Leukemia, Lymphoma, Myeloma, Thrombocytopenia Study Notes
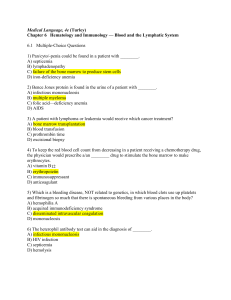
advertisement

Leukemia Background ● ● ● Etiology ● Group of cancer affecting the blood and blood forming tissues of ○ Bone marrow ○ Lymph system ○ Spleen Affects all age groups Accumulation of dysfunctional cells due to loss of regulation in cell division Combo of genetic + environment ○ Abnormal genes ○ Chemical agents, chemo drugs, virus, radiation, immunologic increase Clinical Manifestations Cause: bone marrow failure or infiltration of leukemia to tissues ● Bone marrow failure by overcrowding of abnormal cells and not enough production of bone marrow elements What occurs… ● Anemia ○ Sx: fatigue, SOB, pallor, tachycardia, systolic murmurs ● Thrombocytopenia ○ Sx: increased risk for bleeding, petechiae, ecchymosis, bleeding ● Decreased WBC ○ Sx: increase risk for infection, fever, lymphadenopathy (swelling of lymph nodes) Leukemia can travel to other organs causing… ● Splenomegaly ● Hepatomegaly (w/ or w/o jaundice) ● Lymphadenopathy ● Bone pain ● Meningeal irritation ● Oral lesions ● Seizures, disorientation, confusion Diagnostic Studies First do (to dx and classify)… ● Peripheral blood evaluation ● Bone marrow exam Other options include… (cells outside of blood and bone marrow) ● Lumbar puncture ● PET/CT scan Interprofessional Care GOAL: ATTAIN REMISSION -how to attain it… 1. Combo drug therapy 2. Chemotherapy Stages of chemo: 1. Induction a. Goal: bring about a remission b. Destroy all leukemia cells in 3 areas to restore hematopoiesis (blood cell production) i. Tissues ii. Peripheral blood iii. Bone marrow c. Normal findings: pt will become ill from.. i. Neutropenia ii. Thrombocytopenia iii. Anemia 2. Consolidation (postinduction or post remission) a. Start after induction b. Time frame: months c. Goal: eliminate remaining cells that may not be clinically or pathologically evident 3. Maintenance a. Goal: Keep body free of leukemia cells Combo drug therapy 1. Corticosteroids 2. Radiation therapy a. Total body radiation (TBI) prepares pt for bone marrow transplant 3. Immunotherapy and target therapy a. Use for specific types 4. Hematopoietic stem cell transplant (bone marrow transplant) a. GOAL: eliminate all leukemia cells using combo of chemo w/ or w/o TBI i. End result: eliminates pt stem’s cells are replace w/ new ones b. Categories i. Allogeneic 1. Complications (cells did not originate from themselves) a. Graft v. host disease b. Relapse of leukemia c. Infection & sepsis ii. Syngeneic iii. Autologous c. Source of cells i. Bone marrow ii. Peripheral blood iii. Umbilical cord blood Nursing Management ● ● ● ● ● ● Ask for health hx ○ Questions to ask include: ■ Exposure to toxins ■ Chromosome abnormalities ■ Frequent infections Perform routine assessments Monitor lab results ○ Look at platelet count, Hgb, Hct, WBC Monitor for chemo S/E ○ N/V, hair loss Monitor for bleeding Institute neutropenic precautions ○ Watch your diet ● Education 1. 4. 5. Med management a. Pt should recognize acute S/E of tx are temporary b. Review long term A/E i. Fertility Infection prevention a. HANDWASHING! Neutropenic precautions a. Avoid uncooked food!!!! i. Fresh fruit, veggies, raw meat Bleeding precautions Anticipated course of illness (set realistic goals) ● ● ● ● Increase risk for infection Risk of sepsis Relapse Tx related death 2. 