in this state, respectively. The values of Imin and Imax vary for
according to the stages of infection (mild, moderate or severe) [17].
The progression probability from a pre-symptomatic to a symptomatic or
asymptomatic are randomly defined by the following probabilities: 67% of
infectious individuals go to a symptomatic state; the remaining 33% become
asymptomatic and they will recover. Nevertheless, asymptomatic individuals are infectious and can transmit the disease to others. In general, these
individuals are“recovered” between 5 to 10 days after entering this state [24].
Milder symptoms include a dry cough, headache, fever, and loss of smell
and taste and the recovery takes up to two weeks. Severe symptomatic
individuals are subject to hospitalization, which is limited by the maximum
number of beds available in hospitals.
All simulated scenarios take into account the average occupancy percentage of beds that are used for the treatment of other diseases (50%). In the
model, hospitalized individuals are considered isolated and they are no longer
able to transmit the virus. In severe cases where there are no beds available
in the hospital, individuals may die due to COVID-19 complications, corresponding to the state D.
Hospitalization time is defined by the equation:
Ht = rn(Hmax − Hmin ) + Hmin ,
173
174
175
176
177
178
179
180
182
(4)
where rn ∈ [0,1] is a random number uniformly distributed and; Hmin = 5
days and Hmax = 15 days are the minimum and maximum period of hospitalization, respectively [25]. During hospitalization, individuals may: recover
from COVID-19, R, or; be admitted to the intensive care unit, ICU , if their
health status worsens and beds are available.
The number of beds available in intensive care units used in the model
are according to data obtained from Brazil Datasus [26]. The duration of an
ICU stay is determined by the expression:
ICUt = rn(ICUmax − ICUmin ) + ICUmin ,
181
(3)
(5)
where rn ∈ [0, 1] is a uniformly distributed random number; ICUmin = 3.8
days and ICUmax = 15.6 days are the minimum and maximum time of
7
193
treatment in ICU, respectively [25]. Individuals in ICU may: improve their
health status and recover, R, or; their health condition worsens and they die
because of COVID-19 complications, D.
When the transition from pre-symptomatic, P , to asymptomatic, A, or
symptomatic, Si , occurs, the individual can recover from the disease. In any
of these states, recovery can happen depending on the individuals age and
infection severity. To simulate this situation, a random number between 0
and 1 obtained from a uniform distribution is compared to the probability
of recovery of the individual [27]. In the case of recovery, he/she initially
becomes immunized against reinfections and no longer transmits the disease
to other agents.
194
3. Results
183
184
185
186
187
188
189
190
191
192
195
196
197
198
199
200
201
202
203
204
205
206
207
208
209
210
211
212
213
214
215
216
217
218
An in silico population is place in a square lattice of linear size L = 632
resulting in a populations of N = L×L individuals. The value of N = 399,424
is approximately the population of Macapá, the capital of the Brazilian state
Amapá. All results are obtained as the average over 100 realizations for each
scenario presented.
Thus, the ABM model is implemented to study the following scenarios:
different probabilities of vaccination; the population fraction which is under social distancing; vaccination and social distancing starting at different
outbreak moments and; in case of vaccination, which vaccines are used.
Each simulation step represents one day and all scenarios begin at day
t = 0; maximum simulation time is t = 400 days. In all scenarios, individuals
are randomly assigned with several characteristics according to the most
recent Brazilian population distribution [30]. Still at t = 0, all individuals are
in the susceptible state with exception of Iini = 5 individuals, which will start
as pre-symptomatic infectious (initial condition for disease propagation).
For each simulated scenario, if vaccination occurs, the population may be
vaccinated with one of the available vaccines in Brazil, namely: AstraZeneca,
Sinovac-CoronaVac, Janssen and Pfizer. Initially, vaccination covers 85%
of the population [31], following the percentage of doses received in Brazil
showed in Table 1.
