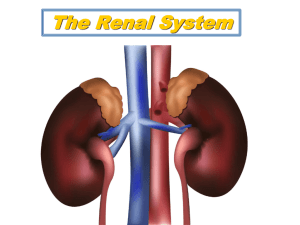
CHAPTER 32: THE URINARY SYSTEM . the main function is of the urinary system is to help maintain homeostasis by controlling the composition, volume & pressure of the blood. it contains 2 kidneys, ureters, 1 bladder and 1 urethra it filters & restores water & solutes to the blood other functions include: a) regulation of blood volume and composition: adjust the fluid volume of blood and therefore regulates the interstitial tissue fluid volume; helps to regulate the Na+, K+ and Ca+, Cl- ions and phosphate in the blood b) maintenance of blood omolarity : by separately regulating loss of water and loss of solutes in uring, the kidneys maintain a constant blood osmolarity close to 290 milliosmoles/L (mOsm/Liter) c) regulation of blood pressure: the kidneys regulate BP via renin-angiotensin pathway d) contributes to metabolism : the kidneys synthesize & secrete erythropoietin ( hormone that promotes RBC production) e) regulation of blood pH : the kidneys excrete H+ into urine and conserve bicarbonate ions to buffer the H+ - this regulates blood pH f) regulation of blood glucose: the kidneys can deaminate the amino acid glutamine used it for gluconeogenesis and release glucose into the blood g) release of hormones: the kidneys release 2 hormones - calcitrol (an active form of vitamin D) which regulates Ca+ homeostasis, and erythropoietin which stimulates the production of RBC’s h) excretion of waste : by forming urine the by-products of metabolism can be excreted (amonia & urea) & creatinine from muscle metabolism and uric acid from catabolism of nucleic acids KIDNEYS: Are paired reddish, kidney bean shaped, retroperitoneal ( behind peritoneum like the adrenals & ureter); they lie at level of T12- L1or 3 Anatomy: 1. each has a hilus thru which the ureter runs out of the organ and the lymph & BV run also; in the hilus is the entrance to the cavity of the renal sinus 2. the organ is divided into cortex & medulla 3. the medulla is divided into 8-15 cone shaped renal pyramids. The base o f the pyramid faces the cortex, the apex faces into the hilus 4. the cortex extends from the capsule to the base of the renal pyramids ; the part that extends between the pyramids is called the renal columns 5. the nephron is the functional unit of the kidney (there are 1 million) and they are found in the cortex & medulla. There numbers are fixed at birth, they don’t regenerate 6. urine that is generated in the nephron goes into papillary ducts --- into cup-like structures called renal calyces ---renal pelvis --- ureter ---bladder Blood supply 1. there is an abundant supply of vessels: the kidney receives 20-25% of resting cardiac output via renal arteries (1.2 L / min) 2. renal arteries ----segmental arteries (there are 5 of these that supplies segments) ---lobular arteries (between pyramids) --interlobular arteries (at the corticomedullary jxn) -- accurate arteries ( run across the top of the pyramids) -----eventually lead to afferent arterioles (each nephron receives ONE afferent arteriole which divides into a ball of capillaries called glomerular capillaries. The capillaries leave the nephron as efferent arterioles 3. efferent arterioles divide and form a network of capillaries called the peritubular capillaries ( they surround the tubules in the renal cortex. They can form vasa recta. ---- they join to form interlobular veins --- arcuate veins ---interlobar veins -- segmental veins ---- renal veins 4. 100% blood volume passes into cortex- <10% goes thru to medulla , and 1% to the papillae. In cases of sock (for example) the blood can be re-directed to the medulla= this doesn’t permit filtration but does maintain urine –cncentrating ability of kidneys Nephron: 1. 2. composed of 2 parts: a renal corpuscle where the blood is filtered & a renal tubule into which the filtrate passes. nephrons have 3 functions : a) filtration; substances in the blood that are small can filter into the tubules b) tubule secretion: c) reabsorption: the tubes can reabsorb anything of use to the body 3. Glomerulus: is a unique HIGH –pressure capillary filtration system located between 2 ARTERIOLES. The afferent arteriole has a larger diameter vs efferent- the afferent has a very high BHP for a capillary which allows easy filtration into BC. Peritubular capillaries arise form efferent arterioles – they are low pressure for absorption - they surround all pts of nephron (but mostly the upper regions around BC) , and rejoin the veins as they leave the kidney. In the Juxta-medullary nephrons, the efferent arterioles continue as VERY long , thin walled looped vessels called vasa rectae which loop around the very long LOH for exchange and reabsorption . By performing these functions, the nephrons maintain homeostasis of the blood. like a recycling plant 4. renal corpuscle: a) they all lie in the cortex & they consist of 2 parts: a glomerulus (capillary network) a glomerular (Bowman’s) capsule b) there relationship is similar to a hand punched into a limp balloon c) Bowman’s capsule consist of a bi-layer of epithelial cells. The outer cells are SSE and are called the parietal layer. The inner layer is the visceral layer , closest to the glomerulus, consisting of modified SSE called podocytes. They stick closely to the glomerulus capillaries & together they form an endothelial--capsular (filtration ) membrane barrier that can act as a filter As the fluid filters out of the capillaries (water & solutes) and the capillaries, filtered substances pass thru 3 layers of membranes: GLOMERULUS: filtrate is formed in the RC which includes BC & glomerulus ; the glomerular basement membrane is made of collagen , mucopolysaccharides and glycoproteins. a) Three layer filtration barrier membranes in the glomerulus includes( from capillary to