FloTrac System: Stroke Volume Measurement & Fluid Loading Assessment
advertisement

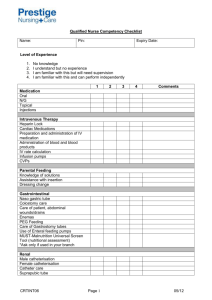
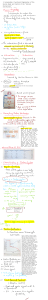
The FloTract System— Measurement of Stroke Volume and the Assessment of Dynamic Fluid Loading Brian Hashim, MD Adam B. Lerner, MD Beth Israel Deaconess Medical Center Boston, Massachusetts The FloTrac system was introduced in the United States by Edwards Lifesciences of Irvine, CA in April of 2005. As with other potentially competing systems which are discussed elsewhere within this publication, namely PiCCO and LiDCO, this system has been marketed as a device that can provide accurate and reliable measurements of cardiac output (CO) in a continuous fashion as well as calculations of systemic vascular resistance (SVR) and the dynamic parameter of stroke volume variation (SVV) (FloTrac System Brochure, Edwards Lifesciences, 2007). SVV, important for its ability to predict fluid responsiveness, is also discussed in detail elsewhere within this publication. The heart and soul of the FloTrac system is a proprietary software algorithm that analyzes characteristics of the arterial pressure waveform and uses this analysis along with patient-specific demographic information to determine blood flow. Obviously, not all elements of this algorithm have been revealed by Edwards Lifesciences so as to protect their product from competitors. However, the foundation of this algorithm has been made available by them and can be summarized as follows. (Case Study—‘‘Getting ml/beat from mmHg’’ Arterial REPRINTS: ADAM B. LERNER MD, DEPARTMENT OF ANESTHESIA, CRITICAL CARE, AND PAIN MEDICINE, BETH ISRAEL DEACONESS MEDICAL CENTER, 1 DEACONESS ROAD CC470, BOSTON, MA 02215; E-MAIL: ALERNER@ BIDMC.HARVARD.EDU INTERNATIONAL ANESTHESIOLOGY CLINICS Volume 48, Number 1, 45–56 r 2010, Lippincott Williams & Wilkins www.anesthesiaclinics.com | 45 46 ’ Hashim and Lerner Pressure-based Cardiac Output, The Edwards FloTrac Algorithm, Edwards Lifesciences, 2008.) Starting with CO = heart rate (HR) stroke volume (SV), the system first uses the arterial trace to determine a pulse rate (PR) calculated by counting the number of pulsations in 20 seconds. Though PR represents only perfused cardiac beats and therefore is not always equivalent to HR, the algorithm modifies the equation to CO = PR SV. This modification can become important when comparing SV measurements derived from other techniques, such as thermodilution, when HR and PR may diverge. For this reason, and because of their impact on the arterial waveform itself, persistent dysrhythmias can have significant impact on the accuracy of FloTrac-derived data. In these settings, the FloTrac system-derived measurements should probably not be used to make clinical decisions. For the determination of SV, the algorithm uses the following equation: SV = the standard deviation of the arterial pressure (sAP) chi (w). The standard deviation of the arterial pressure (sAP) is practically related and proportional to pulse pressure and to SV. The sAP around the mean arterial pressure (MAP) is used in an attempt to eliminate the effects of changes in vascular tone. The sAP is then used to determine the standard deviation of the pulse pressure as this is directly proportional to SV. Changes in sAP also provide information on the amplitude of the pressure waveform. When this amplitude information is put into the context of the kurtosis of the waveform, that is, the concentration of the waveform about the mean pressure or the distinctness of the peak, it allows for an attenuation of the impact of pressure wave reflectance and differences in arterial compliance between different arterial sites. (Fig. 1) This is what allows for the potential use of any arterial cannulation site in the FloTrac algorithm. In the current version of the FloTrac algorithm, version 1.10, sAP is calculated after 20 seconds of waveform retrieval are analyzed at 100 times per second (2,000 generated data points). One of the most essential components of the algorithm is w. It is a proprietary polynomial equation that relates the impact of vascular tone on pulse pressure. The variables used to determine w are PR, sAP, MAP, and an estimate of arterial compliance based on patient demographics such as body surface area, age, sex, and on the shape of the arterial waveform. When referring to shape, the algorithm specifically analyzes the kurtosis, described above, and skewness, or lack of symmetry, inherent in the waveform. These characteristics of overall shape are directly related to the resistance and compliance of the arterial tree. (Fig. 1) The ‘‘rough’’ FloTrac algorithm estimates of aortic compliance are based on the work carried out by Langewouters et al.1,2 Using cadavers, Langewouters et al were able to find a direct correlation among age, sex, and MAP as they