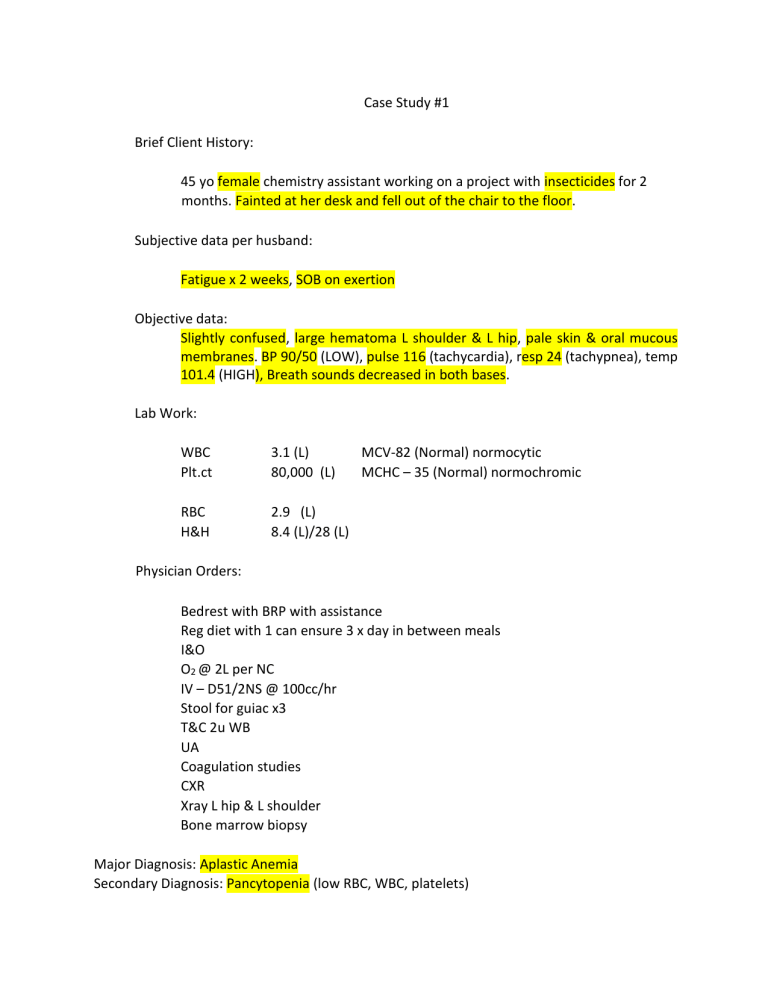
Case Study #1 Brief Client History: 45 yo female chemistry assistant working on a project with insecticides for 2 months. Fainted at her desk and fell out of the chair to the floor. Subjective data per husband: Fatigue x 2 weeks, SOB on exertion Objective data: Slightly confused, large hematoma L shoulder & L hip, pale skin & oral mucous membranes. BP 90/50 (LOW), pulse 116 (tachycardia), resp 24 (tachypnea), temp 101.4 (HIGH), Breath sounds decreased in both bases. Lab Work: WBC Plt.ct 3.1 (L) 80,000 (L) RBC H&H 2.9 (L) 8.4 (L)/28 (L) MCV‐82 (Normal) normocytic MCHC – 35 (Normal) normochromic Physician Orders: Bedrest with BRP with assistance Reg diet with 1 can ensure 3 x day in between meals I&O O2 @ 2L per NC IV – D51/2NS @ 100cc/hr Stool for guiac x3 T&C 2u WB UA Coagulation studies CXR Xray L hip & L shoulder Bone marrow biopsy Major Diagnosis: Aplastic Anemia Secondary Diagnosis: Pancytopenia (low RBC, WBC, platelets) Describe the patho: RBC’s made by the bone marrow will be associated with impaired cellular regulation. In this patients case it is caused by Insecticides 2. List the nursing diagnoses: Impaired tissue perfusion, fatigue, activity intolerance, risk for bleeding, acute confusion, risk for injury, ineffective breathing pattern risk for falls. 3. Explain the reason for each Dr. order: • Bedrest with BRP with assistance—so the client will not fall due to fatigue and she already fainted. • Reg diet with 1 can ensure 3 x day in between meals—so that she can recover with the correct nutrition needed • I&O – to make sure kidneys are working efficiently • O2 @ 2L per NC – client is having on exertion • IV – D51/2NS @ 100cc/hr – to keep fluid + electrolytes balanced • Stool for guiac x3 – check stool for blood • T&C 2u WB – (whole blood) to increase o2 carrying abilities • UA – check for blood or infection • Coagulation studies – to establish baseline of bleeding and coagulation times • CXR – check lungs for infection • Xray L hip & L shoulder – injury from falling • Bone marrow biopsy—to tell us if bone marrow is damaged or low and see what is wrong 4. What complications are likely to delay improvement and why? Infection due to WBC being low, low o2 getting thru body since her RBC are low, risk of bleeding since her platelets are low. 5. List the treatment choices including meds Erythropoietin (increase RBC production), filgrastim (increase WBC’s) blood transfusion Possible splenectomy 6. Describe the client after 2 weeks of improvement. Include physical assessment and lab data. The client will have more energy and all symptoms should have improved. RBC, WBC, Platelets and H+H should all be normal now. Case Study #2 71 year old female, slightly overweight. Felt “bad” for a month. Couldn’t get OOB today and called her son. He brought her to ER. Client too weak to talk, son is poor historian, no previous records. Client presents in the ER with: Severe weakness and fatigue. SOB, dizziness, confusion, anorexia. Denies pain, nausea, vomiting. Brief Assessment: Skin dry with poor turgor, no petechiae. Resp 28 (tachypnea), rapid & shallow. Breath sounds clear. BP 94/54 (LOW). Pulse 125 (tachycardia), weak & thread, regular. Slow capillary refill. Tongue beefy red. Lab Work: WBC 8.0 (L) RBC 3.0 (L) Hgb 7.4 (L) Hct 28 (L) MCV 69 (L) microcytic MCHC 27 (L) hypochromic Physician Orders: Admit for anemia: O2 per NC at 2L VS q4h IV‐D51/2NS @ 75cc/hr Bedrest NPO Foley to cavity drainage T&C 4 u PRBCs CXR EKG Chem profile Ask son to bring in all home meds. Case manager to assess home situation. What disease/conditions will need to be ruled out as the cause of the anemia? thalassemia, and chronic blood loss 2. What meds might you expect the doctor to order? Why? Iron supplements to help raise H+H patient could possibly need an iron transfusion to raise iron faster. 