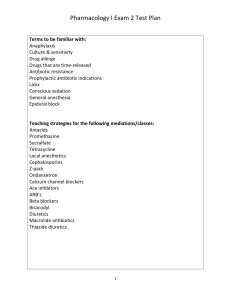
Exam 3 Study Guide Hi Everyone! Here is some help for exam 3. STUDY GUIDE FOR EXAM 3 This test examines three areas: Cardiovascular, Renal, and Respiratory Pharmacology. Many times, you will have a patient who is compromised in all 3 areas and will need drugs that affect all 3—that is why we studied all 3 together (it was not just to overwhelm you!). As you study, keep the interplay between the drugs in mind—it will be apparent especially between the Renal and Cardiac and Renal and Respiratory drugs—Renal drugs are important—though we don’t have many of them. Cardiovascular We started with Heart Failure. Remember a couple of things here: Know the effects and side effects of Digoxin, and also the presentation of Dig toxicity. How is it treated? In the acute patient, Milrinone may be used—it increases the force of contraction. ACEI are mainstay drugs in HF. Lisinopril is the prototype (but know the other ‘pril drugs as well—any drug ending in PRIL is an ACEI). It is well tolerated, but may cause a cough…sometimes can cause angioedema (life-threatening), and causes hyperkalemia. It does NOT work on the heart, but helps with BP, cardiac remodeling and fluid management overall in the body. Related to the ACEI are the Angiotensin Receptor Blockers (ARBs). One that is used a lot in HF is Valsartan. A combination drug—Sacubitril/Valsartan—is a newer drug for HF, as is Ivabradine. Also know that diuretics (discussed later) are used in HF, especially hydrochlorothiazide and furosemide, and that potassium levels need to be monitored in these patients! Finally, the patient with HF often takes something to control blood pressure—see below, but a beta blocker is often used. Heart Failure Drugs: Digoxin, lisinopril, valsartan, hydrochlorothiazide, furosemide, milrinone, sacubitril/valsartan, ivabradine; remember, beta blockers are often used in these patients, too. For Hypertension, there are many drugs, and three classes are used the most. Calcium channel blockers (Amlodipine, Nifedipine, Verapamil) are used a lot for HTN. Know their main SE (headache, constipation, cardiac suppression). They are also used for dysrhthymias and chest pain. Another big class of drugs for HTN is ACEI/ARBs. Again, the side effects are as above—and they should never be used in pregnancy (true for most antihypertensives). The good thing about ACEI is that it is OK for a patient to discontinue them abruptly without getting rebound HTN. Related to the ACEI are the ARBs such as Losartan and Valsartan. Newer related drugs are Eliskiren and Eplerenone. Same side effects but maybe your patient won’t develop that cough! Beta Blockers are one of the “big four” classes of drugs we studied (along with CCBs, ACEI/ARBs and thiazide diuretics)—but remember, they are no longer considered drugs of first choice. Beta blockers all end in OLOL. Good ones to know are Propranolol, Metoprolol, Atenolol, Labetolol and Carvedilol (a rule breaker with respect to the ‘olol name thing) Know how they work and their MAIN side effects—tiredness, reduced exercise tolerance (due to decreased heart rate!). These drugs are also used in HF patients to reduce the work of the heart, and are useful for atrial dysrhythmias like a-fib. Make sure you know the difference between Beta 1, beta 1 and 2, and alpha 1, beta 1, beta 2 blockers. Most commonly used for HTN are the thiazide diuretics, but furosemide, amiloride, spironolactone and mannitol may all be used. With all diuretics, electrolytes must be monitored, and in some cases, the patient will require electrolyte replacement—especially of potassium. Remember, the thiazide diuretics will cause minor potassium loss. Sometimes an ACEI or ARB is prescribed with these to offset that K loss. Do you know that most patients are advised to take their antihypertensives AT NIGHT to limit their side effects? The only patients who are NOT, are the ones taking diuretics, since diuretics make you urinate! Other antihypertensives to know for the test are Hydralazine (may be used in pregnancy), Clonidine (good for ISH but watch that rebound HTN if discontinued!), Nitroprusside (for hypertensive emergency), Minoxidil and Prazosin (for side