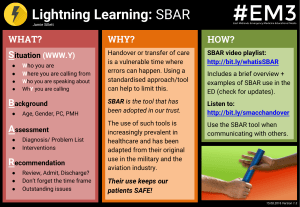
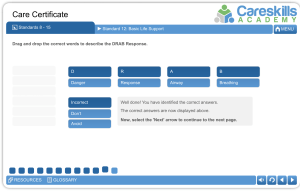
A-E Respiratory Assessment Handbook Page 2 - Introduction Page 3 - Critical Care Outreach Page 4 - The A-E Assessment Page 5 - A: Airway Page 6 - B: Breathing Page 7 - C: Circulation Page 8 - D: Disability Page 9 - E: Exposure Page 10 - Handover Tools: SBAR Page 11-12: Case Study Page 13 - Where to Find Us Jodie Bryant Associate Professor Specialist Physiotherapist Introduction Aims of this Tutorial Build confidence and understanding of .... 1. The need for systematic assessment models 2. Early recognition systems to identify patient deterioration 3. Methods of systematic assessment 4. What happens next .... In the Past... Before a structured assessment for acute respiratory conditions, things got a bit muddled! Unfortunately, pathologies and symptoms were easily missed without the defined structure of an assessment. What Changed? 1870 - During the Crimean War, Florence Nightingale organises patients so that those most unwell, and therefore requiring the most intensive nursing, are located nearest the nursing station. In December 1953, Bjorn Ibsen sets up the first intensive care unit in Copenhagen, during the polio pandemic And then... "There are increasing numbers of critically ill and at-risk patients in acute hospitals who are suffering potentially preventable, serious complications that may result in death because of a lack of appropriate systems, skills, and expertise outside of the ICU" Critical Care Outreach The issues on the last highlight the importance of patients being able to access "Critical Care" even if they are not on a "Critical Care Unit". Hence the birth of Critical Care Outreach! Critical care outreach teams (CCOT) offer intensive care skills to patients with, or at risk of, critical illness receiving care in locations outside the intensive care unit Evidence that level 1 care of acutely deteriorating patients was ' suboptimal' - why? High in-hospital mortality (NICE) All patients should be monitored Role = Identify, monitor, instigate, act, review Prevent or facilitate admission Track and Trigger Systems = Prevent Death 1. Track patient deterioration: Regular monitoring of physiological observations and patient behaviour 2. Trigger escalations in clinical monitoring and rapid response by critical care outreach teams Track and Trigger systems were created to help allow clinicians identify the Trends of Observations that may highlight patients who are at risk of deterioration. The A-E Assessment The Underlying Principles Systematic and Repeatable Built on Underlying Principles Assesment and Reassesment Cycle Life threatening issues identified immediately Seek help Team effort Communication "Who You Gonna Call?!" It is always important to think about "Who can you get help from?" Whether that be other physiotherapists, doctors, nurses, and other members of the MDT, you are not alone, and we should actively think that way during our assessment and treatment First Steps: Your Safety If you are not safe you cant help anyone Look Ask "Jodie , Jodie how are you, can you hear me?" Assess the response 2222 if needed, SHOUT for help - do you need to start CPR? Get the kit and the people you need A - Airway Patent / obstructed - How??? Patient level of consciousness Oxygenate Seek support Act within your scope Airway clearance (Suction, OP/NPA, Opening Manouvres, Treat the cause, ? Intubation required) Extra Notes Section... B - Breathing Identify life threatening breathing concerns Look, Listen, Feel for Signs of Respiratory Distress Respiratory Rate - Normal or abnormal, cause? Rhythm, Depth and Quality of breathing FiO2, method of delivery, Sp02, pa02, pCO2, ABG Auscultate Fremitus Palpation and visualisation of chest wall Percussion CXR Other diagnostics e.g. Spiro, bronch, CT, DD Extra Notes Section... C - Circulation Identify life threatening circulatory concerns Look - Colour of patient, skin colour Feel - Limb Temperatures Capillary refill time Chest pain or tightness Pulse rate (bounding, weak, regular) Heart rate and rhythm Consider PMH e.g. tamponade Blood pressure (ART line / manual) Urine output (0.5 ml per kg per hour) Drains output Extra Notes Section... D - Disability Identify life threatening neurological concerns Review your ABC if needed Previous baseline Admission details Drugs and medications Glasgow coma scale / AVPU score / AMTS Painful stimuli Pupil size and reactivity Blood sugar Pain (SCALE) Functional assessment Recovery position required Extra Notes Section... E - Exposure Identify Life Threatening Concerns Expose Patient, Dignity Temperature Blood loss Also... Full History, Handover Medications Blood tests and other diagnostics Document Assess, reassess Ceiling of care Ongoing physiotherapy Extra Notes Section... Constant Reassessment Handover Tools - SBAR SBAR Situation - Background - Assessment - Recommendations SBAR is an excellent tool to be able to use to help you communicate and handover with the team. Having another structured framework like this will really help improve your confidence when communicating with other members of the team, because you have a really good idea of what things to include in your handover. Case Study Marlene Admitted after fall from mountain bike Called to see as Sp02 dropping In Side Room on T+0 ward 3 Days Post Injury This is your chance to make notes on the Case Study whilst listening to Jodie! What are the key things to think about? Young patient Alone Potential rib injury from falling off bike Why are things worsening for her? A Airway B Breathing C Circulation D Disability E Exposure Case Study RR - 24 SPO2 - 90% FIO2 - 4l nasal specs TEMP - 38.3 BP - 130 /87 HEART RATE - 120 CONCIOUSNESS - A What is Marlene's NEWS Score? CXR Findings? What are your key Assessment Thoughts? Key SBAR Thoughts? Who are you going to call? Where to Find Us! MEMBERSHIP THE EXCLUSIVE ALL-IN-ONE SUBSCRIPTION member.clinicaphysio.com All Live Webinars All On-Demand Webinars Handbooks + Personalised Certificates Our Brand New Member-Only Podcasts Written Resources Early Access Videos Community Forums and Support Exclusive Course Discounts On-Demand Webinars www.clinicalphysio.com/on-demand-webinars If you liked this webinar, you may also like... Respiratory Assessment Made Simple Chest X-Rays Arterial Blood Gases @clinicalphysio @clinicalphysio Clinical Physio