Nursing Ethics: Autonomy, Beneficence, and Informed Consent
advertisement
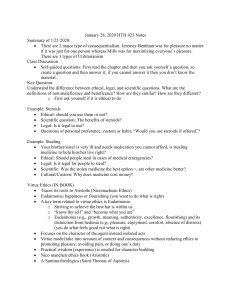
Bachelor of Science in Nursing 2YA ETIC111: BSN 2ND YEAR 1ST SEMESTER FINAL 2021 Coverage for Final: • Autonomy and Beneficence • Non-maleficence and Justice • Some Ethical Issues - Care at the Beginning of Life - Care at the Promotion of Life - Care at the End of Life - - • • • • • - - • • • - - AUTONOMY & BENEFICENCE Autonomy Derived from the Greek words ‘auto’ meaning ‘self’ and ‘nomos’ meaning ‘rule’. Thus, autonomy means self-law or law to oneself. The original usage then of autonomy is to mean ‘self-rule’ or ‘self-governance’ of independent city-states Capacities for Self-Governance: • To Understand (moral reflection) the issue and what the situation is all about and to reason out and give one’s opinion/ • To Deliberate (effective deliberation) by weighing the pros and cons of the issue. • To Make an Independent choice (free choice) basic to making an independent choice is one’s capacity to make decisions. Practical Implication of respect for Autonomy in medical practice Right of the patient, that is, right to self-determination which is guaranteed by the patient’s bill of rights. Informed consent Actual directive Advance directive/Living will Refusal of treatment Informed Consent Informed consent is also known as enlightened consent, to mean, any prior substantial or therapeutic and research participation, patient must have a full information of what procedure is all about, objective, need and advantage. It is also a form of invitation to a patient to participate in his health care decisions. Two Settings: • Therapeutic setting • Research setting Elements of informed consent: Threshold elements Disclosure/Information Competence/comprehension Voluntariness Disclosure/Information The extent of information given to the patient by the physician/nurse relating to the medical procedure. The expenses to be incurred, likewise is decisive whether consent is to be given by the patient for medical procedure Competence/comprehension The patient’s level of education greatly affects one’s own decision and the level of emotion to the extent relevantly possible. The health care provider can appropriately assess the accessibility of the language that will understood by patient. - Patient can finally render an intelligent decision Voluntariness - This element of informed consent is customarily understood as free and willfully given by the patient. The issue at hand is that the patient must be given sufficient time and ample space The Two function of informed consent • Projective (to safeguard against the tension of integrity) • Participative (to be involved in the health care decision making) Two basics of obtaining consent 1) Written consent (it is often use upon admission of patient into the hospital, another used it maybe dream necessary for other procedure likely surgery) 2) Verbal consent (it usually comes the comes in the form of an implied consent like when a patient seeks consultation with is physician) Significance and justification of informed consent 1) Patient of an opportunity to be an informed participant in health decision. 2) it is also a legal document and as a form of an assurance of safety for the and for healthcare professionals (ex: invasive procedure such as: surgery, anesthesia, and others) 3) A form of protocol of the research process because most research involve patient’s lives. 4) It emphasizes honesty trait of the professional to carry in their very selves an honest character when asking patient to sign informed or enlightened consent. 5) It reduces risks and avoids unfair treatment and exploitation by the professional and it is also regulatory and institutional control. 6) It also protects the autonomous choice, by which the claim of patient’s right to autonomy was promoted. Barriers to informed consent vis-à-vis nursing intervention • Language: the nurse can use intermediary such as a translator to translate information to language that can be understood by the patient. • Cultural differences: the nurse can use intermediary or let patient meet other persons who underwent the same medical procedure or treatment of the same culture background as the patient. • Physical impairment/illiteracy: the nurse can show pictures, videos, literature, and other related teaching aid. • Incompetence: the nurse help to ensure that decision made by the person responsible for the patient is for letters benefit and wellbeing. • General it is ethical as well as legal responsibility of the nurse to overcome these barriers and everything in her capacity to ensure that the patient sufficiently gets all the needed information to make an informed decision. - Actual directive and advance directive The right to self-determination originated from the principle of autonomy which entails every individual to informed consent including the right of person of legal age and sound mind to voluntarily refuse a diagnosis. J.A.K.E 1 of 7 ETHICS – BSN 2ND YEAR 1ST SEMESTER FINAL 2021 - Actual