3. Complications Additional Info ○ Limit your exposure to germs. ... ○ Pay attention to your skin. ... ○ Get enough rest. ... ○ Seek medical help immediately for a fever. Address psych needs ○ Anxiety, fear, depression (common) Classifications -based on WBC ● Acute lymphocytic leukemia (ALL) ○ Common in children ● Acute myelogenous leukemia (AML) ○ ⅓ of all leukemias ■ Most of which are adults ○ Onset: abrupt, dramatic ■ Manifestations: serious infections, abnormal bleeding ● Chronic myelogenous leukemia (CML) ○ Philadelphia chromosome*** ■ Genetic marker ■ Seen in majority of cases ○ Onset: chronic, stable → acute, aggressive (blastic phase) ● Chronic lymphocytic leukemia (CLL) ○ Common in adults (old ppl) Hodgkin Lymphoma Background Etiology ● ● ● Rapid increase of abnormal giant multinucleated cells- Reed-Sternberg cells*** Males 2x more likely to have it then females** Most pt are cured Cause: unknown Factors that play a role in development: ● Infection w/ EBV virus ● Genetic predisposition ● Exposure to work toxins ● Presence of HIV infection* Spreads by infiltrating other organs: 3 main organs ● Lung ● Spleen ● Liver Additional Notes Clinical Manifestations Stages ● Involves # of lymph nodes above or below diaphragm ● ● ● ● ● Other ● Onset: gradual Initial sign: enlargement of cervical, auxiliary, or inguinal lymph nodes (cause unknown) ○ Other location: mediastinal node mass Nodes are movable and nontender Not painful ○ Unless exert pressure on adjacent surrounding nerves Asymptomatic pt Flu-like sx ○ Weight loss ○ fatigue/ weak ○ fever/chills ○ Tachycardia ○ Night sweats ○ Generalized itchy w/o lesions Sx if you have worse prognosis (B SYMPTOMS)** ● fever #> 100.4F ● Drenching night sweats ● Weight loss exceeding 10% in 6 months Non-Hodgkin's Lymphoma Background Broad group of cancers consisting of… ● B cells ● T cells ● Natural killer cells Affect all ages Etiology Cause: unknown Factors that play a role: ● Chromosomal translocations ● Infections ● Environmental factors ● Weakened immune system Clinical ● Present w/ widespread disease at time of dx Manifestations ● ● Primary manifestation includes: ○ Painless lymph node enlargement (gets big or small over time) Other sx ○ Hepatomegaly ○ Jaundice w/ liver involvement Lymphoma Background Diagnostic studies Originate in bone marrow and lymphatic structures 2 major types ● Hodgkin’s lymphoma ● Non-Hodgkin’s lymphoma (NHL) ● ● ● ● Management ● ● Complications ● ● ● ● ● Lab testing ○ Peripheral blood analysis ○ Expected findings: ■ Increased ESR ■ Hypercalcemia (bone involvement ■ Hypoalbuminemia (liver involvement) Lymph node biopsy ○ Expected finding ■ Hodgkin lymphoma= Reed-Sternberg Cell Bone marrow exam Testing specific for NHL ○ MRI ■ To determine CNS involvement ○ Lumbar punctures Tx ○ Chemo ○ Biotherapy ○ Radiation ○ Sometimes phototherapy and topical therapy Nursing care focuses on managing ○ Problems related to disease ○ Pancytopenia ○ S/E of therapy ○ Psychosocial considerations ■ Physical & spiritual consequences ■ Fertility issues ■ Long term effects of therapy Infection Sepsis Tx failure (relapse of disease) Increased risk for secondary cancer later in life Tx-related death Multiple Myeloma Background Cancerous plasma cells proliferate in bone marrow —> destroy bone Accounts for 18% of all hematologic cancers ● Occurs between ages of 65-74 Etiology Cause: unknown Factors that play a role: ● Exposure to organic chemicals (benzene) ● Herbicides ● Insecticides ● Viral infections (HIV) increase risk* Involves excess production of plasma cells creating monoclonal antibodies (monoclonal= one of a kind= ineffective) ● Infiltrates bone marrow ● Monoclonal proteins (M proteins)- consists of light and heavy chains ● Bence Jones- proteins that are the light chain part of monoclonal antibodies ○ Manifestation in urine Clinical Manifestation ● ● ● ● Diagnostic Studies ● ● Treatment ● Onset: slow and subtle (gradual) Main sx: skeletal pain ○ Location: pelvis, spine, ribs Development of diffuse osteoporosis (M-protein begins to destroy bone) including… ○ Osteolytic lesions occurring in skull, vertebrae, long bones, ribs ○ Vertebral compression→ vertebral collapse of vertebrae + spinal cord compression Calcium loss from bones causes hypercalcemia ○ Hypercalcemia sx