Social distancing measures consider the following proportions of “isolation”: piso , of 50, 80 or 90%. Both vaccination and social distancing may
start in the t = 0th or t = 20th simulation day. In situations where all
four vaccines are applied, the percentage, pvac , of the eligible population to
8
Par.
Tmax
L
N
β
Iini
RCmax
pP →A
pSl
pSm
pSS
pH→ICU
Agemin
Hbeds
Description
maximum simulation period
linear size of the lattice
total population
infectivity parameter
number of P individuals at t = 0
maximum daily random contacts
prob. to progress from P to A state [8]
prob. to become Sl [8]
prob. to become Sm [8]
prob. to become SS [8]
prob. to be admitted in ICU [28]
Minimum age for vaccination [19]
number of hospital beds [26, 29]
Value
400 days
632
L×L
0.27 (calibrated)
5
3
0.33
0.81
0.14
0.05
0.25
5 years
2.03/1,000 inhab.
Table 2: Parameters used in the model.
219
220
221
222
223
224
225
226
227
228
229
230
231
232
233
234
235
236
237
238
be immunized may be of 50, 75, 85 or 95%. Besides, the interval between
simulation start to vaccination use may be a delay of 0, 20 or 40 days.
Immunization of an entire country using a single vaccine type, with the
highest efficacy and starting immediately after an outbreak, is unfeasible for
most countries facing an epidemic. Even so, it is critical to establish a baseline scenario to compare to COVID-19’s spread in a “no vaccine scenario”.
In addition, we simulate the most real situation: using a mix of the available
vaccines to immunize the population, after a certain time (e.g. the period
needed to develop and distribute vaccines), from the initial identification of
the epidemic.
Figure 2 shows the first set of simulations where vaccination and social
distancing start at t = 0th day for 85% of the eligible population for immunization. In this figure, each subfigure represents a different fraction of social
distancing, piso : (a), 0%; (b), 50%; (c) 80% and; (d), 90%.
In the scenario where no social distancing is implemented (Fig. 2(a)), the
number of infections has its peak on 27% of the total population when no
vaccine is applied (blue line). Keeping the same initial conditions, depending
on the vaccine used, the peak infections are: 20.3%, after 65 days, for SinovacCoronaVac (green line) and; 6.1%, after 90 days, for Pfizer vaccine (purple
line).
9
239
240
241
For different social distancing values (Figs. 2(b)-(d)): 50%(b), 80%(c)
and 90%(d), respectively, as expected, there is an evident reduction in the
number of infectious individuals. These results are unequivocally obtained
due to the combination of social distancing and vaccination.
Figure 2: COVID-19 prevalence in Brazil with vaccination and social distancing in t = 0th
day. Each curve represent the applied vaccine: Blue, no vaccination; Orange, Astrazeneca;
Green, Sinovac-CoronaVac; Red, Janssen; Purple, Pfizer and; Brown, all vaccines used in
Brazil. Parameters are: pvac = 85% in all subfigures; piso : (a), 0%; (b), 50%; (c), 80%;
(d), 90%.
242
243
244
245
246
247
248
249
Notice that in all Figures 2(a)-(d) that Janssen’s vaccine (red line) has
a similar behavior as the set of vaccines used in Brazil (brown line). In
Fig. 2(a), the set of vaccines applied in Brazil led to a infection peak after
the 75th day, i.e., with 12.5% of the population. However, if piso = 90
(Fig. 2(d)) this peak is reduced to 1.3% in the 270th day after the simulation
beginning. This meaningful reduction in the spread of COVID-19 would be
sufficient to avoid the overburden of hospitals and its consequences.
10
Figure 3: COVID-19 prevalence in Brazil with vaccination and social distancing in the
t = 20th day. Each curve represents a vaccination strategy: Blue, no vaccine; Orange,
Astrazeneca; Green, Sinovac-CoronaVac; Red, Janssen; Purple, Pfizer and; Brown, all
vaccines applied in Brazil. Parameters are: pvac = 85% in all subfigures; piso : (a) 0%, (b)
50%, (c) 80%; (d) 90%.
