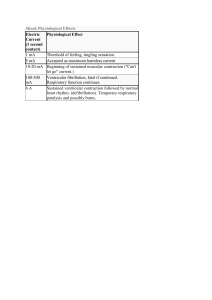
Antiarrhythmic Agents Drug Class MOA Indications Side Effects Quinidine 1A Treatment of acute/chronic SVT, WPW syndrome N&V, Diarrhea Interferes with normal neuromuscular transmission Low therapeutic ratio: heart block, hypotension, proarrhythmia Procainamide 1A Inhibit fast Na+ channels – lengthen the action potential duration & effective refractory period Decreases the slope of phase 4 depolarization Alpha blocking drug Inhibit fast Na+ channels – lengthen the action potential duration & effective refractory period Similar to quinidine – less prolongation of QT interval Decreases the slope of phase 4 depolarization Used in pts with Afib to suppress ventricular irritability Paradoxical vtach Hypotension d/t myocardial depression May provoke a lupus-like syndrome, N/V, & lots of other side effects Disopyramide 1A Inhibit fast Na+ channels – lengthen the action potential duration & effective refractory period Similar to quinidine - Decreases the slope of phase 4 depolarization For suppressing atrial and ventricular tachyarrhythmias Moricizine 1A Treatment of sustained ventricular arrhythmias Lidocaine 1B Suppression of ventricular arrhythmias (reentry, PVCs, vtach) Minimal side effects: in high doses can decrease AV node and His-Purkinje conduction Mexiletine 1B 1B Chronic suppression of ventricular tachyarrhythmias No longer available in US (end of story) Similar to lidocaine – electrophysiologic Tocainide Phenytoin 1B Inhibit fast Na+ channels – lengthen the action potential duration & effective refractory period Decreases the fast inward sodium ion current Decreases automaticity Inhibit fast Na+ channels – shorten the action potential duration and the normal ventricular refractory period Delays rate of phase 4 depolarization Inhibit fast Na+ channels – shorten the action potential duration and the normal ventricular refractory period Inhibit fast Na+ channels – shorten the action potential duration and the normal ventricular refractory period Inhibit fast Na+ channels – shorten the action potential duration and the normal ventricular refractory period MOA is similar to lidocaine (delays rate of phase 4 depolarization) Anticholinergic effects cause dry mouth, urinary hesitancy QT interval prolongation Paradoxical vtach Myocardial depression, hypotension, CHF Proarrhythmic effects occur in 3-15% of patients CNS disturbances: ataxia, nystagmus, vertigo, slurred speech, sedation, confusion Flecainide 1C Effective in suppressing ventricular arrhythmia d/t digitalis toxicity Paradoxical vtach Torsades de Pointes Effective in suppression of VPBs and Vtach Propafenone 1C Effective oral agent for suppression of ventricular/atrial tachyarrhythmias Proarrhythmic in patients with LV dysfunction, preexisting ventricular arrhythmias, or sustained Vtach SE: vertigo, blurred vision, taste disturbances Propranolol Esmolol Metoprolol 2 Effective for reducing the arrhythmias provoked SNS activity (stress, thyrotoxicosis, pheochromocytoma) SE: bradycardia, hypotension, myocardial depression, bronchospasm; Worsening CHF; Potentiation of pre-existing conduction blockade (rebound SVTs) Upregulation of b-adrenergic receptor density CNS side effects: mental depression, fatigue Inhibit fast Na+ channels – potent sodium channel blocker, markedly decreasing the rate of phase 0 depolarization and conduction speed of cardiac impulses Fluorinated local anesthetic analog of procainamide Delays conduction in bypass tracts (WPW) Inhibit fast Na+ channels – potent sodium channel blocker, markedly decreasing the rate of phase 0 depolarization and conduction speed of cardiac impulses Has weak B adrenergic and calcium channel-blocking effects Decrease the rate of spontaneous phase 4 depolarization (↓ ANS activity) Slow the speed of conduction of impulses through cardiac atrial tissues, prolonging the PR interval Proarrhythmic with LV dysfunction Prolongs QRS by 25% or more Amiodarone 3 Inhibit potassium channels (phase 3) – resulting in the prolongation of cardiac myocyte depolarization, action potential duration, and effective refractory period Prolongs the refractory period of all cardiac tissues Exhibits non-competitive blockade of alpha- and beta-receptors Has potent vasodilating properties Dilates coronary arteries and increases coronary blood flow Refractory supraventricular/ventricular tachycardia: Tx of: post-cardiac surgery afib, WPW tachyarrhythmias, decreases mortality after MI **Amio possesses Class I and Class II effects Pulm: toxicity: pulmonary alveolitis (incidence: 5-15%, mortality: 5-15%) may be r/t & accelerated by high FiO2 exposure risk may be increased by CPB *Has a long elimination half time, and a large Vd CV: QTc interval prolongation, bradycardia, decreased responsiveness to SNS activity and catecholamines (blockade of alpha and beta receptors) Potentiation of myocardial depressant effects of GA, alpha and beta blockade, calcium channel blockers Neuro: toxicity – peripheral neuropathy, tremors, sleep disturbances, HA, proximal muscle weakness Nausea, diarrhea Bradycardia, QT prolongation Increased serum creatinine Provokation of Torsades d/t QTc prolongation Dronedarone 3 Noniodinated benzofuran derivative of amiodarone Blocks sodium, potassium, and calcium channels, and sympatholytic effects Indicated for tx of resolved/cardioverted afib/aflutter Sotalol 3 Non-selective BB at low doses Prolongs cardiac AP in the atria, ventricles, and accessory pathways A long-acting BB with L and D isomers Tx of sustained Vtach of Vfib Ibutilide 3 Dofetilide 3 Potent, pure potassium channel-blocking agent Bretylium Verapamil Diltiazem 3 4 No longer available in US Calcium channel blockers (not dihydropyridines) Inhibit slow calcium channels (phase 4) Potent AV node depressant effects and decreases the activity of the SA node Digoxin Oth er Adenosine Oth er Effective for conversion of recent onset afib/flutter to NSR Afib, Aflutter Resolved/Cardioverted Afib/flutter Also prolongs QT interval Highly effective in terminating PSVT (a re-entry tachycardia involving AV node) Provocation of heart block in patients with conduction system decrease Myocardial depression and decreased CO in patients with poor LV function Can enhance conduction through accessory pathways (WPW) increasing the ventricular response rate Transient AV block Bronchospasm – antagonized by methylxanthines (theophylline, caffeine) Tx/prevention of atrial tachyarrhythmias Slows conduction of cardiac impulses through the AV node Electrophysiologic effects resemble verapamil & diltiazem Stimulation of adeonosine1 receptors increases potassium conductance, shortens AP duration, and hyperpolarizes cardiac cell membranes Tx PSVT, WPW Causes dose-dependent prolongation of QTc