podocyte consist of; an endothelial fenestrated cell membrane (with pores) a BM of the endothelium slit membranes that pass between the finger-like projections (pedicles) of the podocytes b) the spaces between the podocytes and the BM act as a pore filtering by size preventing RBC, etc from being filtered out while allowing smaller particles, gases, water etc to filter. Alterations in the thickness, structure of the BM is indicative of kidney diseases. No proteins are allowed to filter out. c) MESANGIAL cells- are also present in glomerulus. These are epithelial cells which surround the capillary ehere the endothelium is not complete or where there is little BM. They produce a intercellular substance similar to BM which covers the capillary endothelium . They are phagocytic, cleaning the intercellular space, and respond to neurohormonal substances by exhibiting contractile properties so that they can regulate filtration pressure -0 maybe. In some diseases the mesangial compartment is hyperplastic – see below for intra and extra mesangial cells function The Filtration Membrane: the endothelial cells of the glomerular capillaries and the podocytes that encircle them form the filtration membrane or endothelialcapsular membrane which is a sandwich-like a assembly permitting filtration of water and small solutes, but prevents filtration of proteins, blood cells, platelets. The filtered material moves thru 3 barriers: a) fenestrations of the glomerular endothelial cells = they are leaky and have large pores (70-100 nm) permitting solutes to filter out of blood , but no proteins or cells b) basal lamina = of the endothelial cells is a thin layer of fibers in a glycoprotein matrix that prevents filtration of larger plasma proteins c) filtration slits of the foot-like processes of the podocytes (pedicels) = thousands of foot-like processes (pedicels) wrap around the glomerular capillaries. The spaces between the pedicels are the filtration slits. A thin membrane (slit membrane) extends across the filtration slit & permits the passage of molecules of <6-7nm diameter and water or solutes, very small proteins, ammonia, urea and ions the principle of filtration - is the use of pressure to force fluids and solutes thru a membrane & is the same Starlings law of capillaries. The volume of fluid filtered is larger than in other capillaries : a) because they are ling and extensive, and present a larger surface area for filtration. The amount of surface area available for filtration is regulated by mesangial cells so that when they are relaxed, the surface area is maximal and GFR is high, and when contracted, surface area is reduced and GFR is decreased b) the filtration membrane is thin and porous – despite having several layers of thickness c) glomerular capillary is high – because efferent arterioles are smaller in diameter than afferent arterioles, resistance to the outflow of blood from the glomerulus is high. As a result, BP in glomerular capillaries is higher than in other capillaries and the higher pressure produces more filtrate. 4. renal tubule & ducts: a) from the capsular space the fluid passes to the --- PCT (denotes proximity to glomerulus)/ lie in the cortex ---loop of Henle (nephron loop) which extends into the medulla , loops & returns to cortex ----- DCT (denotes proximity to glomerulus) & lies in the cortex --- single collecting duct CD then -- converge into papillary ducts b) there are millions of nephrons; but fewer collecting ducts & papillary ducts; 1million per kidney which diminishes by 10% per decade after 40yrs . c) the DCT has 2 segments : the diluting segment d) difference between the cortical & juxta-medullary nephrons: lies in the fact that there is a short thick loop of Henle (cortical) and a long loop of Henle (JGN). 85% of nephrons have short loops & 15% have long loops for more urine concentration. The long loops receive blood supply via vasa recta (the long loops enable you to secrete concentrated or dilute urine) 5. histology of the nephron & tubes a) parietal cells are squamous which is better for filtering/ podocytes are modified SSE b) PCT cells are cuboidal with microvilli , like small intestine, they serve absorptive function. -- 65% of water is filtered thru these c) Descending limb of loop of Henle have SSE d) Ascending limb of Loop of Henle have simple cuboidal to low columnar epithelial cells e) Ascending limb of (thick) loop of Henle nearest the afferent arterioles (near the glomerulus) contain e specialized cells called macula densa cells (MD) - they are columnar & crowded near the afferent arteriole cells. They monitor Na+ & Clconcentrations of fluid in the tubule. . f) cells of the afferent arterioles (modified smooth muscle cells) that are nearest the macula densa are specialized , & together with the macula densa cells are called the juxtaglomerular apparatus (JGA). This is a very important region as it regulates the arterial blood pressure and the rate of filtration by the kidneys g) cell of the DCT & collecting ducts are cuboidal with microvilli. Most are principal cells that respond to ADH & aldosterone. A few are intercalated cells which secrete H+, to help balance pH. The CD empty into the papillary ducts which are lined by simple columnar cells. URINE FORMATION : Renal Physiology major work of the urinary system is done by the kidneys & tubules 3 processes are involved in the formation of urine: a) glomerular filtration – 1st step where water and solutes in plasma pass into glomerular capsule which empties into the renal tubules b) tubular reabsorption – where most of the water is reabsorbed by the CD and tubules and the reabsorbed material is returned to blood via the vasa recta c) tubular secretion – the CD and tubules secrete materials into the fluids such as wastes, drugs and excess ions Glomerular Filtration 1. is the amount of filtrate formed in all renal corpuscles of both kidneys each minute urine formation begins with filtration in the Bowman’s capsule, and a lot of fluid free of proteins is extracted from the blood 2. 