250
251
252
253
254
255
256
257
258
259
260
In Figure 3, as in the previous scenarios, pre-symptomatic individuals
enter the system at day t = 0 but vaccination and social distancing only
start in the t = 20th day. In this case, regardless the vaccine used, lines
have sharper peaks in comparison to those obtained in Figure 2. The curves
have a remarkably similar behavior to that of the outbreak beginning. These
results suggest that virus transmission is uncontrolled and, as a consequence
(and proportionally), so is the number of severe COVID-19 cases. Therefore,
this scenario may lead to hospitals overburdening and, depending on the
available resources, the health care system may collapse.
Figure 4 shows the total number of infectious individuals for different
isolation scenarios, piso : 0%(a), 50%(b), 80%(c) and 90%(d), respectively.
11
Figure 4: COVID-19 prevalence in Brazil with vaccination and social distancing started
in the t = 0th day. Each curve represents the populations fraction eligible for vaccination:
Blue, 0%; Orange, 50%; Green, 75%; Red, 85% and; Purple, 95%. In subfigures, social
distancing, piso , parameters are: (a) 0%; (b) 50%; (c) 80%; (d) 90%.
261
262
263
264
265
266
267
268
269
270
271
272
Finally, each line represents the percentage of eligible population for immunization, pvac : Blue, 0%; Orange, 50%; Green, 75%; Red, 85% and; Purple,
95%.
In the same panel, for the scenario where pvac = 95% and piso = 0%,
Fig. 4(a), purple line), after the 80th day infection is 11.2% of the population.
On the contrary, for pvac = 95% and piso = 90% (Fig. 4(d), purple line)
there is a noticeable reduction on virus spreading as the infectious peak is
0.5%, occurring in the 370th day. Comparison between these data supports
the importance of social distancing, since there is a 95.5% reduction in the
number of cases between purple lines in Figs. 4 (a) and (b).
Figure 5 also shows the scenarios with four most used vaccines in Brazil.
However, in this case, vaccination and social distancing start in the t = 20th
12
Figure 5: COVID-19 prevalence in Brazil with vaccination and social distancing started
in the t = 20th day. Each curve represents the population fraction eligible for vaccination:
Blue, 0%; Orange, 50%; Green, 75%; Red, 85% and; Purple, 95%. In subfigures, social
distancing, piso , parameters are: (a) 0%; (b) 50%; (c) 80%; (d) 90%.
273
274
275
276
277
278
279
280
281
282
283
284
day. Infections peaks in Figures 5(a)-(d) tend to be dispersed as vaccination
and social distancing cover a larger percentage of the population.
The purple line in Figure 5(a) shows the scenario for pvac = 95% and
piso = 0%, with a peak of infected individuals of 13.2% in the 60th day.
However, for the scenario where pvac = 95% and social distancing is raised
to piso = 90% ( Figure 5(d,purple line), the infection peak of only 0.98%
occurs approximately in the 120th day. These data restate the importance
of vaccination in combination with social distancing, not only to reduce the
infection peak, but also to delay it, as well.
An even more noteworthy comparison lies between data from Figs. 4 and
5 for pvac = 95% and piso = 0% (purple lines). When interventions start in
day 0: infection peak is 11.2% in the 80th day; for pvac = 95% and piso = 90%
13
285
286
287
288
289
290
291
292
infection peak is ≈ 0.5% in the 370th day. Furthermore, when interventions
begin in the 20th day: for pvac = 95% and piso = 0% infection peak is
13.2% in the 60th; for pvac = 95% and piso = 90% the infection peak of is
0.98% in the 120th day. These data show any delay to initiate public health
interventions may significantly hold back its impact to control virus spread.
The 20 days delay (both vaccination and isolation), as used in this model,
had a remarkable impact on scenarios outcomes. Distinctively better results
are obtained on those cases with the higher control of virus transmission.