directive is an instruction that was given on the very moment that is being done by any person with a normal condition. - Advance directive, on the other hand, is an issue given in anticipation of what a person might think would happen relative to his/her health condition. • Biological parents of the patient • the oldest child of the patient if of legal age • legally adapting parents of the patient • nearest kin • municipal health officer of the place where the hospital is located/medical director Two forms advance directive 1) Living Will (instructional directive) - A will by which any competent adult give direction and instruction for future care in the event that the patient involve can no longer make due to terminal or severe illness or an impending death 2) Medical Power of Attorney (Health care proxy) - A probable patient can name a person trusted so as to act in their behalf as an agent/proxy in making health care decisions in an event of incapacity. - - - - - - Practical Implication/issues of limiting Autonomy Paternalism (Parentalism) Paternalism (Parentalism) comes from the Latin word ‘pater’ to mean father. The conflict between respect for autonomy and the desire to help the patient (beneficence) brings the problem into forefront of paternalism. Paternalism describe as ‘the principle and practice of paternal administration; government as by a father; the claim or attempt to supply needs or to regulate the life of a nation or community in the same way a father does to the children. Two important features of Paternalism: That the father acts beneficently, namely, in accordance with the conception of the interest of his children and he makes all or at least some of the decisions relating to his children’s welfare, rather then letting them make those decision. In medicine, Paternalism is applied when health care givers such as doctor, nurses and the like, assumed the authority to make decision for and in behalf of the patient without their consent or knowledge. Placebo (Latin for "I shall please") is a pharmacologically inert substance (such as saline solution or a starch tablet) that seems to produce an effect similar to what would be expected of a pharmacologically active substance (such as an antibiotic) The Placebo Effect The placebo effect consists of several different effects woven together, and the methods of placebo administration may be as important as the administration itself a simulated or otherwise medically ineffectual treatment for a disease or other medical condition intended to deceive the recipient. Sometimes patients given a placebo treatment will have a perceived or actual improvement in a medical condition, a phenomenon commonly called the placebo effect or placebo response. - - - - Resuscitation A form of medical intervention done in a series of steps directed to sustain adequate circulation of oxygenated blood to vital organs while an effective heartbeat was restored. Do not Attempt Resuscitate (DNAR) or commonly known as Do not Resuscitate (DNR) a request to forego resuscitation maneuvers. Indications for DNR orders When the patient condition is terminal, and death is immanent so that life support only prolongs the dying process. When the patient is irreversibly comatose or in persistent vegetative state and there is no hope of improvement. When the burden of treatment far outweighs the benefit (adapted from the Southeast Asia Center of Bioethics). The following are reasons for DNR orders, these were taken from different sources gathered: • No medical benefit • Poor quality of life before CPR • Poor prognosis • Severe brain damage • Extreme suffering or disability in a chronically or terminally ill patient • Request by a patient or family member • Enormous cost and personnel commitment as opposed to the low probability of patient recovery • By not administering any cardiopulmonary in the event of cardiac arrest • We are letting the person go in peace and dignity. Beneficence Etymologically, comes from the two Latin words: • “bonus” where bene was taken to mean “good” • “fic” where fiche was taken to mean “to act or do”. It refers to “action done for the good of the others”. In the language of medicine, this principle highlights the duty of health provider to do good and take positive steps, such as prevention and removal of harm to the patient. Beauchamp, Childress & Psyche believed that it could be seen through associated acts of kindness, charity, humanity, altruism & love. Beneficence was often thought to broadly include all form of actions. (Benevolence & Provenance, intended to benefit other persons. So, beneficence refers to an action done benefit others. • Benevolence – refers to the character, trait or virtue of being disposes to act for the benefit of others. • Provenance – is the attentiveness dictated by kindness to anticipate what one needs since each one of us, has that inner goodness that pushes us to alleviate the pain and discomfort to others. Therefore, Beneficence goes hand in hand with benevolence and provenance. Obligatory and Ideal Beneficence