3. List the nursing diagnoses for the client. Activity intolerance, risk for bleeding, risk for injury, ineffective breathing pattern, decreased cardiac output, acute confusion, risk for falls, fatigue, risk for injury, imbalanced nutrition, overweight, impaired standing, ineffective peripheral tissue perfusion, impaired walking. 4. Describe the client after 3‐4 days of improvement. Include the physical assessment and lab work. Increased energy, no SOB, normal b/p H+H should be increasing, cap refill should be <3 sec, skin should not be as dry, client should be A+O, and have an appetite 5. List the expected outcomes for this client. Patient should start to feel better. If she is taking oral iron supplements it could take 612 months for her iron to be normal. But everything should start to improve with continued treatment 6. What complications are likely to occur and why? Reaction to iron infusion, blood loss or injury from being weak. Constipation 7. Suggest discharge orders, include meds. Continue iron supplements if taking orally, follow up why HCP for repeat labs and continued care. Call in rx to a pharmacy, teach client about iron rich foods. Case Study #3 Mr. C 73 yo male with bowel obstruction, exp. Lap. Removal of adhesions and 6 inches of colon. 2 days post‐op, he spikes a temp of 102.4(high) and treatment begins for sepsis. 1 day later c/o HA, dizziness, weakness, increased abd. Pain, gums bled when brushing teeth this AM. Brief Assessment: Abd distention, urine pink‐tinged, BP 128/84, pulse 112(tachycardia), resp 24,(tachypnea) temp 101.4. Slight oozing blood @ IV site and abd. incision You Suspect: D.I.C. Lab Work: H&H PT PTT 10(L)/34(L) 20 sec (H) 60 sec (H) Fibrinogen Platelet CT 100 (200‐400) (L) 20,000 (L) Fibrin degradation productions (FDP) 50 (less than 10) (H) Physician Orders: Bedrest Portable CXR T&C 4u WB Give 2u FFP, 10 platelet packs, 1 u cryoprecipitate, 1 u WB Bleeding continues – gauze on incision is saturated every 30 minutes. New Order: Transfer to ICU Heparin 7500u IVP, then drip 1000u/hr Repeat PTT & fibrinogen q4h and call to MD Why is heparin ordered? Why is it controversial? How is it monitored? Can be used to decrease micro clots from forming and using up clotting factors. Bc heparin is used to thin blood and the patient is bleeding out but we are trying to shock the body into doing what it should be doing and at this point you throw everything you can at the patient bc it can’t get much worse. Monitor labs and function. 2. Explain the purpose of each type of transfusion given. • Platelets—increase platelets • Fresh froze plasma—no rbc. No wbc, no platelets but helps with coagulation factor deficiency • Cryoprecipitate—man made plasma clotting factors (factor 13) help increase clotting after trauma 3. What hemodynamic, extremity and skin problems are watched for? What S&S will you assess for? Regularly access vital signs and hemodynamic status Manifestations of micro emboli so they can have cyanotic nail beds and pain. Bleeding gums and bleeding or oozing of the incisions. 