Figure 6: COVID-19 prevalence in Brazil with vaccination and social distancing started in
the t = 40th day. Each curve represents the populations fraction eligible for vaccination:
Blue, 0%; Orange, 50%; Green, 75%; Red, 85% and; Purple, 95%. In subfigures, social
distancing, piso , parameters are: (a) 0%; (b) 50%; (c) 80%; (d) 90%.
293
294
295
296
In Figure 6, where interventions start in the t = 40th day, it is possible
to see that all infection peaks happen closer to each other, almost at the
same point. For pvac = 95% and piso = 0% (Fig. 6(a),purple line), the
maximum is 26.3%; for piso = 90% and pvac = 95% (Fig. 6(d), purple line)
14
297
298
299
300
301
302
303
304
305
306
307
the maximum is 13.8%. Comparing both scenarios, despite the difference
of almost 50% on the infection peak, this reduction is approximately 90% if
social distancing practice is extremely high. Note that this result considers
the best scenario modeled ,i.e., the highest vaccination and social isolation
distancing percentage.
For scenarios in which smaller fractions of the population are subjected to
interventions (vaccination and/or social distancing), the number of infected
individuals is worrisome and the health system may become overburdened. It
is fundamental to highlight that delaying interventions for more than a month
may completely frustrate any infection control, as even the best vaccination
rates proved to be insufficient to completely contain virus spread.
Figure 7: Hospital beds occupation due to COVID-19 with vaccination and social distancing started in the t = 0 day. Each curve represents a set of (pvac , piso ) parameters: Blue,
(0%, 0%); Orange, (0%, 90%); Green, (50%, 50%); Black, (50%, 80%); Purple, (50%,
90%); Brown, (85%, 50%); Pink, (85%, 80%); Grey, (85%, 90%); Yellow, (95%, 50%);
Cyan, (95%, 80%) and; Red, (95%, 90%).
308
309
310
In Figure 7 is shown the fraction of occupied beds by patients hospitalized due to COVID-19. In all simulations, the estimated maximum capacity of hospitals for patients admission with severe COVID-19 is given
15
Figure 8: Hospital beds occupation due to COVID-19 with vaccination and social distancing started in the t = 20th day. Each curve represents a set of (pvac , piso parameters:
Blue, (0%, 0%); Black, (50%, 80%); Purple, (50%, 90%); Brown, (85%, 50%); Pink, (85%,
80%); Grey, (85%, 90%); Yellow, (95%, 50%); Cyan, (95%, 80%) and; Red, (95%, 90%).
311
312
313
314
315
316
317
318
319
320
321
322
323
324
325
by Ref. [26, 29]. In addition, also in all scenarios, vaccination and social
distancing measures are started on the first day of each scenario.
For pvac = 50% and piso = 50% (green line), and for pvac = 0% and
piso = 90% (orange line), both curves represent a critical hospital occupancy
zone, between 80 and 100% of hospital bed usage. In these cases, even the
ideal scenario (vaccination and social distancing start in the first day), the
parameters combination, pvac and piso , are not as effective to control the
disease spread and to reduce the number of severe infection cases either.
In Figure 7, using the combination pvac = 50% and piso = 80% (black
curve), the maximum occupancy reaches 64.6%, what drives the health system to an intermediate alert zone,i.e., between 60 and 80% of occupied beds.
The remaining vaccination and isolation sets take the system out of the alert
zone because virus transmission is controlled. The most effective pair of parameters, pvac = 95% and piso = 90% (red curve), leads the system to a
maximum of only 1.5 hospitalization per 100,000 inhabitants.
16
Figure 9: Hospital beds occupation due to COVID-19 with vaccination and social distancing started in the t = 40th day. Each curve represents a set of (pvac ,piso ) parameters: Blue,
(0%,0%); Black, (50%,80%); P urple, (50%,90%); Brown, (85%,50%); P ink, (85%, 80%);
Grey, (85%, 90%); Yellow, (95%, 50%); Cyan, (95%, 80%) and; Red, (95%, 90%).