Some ethnical theories like Utilitarianism are based on the principle of beneficence. This means, that goodness and kinddeed form the substratum of the Utilitarian Theory. J. Bentham and W.D. Ross differ in the meaning of beneficence, yet they employed the term beneficence as a positive obligation, to others, though some critics denied this kind of beneficence for he holds that the beneficence is a J.A.K.E 2 of 7 ETHICS – BSN 2ND YEAR 1ST SEMESTER FINAL 2021 - • • - - - - - - virtuous ideal/acts of charity, thus any person therefore is not morally deficient if he/she failed to act beneficently. Beneficence then is sometimes an admirable ideal of action that exceeds obligation. Nobody denies that the Beneficent acts is morally meritorious and therefore, morally praiseworthy away from a personal obligation. Example: Donating one’s kidney to a stranger. - We are not morally required as morality dictates to perform all possible acts of generosity or charity that will benefit others. By this, Ideal Beneficence means going out of one’s way in order to do good to others, while Beneficence, is merely goodness to others without going out of one’s way. To sum up, Ideal Beneficence is benevolent act that involves going out of one’s way to do good as that of Good Samaritan. Obligatory Beneficence is a mandatory act to do good and to give aid to those who are in need. Practical Applications of the Principle of Beneficence Protect and defend the right of others Prevent harm from occurring to others Remove conditions that will cause harm to others Help persons with disabilities Rescue persons in danger The principle of beneficence is already practice by Filipinos by showing one’s goodness such as, delicate and generous hospitality and this is shown in different situations like; Sharing of goods & Lending of money, materials, equipment and even human resources like bayanihan. NON – MALEFICENCE One’s own obligation to do good in the practice of medicine is also limited by one’s own obligation to avoid evil/harm. One’s avoidance of harm on others is embedded into what we call, the principle of nonmaleficence. In medical ethics it has been closely associated with the maxim, primum non nocere, which means, above all (or first) do no harm (Beauchamp and Childress, 2001). This maxim expresses an obligation of nonmaleficence in the Hippocratic tradition, ‘I will use treatment to help the sick according to my ability and judgment, but I will never use it to injure or wrong them’. This principle helps in decision-making about issues that may alter one’s own life, such as on killing and letting go, withholding and withdrawing treatment, use of extraordinary and ordinary means/procedures and other issues. Nonmaleficence comes from a Latin word: ‘non’ to mean ‘not’; ‘malos’ from which ‘male’ is taken to mean ‘bad/evil’ and ‘faceo’ from which ‘fic’ comes which means ‘do/make’. Thus, the term nonmaleficence means not to make or to do bad or to make evil things intentionally. In medicine, nonmaleficence means not to inflict harm which is not different from ‘not doing evil or bad things. This principle requires a health care provider to prevent or refrain from any sort of actions that eventually causes harm to patient and more importantly when the action is never been justified. Distinction Between Non-Maleficence and Beneficence Generally, an obligation of nonmaleficence is more stringent than obligations of beneficence and in some cases, nonmaleficence perhaps may override beneficence. Beauchamp and Childress suggested the following schema to distinguish the principle of nonmaleficence and beneficence. But the said authors do not propose a hierarchical order Instructive Principle Bioethical Principle One ought not to inflict evil or harm Nonmaleficence One ought to prevent evil or harm Beneficence One ought to remove evil or harm Beneficence One ought to do or promote good Beneficence Examples: 1. Do not kill 2. Do not cause pain or suffering to others 3. Do not cause offense to others 4. Do not incapacitate others 5. Do not deprive others of the goods of life Criteria on Determining Negligence 1. The professional must have the duty to the affected party 2. The professional must breach that duty 3. The affected party must experience a harm 4. The harm must be caused by the breach of duty - Principle of Non-Maleficence Affirms the need for medical competence A part of Filipino character through avoidance of confrontational dialogue that will eventually cause harm to others Practical Application/Implication of the Principle of NonMaleficence Withholding Treatment and Withdrawing Treatment - are bioethical issues which can be acted upon or justified by the following conditions: 1. When the case is irreversible any form of treatment will not benefit the patient 2. When death is immanent or when patient is already dead Ordinary and Extra-ordinary Treatments • Ordinary treatment comprises of the provision of necessities of life that usually pertain to food, normal respiration and elimination process. Hence like intravenous