include ■ Renal, GI, neuro problems ● Polyuria ● Anorexia ● Confusion ● Heart problems Lab testing ○ Increased plasma cells in bone marrow ○ M-protein found in blood + urine ○ Pancytopenia (deficiency in WBC, RBC, platelets) ○ Hypercalcemia ○ Bence Jones protein in urine ○ High serum creatinine (measure of how well your kidneys are performing their job of filtering waste from your blood) Radiologic (show thinning of bones or fractures) ○ MRI ○ PET ○ CT scan ○ Skeletal bone survey Corticosteroids ○ Prednisone ● ● ● ● ● Interprofessional + Nurse Management ○ Methylprednisolone Chemo Immunotherapy Target therapy Bisphosphonates ○ For tx of osteoporosis that ends of developing Bone marrow transplant NO CURE! Work on tx the sx → produce remission → prolong life Goals: 1. Control pain 2. Prevent pathologic features Major focus of nursing care= SAFETY ● Due to bone involvement and bone breakdown ● Considerations ○ Use caution when moving and ambulating pt ■ Potential to cause a fracture Tx options 1. Immunotherapy and target therapy 2. Ambulation (helps bone reabsorb more calcium) 3. Hydration (tx of elevated calcium, prevent kidney failure) a. Give IV fluids i. Goal: maintain urine output of 1.5-2L/day 4. Use of braces a. To help with pain 5. Prompt assessment/ tx of infections 6. Psychosocial needs If final and acute, pt is unresponsive to tx ● Initiate convo about palliative or hospice care Complications ● ● ● ● ● Hypercalcemia Dehydration Fluid and electrolyte imbalance Renal damage Neurologic changes (peripheral neuropathy) Patient education ● ● ● Focus on bleeding risk and infection risk Prevention of fractures When to call HCP Thrombocytopenia Background Normal Hemostasis (stoppage of blood flow) ● Involves the vascular endothelium, platelets, and coagulation factors ● Function ● Etiology ○ Stop hemorrhage ○ Repair vascular injury Abnormalities (disruption in components) ○ Bleeding ○ Thrombotic disorders Reduction of platelets below 150,000/ul (150 x 10^9/L) [NORMAL PLATELET COUNT : 150k to 450k/ul) Low platelets result in… ● Abnormal hemostasis ○ Prolonged bleeding from minor trauma ○ spontaneous bleeding where there is no known cause Cause: genetic or acquired 1. Inherited 2. acquired* a. Due to ingestion of certain meds b. Immune thrombocytopenia purpura (ITP) i. Most common ii. Abnormal platelet destruction iii. Manifestation 1. Acute in children 2. Chronic in adults iv. Onset from… 1. Viral infection 2. H. pylori 3. Autoimmune (lupus) v. Etiology 1. Shortened platelet survival 2. Antibodies mistake as foreign bodies causing them to be killed off c. Thrombotic thrombocytopenic purpura (TTP) i. Characteristics 1. MAHA (anemia) 2. Thrombocytopenia 3. Neurologic changes 4. Fever (absence of infection) 5. Renal problems ii. Uncommon iii. Enhanced aggregation of platelets that form into microthrombi iv. Medical emergency! 1. Bleeding and clotting occur at same time v. Manifestations 1. Females 2. Healthy adults vi. Onset from… 1. Autoimmune 2. Ingestion of certain meds 3. Pregnancy 4. Preeclampsia 5. infection d. Heparin-induced thrombocytopenia (HIT) i. ii. iii. iv. Clinical Manifestations Diagnostic studies Assoc. w/ use of heparin Life threatening! Onset 1. 5-14 days after heparin therapy Characteristics 1. Platelet count < 250k 2. Platelet destruction 3. Vascular endothelial injury 4. VTE*** (DVT) Symptomatic ● Common sx: bleeding (mucosal or cutaneous) ○ Results in… ■ Petechiae ● Flat, small, red brown microhemorrhages that develop in the skin ■ Purpura ● Many petechiae ● Pain and tenderness present ■ Bruising (ecchymosis) ● Due to hemorrhage Major complication: hemorrhage ● Onset ○ Acute (drastic) ○ Subtle (less noticeable) ■ First detection the anemia from blood loss ○ Internal ■ Manifestations ● Weakness ● Dizzy ● Tachycardia ● Hypotension ● Abdominal pain ■ Prolonged bleeding after routine procedures ○ External ● Areas affected ○ Joints ○ Retina ○ Brain ● Monitor for ○ Epistaxis (nose bleeds) ○ Gingival bleeding ○ Joint bleeding ○ Brain bleeding ● ● ● Decreased platelet count on CBC <150,000/ul ○ Prolonged bleeding count <50,000/ul ○ Spontaneous hemorrhage count <20,000/ul Hx and assessment* Lab testing (PT, APTT) ○ Findings: normal Interprofessional care Nursing Management Tx based on cause 1. ITP a. Corticosteroids b. Immunoglobulins c. Monoclonal antibodies d. Removal of spleen (splenectomy) 2. TTP a. Corticosteroids b. Immunosupressive therapy c. Plasmapheresis 3. HIT a. STOP HEPARIN (including fushing) b. Maintain anticoagulation w/ other meds (ex: warfarin) i. Only start warfarin if platelet count 150,000/ul c. Plasmapheresis- if severe clotting d. Considerations i. Never give heparin again (lovenox) Avoid aspirin or other drugs that affect platelet fx or production ● Discourage use of OTC meds ○ Especially those caused acquired thrombo and reduced platelet fx (ASPIRIN) ○ Have pt check with HCP ● Have pt know when to seek care if they notice S/S assoc. w/ bleeding ○ If they see prolonged nosebleeds, petechiae ● Observe early sx if pt receives chemo ○ Thrombo. Known S/E of chemo In acute care settings.. 1. Assess for bleeding*** a. Any bleeding needs eval and tx GOAL: PREVENT OR CONTROL HEMORRHAGE 2. Admin platelets per orders 3. Monitor labs a. Platelet count b. Coagulation studies c. Hbg, Hct 4. Use small gauge needles if need to do SUBQ injections a. Apply direct pressure for at least 5-10 min after injection b. Can use ice pack 5. AVOID IM! 6. Teach importance of following self-care measures to reduce risk of bleeding Anaphylaxis Background ● Hypersensitivity reactions ○ Immune response is overreactive against foreign antigens or reacts against its own tissue→ tissue damage ○ Classifications based on ■ Source ■ Time sequence (immediate or delayed response) ■ Immunological mechanisms causing injury ○ Types ■ IgE-mediated-TYPE 1 ■ Cytotoxic- TYPE 2 ■ Immune complex- TYPE 3 ■ Delayed hypersensitivity-TYPE 4 ○ TYPES 1-3 ■ Immediate ■ Examples of humoral immunity ○ TYPE 4 ■ Delayed ■ Related to cell-mediated immunity Type 1 hypersensitivity reaction ● acute , potentially life threatening ● Occur only in ppl who are highly sensitized to specific allergens ○ Sx include ■ Smooth muscle contraction ■ Increased vascular permeability ■ Vasodilation ■ Hypotension ■ Increased secretion of mucus ■ Itching Genetic predisposition o the development of allergic diseases Etiology Common allergic rxns are: ● Food ○ Milk ○ Peanuts ○ Tree nuts ○ Fish ○ Chocolate ○ Strawberries ● Insect stings ● Latex ● Meds (common penicillin)**** Clinical Manifestations When localized… ● Cutaneous wheal and flare rxn ● Occurs in min or hrs ● Usually not dangerous When systemic… ● Occurs within min ● Life threatening ● ● ● Diagnostic studies ● ● ● Interprofessional Care ○ Due to bronchial constriction ○ Airway obstruction ○ Vascular collapse Dyspnea Bronchial edema and angioedema ○ Swelling in the deeper layers of skin ■ Often around face and lips Progression to shock ○ Rapid or weak pulse ○ Hypotension ○ Dilated pupils ○ Cyanosis ○ LOC or death ← if not tx Lab testing ○ CBC w/ differential ■ Elevated eosinophils ○ IgE level ■ High antibodies Skin allergy testing ○ Allergen applied to skin prick or scratch or injected into skin (ID) ○ Causes wheal and flare responses if positive allergy Blood allergy testing ○ RAST testing ■ Use for pt that present with allergies to medications, foods, etc Emergency tx ALWAYS starts w/ ABC ● Ensure and establish a patent airway ** ● Assess respirations ● Establish IV access for emergency fluids/med ○ to tx hypotension Expected meds ● Drug of choice: epinephrine** ○ Given parenterally ■ IM ● Pt over 60 kgs: give 0.3-0.5 mg ○ Give in mid-outer thigh ○ Repeat every 5-15 min ■ IV Make sure to know what meds pt is on (beta blockers= metoprolol) ■ Resistance to tx w/ epi Give high flow oxygen ○ Usually 8-10L/min via face mask ■ Give up to 100%, if needed Nebulized albuterol tx ○ For bronchospasms resistant to epi IV benadryl or diphenhydramine ○ For itching or urticaria (hives) Corticosteroids ○ Given IV ○ Common med: methylprednisolone ○ ● ● ● ● Nurse management Teaching 1. 