326
327
328
329
330
331
332
333
334
335
336
337
338
339
340
Figures 8 and 9 present the scenarios where vaccination and social distancing start in the t = 20th and t = 40th days, respectively. In these
figures, we have omitted the combinations of pvac and piso that exceeded
hospital capacity.
In Figure 8, the combination of pvac = 50% and piso = 80% (black curve)
causes a 72.5% occupancy, a value inside the intermediate alert zone. All
scenarios in which social distancing is not present (piso = 0%) result in an
exceed hospital capacity, causing deaths due to lack of available beds. For
scenarios showed in Figure 9, only the combinations pvac = 85 or 95%, plus
piso =80 or 90% (Pink, Grey, Cyan and Red lines), does not cause an exceed
in the hospitals capacity.
For pvac = 50% and piso = 90% (purple lines), hospital beds’ occupancy
are 97.9%. Although all simulations lead to a critical state, scenarios with
piso = 90% are the most effective to slow down the infection spread. Consequently, there is a reduction in the number o deaths due to the most severe
17
341
342
forms of the disease. In these cases, the maximum occupancy is 94.4% for
pvac = 85% (grey line) and, 93.4% for pvac = 95% (red line).
Figure 10: COVID-19 health states for vaccination and social distancing started in the
t = 0th day. Each curve represents a health state: Blue, susceptible; Orange, exposed;
Green, infectious; Red, recovered; Purple, dead due to COVID-19 and; Brown, vaccinated.
Parameters are: pvac = 85% in all subfigures; piso : (a) 0%, (b) 50%, (c) 80%; (d) 90%.
343
344
345
346
347
348
349
350
351
352
353
Figures 10, 11 and 12 show details about population health status during a
COVID-19 outbreak. Colors in the lines represent an individuals health state
namely: susceptible, Blue; exposed to virus, Orange; infectious, Green; recovered, Red; vaccinated, Brown and; dead, purple. Vaccination is available
to 85% of the eligible population and variable social distancing percentage.
The most successful scenario for the population has piso = 90% and interventions start immediately (t = 0) (Figure 10(d), green line) which outcome
is an infection peak of 1.3% int the 270th day. Still in this scenario, the
cumulative number of deaths due to COVID-19 is approximately 0.18% of
the total population, or 180 deaths per 100,000 people.
Simulating the same scenario (piso = 90%), but interventions start in the
18
Figure 11: COVID-19 health states for vaccination and social distancing started in the
t = 20th day. Each curve represents a health state: Blue, susceptible; Orange, exposed;
Green, infectious; Red, recovered; Purple, dead due to COVID-19 and; Brown, vaccinated.
Parameters are: pvac = 85% in all subfigures; piso : (a) 0%, (b) 50%, (c) 80%; (d) 90%.
354
355
356
357
358
359
360
361
362
363
364
365
366
t = 20th day (Figure 11(d), green line), the infection peak is 1.74% in the
120th day. In the end of the simulation, there are 329.5 deaths per 100,000
people. As expected, if interventions start later, i.e, in the t = 40th with
piso = 90% (Figure 12(d), green line), the outcome is remarkably worse. The
infection peak reaches 13.8% in the 60th day with 5.4% of the population
deceased, or 5,392 deaths per 100,000 people.
The number of COVID-19 death cases when interventions start after 20
days is almost twice as high as when they start immediately. Moreover, a 40
days delay in interventions amplifies dramatically the increase in deaths,
almost 30 times higher. This critical situation, mixed with the possible
overburdening of hospitals (see Figure 9) may result in the country’s health
system collapse. In other words, insufficient infection control to deal with of
severe COVID-19 cases and, therefore, a scenario ineffective to fight against
19
Figure 12: COVID-19 health states vaccination and social distancing started in the t =
40th day. Each curve represents a health state: Blue, susceptible; Orange, exposed;
Green, infectious; Red, recovered; Purple, dead due to COVID-19 and; Brown, vaccinated.
Parameters are: pvac = 85% in all subfigures; piso : (a) 0%, (b) 50%, (c) 80%; (d) 90%.
367
the epidemic.