fluids, nasogastric tube feedings, indwelling catheters, are some among the many considered ordinary and necessary measure of treatment and may be sustained even if the case is irreversible. • Extra ordinary treatment comprises of the use of aggressive modalities vis-à-vis the capacities of the family or maybe some family who can very well afford it, continue to give extra ordinary measure. But this means do not necessarily offer any benefit to the patient. - - Killing and Letting Die In ordinary language ‘killing’ is a causal action that deliberately brings about another’s death ‘Letting die’ is ‘prima facie’ acceptable in medicine under two conditions: A medical technology is useless (medically futile) and patients (or valid surrogate/proxy) have validly refused a medical technology, JUSTICE Justice comes from the Latin word "jus" means "right". Justice is a concept of moral rightness based ethics, rationality, law, natural law, religion, equity and fairness, as well as the administration of the law, taking in to account the inalienable and inborn rights of all human beings and citizens, the right of J.A.K.E 3 of 7 ETHICS – BSN 2ND YEAR 1ST SEMESTER FINAL 2021 - - - - - - - all people and individuals to equal protection before the law of their civil rights, without discrimination on the basis of race, gender, sexual orientation, gender identity, national origin, color, ethnicity, religion, disability, age, wealth, or other characteristics, and is further regarded as being inclusive of social justice. Formal Principle of Justice Aristotle in Nichomachean Ethics • Equals must be treated equally • Unequal must be treated unequally Material Principle of Justice Principle that specifies the relevant characteristics for equal treatment are called "Material" because they identify the substantive properties of distribution. Engelhadrt, Keusch, Wildesand others have suggested the following material principle of Justice. • to each person an equal share • to each person according to need • to each person according to contribution • to each person according to free-market exchange Wildes and others have suggested the following material principle of Justice • to each person according to merit • to each person according to effort SOME ETHICAL ISSUES Care at the Beginning of Life The way life is brought into existence (reproductive technology) and the way in which the nature of future human lives are intervened with (like, embryonic stem cell research, human cell line and commodification) reflect this age of consumer mentality and market ethics. Babies have to come at the appropriate time, number and space. For a service fee, then, sex were selected, genes were improved. Children therefore were made to satisfy the desire market (like baby making parent, supplier or baby breaking experimenters). Though this may sound economically good yet its not done for the common good. Commercialization had led to the continued use and abuse of human life and human person. Issue at the beginning of life is peculiar because it involves: mother/woman, father/man and fetus that cannot give consent, has no wishes and cannot defend itself. Nurses in this regard must be able to inculcate in the minds of those proxies to act in and for the best interest. Natural reproduction The female ovaries expel the mature egg towards the Fallopian tubes every 28 days. The male’s testes produce the sperms which are expelled at ejaculation. With the conjugal act the perms are deposited in the vaginal canal. The sperm travel up the uterus into the uterus into the Fallopian tubes and there fertilize the egg. The fertilize egg (mean the embryo) travels down to the uterus where it is implanted, develops, grow (embryo, fetus) after 9 months the baby is born. Principles 1) Inviolability of Life. All human from the moment of conception (fertilization) and through all subsequent stages is sacred. Thus, all have the duty to affirm, respect, love and 2) 3) 4) 5) 6) - - - defend it. Violation of this principle occurs like in: abortion, in vitro-fertilization and stem cell research. Stewardship. Man msut take care, cultivate, creatures within the creature’s innate nature and teleology and within man’s knowledge and understanding. Violations arises in: surgical sterility, substitution of reproduction, use of hormones, intrauterine devices (IUD) donation of sperm or egg genetic manipulation. Double Effect. A foreseen evil effect may be allowed if the foreseen intended good effect is greater than and does not result from the evil effect. This is applied into maternal-fetal conflict, removal of diseased organ like in ectopic pregnancy, anencephalic ifants. Nonmaleficence. Do no and risk no harm. This is applied into: sterilization, hormones psychological harm psychological and financial effect of new technologies. Beneficence: do good and provide a benefit. This applies when removing diseased organs, facilitating pregnancy, educating on responsible parenthood. Respect for Person. 1) Not to be denatured/destroyed. Issues/ and violation arises in: artificial methods of reproduction (like: IVF and AID or AIH), cloning. 