effects). AND….the diuretics! Drugs for Hypertension: Beta blockers, calcium channel blockers, ACEI, ARBs, thiazides, furosemide, spironolactone, mannitol, eliskiren, eplerenone, hydralazine, clonidine, nitroprusside, minoxidil, prazosin We studied angina (chest pain)! Know how the nitrates work and the timeframe of PO, vs. sublingual vs. the patch nitrates—which works the fastest? How does tolerance develop and what can a patient do to prevent it? Do beta blockers work for all types of angina? Do nitrates? Calcium channel blockers? Which drugs or other compounds should be avoided in the patient taking nitrates? Drugs for angina: Nitroglycerine preps, Isosorbide dinitrate, Amlodipine, Propranolol, Metoprolol, Atenolol. We studied drugs to prevent clots which can cause chest pain! Make SURE you know the difference between drugs that prevent clots—those that are antithrombotic vs. antiplatelet (Warfarin, rivaroxaban, epixaban and heparin and the low molecular weight heparins like Enoxaparin are antithrombotic…..aspirin and Clopidogrel are antiplatelet) vs. clot busters (Tenecteplase is a clot buster). When are these used? Yes, this gets a little tricky! Usually, patients are given clot busters when they are having an MI or ischemic stroke—this is confirmed by an EKG for an MI, CT for a stroke. A STEMI is seen when the clot has occluded blood flow and there is ventricular damage. A NSTEMI is seen when there was a clot, but enough blood flow got through, or the patient was treated soon enough, or the patient’s own clot-buster (TPA) started digesting the clot. It also indicates ventricular damage, but maybe to a lesser degree. Most patients are told to chew an aspirin before they hit the ED, and once there, Enoxaparin is thrown in for good measure. But the only drug that will dissolve a formed clot is a drug like TNKase. When the patient is discharged, they leave the hospital on Warfarin or rivaroxaban and sometimes an aspirin a day…or on Clopidogrel and rivaroxaban (or Warfarin) or an aspirin a day. If on Warfarin, the patient will have to have his INR monitored and will have to watch his diet, since Warfarin is a vitamin K antagonist—so eating vitamin K-rich foods (dark leafy greens, nuts, berries) will antagonize the drug. The new anticlotting drugs Pradaxa, Apixaban and Rivaroxaban allow some patients (who fit the criteria for use) to NOT be monitored and to not have to worry about drug-food interactions since they do not affect vitamin K. They still cause BLEEDS as a side effect, though, so patients have to be careful! Pradaxa has a reversing agent. Drugs to prevent clots: warfarin, rivaroxaban, apixaban, heparin, enoxaparin, aspirin, clopidogrel, tenecteplase As for Antidysrhythmic Drugs…make sure you know that beta-blockers (Propranolol), Calcium channel blockers (Verapamil), Quinidine, Amiodarone and Lidocaine may all be used, and that the patient taking these will have to monitor their heart rate and be ADHERENT with meds! Amiodarone is a high alert med for drug interactions. Also, how and when is Adenosine used? Drugs for dysrhythmias: beta blockers, CCBs, quinidine, lidocaine, amiodarone, adenosine For Lipid Management…the statins are the most widely used drugs. Simvastatin and Rosuvastatin are the most popular, as is Atorvastatin. All may cause muscle aches and liver toxicity, so these need to be monitored for. They are unsafe to use in pregnancy. Know how they affect the lipid pattern. Other lipid drugs to know are Gemfibrozil, Fenofibrate, Colesevelam, Ezetemibe. What are the main side effects? What lipids do the statins lower? What about Gemfibrozil and Fenofibrate? Drugs for Lipid Management: atorvastatin, simvastatin, rosuvastatin, fenofibrate, gemfibrozil, colesevelam, ezetimibe Finally, for Anemias, make sure you know how to give iron by the PO route and the Z-track technique! Also review B-12 and folic acid use. Know Epoietin, Filgrastim and Thrombopoietin uses. Drugs for Anemias: iron, B-12, folic acid, epoietin, filgrastim, thrombopoietin Renal Make sure you know the uses of these important drugs—especially Thiazides (Chlorothiazide, Hydrochlorothiazide, Chlorthalidone), Loops (Furosemide, Bumetanide) and potassium sparing diuretics (Amiloride, Spironolactone)…and the few uses of Mannitol. Thiazides are used mostly for BP control and mild edema in early HF….Furosemide for more severe BP issues and more severe HF. The K-sparing diuretics are used as combination drugs with other drugs that make one LOSE potassium (such as the thiazides)…that way the net effect on potassium is zero. Monitoring of electrolytes (especially K) is always important with all of these drugs! Drugs for Renal: chlorothiazide, hydrochlorothiazide, chlorthalidone, furosemide, bumetanide, amiloride, spironolactone, mannitol Respiratory The main use of these drugs is in asthma, though other COPDs use these drugs, too. Their main goal is to ease breathing, and that may be accomplished several ways: They may open up the airways through an action on bronchiolar smooth muscle, they may reduce inflammation, they may reduce the activity of cells that would otherwise get involved in inflammatory processes and remodeling in the lung as part of the disease process. As you study these drugs, learn which of the actions the drugs you are studying has—it will help you to know if the drug you are studying works quickly or more slowly in the lung. The drugs that work quickly give your patient relief NOW….but the ones that work more slowly give her relief in the long run, and prevent potential inflammatory damage to the lung. The most commonly used drugs in asthma and COPDs are the short-acting beta-agonist (SABA) inhalers. Examples are Albuterol (Ventolin) and Levalbuterol (Xopenex). These drugs work quickly as agonists on the Beta-2 receptor to cause relaxation of smooth muscle in the airway, opening it up. A problem that may develop is that the patient may develop tolerance to this kind of drug, so they cannot keep “puffing” on their inhaler and keep expecting it to work! Patients who have more severe asthma are better off using long-acting beta agonists (LABA)—tolerance does not develop as readily, but they do not provide “instant relief”. Salmeterol and Formoterol are examples. To prevent inflammation in the lung that results with an asthma attack, the patient may use a steroid—either inhaled, PO or even IV if the attack is bad enough. Examples include SoluMedrol IV, Prednisone PO, and Budesinide INH, Fluticasone, Mometasone, Beclomethasone. The best choice is an inhaled steroid, and many patients take these either alone or combined with a beta agonist to prevent asthma attacks. An example of a combined product is Fluticasone/Salmeterol (Advair). PO Steroids have tons of side effects so it is never a good idea to keep a patient on them long term. They are usually used as a short course therapy in patients who have severe, recurrent asthma. But…They suppress the immune system, suppress growth, cause high BP, ulcers, personality changes, fat build up, metabolic changes, diabetes, menstrual irregularities, etc., etc., etc….they are nasty drugs! The other choice in antiinflammatory drugs for PO use are leukotriene inhibitors. An example is Montelukast (Singulair). Other inhaled drugs for COPD’ers include Cromolyn, Nedocromil, and anticholinergics like Tiotropium and Ipratropium. None of these drugs works instantly to provide asthma or COPD relief, but over the long haul, they do reduce lung damage due to pathology. Know how to use the drugs for asthma! Newer drugs for asthma are biologics— injectables that are monoclonal antibodies. Omalizumab is an example for allergic asthma. Bevilizumab is for non-allergic asthma. There are a few other drugs in this section. In some COPD patients, drugs such as Theophylline or Aminophylline may be used. Make sure you know who uses these and why. Also, some drugs are used as cough suppressants—including the opioids! This is not a great use for these drugs, however. Finally, antihistamines are used in patients with seasonal allergies. There are 2 classes of these, the sedating kind (like Benedryl) and the non-sedating kind (like Loratidine). Make sure you know the difference between those two! Respiratory Drugs: Albuterol, levalbuterol, salmeterol, formoterol, solumedrol, prednisone, fluticasone, mometasone, beclomethasone, tiotropium, cromolyn, nedocromil, ipratropium, montelukast, omalizumab