3. 4. 5. 6. blood pressure forces water & dissolved solutes thru the endothelial-capsular filtration membrane the fluid that enters the capsular space on its way into the tubules is the glomerular filtrate and it has the consistency of plasm without proteins about 150 liters of filtrate is formed in females and 180 L/males; about 178-179 is reabsorbed so only 1-2 liters is excreted/180 filtered, in a healthy person GFR : 125 ml/min or 180 liters/day ( this is 29% of the blood flowing thru the kidneys) the GFR remains high b/c of several anatomical features of the glomerular apparatus; the glomerular filtration pressure is 2-3X higher than in other cap beds, allowing for consistent filtering of blood. The high GFR is regulated in part by afferent & efferent arterioles. CONSTRICTION of the EFFERENT arterioles, increases resistance pressure and thereby increases GFR . CONSTRICTION of the AFFERENT arterioles- causes reduction in RBF an, glomerular filtration pressure and GFR. homeostasis of body fluids requires that the kidneys maintain a relatively constant GFR (too low, waste accumulates; too high = too much is excreted) The Net Filtration Pressure 1) is the total pressure that promotes filtration 2) it consist of one pressure that promotes filtration (GBHP) and 2 that oppose filtration (CHP & BCOP) GBHP : is glomerular blood hydrostatic pressure; it pushes water from the blood – capsule. It is high b/c of capillary blood pressure CHP: is capsular hydrostatic pressure; is backpressure that opposes filtration; it is caused when new filtrate hits wall of capsule space & runs into fluid already in the capsule BCOP: blood colloid osmotic pressure; is back-pressure that opposes filtration; it is mainly due to the presence of proteins (albumins & globulins) in the blood, that can’t pass thru the filter NFP == GBHP - (CHP - BCOP) 55mg Hg –15mm Hg-30mmHg 10 mmHg This means that a pressure of only 10mm Hg causes a normal amount of plasma to filter from the glomerulus into the capsular space TUBULAR REABSORPTION & TUBULAR SECRETION: Principles of tubular reabsorption & secretion: a) normal GFR is so high that within ½ hr the amount of fluid entering the PCT is equal to the total plasma volume b) under normal condition, ~ 1ml of filtered fluid from the 125ml/min ends up as urine = 60m/hr produced c) 99% of the glomerular filtrate is reabsorbed via the tubules in a process called tubular reabsorption (2nd unction of the nephron & tubules) d) epithelial cells of the tubules reabsorb with the PCT carrying out most of this function d) in this process, water and solutes move from the tubule lumen back into the blood within the peritubular capillaries and vasa recta. e) solutes move by both active & passive transport processes. The solutes include glucose, amino acids, urea, ions (Na+, K+, Ca+, HCO3, & HPO4); all but urea are mostly reabsorbed. ; water is reabsorbed via osmosis (gradient concentrations); proteins and small peptides are reabsorbed via pinocytosis reabsorption routes: 1) substances move either between cells or thru the tubule cells 2) paracellular reabsorption is a passive process whereby tubular fluid can “leak” between the cells in spite the presence of tight junctions at the apical border of the cells. In some parts of the tubes, it accounts for 50% of reabsorbed ions & water 3) in transcellular reabsorption, a substance passes from the fluid in the tube lumen thru the apical border of the cell across the cytosol, and out into the interstitial fluid at the basolateral side of the cell Transport mechanisms: 1) primary active transport - is the process of moving substances against the gradient splitting ATP’s. The activity of the Na+/K+/ ATPase pump ensures that Na+ ions are pumped out of the cell to keep the cytosolic levels low. To maintain this pump in the kidneys, 6% of total ATPs consumed are used (same amount as it takes to run diaphragm for breathing at rest) 2) secondary active transport - uses energy stored in an ion’s electrochemical gradient (not ATP lysis) to drive another substance across the membrane. This process couples the “downhill” movement of an ion along its electrochemcial gradient, to the “uphill” movement of a 2nd substance against its electrochemical gradient. 3) The membrane proteins that carry out 2nd transport are called symporters when they move >2 substances in same direction, and antiporters when they move >2 substances in opposite directions across a membrane. 4) Water absorption is via osmosis in the tubules & CD. 90% of filtered water occurs with the with the reabsorption of Na+ & Cl- and glucose and is termed obligatory water reabsorption (water is “obliged” to follow the solutes that are absorbed), and this occurs in the PCT & descending loop of Henle b/c these are ALWAYS permeable to water. The other 10% is absorbed by facultative water reabsorption in the CD because of regulation by antidiuretic hormones (adapting to a need). Reabsorption in the PCT 65 % pf all reabsorption occurs here ; most solute & water if reabsorbed here and most processes involve Na+. Two different types of Na+ transporters are found in the PCT : (1) different Na+ symporters (2) Na+/H+ anti-porters effect Na+ reabsorption in exchange for H+ secretion a) the Na+ symporters promote reabsorption of 100% of the filtered glucose and amino acids; 80-90% HCO3 and 65% water, Na+, K+ ; 50% of the Cl- and urea, variable amounts of Ca+, Mg+ – bulk reabsorption occurs here. Na+-glucose symporters in the apical membrane of the PCT cells absorb 2Na+ and 1 glucose