2) to be an end and not a means to an end. This happens in contraceptions, commodifications of sperm/egg, uterus dysfunction, and embryonic manipulation. Assisted reproduction The right to procreate is limited by man’s nature. Artificial methods that help the conjugal act and ultimately reproduction are praiseworthy. Like, the use of folic acid, sex education, fertility awareness and planning, fertility drugs or hormones, viagra (for sexual dysfunction) microsurgery to correct reproductive organ defects, delivery with forceps, these assisted reproductions abide with the bioethical principles. Artificial insemination by AIH/AID including zygote implantation into fallopian tube (ZIFT), intracytoplamic sperm injection (ICSI) replace the conjugal act and are illicit. In-vitro fertilization and embryonic transfer (IVF-ET) In IVF-ET the gametes are separately harvested, in number of eggs are fertilized in ‘Patri Dish’ some zygotes are implanted into the mother, and unwanted embryo may be removed. This is not in conformity with the following principles: a) Inviolability of Life (some unwanted zygote are allowed to die) b) Stewardship (the procedure is artificial and it substitutes the conjugal act) c) Nonmaleficence (the baby may develop the ‘genealogical bewilderment syndrome’, also, if sperm is from a donor, the unknown biological lineage may lead to incest or inherited diseases. Mothers are psychologically harm by series of unsuccessful attempt) d) Justice (if private funds are used the prohibitive cost limits availability to the rich. If public funds are used, more essential needs are abandoned) e) Respect for Person (the human body, the uterus, sperm egg becomes commodities trafficked, transferred or sold; the baby is not a gift but a product of other’s will to be disposed of as desired (the unused embryo; ‘take home’ baby in term of wasted babies are often not shared with parents) J.A.K.E 4 of 7 ETHICS – BSN 2ND YEAR 1ST SEMESTER FINAL 2021 - - - - - - - Cloning the reproduction of a genetic copy of another human being either through ‘splitting’ of the embryo’s cell or through somatic cell nuclear transfer. The latter, involved the removal of the nucleus from the unfertilized female egg and its replacement by the nucleus of a cell taken from donor. Embryos are cloned either to provide human embryonic stem cells (ES cells) as precursors for differentiated cells to treat diseased (mean therapeutic cloning) or to produce a new individual by implanting it in a woman’s uterus (mean reproductive cloning). Now, harvesting of human ES cells requires destruction of the embryo. Cloning violates: f) Inviolability of Life (embryo are destroyed in the therapeutic cloning) g) Stewardship (the process is artificial) h) Nonmaleficence (the psychological and physical risks to mother and child. In accdition the concept of the ‘family’ is perhaps destroyed) i) Respect for Person (denatured and destroyed by stockbreeding with no uniqueness ans individuality; parents were reduced to a mere provider of human ‘materials’, like, sperm, egg and uterus) Human Embryonic stem cells (Human ES cells) the production of human embryos/the use of surplus embryos from IVF or aborted embryos or frozen embryos. The isolation of the inner cell mass (ICM) which is cultured and subcultured to form colonies then cell lines must be done early in the embryonic life and destroyed the embryo (nonmaleficence). This intentional killing is morally illicit. Thought the end may be praiseworthy as in a regenerative medicine, it cannot justify the means (double effect). To use commercially available or supplied ES cells obtained from them is proximate material cooperation with scandal in the act of embryo destruction (respect for person and nonmaleficence). Prevention of reproduction There are two ways by which reproduction may be prevented it is through contraceptive and abortive. There are some obvious reasons why other people choose this methods, one is space pregnancy, health, economics, unreadiness, no desire to be obligated to try to have children and others. Contraception any action which in anticipation of the conjugal act (castration, tube ligation, vasectomy, oral or parental hormones to prevent ovulation) or in its accomplishment (like, spermatocides in creams, jellies, foams or suppositories, coitus interuptus, condoms, diaphragm, hormones which thicken cervical muscus) or in the development of its natural consequences (like IUD, abortion, fetal reduction) whether as an end or means, prevents the creation of new life (anti-life). Contraceptives treat fertility as a negative value that should be suppressed. It vilates or it is nonconformity to: a) Inviolability of life (drugs and devices that inhibit fertilized ovum transport to and implantation in the uterus or its development are abortificient. They kill the fetus. b) Stewardship (it promotes hedonistic mentality with refusal to accept the reproductive responsibility of sexual or to recognize a new human being. (perhaps