relate to aortic compliance and www.anesthesiaclinics.com FloTract System ’ 47 Figure 1. The impact of arterial resistance and compliance on arterial waveform skewness and kurtosis, respectively. As depicted by the waveforms on the left, as arterial resistance increases, the skewness or lack of symmetry of the arterial waveform also increases. As depicted on the right, as arterial compliance increases, the kurtosis or distinctness of the peak of the arterial waveform decreases. The skewness and kurtosis of the arterial waveform are measured by the FloTrac system every 60 seconds to assess the impact of arterial compliance and resistance on pressure. This is used to determine w. (Adapted from: Case Study—‘‘Getting mL/beat from mm Hg’’ Arterial Pressure-based Cardiac Output, The Edwards FloTrac Algorithm, Edwards Lifesciences, 2008.) developed a mathematical formula to determine compliance based on these variables. The algorithm uses the analysis of the skewness and kurtosis of the arterial waveform to further refine the resistance and compliance estimates. Using all of these variables, the algorithm makes a determination of w. The first version of FloTrac software, version 1.01, performed this determination or calibration of w every 10 minutes. As changes in hemodynamics and clinical interventions can occur in a much shorter time frame, this 10-minute interval was seen as a potential limitation to the accuracy of FloTrac-derived data. This seemed to be demonstrated in several of the investigations of the device with this software version.3–7 The software has undergone 3 revisions to deal with this issue. The newest version of software, version 1.10, and its immediate predecessor, version 1.07, perform the recalibration of w every 60 seconds. This modification has been demonstrated by several investigators to improve the accuracy of the system’s results.8–10 Once w and sAP are calculated, SV is determined and output to the Vigileo display system. Calculations of CO, SVR, and SVV can then follow from the SV determination. www.anesthesiaclinics.com 48 ’ Hashim and Lerner The FloTrac has some features that are appealing to the clinician. First off and as mentioned earlier, the system can theoretically be used with any arterial line; there is no need to place a specially designed proprietary catheter. As many cardiac surgical as well as critically ill patients already have an arterial line in place, there is no additional risk involved with the placement of other invasive vascular lines. In addition, there is no apparent limitation as to the location of the arterial cannulation. This flexibility is enabled by the FloTrac algorithm’s supposed ability to adjust for differences in waveform that result from these variations. In support of this, the system has been shown by some investigators to provide reliable measurements from either a radial or femoral arterial catheter location.7,11 However, other investigators have expressed concern about differences in measurements of pressure from different sites, particularly in the setting of hemodynamic instability and/or the use of vasopressors. Compton et al12 found significant introduction of error in FloTrac measurements of CO when differences in MAP between 2 different sites were more than 5 mm Hg. Although the site of cannulation may not be important, the quality or ‘‘fidelity’’ of the tracing is extremely significant. As the system relies on an analysis of waveform shape, proper dampening of the arterial monitoring system is required to improve the accuracy of the FloTrac system’s calculations. (Case Study—‘‘Getting ml/beat from mm Hg’’ Arterial Pressure-based Cardiac Output, The Edwards FloTrac Algorithm, Edwards Lifesciences, 2008.) The second major appealing feature to the clinician is the fact that the FloTrac system does not require external calibration. As described in detail, the FloTrac algorithm does its own calibration based on patient demographics and waveform analysis. The PiCCO and LiDCO systems first released into clinical practice required that a manual calibration be performed in the individual patient and at relevant intervals to allow for accurate calculations. The PiCCO system requires a transpulmonary thermodilution for calibration whereas the LiDCO system requires lithium dilution.13,14 These calibrations allow for adjustments to individual patient variables such as vascular tone. Of course this lack of need for external calibration in the FloTrac system is only a potential benefit; it is realized only when and if the internal calibration results in valid and accurate measurements. There are several principal limitations to the FloTrac system as outlined by the manufacturer. First off, the device has only been studied in and is only recommended for use in adult patients. Second, as there is total dependence on the arterial line waveform