molecules and carries them into the cell. Glucose leaves the cell at the basolateral membrane side via facilitated diffusion and diffuses into the peritubular capillaries. Other Na+ symporters reclaim Phosphate, amino acids and lactic acids b) many substances (glucose , a.a.) freely filtered in glomerulus are reabsorbed by ATP –dependent co-transporters . The maximum amount of a substance that these transport systems can reabsorb is called the transport maximum – it is related to the number of carrier proteins that are available & is usually sufficient to reabsorb all of the filtered substances. The plasma level at which a substance appears in the urine is called the reanl threshold . Under some circumstances, the am’t of substance filtered in the glomerulus exceeds the Tm. (when gluc levels are high in uncontrolled DM- the am’t of glc filtered exceeds the Tm (!320mg/min) and gluc spills into urine) d) Na+/H+ antiporters filter Na+ down the gradient into the PCT (reabsorbed) cell in exchange for H+ secreted into urine. PCT cells MUST continually produce H+ ions to keep the antiporters running. e) Production of H+ ions = CO2 diffuses from blood or tube fluid or is produced by metabolic reactions within PCT cells. In the presence of CA (carbonic anhydrase) in the cells, CO2 combines with H2O to form carbonic acid (H 2CO3 ) which dissociates into H+ + HCO3- (bicarbonate) f) Reabsorption of bicarbonate = after H+ is secreted into filtrate (80-90%) of it combines with filtered HCO3- from the blood to form carbonic acid (H2CO3) which dissociates into CO2 & H2O (CO2 enters into the cell to form bicarbonate and generate H+ ions). CA is present in the brush border of the PCT cells. As HCO3- levels rise in the cell, it leaves cells via facilitated diffusion and goes into the blood together with Na+ g) Passive reabsorption of Cl-, K+, Ca+, Mg+, urea & water = in the 2nd ½ of the PCT, electrochemical gradients of these ions exist and promote passive diffusion into the peritubular capillaries h) Reabsorption of Water via osmosis = reabsorption of Na+ and other solutes promotes the reabsorption of water via osmosis. Reabsorption of the solutes raises the osmolarity of the urine promoting reabsorption of water to restore osmotic balance. Cells lining the PCT & descending loop have molecules of aquaporin-1, a membrane protein that functions as a water channel, making these parts permeable to water I) Secretion of NH3 and NH4+ in the PCT: ammonia (NH3) is derived from deamination (amino group removal) from proteins in the liver, and most is converted to urea (less toxic). Both are released in sweat, but most is excreted by PCT PCT cells produce additional ammonia by deaminating glutamine in a reaction that generates NH+3 and HCO-3. Most of the NH+3 (ammonia) converts quickly into ammonium ion (NH4+) which can substitute for H+ in the Na+/H+ antiporters and be excreted. Ammonia production and secretion increases during acidosis (<7.35) increasing blood HCO3which raises blood pH. The opposite is true in aklalosis (>7.45). The PCT also secretes penicillin, aspirin and morphine ; but many of these are protein bound in blood so not filtered so this is only a fraction of the circulating drugs eliminated this way Reabsorption in the Loop of Henle: 1) The fluid entering this section (flow rate of 45 ml/min) is different than plasma or glomerular filtrate, however the osmolarity is the same b/c of osmosis of water keeping up with solute effusion 2 ) 20- 30% of the Na+ & K + & 10% of HCO-3 & 35% of Cl- is reabsorbed in the LOH; 15% of filtered water; here for the 1st time reabsorption of water via osmosis isn’t coupled to reabsorption of filtered solutes; so here in the LOH the stage is set for the independent regulation of both volume and osmolarity of body fluids 1) Na+-K+-2Cl- symporters are present in the apical part of the thick ascending limb of LOH & they reclaim 1Na+, 1K+ and 2Cl- ions simultaneously from the tubular fluid. Na+ is actively transported into the interstitial fluid at the base of the cells and passively diffuses into the vasa recta. Cl- diffuses thru leakage channels in the base of the cell and then into the vasa recta . K+ leaks BACK into the tubular fluid by diffusion, thru leakage channels returning to the urine. 2) The ascending limb of LOH is impermeable to water so the 15% of water absorb here is in the descending limb . 3) The osmolarity of the fluid progressively increases as it flows along the ascending limb on the way out of the kidney 4) It is HERE that urine is concentrate din the longest LOH (see below) Reabsorption in the DCT : 1) fluid entering here flows @ 25 mL/min has 80% of the water filtered out of it and reabsorbed 2) in the DCT, Na+-Cl- symporters continue to reabsorb Na+ & Cl- which exit the tubule cells in the base of the cells via leakage channels and enter into the peritubular capillaries 3) two hormones act on the principle cells in the distal end of the DCT & the CT to reabsorb the remaining water and solutes and this represents the fine tuning absorption: these are: a) Aldosterone = secreted by the adrenal cortex (z.gl.) ; affects the principle cells and the CT to increase Na+ & water reabsorption & K+ secretion into urine ; the PCs increase the number of Na+ pump proteins inserted into the cell membrane and increase the activity of existing Na+ pumps and leakage channels in response to aldosterone. If aldosterone is low, less Na+ is reabsorbed , and less K+ is secreted into urine causing blood K+ levels to rise which can bring on cardiac rhythm disturbances b) ADH = produced by the post. Pituitary in response to stimulus from the hypothalamus; affects the P cells and the CT so that the tube is more permeable to water, so more is absorbed ; when ADH is low up to 400-500 mls of urine