as god is the final Creator) c) Nonmaleficence (castration removes a healthy organ, tubal occlusion or ligation and vasectomy prevents a - - healthy function. IUD promotes infection as well. Contraception as well promotes a premarital sex, extramarital sex, or homosexuality. d) Respect for person. (to have one spouse use the other spouse as a means for one’s satisfaction or pleasure is a sign of disrespect) Abortion the process of deliberately terminating pregnancy with the resulting death of an entity or it is a process of deliberately terminating pregnancy at any stage of its development. Types of abortion: • Direct abortion or induced: it a kind of abortion with the intentional of immediate purpose of ending or destroying the fetus at any stage of after its conception. • Indirect abortion is a process of terminating pregnancy directly in which the moral object of the action is the therapy of the mother and the death of the fetus is a side effect that is inevitably unavoidable effect. Ex., removal of pathological tube containing a fertilized ovum in an ectopic pregnancy, removal of the cancerus gravid uterus. This act is justified by the principle of double effect. Obviously direct abortion violates the principles of natural reproduction. Abortion is done through: a) Injection with concentration saline (salt) (it is an injection of a concentrated saline solution into the their mothers womb. It burns their skin off them while were still alive the babies breathe it in and swallow it, frying their insides. Some of babies were born alive despite this torture and are then ‘disposed of’) b) Dilation and evacuation dilation (this is characterized by using a suction tube to remove the fetus and placenta) c) Hysterotomy (abortion by caesarian surgery) d) Vacuum aspiration (is a method by suctioning of the lining of the uterus through the use of a thin and flexible tube inserted through the opening of the cervix) Care at the Promotion of Life: Organ Transplantation and Donor - Advance in surgery and introduction of new drugs have led to the steady growth of organ transplantation and donation. The removal of the organ from one being and its implantation into another has saved lives or made lives better. Unfortunately, organs are scarce resource. - Thus, many who need new organs die while on the waiting lists. This lack of organs has led to abuses such as robbing, maiming, or even killing of donors, commercialization of organs by health care givers, middlemen or institutions and coercion exploitation of disadvantaged donors or needy recipients. It is in the abuse that violation occurs. • • • • • Terms to consider Organ donation means the giving of tissue/organ/body by a person to another person or to an institution Donor the given who may be a cadaver (with an assumptive document by the donor when still alive or by proxy) or a living person (either by relatives, non-relative) Vendor is a person who exchange their organ for money Recipient the receiver of the organ given by the donor or institution; a recipient who pay the organ is a buyer Organ transplantation means the transfer or the planting across of organ from donor/vendor to recipient/buyer J.A.K.E 5 of 7 ETHICS – BSN 2ND YEAR 1ST SEMESTER FINAL 2021 • • - - 1) 2) 3) 4) - Xenotransplantation is the planting of an organ from animal organ to human beings. Allotransplantation it is the transplantation of the organ from one body to another body of the same species. Organ donor Our main concern is to care life that is the life of the donor. The principle stewardship and nonmaleficence state that man must take care of his body and do no harm to it. If the donor is the cadaver, harvesting an organ will do no harm. If the donor is living, taking away a healthy organ is not taking care one’s body: no life is saved, no health is restored. Removal of organ may even be mutilation. However, a very proportionate reason and a meritorious act my override the rule of stewardship and nonmaleficence. The rule of unselfish love, solidarity love of neighbor, beneficence, and charity these may supercede the rules of stewardship and nonmaleficence. In such a case it is praiseworthy, for it takes what it means to belong to a human society that we are fulfilling our duty to one another (deontological duty) and to contribute to the goal of medicine (healing). By this it makes the giver a better person. Still in spite of its meritorious promise there are some requirement before an organ may be considered moral/bioethically acceptable: The harm and risk must be minimal and proportionate to the benefits to be derived. Things need to be considered: a) Accurate definition of death must be followed and observed b) The dying cannot be killed c) The organ to be removed must not be a necessary condition for life or for personal procreation, like, brain and gonads d) An part of the body that can easily be regenerated can be given such as blood, hair, bone marrow e) A second kidney or a portion of the liver these are nor necessary for the personal or procreational identity The donor must be care for before, during and after the donation. This includes the following consideration: a) Proper screening b) Standard of health care c) Reimbursement of medical expenses d) Disability and livelihood lost (burial expenses of the cadaver) e) Prevention of discrimination in job f) Prevention in community acceptance The intrinsic worth and dignity of the donor must be respected. The following must observe: a) Free and informed consent must be given b) Information given should include process of matching, the chance of success of the transplant and permission to refuse c) Financial need and ignorance make te marginalized vulnerable to exploitation In case of cadaver, consideration must be observed: a) consent for the donation must be given or obtained specially person that met an accident Organ Recipient Stewardship dictates that in case of serious illness man has the right and the obligation to take necessary measures to promote life and health. - - - - - A new organ may preserve life of the person. To the extent that if it is available one has a right to and obligation to get it. Some bioethical consideration are required for it to be morally and bioethally accepted: 1) respect for autonomy must be allow the recipient to choose how to get an organ. It requires: to give free and informed consent 2) there must be justice in allocation. Justice as equal benefits for everyone in need would dictate giving nothing to anyone and letting everyone die. It is pointless and harms all.. the following must be consider: a) The criterion for judging equality is based on the chance of success b) The ability to pay the costs of the transplant and the expensive anti-rejection medication determines success and access c) Given the case that both are capable to spend has success and access, the first come first serve must be serve. What the nurse can do, they must contribute on the communal dialogue and public education must be given, so that the main goal of organ transplantation shift back to its true nature of: a. commodities to self love a) Commercialization to charity b) Potential donors must be protected against harm, thus become an advocate of the donors c) Educating donors that selling organ is not encourage d) Nurse should address the underlying poverty, ignorance and vulnerability of people that sells their organs; organs ‘should not be for sale’ Care at the End of Life: Euthanasia and Physician Assisted Suicide One’s values regarding life and death are reflected in how one dealt with the dying. If one cannot bear to see suffering, then one resorts to an “advance” death, such in euthanasia, suicide, or physician assisted suicide. If one sees life as the highest value with death as a form of human defeat, or if one is overly influenced by available new technology and biological idolatry then one does everything to prolong life beyond one’s one time and this is known as dysthanasia. On the other hand, if one sees death as the culmination of a good life, to be valued only until its natural end, one looks for a good death this is orthothanasia. Before proceeding to the types of death, it is important to determine first signs of the moment of death, signs of death and when to pronounce that a person is dead. Moment of death 1) Inevitable and critical moment when organism ceases to function as specified, unified, homeostatic system and becomes disorganized into a mere collection of heterogeneous chemical substance. To know that body is disorganized we must at least become sure of three things: a) That the body does not now exhibit specific human behavior b) The body does not function humanly in the future c) The body has no more radical capacity for human functions due to its lost of basic structure required for human unity J.A.K.E 6 of 7 ETHICS – BSN 2ND YEAR 1ST SEMESTER FINAL 2021 - 2) 3) 4) 1) 2) The third reason is necessary since medical experience had shown that persons who are in coma nevertheless have sometimes recovered full human consciousness. Such resuscitation is possible, however, after true human death some cells or even organs of the human body for a time by artificial respirator, continue to exhibit some life functions but these functions are not those of human organism but simply a residual life at level of organization like a plant or animal. Thus, the essential point of determining human death is not to decide whether any life is present, but whether human life in the most radical sense of a unified human person is still present. Life force of cell is no longer united to the matter with which it was at any times united. Religious orientation, the separation of the body and the soul (medically, it is understood as, body’s lack of sensation and self-movement. The lose of touch irrevocably with a person who previously was able to communicate and to share our human community of thought, of love, of freedom and or creativity. Signs of death Human organism is irreversibly dysfunctional and dead Less conclusive, absence of breathing and heartbeat Now, the signs are not a