368
4. Concluding Remarks
369
370
371
372
373
374
375
376
377
378
In this work we have developed an agent based model (ABM) in order
to study the influence of vaccination and social distancing on the prevalence
of COVID-19, the disease caused by SARS-CoV-2 infection. We have used
different parameters to simulate interventions, i.e., different vaccination and
social distancing percentages to understand some of COVID-19 dissemination
aspects.
Taken together, our results showed that: i) to maximize its efficiency, i.e.,
to obtain better control of infection, interventions should be implemented as
soon as possible; ii) delaying interventions will raise not only the number of
infections, but also the number of deceased due to COVID-19; iii) delaying
20
385
interventions also raises the risk of overburdening hospitals, possibly leading
health’s system to failure; iv) only vaccination (no social distancing measures)
is not capable of controlling virus dissemination.
Finally, since this work focused on data related to the original strain of
SARS-CoV-2, new data about to SARS-CoV-2 variants should be addressed
in future works. In addition, the possibility of reinfection and the consideration of vaccine booster doses should also be studied.
386
References
379
380
381
382
383
384
387
388
389
390
391
392
393
394
395
396
397
398
399
400
401
402
403
404
405
406
407
408
409
410
[1] Governo do Estado de São Paulo. Sp contra o novo coronavÍrus. https:
//www.saopaulo.sp.gov.br/coronavirus/. Accessed: 07/01/2020.
[2] Veja Saúde.
As diferenças e semelhanças entre outros coronavı́rus e o sars-cov-2. https://saude.abril.com.br/medicina/
as-diferencas-e-semelhancas-entre-o-sars-cov-2-e-outros-coronavirus/.
Accessed: 20/02/2021.
[3] Brenda L. Tesini. Coronavı́rus e sı́ndromes respiratórias agudas (mers
and sars) - doenças infecciosas.
https://www.msdmanuals.com/
pt-br/profissional/doenas-infecciosas/vrus-respiratrios/
coronavrus-e-sndromes-respiratrias-agudas-covid-19-mers-e-sars.
Accessed: 04/02/2022.
[4] Worldometer.
Covid-19 coronavirus pandemic.
https://www.
worldometers.info/coronavirus/#countries, 2021.
Accessed:
07/31/2021.
[5] World
Health
Organization.
Coronavirus
disease
(covid-19):
How is it transmitted?
https://
www.who.int/news-room/questions-and-answers/item/
coronavirus-disease-covid-19-how-is-it-transmitted.
Accessed: 03/12/2021.
[6] Jorge D.C.P. Veiga R.V. et al. Oliveira, J.F. Mathematical modeling
of covid-19 in 14.8 million individuals in bahia, brazil. Nat Commun,
12:333, 2021.
[7] Ministério da SaúdeWorld Health Organization.
teria
for
releasing
covid-19
patients
from
21
Criisolation.
411
412
413
414
415
416
417
418
419
420
421
422
423
424
425
426
427
428
429
430
431
432
433
434
435
436
437
438
439
440
441
442
https://www.who.int/news-room/commentaries/detail/
criteria-for-releasing-covid-19-patients-from-isolation.
Accessed: 06/25/2020.
[8] Donna Christiano. How to tell if your coronavirus symptoms are
mild, moderate, or severe.
https://www.singlecare.com/blog/
news/coronavirus-symptoms-and-incubation-period/. Accessed:
07/18/2022.
[9] Centers for Disease Control and Prevention. Covid-19 pandemic planning scenarios. https://www.cdc.gov/coronavirus/2019-ncov/hcp/
planning-scenarios.htm. Accessed: 10/11/2021.
[10] World Health Organization. Coronavirus disease (covid-19). https:
//www.who.int/health-topics/coronavirus. Accessed: 07/31/2022.
[11] Philip Ball. The lightning-fast quest for COVID vaccines — and what
it means for other diseases. Nature, 589(7840):16–18, December 2020.