can be excreted=dehydration, diabetes insipidus Rabsorption & Secretion in the Collecting Ducts: 1) in the DCT 90% of water and solutes have been reabsorbed 2) principle cells in the DCT absorb Na+ & secrete K+ a) Na+ passes into the principle cells here via leakage channels and the cytosolic Na+ concentration remains low b/c of Na+/K+ pumps across the basolateral membrane. Na+ passes by diffusion into the peritubular capillaries 3) K+ secretion = to adjust for varying dietary K+ levels and to maintain a stable level of K+ in body fluids, PC secrete a variable amount of K+ into urine. The amount of K+ secreted into urine is increased by: a) High K+ plasma levels which stimulates aldosterone release b) Increased plasma aldosterone which stimulates PC to secrete more K+ into urine c) Increased delivery of Na+ - high Na+ in fluid delivered to CD increases rate of Na+ absorption and K+ secretion 4) Intercalated cells reabsorb K+ & HCO3- and secrete H+: a) these cells have proton pumps (H+ATPase) in the apical part of the cell so that they secrete H+ into the fluid even against a concentration gradient, so that urine can be 1000X more acidic than blood. The H+ can be buffered in the urine by combining with ammonia to become ammonium ion (NH+4). The intercalated cells do this when the pH of body fluids is too low b) when body fluid pH is too high, HCO3- is excreted PRODUCTION OF DILUTE OR CONCENTRATED URINE: Overall a persons fluid intake can vary, but the total volume of body fluid is a constant and this homeostasis depends on the ability of the kidney to regulate the rate of water loss in urine. The body produces dilute urine in the face of fluid excess and concentrated urine in the face of reduced intake of water. Formation of Diluted Urine: 1) GFR has the same osmolarity as blood (300mOsm/L). In the tubules, the osmolarity of urine INCREASES as it flows DOWN the descending LOH, and DECREASES as it flows UP the ascending LOH and thru the rest of tubes. 2) these changes are the result of the following: a) b/c osmolarity of the interstitial fluid of the medulla becomes progressively GREATER (due to the countercurrent mechanism) – so more water is reabsorbed along the descending LOH (urine has more solutes in it) b) cells of the thick ascending LOH have symporters that ACTIVELY transport Na+, K+ & Cl- OUT of the tubes into the interstitial space (then into the blood), making the urine more osmolar c) water permeability in the thick ascending LOH is NON-EXISTANT , so water can’t follow the reabsorbed ions, and the urine remains diluted d) in the DCT, more solutes are absorbed without the obligatory reabsorption of water e) without ADH, the cells of the DCT are not permeable to water and the urine continues to become MORE dilute as it moves along so that by the time it drains into the renal pelvis it is 65-70 mOsm/L (4X more dilute than plasma or GFR) Formation of Concentrated Urine: LOH and CD 1) when water intake is low or loss is high, the kidney is under the influence of ADH and produces urine 4X more concentrated that plasma or GFR (1200mOsm/L) 2) the ability of ADH to concentrate urine depends on the presence of an osmotic gradient of solutes in the INTERSTITIAL FLUID OF THE RENAL MEDULLA (especially around the juxtamedullary nephrons) 3) the interstitial fluid increases from 300-1200 at the tip of the LOH b/c of excess Na+, K+, Cl- & urea 4) 2 factors contribute to the formation & maintenance of this osmotic gradient: a) differences in solute & water permeability of the LONG LOH and CD b) the countercurrent flow of fluid in the descending and ascending LOH 5) production of concentrated urine occurs as follows: a) in ling-loop nephrons, symporters in the thick ASCENDING LOH establish the osmotic gradient in the renal medulla by reabsorbing Na+,K+ & Cl- from tubes increasing the osmolarity of the interstitial fluid of the medulla b) cells in the CD reabsorb more water and urea b/c ADH increases the water permeability of the principle cells in this tube area, so water moves via osmosis into the interstitium , then into the vasa recta. With water loss, urea left behind in the urine makes the urine more solute concentrated till it reaches the CD c) urea recycling causes a buildup of urea in the medulla : urea (and water in the presence of ADH) leaves urine in the CD (permeable to urea) and is “recycled” back into urine in the descending and thin ascending limbs of LOH which are permeable to urea. This leads to repeat transfer of urea between segments of the tubes and interstitium called urea recycling . In this way, reabsorption of water from the urine of the ducts(under ADH) promotes the buildup of urea in the interstitial fluid of the medulla, which in turn promotes water reabsorption. 6) the 2nd contributor to the osmotic gradient in the medulla is the countercurrent mechanism, which occurs b/c of the anatomical loop in the tubules of the juxtamedullar nephrons. a) the fluid in the ascending and descending limbs of LOH, move the fluid in opposite directions or counter to each other. – countercurrent flow b) the descending limb IS permeable to water (osmosis), but not solutes EXCEPT urea so the fluid here becomes increasingly more concentrated (1200mOsm/L at the tip). c) In the ascending limb, Na+ -Cl- transporters reabsorb these ions from the urine, but NOT water so the osmolarity of the fluid decreases BUT the reabsorbed ions make the interstitial fluid MORE osmolar establishing and maintaining the gradient in the renal medulla d) OVERALL the fluid becomes progressively MORE CONCENTRATED as it flows along the descending limb, and progressively MORE DILUTE as it moves along the ascending limb. e) the vasa recta also consist of descending & ascending limbs parallel to the limbs of LOH, and blood flows in the opposite directions in these limbs. The osmolarity of the blood entering the limbs = 300mOsm/L as it flows along descending part , ions (Na+,Cl- & urea) from the osmotically high interstitium flows into the blood. Now the blood osmolarity increases as the blood flows into ascending part of vasa recta; the blood flows thru region of interstitium that is less osmotically high, so the ions and urea diffuse from the blood to the interstitium , and reabsorbed water diffuses from the interstitial fluid into the vasa b/c blood leaving and then reentering the cortex via the vasa recta has the same solute concentration , the vasa recta acts as countercurrent exchanger – this system does not create the medullary gradient (that is set up by the LOH), but it does protect it by preventing rapid removal of salt from the medullary interstitial space Regulation of RBF: The mechanisms that regulate GFR operate in 2 main ways (1) by adjusting blood flow into & out of the glomerulus (2) by altering the glomerular capillary surface area available for filtration Coordinated control of the diameter of both the afferent & efferent regulates glomerular blood flow 3 mechanisms control GFR: renal autoregulation, neuronal , hormonal regulation Neural regulation of RBF/GFR: a) the kidney capillaries are supplied with sympathetic ANS fibers that release Norepinephrine causing vasoconstriction thru activation of alpha receptors (plentiful in afferent arterioles) b) with sympathetic stimulation (during exercise or hemorrhage) blood flow is diminished & GFR drops. This has 2 consequences: (1) reduces urine output conserving blood volume (2) permits greater blood flow to other tissue ; this stimulation stimulates release of rennin from JGA cells which accelerates production of AGII c) in shock there can be intense sympathetic stimulation to reduce RBF to zero and GFR also d) other vasoconstrictors : AGII, ADH & endothelins (released from damaged endothelial cells and tissues) In post ischemic acute renal failure ET-I can be very potent vasoconstrictor in kidneys; e) VASODILATORS: NO, dopamine PG E & I2; chronic use NSAIDS (inhibitors PG) can cause reduction in RBF and GFR& are used cautiously with hypertensive or kidney disease persons Hormonal regulation of RBF/ GFR: a) AG II - reduces GFR – it is a potent vasoconstrictor that works on afferent & efferent arterioles and reduces blood flow decreasing GFR b) antrial natriuretic peptide (ANP) -increases GFR . It is secreted by the atrial cells in heart and its release is triggered by the stretching of the heart (blood volume increases). It causes relaxation of glomerular mesangial cells, and increases capillary surface area which increases GFR Renal autoregulation: control of RBF/GFR the kidneys themselves maintain a constant blood flow & GFR despite normal changes in systemic BP (during exercise) & this is called renal autoregulation. It consist of 2 mechanisms: a) myogenic mechanism – part of the job of the JG cells is to sense when stretch of arteriole in high BP (which leads to high GFR) or the opposite – trigger contraction/ relaxation of smooth muscle cells in the afferent arterioles - bringing GFR to normal levels. This mechanisms normalizes RBF and GFR in seconds after BP changes. b) The Juxtaglomerular CXOmplex: Tubuloglomerular feedback – is provided by the macula densa cells of the DCT, as it passes back to the glomerulus. When GFR is above normal (elevated BP) filtered fluid flows more rapidly, and less ions are reabsorbed. The macula cells sense the increased Na+ / Cl-, This info is used to determine how much renin should be released to keep arterial blood pressure within normal limits and a constant GFR. IT is thought that a deceases in GFR slows the flow rate of urine thru tubules, so in the ascending LOH, there can be more time to reabsorb Na+/Cl, which in turn delivers more back into the blood, nd less in the filtrate arriving at the MD region . A decrease in delivery of Na/Cl to MD cells does the following : (1) it decreases resistance in afferent arterioles (which raises GFR (2) increase the release of renin form JG cells . RENIN : serves to convert angiotensinogen --- AGI --- AGII (a potent constrictor of efferent arterioles increasing GFR. This mechanism operates more slowly than the myogenic mechanism. Effect of Increased Protein & /or Glucose load 1) Glucosuria= is used to describe urea with >200mg/dL glucose. The kidneys can’t work fast enough to reabsorb the glucose that enters the filtrate so glucose remains in urine. The most common cause is DM so blood glucose rises above normal. Rare genetic mutations in renal Na+-glucose symport can cause this also 2) RBF & GFR can increase /decrease depending on diet thru mechanisms unkn. IT is thought that after a HIGH protein meal RBF increases (20-30% within 2hrs) : it is thought that since Na+ / & aa are absorbed together there is less Na+ reaching the MD cells, so there is a negative feedback reflex o (JG mechanism) f increasing RBF & GFR – this would allow Na+ excretion to be maintained near normal levels while increasing the excretion of waste production of protein waste – like urea from protein metabolism . It appears to be the same with HIGH glucose levels in DM HORMONAL REGULATION OD TUBULAR REABSORPTION & SECRETION Renin-Angiotensin-Aldosterone System: AG II affects renal physiology in 4 ways 1) it increases GFR by vasoconstriction afferent arterioles 2) it enhances reabsorption of Na+, Cl- and water in the PCT by stimulation activity of Na+/H+ antiporters 3) it stimulates adrenal cortex to release aldosterone which in turn stimulates principle cells (CD) to reabsorb more Na+ + Cl-, so that the osmotic consequence of excreting less Na+ & Cl- is excreting less water, which increases blood volume a) this system is triggered by drop in BP (due to drop in blood volume) so there is less stretch in afferent arterioles. The JG cells release renin which clips off 10-a.a. from AG-I (made in liver). By clipping 2-more a.a. from AG-I , ACE (angiotensin converting enzyme) converts AGI (inactive) into AG-II (Active hormone) Antidiuretic Hormone: ADH or vasopressin regulates facultative water reabsorption by increasing water permeability of principle cells (CD)ADH stimulates the insertion of the aquaporin –2 – containing vesicles into the apical membranes (these are water channel proteins). As a result water permeability increases. The absorbed water moves into the blood via the basolateral membrane surface. When ADH declines, the aquaporin-2 are removed from the membranes via endocytosis and more dilute urine is excreted. A negative feedback system involving ADH regulates water resorption so that when osmolarity or osmotic pressure of the plasma or interstitial fluid increases (water decreases) by as little as 1%, osmoreceptors in the hypothalamus detect the change, and ADH is released. In the absence of AHD, DI results and the patient can excrete 20L urine/day EVALUATION OF KIDNEY FUNCTION: Renal Plasma Clearance: a) is the volume of blood that is “cleaned” or cleared of a substance per unit of time, expressed in mL/ min. High renal clearance indicated efficient excretion of a substance and the reverse is true. Clearance of glucose is normally = 0 b/c it isn’t secreted; In drug therapy, knowing renal clearance is necessary for pharmacokinetics & for determining correct dosage. a) clearance depends on: (1) glomerular filtration (2) tubular reabsorption (3) tubular secretion b) if clearance is high like in penicillin, dosage must be high and it must be given several times/day to maintain therapeutic levels to calculate clearance : renal clearance of substance S= U X V P U & P are the conc. Of substance in urine & plasma & V = urine flow rate in mL/min c) the clearance for creaatinine = GF b/c it is neither reabsorbed CC= 120-140 mL/min. is the easiest way to measure GFR d) clearance of inulin: injected polysaccharide inulin is filtered & not reabsorbed so it is cleared . the am’t of inulin in urine = amount filtered in glomeruli (clearance rate = GFR) so used as a measure of GFR- but time consuming ; maybe in neonates, geriatrics Regulation of Electrolytes: elimination of K+: K+ is filtered, reabsorbed and then secreted as needed into tubular filtrate (DCT)- regulated by aldosterone. Any excess dietary K+ not filtered must be nonetheless secreted into tubular filtrate elimination of Na+ : Na+ is filtered then reabsorbed in the DCT & CD in response to aldosterone (urine can become almost Na+free) elimination of Uric acid – uric acid a product of nucleic acid metabolism is high in tissue fo gout patients, and high in kidney in patients with kidney stones. Uric acid is freely filtered , then reabsorbed but secreted in PCT. The reabsorption /secretion balance is homeostaticly balanced to maintain constant plasma levels elimination of Urea: urea produced in liver by protein metabolism is entirely eliminated in urine-- (25-30 g/day) range eliminated. The kidneys regulated BUN (blood urea nitrogen) levels in range of 8-25 mg/dL – with dehydration, the blood volume and GFR decrease while the BUN increases. They occur inversely like this ---- Blood urea also rises with GI bleed (gut flora turn blood into ammonia) which returns to liver to be converted into blood urea. If GFR is high then only small amounts of urea are reabsorbed into the blood elimination of drugs- only drugs not bound to proteins carried in blood are eliminated by kidney. Thiazide and loop diuretics (furosemide) can cause hyperuricemia and gout thr a decrease in ex fluid and enhanced uric acid reabsorption . Atrial Natriuretic Peptide: these are peptides secreted by the heart in response to cardiac muscle fiber stretching. A large increase in blood volume promotes release of ANP. It functions to inhibit Na+ & water reabsorption in the PCT & CD and suppresses aldosterone & ADH. Natriuresis or increased urination results. ANP can also disrupt the RAA system further decreasing Na+ resorption. Regulation of pH Kidneys regulate pH by conserving HC)3- and secretion of H+ via the tubular secretory mechanisms - tubular fluid can get to ph 44.5. 3 major buffering systems can be used to facilitate safely H+: a) The bicarbonate buffer system : HCO3- + H+ in the renal tubes == carbonic acid which dissociates to CO2 & H20 – the CO2 is then reabsorbed into the tubular cells and HCO3-is regenerated inside the tube cells via carbonic anhydrase b) Phosphate buffer system: PO4 + H+ --- NaH2PO4 ; NaHPO3 +H+ = NAH2PO4 secreted c) Ammonia buffering system – Ammonia made in tubular cells by deamination of glutamine (from liver) diffuses into tubules, joins with H+ and then is secreted ENDOCRINE FUNCTIONS OF KIDNEY RAA mechanism renin released b/c low RBF or ionic compositional change in DCT urine detected ; AG II potent vasoconstrictor Erythropoietin – is a glycoprotein produced by Fb in kidney interstitium – regulates the prod of RBCs in Bone marrow. It is stimulated by hypoxia b/c of anemia, high altitudes, impaired cardiac fxn; ESRD persons are anemic b/c of inability to produce EPO Vitamin D- increases Ca+ absorption from GI to deposit in bone; a) 2 forms exist : natural vit D (cholecalciferol) made in skin from activation by UV and synthetic vit D (ergosterol) b) the active form is 1, 25 dihydroxycholecalciferol – both forms must undergo activation to active form in liver then in kidneys; ESRD patients have low levels of vit D and must be supplemented. Diuretics a) are substances that slow renal reabsorption of water and cause diuresis, an elevated urine flow rate. Caffeine is a natural diuretic that