4. What GI & kidney problems are watched for? What S&S will you assess for? Watching for any signs of organ failure, abdominal distention(pt has) olguria and hematuria 5. What respiratory problems are watched for? What S&S will you assess for? Respiratory distress Cardiopulmonary arrest Tachypnea, abnormal breathing, crackles 6. What neurological problems are watched for? What S&S will you assess for? Hemorrhages or infarctions of the brain. Decreased LOC, seizures, stoke symptoms, coma, decreased motor function, decreased pupil activity 7. What will you explain to the family? What is happening? Why? What is the prognosis? Be sure to use simple terminology. The prognosis is not good, but we are doing everything we can to help your family member. The client is experiencing a life-threatening condition in which the blood is using up all the clotting factors in their body, meaning his blood is causing blood clots in the small blood vessels and cutting off circulation to body and organs. This is a complication of the sepsis which is the infection in his blood. Case Study #4 21 yo single white male, non‐smoker, social drinker, works at Walmart. Presents in the ER vomiting blood Complains of: Low back pain, abd pain Fatigue, anorexia & sore mouth X 1 week Brief Assessment: Multiple bruising on extremities Spleen enlarged and tender Gingival lesions Skin pale and hot, temp 101.6 Lab Work: WBC 31.7 (h) Hgb 10.1 (L) Hct 29% (L) Plt. Ct. 16,000 (L) Physician Orders: I&O Bedrest IV D51/2NS @ 100cc/hr Bone marrow bx T&C 3u WB NGT to low gomco suction, irrigate with iced saline prn Mycostatin oral swish & swallow 3cc q6h Soft diet with 1 can Ensure 3xDay in between meals Bone Marrow biopsy was + for acute lymphoblastic leukemia Surgical placement of portacath. List the nursing diagnosis for the client: acute pain, risk for powerlessness, risk for spiritual distress, impaired tissue perfusion, risk for imbalanced fluid volume, risk for injury, nausea, imbalanced nutrition, impaired oral mucous membrane integrity, Risk for bleeding, risk for decreased cardiac output, fatigue. 2. Explain the reason for each of the complaints and assessment data: Abdominal pain: enlarged liver and spleen Fatigue: anemia Anorexia: n+V Sore mouth: dehydration Bruising: low platelets Gingival lesions: low platelets Skin pale: low H+H Temp: poss. Infection, wbc are not functional 3. What are the teaching needs for this client and his family? Leukemia is cancer of WBC or of cells that develop into WBC that are not functiona;l they invade and destroy bone marrow and they can metastasize to liver, spleen, lymph nodes, testes and brain. Teach client to monitor for evidence of infection. Hand hygiene and to try to prevent injury. 4. Describe the process of bone marrow transplantation: Bone marrow is destroyed or ablated using radiation or chemotherapy and later replaced with healthy stem cells. The body is able to resume normal production of blood cells they can use the clients own cells that are collected before chemo or they can use a donor. Without transplant client will likely die from infection or bleeding. 5. Describe the client after 3‐4 weeks of improvement. Include the physical assessment data and lab work. Should have more energy, more control over pain. Should have improvement in mouth sores. Labs will vary and still need to be checked. 6. What complications are likely to delay improvement and why? Infection or injury because risk for those are already high and their body does not have the ability to fight off infection or help itself heal.