[12] Lorenzo Casalino, Zied Gaieb, Jory A. Goldsmith, Christy K. Hjorth,
Abigail C. Dommer, Aoife M. Harbison, Carl A. Fogarty, Emilia P.
Barros, Bryn C. Taylor, Jason S. McLellan, Elisa Fadda, and Rommie E.
Amaro. Beyond shielding: The roles of glycans in the SARS-CoV-2 spike
protein. ACS Central Science, 6(10):1722–1734, September 2020.
[13] U.S. Food and Drug Administration. Fda approves first covid-19
vaccine. https://www.fda.gov/news-events/press-announcements/
fda-approves-first-covid-19-vaccine. Accessed: 30/08/2021.
[14] Daniel C.P. Jorge, Moreno S. Rodrigues, Mateus S. Silva, Luciana L.
Cardim, Nı́vea B. da Silva, Ismael H. Silveira, Vivian A.F. Silva, Felipe A.C. Pereira, Arthur R. de Azevedo, Alan A.S. Amad, Suani T.R.
Pinho, Roberto F.S. Andrade, Pablo I.P. Ramos, and Juliane F. Oliveira.
Assessing the nationwide impact of covid-19 mitigation policies on the
transmission rate of sars-cov-2 in brazil. Epidemics, 35:100465, 2021.
[15] Agência Brasil. Vacinação contra a covid-19 começa em todo o paı́s.
https://agenciabrasil.ebc.com.br/saude/noticia/2021-01/
vacinacao-contra-covid-19-comea-em-todo-o-pais.
Accessed:
01/20/2021.
22
443
444
445
446
447
448
449
450
451
452
453
454
455
456
457
458
459
460
461
462
463
464
465
466
467
468
469
470
471
472
473
474
475
[16] Ministério da Saúde.
Profissionais de saúde e idosos institucionalizados serão os primeiros a receber doses de vacina contra a
covid-19. https://www.gov.br/saude/pt-br/assuntos/noticias/
profissionais-de-saude-e-idosos-institucionalizados-serao-os-primeiros-a-rece
Accessed: 30/01/2021.
[17] Neha Pathak.
Coronavirus incubation period:
How long
and when most contagious.
https://www.webmd.com/lung/
coronavirus-incubation-period. Accessed: 02/18/2022.
[18] Centers for Disease Control and Prevention. Frequently asked questions
about covid-19 vaccination.
https://www.cdc.gov/coronavirus/
2019-ncov/vaccines/faq.html, journal=Centers for Disease Control
and Prevention. Accessed: 06/23/2022.
[19] Centers for Disease Control and Prevention.
Covid-19 vaccines for children and teens. https://www.cdc.gov/coronavirus/
2019-ncov/vaccines/recommendations/children-teens.html. Accessed: 04/30/2022.
[20] Institute for Health Metrics and Evaluation.
Covid-19 vaccine efficacy summary.
https://www.healthdata.org/covid/
covid-19-vaccine-efficacy-summary. Accessed: 02/01/2022.
[21] Ministério da Saúde.
Plano nacional de operacionalização da vacinação contra a covid-19 - pno.
https:
//www.gov.br/saude/pt-br/coronavirus/vacinas/
plano-nacional-de-operacionalizacao-da-vacina-contra-a-covid-19,
2021. Accessed: 07/30/2022.
[22] Franz Wiesbauer.
Covid-19 disease progression.
https:
//www.medmastery.com/guide/covid-19-clinical-guide/
covid-19-disease-progression, 2021. Accessed: 11/21/2020.
[23] IBGE Instituto Brasileiro de Geografia e Estatı́stica. Tábuas completas
de mortalidade. https://www.ibge.gov.br/estatisticas/sociais/
populacao/9126-tabuas-completas-de-mortalidade.html.
Accessed: 12/01/2020.
[24] Magdalena Osumi.
Covid-19 patients with
likely to stay that way, japan researchers say.
23
no symptoms
https://www.