2. 3. 4. Recognize S/S of anaphylactic rxn Maintain a pt airway Admin meds (ex: epi) a. When recommended or ordered Recognize and tx shock w/ oxygen, fluids, necessary meds ● ● ● ● Have pt try to identify what the allergen is and cause for the response Referral to specialist Teach to min exposure to allergen Teach epi self-injection then call 911 ● Pathogen or microorganism which causes disease, invades the body, multiplies and causes disease, usually causing harm to the host ○ S/S results from the activity of the pathogen which triggers inflammation and other immune responses Pathogen ○ Agents that cause disease ■ Includes bacteria, fungi, virus, protozoa, prions Normal flora protect the body by preventing overgrowth of other microorganisms ○ Under certain conditions and circumstances, imbalance occurs and results in disease Categories ○ Localized ○ Disseminated ○ Systemic Infection Background ● ● ● Types 1. 2. Emerging and reemerging a. Bacterial: H. pylori b. Viral: COVID, flu c. Parasitic: cryptosporidium parvum Antimicrobial-resistant infection a. All pathogenic organisms are highly adaptable 3. Antimicrobial resistant infection ● ● ● HAI ● b. Change and become resistant to tx c. Think MRSA and VRE Health care-associated infections (HAIs) a. CAUTI b. CLABSI c. C. Diff d. MRSA e. Pneumonia Rates have increased ○ HCPs have contributed: ■ Treat viral infections with antibiotics ■ Succumb to patient pressure for medications ■ Use inadequate drug regimens to treat infections ■ Use broad-spectrum or combination agents when first-line agents could be effective Patients have contributed: ○ Skip doses of antibiotics ○ Stop antibiotics before the full course has been taken ○ Save and use antibiotics for “later” Also consider: Limited resources and access to care can result in inadequate treatment of infections Prevention ○ Standard precautions ○ Transmission-based ■ Airborne ■ Droplet ■ Contact Sepsis Etiology Clinical Manifestation Diagnostic studies Localized infections which lead to bacteria entering the bloodstream Systemic inflammatory response to documented or suspected infection Progresses to organ dysfunction ● ● ● ● ● ● ● ● ● ● Presence of infection AND: Altered mental status (AMS) Fever and chills Tachycardia Hypotension (especially SBP <100) Core body temp less than 97 (Hypothermia) Extreme/unexplained pain Tachypnea Hyperglycemia in absence of diabetes Potential significant edema, positive fluid balance (20mL/kg) in 24 hours ● Lab testing ○ Serum and blood sepsis findings ● ■ WBC may be decreased (<4k) or increased (>12k) ■ Lactic acid increased ■ Procalcitonin increased ■ C-reactive protein increased ■ Cultures positive (blood and other samples) ○ Progression to septic shock may have indications of: ■ Decreased platelets ■ Increased PT/INR ■ Increased PTT MEWS score (modified early warning Signs/sepsis recognition) ○ The higher the #, the worse the pt outcome is Interdisciplinary care ● ● ● Treatment of source of infection If bacterial, antibiotic management Oxygen management – Sepsis (and septic shock) may indicate the presence of inadequate tissue perfusion resulting in hypoxia Nursing management ● ● ● ● ● ● Ongoing assessment of VS Assessment of early recognition of shock manifestations Fluid management Skincare Monitoring I/O, especially urine output May be transferred to ICU for invasive cardiac monitoring