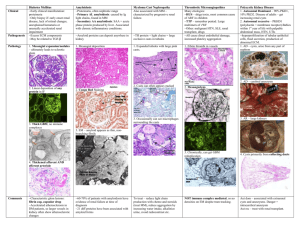
review www.kidney-international.org Renal AA amyloidosis: presentation, diagnosis, and current therapeutic options: a review Sabine Karam1, Mohamad Haidous2, Virginie Royal3 and Nelson Leung4,5 1 Division of Nephrology and Hypertension, University of Minnesota, Minneapolis, Minnesota, USA; 2Department of Medicine, University Hospitals Cleveland Medical Center, Cleveland, Ohio, USA; 3Division of Pathology, Hôpital Maisonneuve-Rosemont, Université de Montréal, Montréal, Quebec, Canada; 4Division of Nephrology and Hypertension, Mayo Clinic, Rochester, Minnesota, USA; and 5Division of Hematology, Mayo Clinic, Rochester, Minnesota, USA Amyloid A amyloidosis is thought to be the second most common form of systemic amyloidosis behind amyloidosis secondary to monoclonal Ig. It is the result of deposition of insoluble fibrils in the extracellular space of tissues and organs derived from the precursor protein serum amyloid A, an acute phase reactant synthesized excessively in the setting of chronic inflammation. The kidney is the most frequent organ involved. Most patients present with proteinuria and kidney failure. The diagnosis is made through tissue biopsy with involvement of the glomeruli in most cases, but also often of the vessels and the tubulointerstitial compartment. The treatment usually targets the underlying etiology and consists increasingly of blocking the inflammatory cascade of cytokines with interleukin-1 inhibitors, interleukin-6 inhibitors, and tumor necrosis factor-a inhibitors to reduce serum amyloid A protein formation. This strategy has also shown efficacy in cases where an underlying etiology cannot be readily identified and has significantly improved the prognosis of this entity. In addition, there has been increased interest at developing effective therapies able to clear amyloid deposits from tissues, albeit with mitigated results so far. Kidney International (2023) 103, 473–484; https://doi.org/10.1016/ j.kint.2022.10.028 KEYWORDS: AA amyloidosis; clinical presentation; pathogenesis; treatment Copyright ª 2022, International Society of Nephrology. Published by Elsevier Inc. All rights reserved. Correspondence: Sabine Karam, Division of Nephrology and Hypertension, 717 Delaware Street SE, Minneapolis, Minnesota 55414, USA. E-mail: skaram@umn.edu Received 12 July 2022; revised 26 October 2022; accepted 31 October 2022; published online 9 December 2022 Kidney International (2023) 103, 473–484 S ystemic amyloidoses are a rare and heterogeneous group of diseases that result from the ability of certain proteins to misfold and polymerize into insoluble amyloid fibrils. These fibrils are deposited in the extracellular space of tissues and organs, causing tissue damage and significant morbidity and even mortality.1 To date, 36 proteins have been associated with amyloid formation in humans.2 Amyloid A (AA) amyloidosis is derived from serum AA (SAA) protein, an apolipoprotein of high-density lipoproteins that serves as an acute phase reactant synthesized in the liver.3,4 The stimuli in AA amyloidosis usually stem from chronic inflammatory conditions, such as autoimmune diseases (rheumatoid arthritis [RA], juvenile chronic polyarthritis, ankylosing spondylitis, and inflammatory bowel diseases), chronic infections (tuberculosis and osteomyelitis), familial periodic fever syndromes, such as familial Mediterranean fever (FMF), neoplasms, and Castleman disease, among others.5 A fraction of patients with AA amyloidosis have chronic skin or other soft tissue infections related to injection-drug use (skin poppers).6 Furthermore, monoclonal gammopathies, which included Waldenström macroglobulinemia, Schnitzler syndrome, multiple myeloma, and monoclonal gammopathy of undetermined significance, have been recently speculated as a rare cause of AA amyloidosis in a French registry.7 A hereditary form of AA amyloidosis has been recently described.8 Sikora et al.8 examined a family with primary AA amyloidosis where the mutation was in the promoter of the SAA1.1 gene and not in the gene itself. The genetically affected individuals had sustained elevation in SAA levels, and all developed proteinuria, chronic kidney disease, and systemic deposition of amyloid composed specifically of the SAA1.1 isoform.8 Finally, the etiology is unknown in some cases, which are labeled as idiopathic.9,10 AA amyloidosis is the second most common form of amyloidosis behind Ig light chain (AL) amyloidosis.11 Although AA amyloidosis is a systemic disease, the clinical picture is dominated by kidney involvement.12 AA amyloidosis causes kidney dysfunction with proteinuria in >80% of cases that progress to kidney failure if left untreated.10 Previously, there were few treatment options for patients with AA amyloidosis. Fortunately, the incidence of AA amyloidosis has been decreasing as underlying inflammatory conditions and infections are increasingly better managed.13 Moreover, the advent of new drugs that target various processes involved in 473 review S Karam et al.: Renal AA amyloidosis: diagnosis and management Table 1 | Common etiologies of AA amyloidosis Entity Infections Autoimmune/connective tissue diseases Hereditary inflammatory conditions Other Type Mycobacteria (tuberculosis) Bronchiectasis Injection-drug–related infections Osteomyelitis Rheumatoid arthritis Juvenile idiopathic arthritis Psoriatic arthritis Ankylosing spondylitis Crohn disease Vasculitis (polyarteritis nodosa–giant cell arteritis–antineutrophil cytoplasmic antibody–associated vasculitis) Behcet disease Celiac disease Familial Mediterranean fever Muckle-Wells syndrome Cryopyrin-associated periodic fever syndrome Tumor necrosis factor receptor-associated periodic syndrome Mevalonate kinase deficiency/hyper IgD syndrome Cystic fibrosis Castleman disease Skin popping Malignancy Obesity AA, amyloid A. the pathogenesis raised new hope for patients. This article will review the pathogenesis of renal AA amyloidosis, its clinical and pathologic presentations, along with its treatment, with emphasis on new targeted therapies. EPIDEMIOLOGY AA amyloidosis was the first type of amyloidosis ever described and was thought to be the most prevalent form of systemic amyloidosis for hundreds of years.14 It has now been supplanted by AL amyloidosis, particularly in the Western world, likely the result of better treatment of the various underlying etiologies. Among 474 cases diagnosed by renal biopsy at the Mayo Clinic between 2007 and 2011, AA amyloidosis represented only 7% of the cases.15 In a review of 16,175 tissue samples of amyloidosis typed by mass spectrometry over 11 years, AA type accounted for only 2.9% of cases.16 The incidence of AA amyloidosis is z1 to 2 cases per million person-years.5,17,18 Two cases per million person-years were reported from Sweden,19 whereas a separate study from England found that number to be 1 case per million personyears.20 The incidence might be higher in low-resource settings where rheumatology services are scarce and economic constraints are numerous, resulting in delay in diagnosis and compromising management of the underlying disease.21 A common theme throughout multiple studies is the current trend of increasing age at diagnosis.5,17,22,23 One study found the median age at diagnosis has increased from 50 to 70 years.5 A male predominance was found in 2 large series of 374 and 474 378 patients.23,24 In most epidemiologic studies, RA is the most commonly associated disease with AA amyloidosis.10,24 In lowincome and low middle-income countries, however, chronic infections remain a major cause, with most cases secondary to mycobacteria, most notably untreated tuberculosis.11,25 Skin popping leading to recurrent infections is a well-recognized cause. In 1 autopsy study, as many as 14% of s.c. drug users had AA amyloidosis,26 and at 1 hospital in San Francisco, 100% of cases of renal AA amyloidosis from 1998 to 2013 were attributed to skin popping.13 There are also geogenetic patterns of AA amyloidosis. Around the Mediterranean basin, untreated FMF is a major culprit. For example, a study from Turkey found that untreated FMF was the leading cause of AA amyloidosis, accounting for 19.7% of cases, whereas chronic rheumatic diseases and chronic infections resulted in 18.5% and 13.5% of cases, respectively.11 AA amyloidosis due to familial periodic fever syndromes affects people of English and Irish descent with tumor necrosis factor receptor-1–associated