476
477
478
479
480
481
482
483
484
485
486
487
488
489
490
491
492
493
494
495
496
497
498
499
500
501
502
503
504
505
506
japantimes.co.jp/news/2020/06/15/national/science-health/
asymptomatic-covid-19-patients/. Accessed: 06/12/2020.
[25] Christel Faes, Steven Abrams, Dominique Van Beckhoven, Geert
Meyfroidt, Erika Vlieghe, and Niel Hens and. Time between symptom onset, hospitalisation and recovery or death: Statistical analysis
of belgian COVID-19 patients. International Journal of Environmental
Research and Public Health, 17(20):7560, October 2020.
[26] Gove.
Relação de leitos por mil habitantes recorte regional gove.
https://www.gove.digital/wp-content/uploads/2020/03/
Leitos.pdf, journal=Gove - Plataforma de Decisão para Eficiência de
Governos. Accessed: 12/22/2020.
[27] Md. Monirul Islam, Saimon Shahriar, Fahima Jannat Koly, Shaila Kabir,
Abu Asad Choudhury, Jakir Ahmed Chowdhury, Md. Rafat Tahsin, and
Md. Shah Amran. Academic journals - african journal of pharmacy and
pharmacology - a cross-sectional pilot study on covid-19 disease pattern, recovery status and effect of co-morbidities in bangladesh. African
Journal of Pharmacy and Pharmacology, May 2021.
[28] Semagn Mekonnen Abate, Siraj Ahmed Ali, Bahiru Mantfardo, and
Bivash Basu. Rate of intensive care unit admission and outcomes among
patients with coronavirus: A systematic review and meta-analysis. PLoS
One, 15(7):e0235653, July 2020.
[29] Francisco Carlos Cardoso de Campos and Cláudia Marques Canabrava.
Brazil in the iuc: hospital care in times of pandemic. SciELO Preprints,
Oct. 2020.
[30] Ana Laura Moura dos Santos Azevedo. Ibge - educa: Jovens.
https://educa.ibge.gov.br/jovens/conheca-o-brasil/
populacao/18318-piramide-etaria.html. Accessed: 15/12/2019.
[31] J. Mendoza.
Covid-19 vaccine:
Immunization brazil
2022.
https://www.statista.com/statistics/1288019/
population-vaccinated-against-covid-brazil/.
Accessed:
05/22/2022.
24
507
508
509
510
511
Supplement: Agent-Based Model for COVID-19: The Impact of
Social Distancing and Vaccination Strategies
Bruno S. de Andrade, Aquino L. Espı́ndola, Aydamari Faria Junior,
Thadeu J. P. Penna
Mortality Table for Brazil.
Age
0
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
Death Probability
(per 1,000 inhab.)
11.566
0.789
0.507
0.386
0.317
0.272
0.242
0.222
0.209
0.205
0.210
0.226
0.257
0.311
0.397
0.668
0.832
0.978
1.091
1.179
1.265
1.351
1.409
1.435
1.436
1.426
1.420
Age
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
Death Probability
(per 1,000 inhab.)
1.423
1.445
1.481
1.522
1.565
1.613
1.666
1.727
1.798
1.881
1.976
2.082
2.202
2.336
2.487
2.661
2.861
3.087
3.334
3.600
3.884
4.186
4.508
4.856
5.231
5.629
6.052
Age
54
55
56
57
58
59
60
61
62
63
64
65
66
67
68
69
70
71
72
73
74
75
76
77
78
79
80+
Table S1: Mortality Table for Brazil - 2020 [23].
1
Death Probability
(per 1,000 inhab.)
6.503
6.992
7.521
8.083
8.677
9.315
10.007
10.769
11.612
12.547
13.582
14.698
15.920
17.302
18.873
20.629
22.526
24.564
26.803
29.268
31.964
34.858
37.969
41.375
45.125
49.231
100.000
Declaration of Interest Statement
Declaration of interests
☒The authors declare that they have no known competing financial interests or personal relationships
that could have appeared to influence the work reported in this paper.
☐The authors declare the following financial interests/personal relationships which may be considered
as potential competing interests: