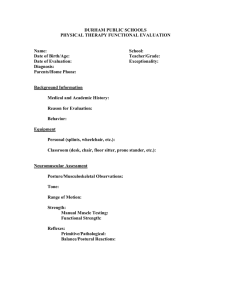
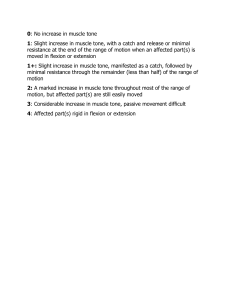
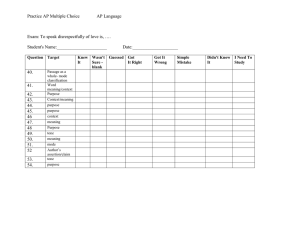
16-10-2014 CEREBRAL PALSY Prof. V.P.Sharma M.S.,(Ortho), DNB(PMR), .FACS, FICS, FIMSA, MAMS, PG (Spine-Aus.) Professor Deptt. of Physical Medicine & Rehabilitation K.G. Medical University, Lucknow CEREBRAL PALSY • C.P. refers to a disorder of motor function resulting from a non progressive brain lesion occurring before the brain is fully mature. C.P. refers exclusive to the motor dysfunction May also have – Cognitive dysfunction seizures or • Lesion is static, symptoms often change with time. • Eg. Hypotonia to hypertonia • increasing dystonia with age • Bony deformities • Contractures Classification 1. Limbs involved - Monoplegia Diplegia Triplegia Quadriplegia Hemiplegia 2 Tone - Hypotomia Spasticity 3 Associated Movement Disorders Dystonia Chorea Athetosis Ataxia Assessment of spasticity • • • • Evaluation of muscle tone R.O.M. Associated movements disorders Psycho Social Assessment Physical and occupational therapy 1. Spastic – – – – Passive ROM Active ROM Spinal mobility Use of varied and differential movement pattern incorporating varied speed and directions – Equipment to aid with weight bearing movement and position transitions. – Promotive muscle Elongation as well as joint mobility & stability Athetoid • Postural tone and balance • Promoting midline & Symmetrical muscle control • Small graded movements Hypotonic • • • • Antigravity positioning of head Trunk control Promoting automatic reactions Stabilization of joins Treatment According to age Infancy and toddler • Optimal movement patterns and postures during daily care activities such as feeding, playing , carrying, toileting and movement. • Adaptive equipments • Special strollers • Bath chairs • Feeding equipments • Fist, hand or limbs splints Pre-school• Promote skill acquisition for independent function. • Therapy promotes movement patterns. strength, endurance and Mobility issues wheel chairs crutches, walkers, strollers, car seats school chairs, splints and orthotics Schooling • • • • Architecture adaptations Home modifications Installing wheel chair lifts Classroom accommodations Ambulation Sports Formal Evaluation tools • Modified ashworth scale (MAS) • Measure resistance to passive movements in upper/lower limbs • Goniometer measurements PROM / AROM • Gross motor functional measure • Assess current level of function and provides goal for treatment. • Paediatric evaluations of disability inventory. • Functional skills in the areas of mobility • Self care • Social functions • Strength measurements by dynamometers Facilitation of movement patterns • Neuro developmental training NDT/ Bobath • Inhitit abnormal muscle tone and primitive reflaxes • Facilitate normal movement patterns via postioning and handling techniques that promote sensation of normal movement • Emphasis is on acquiring functional skills • Weight bearing • Weight shifting • Normalizing tone Electrical stimulation • • • • • • • • • • • FES Other Therapies Strengthening / Stretching Serial casting Functional Activities Dynamic approach repetition of activities by the patient Adaptive equipments Sealing system Walker Canes Splinting low temperature thermoplastics Oral Pharmacotherapy • • • • • • • • • AIM Spasticity Associated movement eg. Dystomia CNS acting Benzodia zepines Diazepam Clonazepam Lorazepam Tizanidine Baclofen PeripheralDantrolene Benzodiazepines • Acts via inhibitory neuro transmitter GABA in spinal cord • Effect relief in painful muscular spasm Improvement in sleep Long term muscle tone Anticonvulsiant property • Side effect Habituation Sedation Secrctions Rebound seizures with abrupt withdranwal Baclofen Action on GABA receptor in spinal cord • Effect Toletrated long term • Muscle tone / Active Passive • Side effect Sedation Truncal hypotomia Change in bladder habits Clonidine quanfacine Tizanidine • Effect - Aplha 2 adrenergic effects - Anti hypertensive - Treat movement disorder & eg tics Dantrolene • works directly on the sarcoplasmic reticulum of muscle and is effective in decreasing muscle tone • Side effect - Muscle weakness - GI upset, fatigue - Hepato Toxicity Intrathecal Baclofen • In patients with spasticity of cerebral origin • Continuous infusion of baclofen in intrathecal space Surgery • Maintain mobility & Stability of joints – Surgery at hip when subluxation or abduction less them 300 Bracing • Improves function – prevent worsening of contractures – Prevents recurrence of deformities after surgical correction Future Direction • Treatment for CP with focus on prevention of CP as well as effective and permanent at the level of brain. Treatment occurs multidisciplinary treatment. most approach effectively to with assessment a and 1. The commonest etiologies for cerebral palsy include all of the following except, I. Prematurity II. Cerebral hypoxemia III. Vitamin C deficiency IV. Hyperbilirubinemia 2. Which of the following is not a Pre-natal cause of C.P., I. Prolonged and difficult labor II. Premature rupture of membranes III. CNS infection (encephalitis, meningitis) IV. Multiple pregnancies 3. Which of the following scale is used for assessment of spasticity- I. GCS II. MAS III. AS IV. AIS 4. Which of the following is not a centrally acting anti spastic medication, I. Diazepam II. Tizanidine III. Dantrolene IV. Baclofen 5. Among the following which is not used for spasticity management in C.P., I. Stretching Exercises. II. Bracing. III. Baclofen IV. Anti spasmodic drugs.