periodic syndrome (TRAPS).27 The major causes of AA amyloidosis are summarized in Table 1. PATHOGENESIS Amyloid fibrils are composed of insoluble and proteolyticresistant protofilaments. These protofilaments arrive from aggregation of misfolded amyloid precursors that possess a cross-b-sheet quaternary structure, a defining structural element.10,28,29 The precursor protein in AA amyloid is SAA, an apolipoprotein produced predominately by hepatocytes, but also by other cells, including macrophages, endothelial cells, and smooth muscle cells.10,24,30,31 It is an acute-phase reactant synthesized under the influence of proinflammatory cytokines, such as tumor necrosis factor-a (TNF-a), interleukin (IL)-1b, and IL-6.10,24,30 SAA possesses multiple functions, including serving as opsonin, allowing bacterial uptake by neutrophils, and inducing expression of matrix metalloproteinase and angiogenesis, promoting tumor metastasis in carcinoma and joint destruction in inflammatory arthritis.32–35 SAA may also play a role in maintenance of normal body weight and protection from hepatic steatosis.36,37 Furthermore, SAA also acts as a hub in interaction networks in lipid homeostasis and immune response.38,39 Aggregation of SAA into amyloid fibrils only occurs when a critical concentration has been reached, and the high plasma concentration persists for a prolonged period.14 Proteolytic cleavage of SAA1 from a 122–amino acid peptide eventually to a 76–amino acid residue by metalloproteases is a crucial step for amyloid formation.40 Interactions with glycosaminoglycans (GAGs) and serum amyloid P component (SAP) promote aggregation and lead to the formation of amyloid (Figure 1).41–43 In addition to GAGs, apolipoprotein A1, apolipoprotein A4, and apolipoprotein E are chaperone proteins found with all amyloid that play an essential role in fibrillogenesis and protection of the amyloid fibrils.44 Genetic susceptibility also plays a role in the genesis of the disease. SAA is genetically polymorphic, and its gene is Kidney International (2023) 103, 473–484 review S Karam et al.: Renal AA amyloidosis: diagnosis and management Neoplasms Castleman’s disease Hereditary inflammatory conditions Skin popping Sustained inflammation Autoimmune/ connective tissue diseases SAA1 gene promoter mutation Infections Increased IL-1, IL-6, TNF-α Liver GAG Macrophages SAA1 Extracellular deposition Amyloid fibrils Amyloid (oligomer) Precursor protein SAP Endothelial and smooth muscle cells Amyloid (monomer) Figure 1 | Pathogenesis of amyloid A (AA) amyloidosis. Serum AA (SAA) 1 is synthesized under the influence of proinflammatory cytokines as tumor necrosis factor-a (TNF-⍺), interleukin (IL)-1, and IL-6. SAA1 is mainly produced by hepatocytes but also by macrophages, endothelial cells, and smooth muscle cells. Aggregation of SAA into amyloid fibrils occurs when a critical concentration has been reached and a high plasma concentration persists for a long period. SAA usually undergoes a process of cleavage, misfolding, and aggregation, followed by a series of interactions with other tissue components, such as glycosaminoglycans (GAGs) and serum amyloid P component (SAP), which eventually leads to deposition as amyloid. AA deposits in the extracellular space of the liver, kidneys, spleen, and heart. located on chromosome 11. The SAA gene products SAA1 and SAA2 are both elevated with acute inflammation, but >90% of the precursor proteins of the AA protein are derived from SAA1.45 Furthermore, in humans, 3 main SAA1 alleles (SAA1.1, SAA1.3, and SAA1.5) are defined by 2 singlenucleotide polymorphisms located in exon 3, resulting in 2 amino acid differences at positions 52 and 57. There seems to be differential amyloidogenicity among the different SAA1 isoforms, with homozygosity for SAA1.1 being a significant risk factor for development of AA amyloidosis in Whites,46 whereas it is homozygosity of SAA1.3 in the Japanese population.47 Experiments with murine SAA1.1 found it binds hyaluronic acid (a GAG) more than SAA2.2, which is important for polymerization.48 Finally, obesity and age also constitute susceptibility factors, especially in idiopathic AA amyloidosis.9,49 It has been postulated that leptin and other inflammatory parameters associated with obesity could contribute to systemic inflammation and amyloidosis genesis.49 For instance, white fat tissue in obese mice contains 45% to 60% of macrophages, of which most have acquired a proinflammatory phenotype.50 Many cases considered initially as idiopathic are in fact caused by rare genetic autoinflammatory diseases, such as TRAPS1 or mevalonate kinase deficiency/hyper IgD syndrome. Therefore, when an autoinflammatory disease is suspected but no specific clinical features are present, a next-generation sequencing panel for genetic autoinflammatory diseases should be performed.51,52 CLINICAL PRESENTATION AA amyloidosis causes a greater degree of kidney dysfunction when compared with AL amyloidosis and is more likely to affect younger individuals.18 In 80% to 90% of cases of AA amyloidosis, the kidneys are involved and patients commonly present with kidney dysfunction with glomerular amyloid deposition that leads to nephrotic syndrome. Left untreated, the renal amyloidosis progresses to end-stage kidney disease Kidney International (2023) 103, 473–484 (ESKD).10,17,24,53,54 In several studies, >10% had already developed ESKD at the time of diagnosis.24,55 In a series of 200 patients, aged >55 years, underlying infections and estimated glomerular filtration rate (eGFR) <45 ml/min were associated with a poor overall survival, whereas patients with proteinuria of >4 g/24 h and eGFR <35 ml/min had an inferior renal survival.55 There is also a predominantly tubular form of AA amyloidosis.56 Patients with this variant may present with a bland urinary sediment and little proteinuria, but they may show signs of distal tubular dysfunction, such as nephrogenic diabetes insipidus.57 Moreover, there have been reports of Fanconi syndrome and renal tubular acidosis, but these are usually in association with nephrotic syndrome.58,59 Also, kidney function appears to deteriorate less rapidly when amyloid deposits are completely absent from the glomerulus.57 Finally, there are rare reports of crescentic pauci-immune glomerulonephritis, perhaps related to rupture of glomerular capillary loops due to amyloid deposition.60 They have been notably depicted in some cases of RA that were anti-neutrophil cytoplasmic autoantibody negative.61,62 In addition to kidney involvement, hepatic and splenic involvement is common along with gastrointestinal (GI) involvement, which is found in around 30% of cases.10,63 The GI manifestations include macroglossia, a dilated and atonic esophagus, gastric polyps, and luminal narrowing or ulceration of the colon, whereas hepatic infiltration is mostly revealed by hepatomegaly and an elevated alkaline phosphatase level.64 Cardiac, thyroid, adrenal, and neurologic involvements have also been reported but are rare.10,24,65–67 DIAGNOSTICS AND PATHOLOGY No clinical or laboratory test has yet superseded histology for the diagnosis of AA amyloidosis. In suspected patients, a tissue biopsy is recommended as a first step to confirm the presence of amyloid. Potential sites to be accessed include abdominal fat and minor salivary glands. More invasive sites, 475 review Figure 2 | Histologic findings in amyloid A (AA) amyloidosis. (a,b) Massive amyloid glomerular deposits characterized by the replacement of the mesangial matrix by acellular, weakly periodic acid–Schiff (PAS)–positive (asterisks) material (PAS stain, original magnification 200) (a) and nonargyrophilic material (b). (b) Subendothelial capillary wall deposits are present with segmental duplication of the glomerular basement membrane (arrowheads) (Jones silver stain, original magnification 400). (c) Predominant deposition of AA amyloidosis along the tubular basement membrane (arrows) (PAS stain, original magnification 100). (d) Immunohistochemistry study using antibodies against serum AA protein strongly stains the amyloid deposits. (e) Congo red stain showing green-yellow birefringence under the polarized light (Congo red stain, original magnification 200). (f) Randomly arranged fibrils on electron microscopy (transmission electron microscopy, original magnification 50,000). To optimize viewing of this image, please see the online version of this article at www. kidney-international.org. like kidney, rectal tissue, or the GI tract, should be explored when there is a high clinical suspicion of their involvement or when more accessible sites are negative. Kidney involvement is defined as a 24-hour urine protein >0.5 g, and the diagnosis is made by a kidney biopsy.17,18 Subcutaneous fat biopsy with Congo red staining and polarized microscopy observation in a population with several types of systemic amyloidosis (AA, AL, and transthyretin-mediated [ATTR]) has a sensitivity of 80% with thorough assessment increasing it to 476 S Karam et al.: Renal AA amyloidosis: diagnosis and management >90% and a specificity of 100%.68 In a study that reviewed 236 histologically confirmed cases, of which 19 were of the AA type, rectal biopsies had a sensitivity of 84%.69 In another study that followed 62 suspected AL or AA amyloidosis cases with negative abdominal fat aspirates, salivary gland biopsies had a sensitivity of 58%.70 Glomerular involvement is almost always present. Glomeruli typically show periodic acid–Schiff stain pale and nonargyrophilic deposits in the mesangium, which can be segmental, not infrequently forming nodules.71 Amyloid deposits can also be found along the capillary wall, sometimes forming amyloid spicules, and at the glomerular hilum. Some vascular involvement is almost constant, with >95% of the biopsies showing AA amyloid in the arterioles and arteries.71 In addition, AA amyloidosis with predominantly vascular infiltration has been described.72 Furthermore, a predominantly tubular form of AA amyloidosis has been described.56,72,73 Inflammation can be seen in 44% of patients and appears as a multinucleated giant cell reaction or a glomerular inflammatory infiltrate within the capillary loops.71 Interstitial inflammation is also common and may be present adjacent to vessels or tubules.12 Congo red stain performed on the formalin-fixed paraffinized tissue shows a characteristic green-yellow birefringence on polarization.5,17 Electron microscopy shows solid, nonbranching fibrils that are 9 to 15 nm in diameter.5 On confirmation of the presence of amyloid, immune stains—including immunohistochemistry and immunofluorescence—are often the first-line approach to determine the type of amyloid.17,18,74,75 In AA amyloidosis, routine immunofluorescence examination is typically negative for IgG, IgA, IgM, C1q, C3, fibrinogen, and k and l antibodies (Figure 2).76 Immunostaining using commercially available antibody against SAA can be helpful by showing a strong staining of the amyloid deposits. However, immune stains against SAA have several limitations, and both false positivity, due to the lack of specificity of the SAA antibody, and false negativity, due to epitope loss by protein crosslinking after formalin fixation, have been described. Moreover, the contamination of amyloid deposits by serum proteins, such as Ig components, may lead to a false-positive staining for Igs.77,78 Amyloid typing by laser microdissection and proteomic analysis by mass spectrometry, performed on formalinfixed paraffin-embedded tissue, is more sensitive and specific than most immune methods for the identification of the amyloid subtype.79 It has emerged as the method of choice for amyloid typing but is currently not used as a standard diagnostic technique because of its limited accessibility due to the few centers that have the facilities and expertise to perform this assay. Immunoelectron microscopy is another highly sensitive and specific method for amyloid typing, which is, however, only available in few expert centers.80,81 An attempt was made to develop a pathologic renal amyloid prognostic score in AA amyloidosis that considered the glomerular, vascular, and interstitial AA deposition, as well as glomerular sclerosis, interstitial inflammatory infiltration, and/or fibrosis and tubular atrophy. The score was divided Kidney International (2023) 103, 473–484 review S Karam et al.: Renal AA amyloidosis: diagnosis and management into 3 grades (renal amyloid prognostic score I, II, and III). Renal amyloid prognostic score grade and interstitial inflammatory infiltration were associated with baseline eGFR, and glomerular amyloid deposition was associated with proteinuria, but only extensive glomerular amyloid deposition (>50%) turned out to be an independent predictor for the development of ESKD.82 The SAP scintigraphy is a tool that can be used to detect and quantify amyloid deposits. This uses highly purified SAP radiolabeled with the g emitting isotope of 123I that localizes amyloid deposits and quantifies the amount of amyloid deposited. It has a sensitivity of 100% in patients with systemic amyloidosis, but cannot type the amyloid and is not available in the United States and many other countries around the world.17 The measurement of SAA levels can be used to estimate the amount of amyloid genesis but is also not available in the United States and many non-European countries. Elevated level >10 mg/L is associated with an increased risk of developing AA amyloidosis, but by itself, SAA level is not enough to make the diagnosis. On the other hand, amyloid burden and kidney prognosis significantly correlate with the SAA concentration, and the risk of death is highest in patients with extremely elevated levels.24 Only a few reports describe the regression of AA amyloid deposits in tissue after treatment. Okuda and Takasugi83 and Hattori et al.84 have reported AA amyloidosis deposit regression in the GI tract in patients treated with tocilizumab (TCZ) for RA. In the kidney, 1 report describes the regression of interstitial AA amyloid deposits in a patient with Castleman disease after treatment with TCZ.85 There was, however, no effect of the treatment on the glomerular deposits. Inui et al. reported a case of AA amyloidosis deposit regression in all kidney compartments in a patient with FMF treated with TCZ.86 Interestingly, most published reports describe significant clinical improvement after specific treatment—such as the resolution of the nephrotic syndrome—despite persistent amyloid deposits on the repeated kidney biopsy.87–89 TREATMENT General principles The mainstay of treatment is to address the primary cause by treating any infection or chronic inflammation. Traditionally, therapies targeting the underlying inflammatory disorder using disease-modifying antirheumatic drugs (DMARDs) and other drugs, such as colchicine, steroids, and cyclophosphamide, have had some success if administered in a timely manner. DMARDs fall into 2 categories: nonbiologics and biologics. Nonbiologic DMARDs include methotrexate (MTX), hydroxychloroquine, sulfasalazine, and leflunomide. In patients with active RA, MTX is suggested as the initial treatment; it is usually administered with nonsteroidal antiinflammatory drugs or steroids. MTX dose is increased as tolerated and as needed to control active symptoms and signs of arthritis, and it is continued for at least 3 months.90 MTX has a faster onset of action, has better tolerance in the long-term, and is comparable or better in terms of efficacy Kidney International (2023) 103, 473–484 when compared with other nonbiologic DMARDs. Also, when compared with leflunomide, sulfasalazine, and hydroxychloroquine, MTX improved survival in patients with RA.91–93 MTX requires close monitoring as it is associated with bone marrow, liver, and lung toxicity.91 Colchicine, an alkaloid with inhibitory effects on multiple cellular functions, including microtubule assembly, cell adhesion, and inflammasome activation, remains the standard of care for FMF as it has been proven to be a valuable treatment when given life-long on a daily basis.94 It is useful to prevent the recurrence and the intensity of febrile attacks and subsequently the development of amyloidosis.95–100 More important, it reduces the occurrence of kidney disease, such as nephrotic syndrome, and prevents its progression.100,101 The minimal recommended dose is 1 mg daily, and the most common reported adverse effects are GI effects, such as nausea, vomiting, and diarrhea; these symptoms usually tend to improve with dose reduction.102,103 The target is ultimately to reduce the amount of circulating SAA protein by reducing its production in the liver.53 Indeed, suppressing SAA leads to prolonged survival, decrease in amyloid effects on organ function, and a regression of AA amyloid deposits.53 The reduction of SAA levels to <7 mg/L has been associated with favorable renal prognosis and should always be monitored if feasible.24 If SAA assays are unavailable, efficacy of the treatment can be assessed through measurement of serial C-reactive protein levels, even though in some patients there could be a discrepancy between the 2 markers.5 As synthesis and secretion of acute-phase SAA is mediated by cytokines (mainly IL-1, IL-6, and TNF-a 53,104), therapies targeting these cytokines and their pathways have recently gained interest. Examples include inhibitors of TNFa, IL-1, IL-1ß, and IL-6.89,105–109 Although they have been shown to be effective for autoimmune-mediated AA amyloidosis and hereditary periodic fever syndrome and at least half of respondents in a population with RA,110 they have also been successful in cases classified as idiopathic. Indeed, in up to 20% to 40% of the cases, no specific cause can be found, which creates a dilemma as to the choice of treatment.10,11,17,106 Since they have been in use, the risk of death of patients with AA amyloidosis has been significantly reduced.111 The one caveat is that these cytokine inhibitors may exacerbate an occult or concomitant infection.112 Tuberculosis, in particular, seems to be an important safety concern.110 Experimental agents for the treatment of renal AA amyloidosis There have also been efforts to either affect the deposition of amyloid in target issues or target its clearance after deposition. For instance, eprodisate is a negatively charged sulfonated molecule structurally similar to heparan sulfate, a GAG that can interfere with the interactions between GAGs and amyloidogenic fibrils, preventing their deposition.36,37,41,109,113 In a double-blind, placebo-controlled trial of patients with renal AA amyloidosis, eprodisate failed to show any effect on 477 review progression to ESKD, although it significantly decreased the rate at which kidney function deteriorated.109 Unfortunately, eprodisate failed to meet the primary endpoint of slowing kidney function decline in a second phase 3 trial.114 It has been suspected that chaperone proteins protect the amyloid fibrils from degradation. To enhance immunotherapeutic clearance of amyloid after deposition, miridesap [(R)-1-[6-[(R)-2-carboxy-pyrrolidin-1-yl]-6-oxo-hexanoyl] pyrrolidine-2-carboxylic acid], also known as CPHPC, was developed to target SAP, one of the chaperone proteins. Miridesap depleted circulating SAP in an open-label study and reduced, to a certain extent, SAP content in affected organs.115 To increase the removal of AA amyloid from tissue, dezamizumab, a fully humanized monoclonal IgG1 anti-SAP antibody, was administered to 23 adult subjects after they received 3 cycles of miridesap, and it triggered immunotherapeutic clearance of amyloid deposited in tissue.116 Unfortunately, several clinical trials investigating these new therapeutic routes were recently interrupted due to futility analysis or a change in benefit/risk profile.117 It is finally worth mentioning the recent development of a prodrug of miridesap with better oral bioavailability and physical stability, currently named GSK294.118 Unfortunately, after administration for 7 days to humans, arrhythmias occurred, the relation of which to GSK294 remains unclear, and the study was terminated. Finally, another route partially explored is the use of antisense oligonucleotides to lower the expression of SAA in the liver. Although this strategy was successful in mice, as it led to both suppressed SAA production and reduced tendency to develop AA amyloidosis, it has yet to be tested in humans.119 Anti-cytokine therapy used in the treatment of AA amyloidosis IL-1 inhibition. Three IL-1 inhibitors are currently avail- able for clinical use: anakinra, canakinumab, and rilonacept, which is approved for clinical use in the United States only. Anakinra is a recombinant nonglycosylated analogue of the IL1 receptor antagonist and, therefore, inhibits both Il-1a and Il1b. It is approved in the United States for the treatment of RA, cryopyrin-associated periodic syndromes, and deficiency of IL-1 receptor antagonist120 and for the treatment of FMF and Still disease in Europe.121 Canakinumab is a human monoclonal antibody that specifically binds to IL-1b and blocks the interaction between IL-1b and the IL-1 receptor and the activation of subsequent inflammatory responses. Canakinumab is approved for the treatment of cryopyrin-associated periodic syndromes and TRAPS and for the treatment of FMF and Still disease.122 Rilonacept is approved for the treatment of recurrent pericarditis, cryopyrin-associated periodic syndromes, and deficiency of IL-1 receptor antagonist.123 None of these 3 drugs is approved for renal AA amyloidosis specifically.124 Anakinra is usually administered as a daily s.c. injection. Canakinumab requires 1 s.c. injection every 4 to 8 weeks and has been used in patients who developed leukopenia or injection site reaction with anakinra. 478 S Karam et al.: Renal AA amyloidosis: diagnosis and management No formal clinical trials have been conducted to evaluate the efficacy of IL-1 inhibition in AA amyloidosis, and the data available are limited to case reports and series. In patients with AA amyloidosis secondary to TRAPS, anakinra induced complete resolution of symptoms with normalization of Creactive protein and SAA levels in 7 patients.125 One of the 2 patients in this series with significant proteinuria achieved a complete regression of the proteinuria, whereas the other had stabilization of proteinuria. In patients with renal AA amyloidosis secondary to FMF, canakinumab improved the kidney function and proteinuria in 2 pediatric patients who were colchicine resistant.126,127 In fact, both anakinra and canakinumab have been reported to be effective for patients with colchicine-resistant FMF-associated AA amyloidosis. In a retrospective study, inflammatory markers, C-reactive protein and erythrocyte sedimentation (ESR) rate, were significantly reduced in all and normalized in 12 of 17 patients who received IL-1 blockade with significant improvement in proteinuria.128 In another retrospective review of 20 patients with colchicine-resistant FMF, both patients with biopsy-proven AA amyloidosis (one who received anakinra, and the other who received canakinumab) had significant improvement of their proteinuria with treatment.129 A systematic review of the literature found 18 patients with FMF with established AA amyloidosis treated with anakinra and 1 patient who received canakinumab. Four patients had nephrotic syndrome, and 8 had end-stage kidney disease. Five patients also received a kidney allograft before initiation of the drug. A decrease in proteinuria was observed in all patients with nephrotic syndrome, and no recurrence of AA amyloidosis was reported in the 7 patients receiving a kidney transplant who were started on the drug either before after receiving the transplant.130 On the other hand, the largest observational cohort from Turkey, which included 44 patients with FMF and AA amyloidosis, reported mixed results with anakinra or canakinumab. Among 35 patients not on kidney replacement therapy, kidney function was maintained or improved in 79.4% but deteriorated in 20.6%. Patients with creatinine levels <1.5 mg/dl at onset benefitted more from IL-1 inhibition with regard to their kidney functions and acute-phase reactants.131 Regarding patients with AA amyloidosis of unknown etiology, a review of 11 patients treated with anakinra found that 9 had complete or partial remission. A complete response in this study was defined as normalization of SAA (#10 mg/L) and resolution of chronic disease symptoms and flares/exacerbations, whereas a partial response was defined as improvement but not normalization of SAA and/or an improvement in disease symptoms.106 Finally anakinra seems to be efficient at treating nephrotic syndrome in patients with AA amyloidosis and autoinflammatory disease associated with CIAS1/NALP3/cryopyrin gene mutations.132 IL-6 inhibitors. TCZ, an IL-6 inhibitor, is another promising therapy for AA amyloidosis. IL-6 is a glycopeptide produced by various, including fibroblasts, osteoblasts, endothelial cells, T cells, and B cells.133,134 It is thought to exert its effects via 2 different signaling pathways, classic cis Kidney International (2023) 103, 473–484 review S Karam et al.: Renal AA amyloidosis: diagnosis and management signaling and trans signaling, the latter being responsible for most proinflammatory responses.135 TCZ inhibits both signaling pathways.136 IL-6 also plays a pivotal role in SAA synthesis. In a study using HepG2 cells, a cell line derived from hepatocytes, IL-6 stimulation alone was able to induce a weak expression of SAA1 and SAA2 mRNA, whereas almost no expression was induced by the stimulation with IL-1b or TNF-a alone.137 Numerous case reports and case series have reported successful outcomes with TCZ administered to patients with AA amyloidosis secondary to various underlying disorders and that were previously refractory to conventional treatment. TCZ was given to a series of 12 heavily pretreated patients with FMF and concomitant AA amyloidosis, 4 of whom also had ankylosing spondylitis and 1 had Crohn disease.138 Of the 12 patients, 11 were treated with colchicine, 5 were treated with anakinra, 3 were treated with canakinumab, 3 were treated with infliximab, 2 were treated with cyclophosphamide, 1 was treated with etanercept, 2 were treated with sulfasalazine, and 1 was treated with azathioprine. At a mean follow-up of 17 months, C-reactive protein was significantly reduced from 18 to 5.8 mg/L, whereas ESR decreased from 48.7 to 28.7 mm/h. FMF attacks were reduced in 91.7% of patients. In 2 patients with eGFR <50 ml/min, proteinuria was reduced by 43% and 37%, whereas kidney function improved from 37.5 to 45.1 ml/min and from 39.9 to 59.0 ml/min. In the patients with eGFR >50 ml/min, kidney function and proteinuria remained stable. TCZ was also administered to 5 patients with RA with AA amyloidosis who were followed up for over a year. Improvement in kidney dysfunction, including proteinuria and a significant decrease in SAA concentration, was noted in 4 of 5 patients (2 were refractory to etanercept).107 In another 5 patients with rheumatic disease and AA amyloidosis refractory to anti–TNF-a therapy and DMARDs, inflammation decreased in all and kidney function either improved or remained stable. Proteinuria also decreased or disappeared in 3 patients.108 In a larger series of 20 patients with chronic inflammatory disorders and AA amyloidosis refractory to other treatments, TCZ was effective at reducing amyloid deposits and at suppressing inflammation over a median followup of 23 months.139 Also, TCZ induced full remission over a year in a patient with Behcet disease and nephrotic syndrome due to AA amyloidosis140 and cleared the interstitial AA kidney deposits in a patient with multicentric Castleman disease.85 Others reported that TCZ improved both inflammation and proteinuria in 2 cases of ankylosing spondylitis.141 TCZ had a beneficial effect on members of the family with genetic AA amyloidosis described by Sikora et al. when prescribed early in the course of the disease.8 Finally, the first nationwide survey of patients with AA amyloidosis in Japan showed a good responses in 95.5% of the 66 patients who received TCZ as opposed to 74.1% of good responses in the 27 patients who received TNF-a inhibitors, suggesting that TCZ was superior, although the samples size was small and the 2 groups were not randomized.142 Siltuximab, a chimeric monoclonal antibody that binds with high affinity to IL-6, is Kidney International (2023) 103, 473–484 the first drug approved for the treatment of multicentric Castleman disease.143 It constitutes currently, with or without steroids, the first-line therapy,144 and leads to durable clinical response and longer disease stabilization, potentially preventing the development of AA amyloidosis.145 Its role in established AA amyloidosis has not been studied yet. Sarilumab, a human anti–IL-6R antibody, was recently approved for the treatment of RA, and is expected to be similarly effective for AA amyloidosis. TNF-a inhibitors. TNF-a inhibitors used in the treatment of AA amyloidosis include etanercept, infliximab, certolizumab, and adalimumab. The rationale to use them would be their ability to reduce SAA levels by inhibiting TNF-a– induced SAA transcription in hepatocytes and by reducing macrophage activation.146 Some retrospective studies and case reports in patients with either inflammatory bowel disease or rheumatic diseases have shown some clinical utility.147–153 For instance, in a retrospective review of a series of 15 patients with rheumatologic disease who received infliximab, etanercept, or both, 3 experienced a sustained decrease in proteinuria with an increase in eGFR.148 In another series of 14 patients with RA treated with infliximab or etanercept, the 24hour creatinine clearance improved in 4 patients and the proteinuria decreased in 3 patients.149 In 6 patients with Crohn disease complicated by AA amyloidosis, reduction of the nephrotic syndrome was observed in 1 patient and stabilization of kidney function was observed in 2 patients.152 In a retrospective study that compared the effectiveness of etanercept with cyclophosphamide in a cohort of Japanese patients with RA, there was significantly better survival and improvement in the eGFR in the etanercept group.154 However, when compared with TCZ retrospectively in a singlecenter study, the 5-year retention rate was much lower for TNF-a inhibitors, and they showed less clinical utility.155 The reason might be a suboptimal propensity to normalize acutephase reactants.151 Serious adverse events observed during long-term follow-up include sepsis and thrombotic events. Targeted therapies in specific populations The use of targeted therapies in patients with TRAPS-related AA amyloidosis was recently reviewed as part of a national case series in France, along with a systematic review of the literature.51 The authors summarized the data for 21 regimens administered to 19 patients. Anakinra was used in 16 patients, of whom 6 improved, 7 stabilized, and 3 worsened their kidney function. Canakinumab was given to 1 patient and improved kidney function. Etanercept was administered to 14 patients, of whom 7 were switched to anakinra because of adverse events or partial remission. Of the remainding patients, 2 improved partially and 1 recovered completely. Interestingly, the administration of infliximab or adalimumab in patients with TRAPS has led to enhanced anti-apoptotic activity and oversecretion of proinflammatory cytokines, leading to paradoxical exacerbation of the TRAPS.156,157 In a review of 20 patients with mevalonate kinase deficiency/hyper IgD syndrome, anakinra (n ¼ 8, 1 success, 5 partial responses, 479 review and 2 failures), etanercept (n ¼ 7, 4 successes, 1 partial response, and 2 failures), and TCZ (n ¼ 5, 4 successes and 1 partial response) were used as therapy.52 In this review, complete response was defined as complete control of the clinical manifestations and normalization of laboratory parameters, partial response was considered as persistence of some clinical manifestations and/or abnormal laboratory findings, and failure was the absence of any substantial impact on disease activity or worsening. Rituximab might be an alternative therapy in some patients with RA with established AA amyloidosis. It has already shown some efficacy in patients with severe active RA who have exhibited an inadequate response to $1 TNF-a inhibitors.158 Its use in established amyloidosis has been reported by various authors for a total of 9 cases, 8 with RA and 1 overlap syndrome with features of polymyositis, scleroderma, and RA.159–161 Kidney function either remained stable or improved in 7 patients, whereas proteinuria improved in 5 cases. Notably, 7 patients had failed TNF-a inhibitor therapy before receiving rituximab. The exact mechanism behind rituximab’s potential efficacy remains unknown. Adverse effects of anti-cytokine therapy In patients with AA amyloidosis, treatment with anakinra is in general well tolerated, with the main adverse event reported being the known transient injection site reactions, which sometimes mandate switching to a different agent.106,128,131,132 Neutrophil counts also need to be monitored with reports of leukopenia.128,162 Patients are usually switched to canakinumab, with infections reported as the main adverse event but also activation of psoriasis and lichen planus.131,163 Infections are also the main adverse event reported with TCZ.107,139 Other minor adverse effects include slightly elevated liver enzymes, mild thrombocytopenia, diplopia, and an increase in blood pressure.138,164 TNF-a inhibitors also seem to be relatively well tolerated, with herpes zoster and venous thrombosis reported with infliximab use148 and an increased risk of infections, especially for patients on hemodialysis165 (Supplemental Table S1). AA amyloidosis and kidney replacement therapy Patients with renal AA amyloidosis who progress to ESKD can be treated with dialysis or kidney transplantation (KT). However, survival on dialysis is poor, with cardiac involvement being a strong predictor of death within the first year of dialysis.166 KT should, therefore, be considered in select patients, but AA amyloidosis can recur after KT. In a French multicenter study that assessed the graft and patient survival of 59 renal recipients, the recurrence rate of AA amyloidosis nephropathy was estimated at 14% and there was a significantly higher incidence of infectious and cardiovascular complications with a reduced survival compared with recipients with another underlying cause of ESRD.167 This recurrence rate was derived from biopsies done based on clinical and/or biological suspicion of recurrence, or “for cause” biopsies. Hence, a higher recurrence rate of AA 480 S Karam et al.: Renal AA amyloidosis: diagnosis and management amyloidosis cannot be excluded, and sequential biopsies may play a role in early detection of recurrence of AA amyloidosis. In a more recent study, postrenal transplant survival was comparable to those with diabetic nephropathy.168 Colchicine has been reported to be effective in preventing recurrence in FMF, but data regarding treatment of established AA amyloidosis with targeted therapies in KT are scarce. In a series of 6 patients with FMF-related amyloidosis (1 of them with nephrotic syndrome, 2 with chronic kidney disease, and 3 with renal transplantation) who received anakinra due to colchicine resistance, there was partial remission of the nephrotic syndrome. In the transplanted patients who were having recurrent FMF attacks despite colchicine and deterioration of the renal function with each attack, the attacks ceased completely.169 In another series of 17 patients with FMF who received concomitantly colchicine and anakinra post-KT, with 4 of them with recurrent AA amyloidosis, partial response (defined as $50% decrease in proteinuria) and complete remission (<0.3 g/d proteinuria) were achieved in only 2 patients (Toz B, Çalışkan YK, Erer B, et al.. Efficacy and safety of IL-1 inhibitors in amyloidosis associated with, familial Mediterranean fever who underwent kidney transplantation [abstract 943]. Presented at 2016/ACR/ARHP Annual Meeting. November 11–16, 2016; Washington DC). CONCLUSION Clinical observations stemming from the therapeutic success achieved so far seem to indicate that the reduction of the SAA protein is presently the most effective treatment strategy for AA amyloidosis. This is often achieved using IL-1, IL-6, and TNF-a inhibitors as opposed to traditional therapies, such as colchicine used for FMF. It is, however, important to identify the disease early to prevent advanced organ damage and to increase the likelihood of organ response. Clinical trials are needed to identify the most appropriate agent. Although the few tested interventions aimed at promoting amyloid clearance did not show a clear clinical benefit, this therapeutic approach deserves to be further pursued to complement existing therapies to improve the outcomes of these patients. DISCLOSURE All the authors declared no competing interests. SUPPLEMENTARY MATERIAL Supplementary File (Word) Table S1. Summary of major available and potential therapies for renal amyloid A (AA) amyloidosis. REFERENCES 1. Desport E, Bridoux F, Sirac C, et al. Al amyloidosis. Orphanet J Rare Dis. 2012;7:54. 2. Picken MM. The pathology of amyloidosis in classification: a review. Acta Haematol. 2020;143:322–334. 3. Obici L, Perfetti V, Palladini G, et al. Clinical aspects of systemic amyloid diseases. Biochim Biophys Acta. 2005;1753:11–22. 4. Urieli-Shoval S, Linke RP, Matzner Y. Expression and function of serum amyloid A, a major acute-phase protein, in normal and disease states. Curr Opin Hematol. 2000;7:64–69. Kidney International (2023) 103, 473–484 S Karam et al.: Renal AA amyloidosis: diagnosis and management 5. Papa R, Lachmann HJ. Secondary, AA, amyloidosis. Rheum Dis Clin North Am. 2018;44:585–603. 6. Harris M, Brathwaite R, Scott J, et al. Drawing attention to a neglected injecting-related harm: a systematic review of AA amyloidosis among people who inject drugs. Addiction. 2018;113:1790–1801. 7. Terre A, Colombat M, Cez A, et al. AA amyloidosis complicating monoclonal gammopathies, an unusual feature validating the concept of "monoclonal gammopathy of inflammatory significance"? Int J Clin Pract. 2021;75:e14817. 8. Sikora J, Kmochova T, Musalkova D, et al. A mutation in the SAA1 promoter causes hereditary amyloid A amyloidosis. Kidney Int. 2022;101:349–359. 9. Stankovic Stojanovic K, Georgin-Lavialle S, Poitou C, et al. AA amyloidosis is an emerging cause of nephropathy in obese patients. Eur J Intern Med. 2017;39:e18–e20. 10. Bunker D, Gorevic P. AA amyloidosis: Mount Sinai experience, 19972012. Mt Sinai J Med. 2012;79:749–756. 11. Ayar Y, Ersoy A, Oksuz MF, et al. Clinical outcomes and survival in AA amyloidosis patients. Rev Bras Reumatol Engl Ed. 2017;57:535–544. 12. Sethi S, Theis JD. Pathology and diagnosis of renal non-AL amyloidosis. J Nephrol. 2018;31:343–350. 13. Lejmi H, Jen KY, Olson JL, et al. Characteristics of AA amyloidosis patients in San Francisco. Nephrology (Carlton). 2016;21:308–313. 14. Westermark GT, Fandrich M, Westermark P. AA amyloidosis: pathogenesis and targeted therapy. Annu Rev Pathol. 2015;10:321–344. 15. Said SM, Sethi S, Valeri AM, et al. Renal amyloidosis: origin and clinicopathologic correlations of 474 recent cases. Clin J Am Soc Nephrol. 2013;8:1515–1523. 16. Dasari S, Theis JD, Vrana JA, et al. Amyloid typing by mass spectrometry in clinical practice: a comprehensive review of 16,175 samples. Mayo Clin Proc. 2020;95:1852–1864. 17. Lane T, Pinney JH, Gilbertson JA, et al. Changing epidemiology of AA amyloidosis: clinical observations over 25 years at a single national referral centre. Amyloid. 2017;24:162–166. 18. Panizo N, Rivera F, López-Gómez JM. Spanish Registry of Glomerulonephritis. Decreasing incidence of AA amyloidosis in Spain. Eur J Clin Invest. 2013;43:767–773. 19. Hemminki K, Li X, Forsti A, et al. Incidence and survival in nonhereditary amyloidosis in Sweden. BMC Public Health. 2012;12:974. 20. Pinney JH, Smith CJ, Taube JB, et al. Systemic amyloidosis in England: an epidemiological study. Br J Haematol. 2013;161:525–532. 21. Wakhlu A, Krisnani N, Hissaria P, et al. Prevalence of secondary amyloidosis in Asian North Indian patients with rheumatoid arthritis. J Rheumatol. 2003;30:948–951. 22. Real de Asua D, Costa R, Galvan JM, et al. Systemic AA amyloidosis: epidemiology, diagnosis, and management. Clin Epidemiol. 2014;6:369– 377. 23. Khellaf G, Benziane A, Kaci L, Benabadji M. AA renal amyloidosis: clinical observations over 20 years. Clin Nephrol. 2022;97:167–172. 24. Lachmann HJ, Goodman HJ, Gilbertson JA, et al. Natural history and outcome in systemic AA amyloidosis. N Engl J Med. 2007;356:2361–2371. 25. Deshayes S, Aouba A, Grateau G, Georgin-Lavialle S. Infections and AA amyloidosis: an overview. Int J Clin Pract. 2021;75:e13966. 26. Menchel S, Cohen D, Gross E, et al. AA protein-related renal amyloidosis in drug addicts. Am J Pathol. 1983;112:195–199. 27. Cantarini L, Lucherini OM, Muscari I, et al. Tumour necrosis factor receptor-associated periodic syndrome (TRAPS): state of the art and future perspectives. Autoimmun Rev. 2012;12:38–43. 28. Pepys MB. Amyloidosis. Annu Rev Med. 2006;57:223–241. 29. Close W, Neumann M, Schmidt A, et al. Physical basis of amyloid fibril polymorphism. Nat Commun. 2018;9:699. 30. Sun L, Ye RD. Serum amyloid A1: structure, function and gene polymorphism. Gene. 2016;583:48–57. 31. Quinton LJ, Blahna MT, Jones MR, et al. Hepatocyte-specific mutation of both NF-kappaB RelA and STAT3 abrogates the acute phase response in mice. J Clin Invest. 2012;122:1758–1763. 32. Shah C, Hari-Dass R, Raynes JG. Serum amyloid A is an innate immune opsonin for Gram-negative bacteria. Blood. 2006;108:1751–1757. 33. Hansen MT, Forst B, Cremers N, et al. A link between inflammation and metastasis: serum amyloid A1 and A3 induce metastasis, and are targets of metastasis-inducing S100A4. Oncogene. 2015;34:424–435. 34. Lung HL, Man OY, Yeung MC, et al. SAA1 polymorphisms are associated with variation in antiangiogenic and tumor-suppressive activities in nasopharyngeal carcinoma. Oncogene. 2015;34:878–889. Kidney International (2023) 103, 473–484 review 35. Connolly M, Mullan RH, McCormick J, et al. Acute-phase serum amyloid A regulates tumor necrosis factor alpha and matrix turnover and predicts disease progression in patients with inflammatory arthritis before and after biologic therapy. Arthritis Rheum. 2012;64:1035–1045. 36. de Beer MC, Wroblewski JM, Noffsinger VP, et al. The impairment of macrophage-to-feces reverse cholesterol transport during inflammation does not depend on serum amyloid A. J Lipids. 2013;2013:283486. 37. Ather JL, Dienz O, Boyson JE, et al. Serum amyloid A3 is required for normal lung development and survival following influenza infection. Sci Rep. 2018;8:16571. 38. Frame NM, Gursky O. Structure of serum amyloid A suggests a mechanism for selective lipoprotein binding and functions: SAA as a hub in macromolecular interaction networks. FEBS Lett. 2016;590:866–879. 39. Frame NM, Gursky O. Structure of serum amyloid A suggests a mechanism for selective lipoprotein binding and functions: SAA as a hub in macromolecular interaction networks. Amyloid. 2017;24(suppl 1): 13–14. 40. Haines MS, Ramirez E, Moore KBE, Fortin JS. Revisiting misfolding propensity of serum amyloid A1: special focus on the signal peptide region. Biochem Biophys Rep. 2022;31:101284. 41. Jayaraman S, Gantz DL, Haupt C, Gursky O. Serum amyloid A forms stable oligomers that disrupt vesicles at lysosomal pH and contribute to the pathogenesis of reactive amyloidosis. Proc Natl Acad Sci U S A. 2017;114:E6507–E6515. 42. Girnius S, Dember L, Doros G, Skinner M. The changing face of AA amyloidosis: a single center experience. Amyloid. 2011;18(suppl 1): 226–228. 43. Aguilera JJ, Zhang F, Beaudet JM, et al. Divergent effect of glycosaminoglycans on the in vitro aggregation of serum amyloid A. Biochimie. 2014;104:70–80. 44. Ogawa M, Shintani-Domoto Y, Nagashima Y, et al. Mass spectrometrybased absolute quantification of amyloid proteins in pathology tissue specimens: merits and limitations. PLoS One. 2020;15:e0235143. 45. Liepnieks JJ, Kluve-Beckerman B, Benson MD. Characterization of amyloid A protein in human secondary amyloidosis: the predominant deposition of serum amyloid A1. Biochim Biophys Acta. 1995;1270:81–86. 46. Booth DR, Booth SE, Gillmore JD, et al. SAA1 alleles as risk factors in reactive systemic AA amyloidosis. Amyloid. 1998;5:262–265. 47. Baba S, Masago SA, Takahashi T, et al. A novel allelic variant of serum amyloid A, SAA1 gamma: genomic evidence, evolution, frequency, and implication as a risk factor for reactive systemic AA-amyloidosis. Hum Mol Genet. 1995;4:1083–1087. 48. Jin L, Syrovets T, Scheller JS, et al. Comparative study on hyaluronic acid binding to murine SAA1.1 and SAA2.2. ACS Omega. 2019;4:13388– 13399. 49. Blank N, Hegenbart U, Dietrich S, et al. Obesity is a significant susceptibility factor for idiopathic AA amyloidosis. Amyloid. 2018;25: 37–45. 50. van den Berg SM, van Dam AD, Rensen PC, et al. Immune modulation of brown(ing) adipose tissue in obesity. Endocr Rev. 2017;38:46–68. 51. Delaleu J, Deshayes S, Rodrigues F, et al. Tumour necrosis factor receptor-1 associated periodic syndrome (TRAPS)-related AA amyloidosis: a national case series and systematic review. Rheumatology (Oxford). 2021;60:5775–5784. 52. Rodrigues F, Philit JB, Giurgea I, et al. AA amyloidosis revealing mevalonate kinase deficiency: a report of 20 cases including two new French cases and a comprehensive review of literature. Semin Arthritis Rheum. 2020;50:1370–1373. 53. Gillmore JD, Lovat LB, Persey MR, et al. Amyloid load and clinical outcome in AA amyloidosis in relation to circulating concentration of serum amyloid A protein. Lancet. 2001;358:24–29. 54. Hunter J, McGregor L. Do inflammatory rheumatic diseases still cause as much harm through amyloidosis? Amyloid. 2011;18(suppl 1):208–210. 55. Palladini G, Riva E, Basset M, et al. Prognostication of survival and progression to dialysis in AA amyloidosis. Amyloid. 2017;24(suppl 1): 136–137. 56. Hiki Y, Horii A, Kokubo T, et al. A case of rheumatoid arthritis with renal tubular amyloidosis. Nephron. 1994;68:394–395. 57. Uda H, Yokota A, Kobayashi K, et al. Two distinct clinical courses of renal involvement in rheumatoid patients with AA amyloidosis. J Rheumatol. 2006;33:1482–1487. 58. Sebastian A, McSherry E, Ueki I, Morris RC Jr. Renal amyloidosis, nephrotic syndrome, and impaired renal tubular reabsorption of bicarbonate. Ann Intern Med. 1968;69:541–548. 481 review 59. Friedman E, Farfel Z, Goldfarb D, Gafni J. Renal tubular acidosis after prolonged remission of nephrotic syndrome in amyloidosis associated with astrocytoma. South Med J. 1989;82:765–768. 60. Berns JS, Rapalino O, Fenves AZ, et al. Case 11-2020: a 37-year-old man with facial droop, dysarthria, and kidney failure. N Engl J Med. 2020;382: 1457–1466. 61. Aggarwal P, Aggarwal A, Dhingira S, Misra R. Renal involvement in rheumatoid arthritis: a case report and review of literature. J Indian Rheumatol Assoc. 2004;12:70–73. 62. Hsieh HS, Chang CF, Yang AH, et al. Antineutrophil cytoplasmic antibody-negative pauci-immune crescentic glomerulonephritis associated with rheumatoid arthritis: an unusual case report. Nephrology (Carlton). 2003;8:243–247. 63. Fushimi T, Takahashi Y, Kashima Y, et al. Severe protein losing enteropathy with intractable diarrhea due to systemic AA amyloidosis, successfully treated with corticosteroid and octreotide. Amyloid. 2005;12:48–53. 64. Ebert EC, Nagar M. Gastrointestinal manifestations of amyloidosis. Am J Gastroenterol. 2008;103:776–787. 65. Stankovic Stojanovic K, Hubert D, Leroy S, et al. Cystic fibrosis and AA amyloidosis: a survey in the French cystic fibrosis network. Amyloid. 2014;21:231–237. 66. Desai P, Mbachi C, Joshi U, Mba B. A tale of three rarities: secondary amyloid A (AA) amyloidosis caused by recurrent sialadenitis and complicated by pulmonary hypertension and adrenal insufficiency. Cureus. 2020;12:e7792. 67. Chincholi T, Ahmed T, Kumar Y, et al. Rare cause of thyroid enlargement: localized AA amyloid goiter - a case report. Int J Surg Case Rep. 2022;92:106876. 68. van Gameren II, Hazenberg BP, Bijzet J, van Rijswijk MH. Diagnostic accuracy of subcutaneous abdominal fat tissue aspiration for detecting systemic amyloidosis and its utility in clinical practice. Arthritis Rheum. 2006;54:2015–2021. 69. Kyle RA, Bayrd ED. Amyloidosis: review of 236 cases. Medicine (Baltimore). 1975;54:271–299. 70. Foli A, Palladini G, Caporali R, et al. The role of minor salivary gland biopsy in the diagnosis of systemic amyloidosis: results of a prospective study in 62 patients. Amyloid. 2011;18(suppl 1):80–82. 71. Verine J, Mourad N, Desseaux K, et al. Clinical and histological characteristics of renal AA amyloidosis: a retrospective study of 68 cases with a special interest to amyloid-associated inflammatory response. Hum Pathol. 2007;38:1798–1809. 72. Westermark GT, Sletten K, Westermark P. Massive vascular AAamyloidosis: a histologically and biochemically distinctive subtype of reactive systemic amyloidosis. Scand J Immunol. 1989;30:605–613. 73. Westermark GT, Sletten K, Grubb A, Westermark P. AA-amyloidosis: tissue component-specific association of various protein AA subspecies and evidence of a fourth SAA gene product. Am J Pathol. 1990;137:377– 383. 74. Yang GC, Gallo GR. Protein A-gold immunoelectron microscopic study of amyloid fibrils, granular deposits, and fibrillar luminal aggregates in renal amyloidosis. Am J Pathol. 1990;137:1223–1231. 75. Picken MM, Pelton K, Frangione B, Gallo G. Primary amyloidosis A: immunohistochemical and biochemical characterization. Am J Pathol. 1987;129:536–542. 76. Erdogmus S, Kendi Celebi Z, Akturk S, et al. Profile of renal AA amyloidosis in older and younger individuals: a single-centre experience. Amyloid. 2018;25:115–119. 77. Picken MM, Herrera GA. The burden of "sticky" amyloid: typing challenges. Arch Pathol Lab Med. 2007;131:850–851. 78. Satoskar AA, Burdge K, Cowden DJ, et al. Typing of amyloidosis in renal biopsies: diagnostic pitfalls. Arch Pathol Lab Med. 2007;131:917–922. 79. Vrana JA, Gamez JD, Madden BJ, et al. Classification of amyloidosis by laser microdissection and mass spectrometrybased proteomic analysis in clinical biopsy specimens. Blood. 2009;114:4957–4959. 80. Fernandez de Larrea C, Verga L, Morbini P, et al. A practical approach to the diagnosis of systemic amyloidoses. Blood. 2015;125:2239–2244. 