for accurate calculations, the FloTrac system requires a consistent and regular waveform that is of high fidelity. The presence of dysrhythmias or improper dampening from kinking or extra tubing and stopcocks can prevent accurate results. In addition, because of the impact on the arterial waveform, Edwards www.anesthesiaclinics.com FloTract System ’ 49 specifically considers the presence of significant aortic regurgitation as a limitation. This is based on the work of Lorsomradee et al4 who, using software version 1.07, showed a loss of accuracy in CO measurements in the presence of ‘‘significant’’ aortic regurgitation. Of note, in this study, ‘‘significant’’ aortic stenosis did not seem to impact accuracy. Third, the device has not been validated in the setting of intra-aortic balloon pumps (IABP) or ventricular assist devices. Lorsomradee et al4 showed that the presence of an IABP prevented the FloTrac system from obtaining results in several patients and that when results were obtained, the accuracy was significantly affected. Lastly, and perhaps most troubling, is the manufacturers consideration of ‘‘shock states or hypothermic episodes’’ as limitations for use as these conditions ‘‘may influence values with radial arterial locations.’’ (Case Study—‘‘Getting ml/beat from mm Hg’’ Arterial Pressure-based Cardiac Output, The Edwards FloTrac Algorithm, Edwards Lifesciences, 2008.) The issue with this limitation is that it leads to speculation as to what degree or type of ‘‘shock’’ or degree of hypothermia is problematic in individual circumstances. This naturally leads to concern with how the FloTrac device will perform in patient situations where there are rapid changes in vascular tone, patient positioning, patient temperature, and volume status, to name just a few. Similarly, as the FloTrac calculations are based on algorithm tuned estimates of vascular compliance and resistance, seemingly any significant change in vascular tone, whether induced by reflex or by medications, could impact the accuracy of the data provided. Although these issues may impact radial arterial catheters to a greater degree, they could potentially affect arterial catheters in any location. Similarly, any deviations in arterial compliance from FloTrac estimates will introduce error. This sentiment of concern has been echoed by several investigative groups.4,5,11,12,15,16 It may in fact be the case that in these patient situations the actual individual FloTrac-derived calculations may be of less value than their general trends over time particularly as an assessment of response to therapy. An overview of the potential benefits and weaknesses of the FloTrac system is provided in Table 1. The rest of this chapter will provide a review of the current literature and its assessment of the system in a variety of clinical environments. ’ Intravascular Fluid Assessment and the FloTrac System As mentioned earlier, in addition to CO, the FloTrac system provides other data that can be useful in patient care. These data include SV, SVR, and the dynamic index of SVV. SVV, which will be discussed in detail elsewhere within this text, has shown great promise in assessing www.anesthesiaclinics.com 50 ’ Hashim and Lerner Table 1. Strengths and Weaknesses of the FloTrac Monitoring System Strengths Ability to use any arterial line No need for central venous access No required external calibration No need for recalibration Weaknesses Requirement of consistent arterial waveform with proper dampening Decreased accuracy in setting of altered vascular tone (eg, sepsis, vasopressor use, etc) Dependence on a regular rhythm Limited accuracy during times of hemodynamic instability the ‘‘fluid responsiveness’’ of mechanically ventilated patients in a variety of clinical situations.17–19 Briefly, SVV is caused by the interaction of the cardiac and respiratory systems; that is, the changes in intrathoracic pressure during controlled ventilation have an impact on SV. This impact on SV increases as preload decreases.20 In addition to preload, other factors affecting SVV include chest wall compliance and ventilation parameters, including tidal volumes and airway pressures. In situations wherein chest wall compliance and respiratory parameters are held relatively constant, SVV can be used as a guide to establishing whether or not a given patient will respond to fluid loading by increasing CO. To our knowledge, the ability of FloTrac system assessments of SVV to predict fluid responsiveness is limited to 6 investigations. Three of these investigations were performed in cardiac surgical patients, 2 in patients undergoing esophageal surgery, and 1 in patients undergoing liver transplantation. de Waal et al21 assessed FloTrac SVV (version 1.01) in 18 postoperative coronary artery bypass grafting (CABG) patients. They found that FloTrac SVV could not predict fluid responsiveness and suggested further investigation with the newer software versions. Hofer et al16 compared SVV measurements determined by PiCCO and FloTrac (version 1.07) in 40 postoperative cardiac surgical patients. They found that both devices performed comparably in terms of predicting fluid responsiveness but that the FloTrac-derived SVV had a lower threshold value for determining responsiveness (9.6% compared with 12.1% for PiCCO). Cannesson et al18 found that FloTrac SVV (version 1.10) predicted fluid responsiveness with ‘‘acceptable sensitivity and specificity’’ (82% and 88%, respectively). Kobayashi et al22 found in 2 separate investigations concerning patients requiring major esophageal surgery, 1 postoperative and the other intraoperative, that FloTrac SVV provided reliable data in determining fluid responsiveness.23 Biais et al17 investigated whether FloTrac SVV (version 1.07) was able to predict fluid responsiveness in 35 patients after liver transplantation. They found that SVV greater than 10% was highly sensitive and specific www.anesthesiaclinics.com FloTract System ’ 51 for fluid responsiveness (94% and 94%, respectively). They also found a significant correlation between the decrease in SVV with volume expansion and the subsequent increase in CO. Also relevant was the fact that 5% of patients initially enrolled in the study had to be excluded due to dysrhythmias. Although only a small number of patients have been studied, it does appear that the newer FloTrac software versions allow for meaningful assessments of SVV. Further studies can serve to reinforce this in other patient populations and to establish what, if any, adjustment to SVV threshold for determining fluid responsiveness is necessary and specific to the FloTrac system. ’ The FloTrac System as a CO Monitor Before entering into a discussion or review of the FloTrac system’s accuracy as a monitor of CO, it is important to talk about the assessment of accuracy. The first issue to consider is the reference point for comparison. In the case of CO measurement, thermodilution performed with a pulmonary artery catheter is generally considered as the practical gold standard. This is not at all unreasonable given the relatively thorough investigation of thermodilution that has occurred over several decades. When a new technique for measuring a given parameter is to be assessed against a gold standard, evaluating correlation between them is not adequate as correlation says little about how close any pair of measurements actually is. Correlation only gives information as to how the series of measurements from the 2 techniques relate to one another. This shortcoming becomes even more relevant when the standard technique has significant error in and of itself. Typically, Bland-Altman analyses, wherein the mean of the result of the 2 techniques is plotted against the difference in their measurements, are performed.24 These analyses allow for the determination of bias (average difference), precision (1 standard deviation of the result comparisons), limits of agreement (2 standard deviations of the result comparisons), and the percentage error [( ± 2 standard deviations)/mean result] between the 2 techniques. It is important to take into account that the inherent error for thermodilution measurements of CO are in the 10% to 20% range.25 On the basis of this error inherent to the gold standard, Critchley and Critchley26 recommended that any new method of measurement for CO be judged acceptable if it also had a similar inherent error. This led to their generally accepted conclusion that so long as the limits of agreement between the new method and thermodilution were within ± 30%, the technique should be considered as acceptable. Given this backdrop, a review of the literature on the FloTrac system as a monitor of CO now follows. www.anesthesiaclinics.com 52 ’ Hashim and Lerner To our knowledge, there have been 18 studies performed to assess the FloTrac system’s accuracy as a CO monitor. Most of these investigations, that is, 12 of the 16 (75%), have occurred in cardiac surgical patients.3–5,7– 9,11,15,27–31 Some of the studies are limited to the intraoperative period, some to the postoperative period, and others include both of these environments. Most have looked at patients that had their surgery performed with cardiopulmonary bypass3–5,7,9,15,28,30 whereas some have looked specifically at patients undergoing off-pump CABG.8,29,31 The likely reason for this focus on cardiac surgical patients is that in most centers a pulmonary artery catheter is routinely placed in these patients and, presumably, all centers place an invasive arterial catheter. Therefore, such study requires little deviation from institutional standards of care for monitoring in this patient population. Of the remaining 5 studies, one involved ICU patients with sepsis,6 one investigated ‘‘unstable’’ patients in a medical ICU,12 one looked at a combination of surgical and medical ICU patients,10 one looked at neurosurgical ICU patients,32 and one involved patients undergoing liver transplantation.33 In total, 575 patients have been involved in these assessments of the FloTrac system’s accuracy. Using the original version 1.01 of the FloTrac algorithm, Mayer et al studied 40 patients undergoing CABG or cardiac valve procedures. Some of the measurements were made intraoperatively and some postoperatively, all at predetermined times. 33% of patients had to be excluded from the intraoperative study period and 15% from postoperative period, mostly due to dysrhythmias. They found unacceptable limits of agreement (>30%) between CO measurements made with FloTrac and intermittent bolus thermodilution in both the intra and postoperative periods (51% and 42%, respectively) As a result, they recommended that FloTrac’s use be limited to the monitoring of trends. In their initial study, Zimmermann et al, using FloTrac version 1.01 performed a very similar study in cardiac surgical patients and had very similar results. They concluded that the FloTrac system’s accuracy did not meet Critchley and Critchley criterion for acceptable accuracy.7 Interestingly, though these two studies led to concern about version 1.01, the rest of the published studies that used this initial software found that CO measurements were within the acceptable range for accuracy in certain situations. de Waal et al’s study of intraoperative and postoperative CABG patients compared FloTrac to bolus thermodilution and PiCCO. They found that accuracy criteria were successfully met during the post cardiopulmonary bypass (CPB) and postoperative periods but not during the pre-CPB period.3 Manecke et al also found acceptable accuracy compared to both bolus and continuous thermodilution techniques in post-operative cardiac surgical patients deemed as ‘‘reasonably stable.’’11 Most of the studies published in the literature on FloTrac CO measurements were performed on intermediate versions of the software, www.anesthesiaclinics.com FloTract System ’ 53 namely 1.03 and 1.07. Chatti et al, in a multi-center study, compared CO measurements made using FloTrac versions 1.03 and 1.07 to those from esophageal Doppler probes in ICU patients.10 They found improvements in accuracy with version 1.07 but that the limits of agreement were still only 59%. Sakka et al also found unacceptable accuracy in septic patients receiving norepinephrine with version 1.07.6 However, in this study, the reference used for comparison was PiCCO derived transpulmonary thermodilution. They found that that the FloTrac system generally underestimated the CO as compared to the data provided by PiCCO, a finding similar to that of Compton et al.12 Prasser et al’s study in neurosurgical ICU patients using version 1.03 also found unacceptable accuracy.32 Lorsomradee et al, in their study of intraoperative CABG patients, also found unacceptable accuracy of CO measurements made with version 1.07 compared to continuous thermodilution.4 Of note, the accuracy was particularly worsened in the presence of aortic regurgitation or an IABP. Senn et al found acceptable accuracy of version 1.07 compared to intermittent thermodilution CO measurements in post-operative cardiac surgical patients.8 This finding was echoed by Mehta et al who compared version 1.07 to intermittent thermodilution during the intraoperative period of off-pump CABG procedures.31 Although Button et al. concluded that FloTrac version 1.07 was comparable to PiCCO, continuous thermodilution, and intermittent measurements of CO in intraoperative and postoperative cardiac surgical patients, they did not report their limits of agreement.28 This prevents a true assessment of the degree of accuracy within their study. The newest version of the FloTrac software seemed to bring some improvement in accuracy, at least in cardiac surgical patients. Most encouraging was the fact that when the Mayer and Zimmermann groups repeated their assessments with the most current software version, version 1.10, they found improvements in the accuracy of the CO measurements. Mayer et al30 found acceptable accuracy in CABG patients during both the intraoperative and postoperative periods, with limits of agreement of 28.3% and 20.7%, respectively. Zimmermann et al,9 although finding improvements in accuracy compared with their previous study, still did not find acceptable limits of agreement and reaffirmed their recommendation that FloTrac ‘‘not be used during and after cardiac surgery.’’ Prasser et al27 found acceptable accuracy in postoperative CABG patients compared to bolus thermodilution. The only other studies that evaluated FloTrac version 1.10 were in the noncardiac surgical environment. Both of them found that FloTrac’s accuracy was not acceptable in their study population. Compton et al12 studied 25 ‘‘unstable’’ medical ICU patients. The criteria for being considered ‘‘unstable’’ were defined as the need ‘‘for fluid resuscitation and/or vasopressor therapy.’’ It is important to note that in their study the www.anesthesiaclinics.com 54 ’ Hashim and Lerner standard for measurement was PiCCO-derived pulse contour CO, not bolus thermodilution through a pulmonary artery catheter. They found a high percentage of error (58.8%) between the 2 techniques and concluded that FloTrac was ‘‘not suitable to replace invasive CO monitoring.’’ Biancofiore et al33 compared FloTrac and continuous thermodilution CO measurements during the intraoperative and postoperative phases of liver transplantation. They also found unacceptable limits of agreement. Summarizing the published experience with the FloTrac system is extremely difficult given the heterogeneity of the available studies. Differences in patient populations, study environments (intraoperative, postoperative, nonsurgical), FloTrac software versions, ventilatory settings, medical interventions, and in the reference standard(s) used (intermittent thermodilution CO, continuous thermodilution CO, esophageal Doppler, PiCCO), combined with the relatively small patient numbers in each study, are all central to this issue. However, there are several general summary statements that seem warranted. First off, there seems to be enough data available to question the accuracy of the system’s measurements in a variety of situations. This seems to be particularly true in ‘‘unstable’’ conditions; situations where there are rapid and significant changes in temperature, vascular tone (from any cause), and/or intravascular volume. In addition, in patient populations wherein significant alterations in vascular tone are inherent (sepsis, liver failure) there also seems to be unacceptable inaccuracies. Obviously, these are the situations where FloTrac-derived data would likely be most helpful in developing care plans. To what extent or how the loss of accuracy in these settings should impact the use of this device has not yet been determined. Second, although it does seem that the newer FloTrac software versions have improved the accuracy of the system’s ability to determine CO, this has not consistently led to sufficient limits of agreement with standard techniques. Lastly, the FloTrac system certainly does seem to be able to accurately measure CO in several challenging environments. This, in addition to its ease of use, makes FloTrac a potentially useful device in the management of many challenging patient care situations. Future improvements in system software and the study of more patients and patient settings will be necessary to better define the role of this unique monitor in the care of the critically ill patient. ’ References 1. Langewouters GJ, Wesseling KH, Goedhard WJ. The static elastic properties of 45 human thoracic and 20 abdominal aortas in vitro and the parameters of a new model. J Biomech. 1984;17:425–435. 2. Langewouters GJ, Wesseling KH, Goedhard WJ. The pressure dependent dynamic elasticity of 35 thoracic and 16 abdominal human aortas in vitro described by a five component model. J Biomech. 1985;18:613–620. www.anesthesiaclinics.com FloTract System ’ 55 3. de Waal EE, Kalkman CJ, Rex S, et al. Validation of a new arterial pulse contourbased cardiac output device. Crit Care Med. 2007;35:1904–1909. 4. Lorsomradee S, Cromheecke S, De Hert SG. Uncalibrated arterial pulse contour analysis versus continuous thermodilution technique: effects of alterations in arterial waveform. J Cardiothorac Vasc Anesth. 2007;21:636–643. 5. Mayer J, Boldt J, Schollhorn T, et al. Semi-invasive monitoring of cardiac output by a new device using arterial pressure waveform analysis: a comparison with intermittent pulmonary artery thermodilution in patients undergoing cardiac surgery. Br J Anaesth. 2007;98:176–182. 6. Sakka SG, Kozieras J, Thuemer O, et al. Measurement of cardiac output: a comparison between transpulmonary thermodilution and uncalibrated pulse contour analysis. Br J Anaesth. 2007;99:337–342. 7. Zimmermann A, Kufner C, Hofbauer S, et al. The accuracy of the Vigileo/FloTrac continuous cardiac output monitor. J Cardiothorac Vasc Anesth. 2008;22:388–393. 8. Senn A, Button D, Zollinger A, et al. Assessment of cardiac output changes using a modified FloTrac/Vigileo algorithm in cardiac surgery patients. Crit Care. 2009;13:R32. 9. Zimmermann A, Steinwendner J, Hofbauer S, et al. The Accuracy of the Vigileo/ FloTrac system has been improved-follow-up after a software update: a blinded comparative study of 30 cardiosurgical patients. J Cardiothorac Vasc Anesth. 2009. [Epub ahead of print]. 10. Chatti R, de Rudniki S, Marque S, et al. Comparison of two versions of the VigileoFloTrac system (1.03 and 1.07) for stroke volume estimation: a multicentre, blinded comparison with oesophageal Doppler measurements. Br J Anaesth. 2009;102: 463–469. 11. Manecke GR Jr, Auger WR. Cardiac output determination from the arterial pressure wave: clinical testing of a novel algorithm that does not require calibration. J Cardiothorac Vasc Anesth. 2007;21:3–7. 12. Compton FD, Zukunft B, Hoffmann C, et al. Performance of a minimally invasive uncalibrated cardiac output monitoring system (Flotrac/Vigileo) in haemodynamically unstable patients. Br J Anaesth. 2008;100:451–456. 13. Della Rocca G, Costa MG, Pompei L, et al. Continuous and intermittent cardiac output measurement: pulmonary artery catheter versus aortic transpulmonary technique. Br J Anaesth. 2002;88:350–356. 14. Hamilton TT, Huber LM, Jessen ME. PulseCO: a less-invasive method to monitor cardiac output from arterial pressure after cardiac surgery. Ann Thorac Surg. 2002;74: S1408–S1412. 15. Breukers RM, Sepehrkhouy S, Spiegelenberg SR, et al. Cardiac output measured by a new arterial pressure waveform analysis method without calibration compared with thermodilution after cardiac surgery. J Cardiothorac Vasc Anesth. 2007;21:632–635. 16. Hofer CK, Senn A, Weibel L, et al. Assessment of stroke volume variation for prediction of fluid responsiveness using the modified FloTrac and PiCCOplus system. Crit Care. 2008;12:R82. 17. Biais M, Nouette-Gaulain K, Cottenceau V, et al. Uncalibrated pulse contour-derived stroke volume variation predicts fluid responsiveness in mechanically ventilated patients undergoing liver transplantation. Br J Anaesth. 2008;101:761–768. 18. Cannesson M, Musard H, Desebbe O, et al. The ability of stroke volume variations obtained with Vigileo/FloTrac system to monitor fluid responsiveness in mechanically ventilated patients. Anesth Analg. 2009;108:513–517. 19. Reuter DA, Felbinger TW, Schmidt C, et al. Stroke volume variations for assessment of cardiac responsiveness to volume loading in mechanically ventilated patients after cardiac surgery. Intensive Care Med. 2002;28:392–398. 20. Michard F. Changes in arterial pressure during mechanical ventilation. Anesthesiology. 2005;103:419–428. www.anesthesiaclinics.com 56 ’ Hashim and Lerner 21. de Waal EE, Rex S, Kruitwagen CL, et al. Stroke volume variation obtained with FloTrac/Vigileo fails to predict fluid responsiveness in coronary artery bypass graft patients. Br J Anaesth. 2008;100:725–726. 22. Kobayashi M, Ko M, Kimura T, et al. Perioperative monitoring of fluid responsiveness after esophageal surgery using stroke volume variation. Expert Rev Med Devices. 2008;5:311–316. 23. Kobayashi M, Koh M, Irinoda T, et al. Stroke volume variation as a predictor of intravascular volume depression and possible hypotension during the early postoperative period after esophagectomy. Ann Surg Oncol. 2009;16:1371–1377. 24. Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. 25. Stetz CW, Miller RG, Kelly GE, et al. Reliability of the thermodilution method in the determination of cardiac output in clinical practice. Am Rev Respir Dis. 1982;126: 1001–1004. 26. Critchley LA, Critchley JA. A meta-analysis of studies using bias and precision statistics to compare cardiac output measurement techniques. J Clin Monit Comput. 1999;15:85–91. 27. Prasser C, Trabold B, Schwab A, et al. Evaluation of an improved algorithm for arterial pressure-based cardiac output assessment without external calibration. Intensive Care Med. 2007;33:2223–2225. 28. Button D, Weibel L, Reuthebuch O, et al. Clinical evaluation of the FloTrac/Vigileo system and two established continuous cardiac output monitoring devices in patients undergoing cardiac surgery. Br J Anaesth. 2007;99:329–336. 29. Chakravarthy M, Rajeev S, Jawali V. Cardiac index value measurement by invasive, semi-invasive and non invasive techniques: a prospective study in postoperative off pump coronary artery bypass surgery patients. J Clin Monit Comput. 2009;23: 175–180. 30. Mayer J, Boldt J, Wolf MW, et al. Cardiac output derived from arterial pressure waveform analysis in patients undergoing cardiac surgery: validity of a second generation device. Anesth Analg. 2008;106:867–872. 31. Mehta Y, Chand RK, Sawhney R, et al. Cardiac output monitoring: comparison of a new arterial pressure waveform analysis to the bolus thermodilution technique in patients undergoing off-pump coronary artery bypass surgery. J Cardiothorac Vasc Anesth. 2008;22:394–399. 32. Prasser C, Bele S, Keyl C, et al. Evaluation of a new arterial pressure-based cardiac output device requiring no external calibration. BMC Anesthesiol. 2007;7:9. 33. Biancofiore G, Critchley LA, Lee A, et al. Evaluation of an uncalibrated arterial pulse contour cardiac output monitoring system in cirrhotic patients undergoing liver surgery. Br J Anaesth. 2009;102:47–54. www.anesthesiaclinics.com