guaranteed bases and signs of death due to some technological advancement that is perfected to aid the lungs and heart to functions artificially as in resuscitation. Such mechanism of resuscitation restored back and sends blood through the body, even if after the unity of the body cease to exist. Be that as it may, it does not lead to a conclusion that an individual organ simulates unity, unity or organism is no longer present because the organs would cease to exist right away if the mechanism is removed. Thus, an artificial sustained heart and lung activity is not a proof that human life still remains. That is why as long as this heart and lung is sustained by mechanical device that runs it artificially the traditional bases of death is impossible to verify. Thus, we ask the question? What then is the basis or are there other clinical signs that can be used not to constitute a new definition of death rather as an alternative, complementary ways the same essential fact, namely, the irreversible cessation of spontaneous heart and lung functions. - Aside from the new technology used, another reason is the possible organ transplant of heart and kidney. It is said to be that the success of transplanting of heart will likely to be very successful if the organs to harvested from a body through which blood is circulating. Hence, surgeons, kept the body alive in the respirator. So then, how is it possible to be sure that the donor is in fact dead? Signs of a dead person 1) Cardiovascular clinical signs (this is used when the person is not attach to respirator. Thus, reliance on technology must be moderated rather than encourage) 2) The new clinical sign must be ascertained by the well-trained professionals (basis must be properly observed. That is for no less than 24 hours when it uses the eeg or electroencephalogram as it is done in the usa: harvard criteria for brain death of 1968, this is used to person who is under a hypothermia and drug-induced coma. But today, short intervals is now allowed within 6 hours, and the eeg is being - - - - - replaced by an angiogram it is an apparatus to test the blood flow in the cerebellum of the patient) Types of Death Euthanasia An action/omission which of itself or by intention causes death, in order that suffering may be eliminated. It procures/imposes death before one’s time. Euthanasia is popular for a variety of reasons: a) Utility: the economic constraints from the escalating health costs for the growing elderly population especially chronically ill, disabled. b) Hedonism: when quality of life is poor or life is a burdensome and useless then the person can be killed. Since patient who see themselves as a burden to others are guilty to be alive. c) Autonomy: a request for an early death may be an attempt of the patient to regain control: even if it be only in deciding when to die, it is practicing the “right to die” Types of Euthanasia: a) Voluntary and involuntary (patient’s initiative) b) Active and passive (healthcare provider’s initiative) Human life must be promoted because we are as stewards of it. Filipinos have seen that disabled newborn as “good luck” and caring a sick person is a privilege. In solidarity, one can’t abandoned, replaced, worst of all, kill another person. May it be in the name of economy, practicality, compassion or autonomy. procuring death is a perversion of a diseased society made worse if done by a family or healthcare provider. It is then a betrayal of the trust and respect that health care providers are known as healers. It harms the victim and at the same the survivors in the spirit of oneness to the one that passway. Dysthanasia the delaying or postponing death beyond its natural time by all means available. Dysthanasia is popular for the following reasons: a) Doctor’s training (reasons: treating is more comfortable than not treating, doctor’s felt guilty to abstain, death of patient is seen as a failure of management) b) Technologic imperative (reasons: advances and success pushes the doctor to use everything, that is, malignant over-diagnosis and over-treatment. It is also biology rather then personhood is the object of medical attention) c) Ignorance (reasons: proxy’s are unaware of the distinction between killing and letting die; lack of information with regard on prognosis pain high quality of end of life care, the best place to die) d) Hospital culture (reasons: rights of patients are considered as preference rather than directives) e) Fear (reasons: doctor’s worry about on the accusation of legal liability and malpractice if everything were not done) f) Philippine culture (to add in the filipino hospital context) (reasons: the filipino non-confrontational attitude makes all concern hesitate to hear ‘badnews’, instead the ‘status quo’ is the main focus) Living should not be a penalty to be prolonged at all cost. To cause suffering unnecessarily in unworthy of trust and respect the healthcare provider has. Priority of using the last moment of life must be given to finish one’s own responsibilities to others. J.A.K.E 7 of 7