inhibits Na+ reabsorption. Alcohol, inhibits secretion of ADH. Loop diuretics (furosamide (Lasix)) selectively inhibit the Na+-K+ -Cl- symporters in the thick ascending LOH. The thiazide diuretics (chlorthiazide (Diuril), act in the DCT by inhibiting Na+-Cl- symporters. BOCK Na+ reabsorption - by blocking Na+ resorption = create osmotic gradient that prevents H2O absorption also Those that act early in nephron tube system = prevent greatest Na+ resorption (65% Na+ reabsorb in PCT; 20% in thick asc. LOH; 10% in early DCT ; 5 % in late DCT or DC) Early loop diuretics are the most effective (act on thick ascending) by inhibiting the Na+/K+/2Cl- transporters –they reduce Na+ & K+ reabsorption but increase Ca+ & Mg+ elimination - Prolonged use of loop diuretics can lead to significant loss of Mg+ but they don’t cause hypocalcemia (b/c of the active resorption of Ca+) - They CAN increase uric acid retention and impair gluc tolerance Thiazide diuretics - prevent Na+ reabsorb in early DCT so are less effective ; do increase K+ loss and can enhance Ca+ reabsorption also Aldosterone antagonist- (K+ sparing diuretics) – reduce Na+ reabsorption and decrease K+ secretion in the late DCT & DC regulated by aldosterone …H+ secretion is linked to K+ reabsorp ( Activity of the H+- K+-ATPase, which couples K+ reabsorption to H+ secretion in intercalated cells, …) these agents interfere with secretion of H+ = metabolic acidosis . these are mild diuretics and are use din combo with other diuretics - They act directly on the aldosterone binding site (spironolactone) preventing aldosterone from entering the tube cell and exerting effects - They act (triamterene) indirectly on the Na+ select channels Osmotic Diuretics – these act on the PCT and ascend LOH – highly permeable to H2O, cause water to be retained in filtrate and promote water diuresis . Mannitol (used to reduce ICP) can be sued to promote diuresis in toxic poisoning; must be given IV or IM ; if given orally can cause osmotic diuresis TEST of RENAL FUNCTION URINALYSIS: 1) 2) 3) 4) volume = 1-2L/day characteristics listed in chart no protein found in urine specific gravity (density) is the ratio of wgt of volume of a substance to the wgt. Of an equal volume of water. It ranges form dilute (1.001) to more dense (1.035) which is higher sg. During marked hydration periods, sp gravity ~ 1.000. The normal ratio between serum and urine osmolarity is 1:3 a high urine to serum ratio is see in conc. Urine 5) Presence of cast (molds of DCT lumen - gel like substance called Tamm _ Horsfall microprotein - formed in tubular epithelium is the protein constituent of casts. (if cast don’t have this proteins they are called – hyaline casts). They develop when protein conc. Is too high in urine (nephrotic syndrome) or when pH urine is too low. The inclusion of cells, or granules promotes formation of other types of casts. 6) Proteinuria – excessive protein excretion . in normal urine ~150mg/L in 1 day is excreted. A urine dip stick detects more than this 7) Albuminuria – (microalbuminuria) indicates a small amount of this smaller plasma protein in urine (<25mg/day is normal ) . Once detected , a 24 hr urine specimen must be taken to quantitate. Glomerular Filtration Rate: GFR is the amount of filtrate formed in ALL the renal corpuscles of both kidneys/min 1) 2) 3) 4) in adults, the GFR = 125 mL/min. in males and 105 mL in females if GFR is too high, needed substances may pass too quickly thru renal tubules and are not reabsorbed, but lost in urine. If GFR is too low, nearly all filtrate will be reabsorbed and waste will be reabsorbed also GFR is directly related to pressures that determine net filtration pressure so any change in NFP will affect GFR; Filtration ceases if GBHP < 44 mm Hg b/c the opposing forces add up to this value. 5) GFR is constant even when the MABP is between 90-180 mmHg Creatinine Clearance (CC)- produced by muscles a by prod of metabolism and its formation and release is constant & proportional to muscle mass. It is freely filtered but NOT reabsorbed (and not secreted directly into tubes from blood). Its blood value is directed by GFR!. The comparison of blood & urine levels provides a good GFR measurement. - Clearance rate for creatinine = c= UV/P (in a minute) (c= clearance rate mL/min ) , U = urine conc , V = urine volume , P = plasma conc. - Normal CC levels 115-125ml/min (corrected for body mass, muscle mass etc) - Test done in 24 hr basis with blood creatinine level drawn at the completion of the 24 hrs urine collection - eGFR = estimated GFR is what most labs report in the formula accounting for age, sex and race- which reflects that CC is less of a good measure of GFR in some populations b/c of differences in muscle mass Cystatin (cyst- atin) C- has been demonstrated to serve as a marker for GFR b/ c it is filtered in the glomerulus and is stable in amt across the population . formulas combining both markers is being developed. Blood Test: to evaluate kidney function BUN = test for blood urea nitrogen resulting from catabolism and deamination of amino acids. When GFR decreases (obstruction, disease) BUN rises. Minimizing protein intake can help reduce this. BUN levels are related to GFR bUT are influenced by protein intake, hydration and GI bleeding (2/3 of renal fxn still barley change the BUN levels) . The BUN –creatinine ratio may be useful Serum Creatinine – a normal serum creatinine usually indicate normal renal fxn; it is used to indicate the functional capacity of kidneys (if the value doubles then GFR probably has fallen to ½ of normal state; a rise in serum creatinine to 3x normal suggest 75% loss of renal fxn and a creatinine ~10mg/dl = 90% loss of renal fxn ) ; normal runs from 0.7mhdL for small frame women to 1.0 -1.5 mg/dl for normal or muscular man