81. Abildgaard N, Rojek AM, Moller HE, et al. Immunoelectron microscopy and mass spectrometry for classification of amyloid deposits. Amyloid. 2020;27:59–66. 82. Celtik A, Sen S, Keklik F, et al. A histopathological scoring and grading system to predict outcome for patients with AA amyloidosis. Int Urol Nephrol. 2020;52:1297–1304. 482 S Karam et al.: Renal AA amyloidosis: diagnosis and management 83. Okuda Y, Takasugi K. Successful use of a humanized anti-interleukin-6 receptor antibody, tocilizumab, to treat amyloid A amyloidosis complicating juvenile idiopathic arthritis. Arthritis Rheum. 2006;54: 2997–3000. 84. Hattori Y, Ubara Y, Sumida K, et al. Tocilizumab improves cardiac disease in a hemodialysis patient with AA amyloidosis secondary to rheumatoid arthritis. Amyloid. 2012;19:37–40. 85. Yamada Y, Ueno T, Irifuku T, et al. Tocilizumab histologically improved AA renal amyloidosis in a patient with multicentric Castleman disease: a case report. Clin Nephrol. 2018;90:232–236. 86. Inui K, Sawa N, Suwabe T, et al. Long term administration of tocilizumab improves renal amyloid A (AA) amyloidosis deposition in familial Mediterranean fever. Mod Rheumatol Case Rep. 2020;4: 310–311. 87. Keven K, Nergizoglu G, Ates K, et al. Remission of nephrotic syndrome after removal of localized Castleman’s disease. Am J Kidney Dis. 2000;35: 1207–1211. 88. Lee YH, Kim EY, Jeong DW, et al. Complete remission of nephrotic syndrome without resolution of amyloid deposit after anti-tumor necrosis factor alpha therapy in a patient with ankylosing spondylitis. J Clin Rheumatol. 2016;22:86–88. 89. Matsui M, Okayama S, Tsushima H, et al. Therapeutic benefits of tocilizumab vary in different organs of a patient with AA amyloidosis. Case Rep Nephrol. 2014;2014:823093. 90. Emery P, Breedveld FC, Hall S, et al. Comparison of methotrexate monotherapy with a combination of methotrexate and etanercept in active, early, moderate to severe rheumatoid arthritis (COMET): a randomised, double-blind, parallel treatment trial. Lancet. 2008;372: 375–382. 91. Maetzel A, Wong A, Strand V, et al. Meta-analysis of treatment termination rates among rheumatoid arthritis patients receiving disease-modifying anti-rheumatic drugs. Rheumatology (Oxford). 2000;39:975–981. 92. Choi HK, Hernan MA, Seeger JD, et al. Methotrexate and mortality in patients with rheumatoid arthritis: a prospective study. Lancet. 2002;359:1173–1177. 93. Wasko MC, Dasgupta A, Hubert H, et al. Propensity-adjusted association of methotrexate with overall survival in rheumatoid arthritis. Arthritis Rheum. 2013;65:334–342. 94. Leung YY, Yao Hui LL, Kraus VB. Colchicine–update on mechanisms of action and therapeutic uses. Semin Arthritis Rheum. 2015;45:341–350. 95. Ozdogan H, Ugurlu S. Familial Mediterranean fever. Presse Med. 2019;48(pt 2):e61–e76. 96. Zemer D, Revach M, Pras M, et al. A controlled trial of colchicine in preventing attacks of familial Mediterranean fever. N Engl J Med. 1974;291:932–934. 97. Dinarello CA, Wolff SM, Goldfinger SE, et al. Colchicine therapy for familial Mediterranean fever: a double-blind trial. N Engl J Med. 1974;291:934–937. 98. Goldstein RC, Schwabe AD. Prophylactic colchicine therapy in familial Mediterranean fever: a controlled, double-blind study. Ann Intern Med. 1974;81:792–794. 99. Wright DG, Wolff SM, Fauci AS, Alling DW. Efficacy of intermittent colchicine therapy in familial Mediterranean fever. Ann Intern Med. 1977;86:162–165. 100. Zemer D, Pras M, Sohar E, et al. Colchicine in the prevention and treatment of the amyloidosis of familial Mediterranean fever. N Engl J Med. 1986;314:1001–1005. 101. Saatci U, Bakkaloglu A, Ozen S, Besbas N. Familial Mediterranean fever and amyloidosis in children. Acta Paediatr. 1993;82:705–706. 102. Slobodnick A, Shah B, Krasnokutsky S, Pillinger MH. Update on colchicine, 2017. Rheumatology (Oxford). 2018;57(suppl 1):i4–i11. 103. Stewart S, Yang KCK, Atkins K, et al. Adverse events during oral colchicine use: a systematic review and meta-analysis of randomised controlled trials. Arthritis Res Ther. 2020;22:28. 104. Malle E, Steinmetz A, Raynes JG. Serum amyloid A (SAA): an acute phase protein and apolipoprotein. Atherosclerosis. 1993;102:131–146. 105. Dember LM. Amyloidosis-associated kidney disease. J Am Soc Nephrol. 2006;17:3458–3471. 106. Lane T, Wechalekar AD, Gillmore JD, et al. Safety and efficacy of empirical interleukin-1 inhibition using anakinra in AA amyloidosis of uncertain aetiology. Amyloid. 2017;24:189–193. 107. Miyagawa I, Nakayamada S, Saito K, et al. Study on the safety and efficacy of tocilizumab, an anti-IL-6 receptor antibody, in patients with Kidney International (2023) 103, 473–484 S Karam et al.: Renal AA amyloidosis: diagnosis and management 108. 109. 110. 111. 112. 113. 114. 115. 116. 117. 118. 119. 120. 121. 122. 123. 124. 125. 126. 127. 128. 129. rheumatoid arthritis complicated with AA amyloidosis. Mod Rheumatol. 2014;24:405–409. Hakala M, Immonen K, Korpela M, et al. Good medium-term efficacy of tocilizumab in DMARD and anti-TNF-alpha therapy resistant reactive amyloidosis. Ann Rheum Dis. 2013;72:464–465. Dember LM, Hawkins PN, Hazenberg BP, et al. Eprodisate for the treatment of renal disease in AA amyloidosis. N Engl J Med. 2007;356: 2349–2360. Pamuk ON, Kalyoncu U, Aksu K, et al. A multicenter report of biologic agents for the treatment of secondary amyloidosis in Turkish rheumatoid arthritis and ankylosing spondylitis patients. Rheumatol Int. 2016;36:945–953. Kuroda T, Tanabe N, Kobayashi D, et al. Treatment with biologic agents improves the prognosis of patients with rheumatoid arthritis and amyloidosis. J Rheumatol. 2012;39:1348–1354. Malcova H, Strizova Z, Milota T, et al. IL-1 inhibitors in the treatment of monogenic periodic fever syndromes: from the past to the future perspectives. Front Immunol. 2020;11:619257. Kisilevsky R, Lemieux LJ, Fraser PE, et al. Arresting amyloidosis in vivo using small-molecule anionic sulphonates or sulphates: implications for Alzheimer’s disease. Nat Med. 1995;1:143–148. Drug Discovery & Development. Bellus Health: Phase 3 results of Kiacta for AA amyloidosis. Published June 21, 2016. Accessed December 15, 2022. https://www.drugdiscoverytrends.com/bellus-health-phase-3results-of-kiacta-for-aa-amyloidosis/ Gillmore JD, Tennent GA, Hutchinson WL, et al. Sustained pharmacological depletion of serum amyloid P component in patients with systemic amyloidosis. Br J Haematol. 2010;148:760– 767. Richards DB, Cookson LM, Barton SV, et al. Repeat doses of antibody to serum amyloid P component clear amyloid deposits in patients with systemic amyloidosis. Sci Transl Med. 2018;10:eaan3128. Nevone A, Merlini G, Nuvolone M. Treating protein misfolding diseases: therapeutic successes against systemic amyloidoses. Front Pharmacol. 2020;11:1024. Richards D, Bamford M, Liefaard L, et al. Identification, preclinical profile, and clinical proof of concept of an orally bioavailable pro-drug of miridesap. Br J Pharmacol. 2020;177:1853–1864. Kluve-Beckerman B, Hardwick, Du L, Benson MD. AA amyloidosis: potential therapy with antisense oligonucleotides. Amyloid. 2011;18(suppl 1):200–202. KINERET [prescribing information]. Stockholm, Sweden: Swedish Orphan Biovitrum AB (publ). Accessed December 15, 2022. https:// www.kineretrx.com/ European Medicines Agency. Kineret. Updated July 20, 2022. Accessed December 15, 2022. https://www.ema.europa.eu/en/medicines/human/ EPAR/kineret Novartis. Ilaris. Accessed December 15, 2022. https://www.ilarishcp. com/ Kiniksa. Arcalyst. Accessed December 15, 2022. https://www.arcalyst. com/hcp?gclid¼Cj0KCQjwgMqSBhDCARIsAIIVN1WqjnqH2ovJe95 9VmWtg9JiAiz2SH2O1iL4-oNEdN9-AB6tfFY155MaAlvEEALw_wcB Junge G, Mason J, Feist E. Adult onset Still’s disease-the evidence that antiinterleukin-1 treatment is effective and well-tolerated (a comprehensive literature review). Semin Arthritis Rheum. 2017;47:295–302. Obici L, Meini A, Cattalini M, et al. Favourable and sustained response to anakinra in tumour necrosis factor receptor-associated periodic syndrome (TRAPS) with or without AA amyloidosis. Ann Rheum Dis. 2011;70:1511–1512. Sozeri B, Gulez N, Ergin M, Serdaroglu E. The experience of canakinumab in renal amyloidosis secondary to familial Mediterranean fever. Mol Cell Pediatr. 2016;3:33. Brik R, Butbul-Aviel Y, Lubin S, et al. Canakinumab for the treatment of children with colchicine-resistant familial Mediterranean fever: a 6month open-label, single-arm pilot study. Arthritis Rheumatol. 2014;66: 3241–3243. Varan O, Kucuk H, Babaoglu H, et al. Efficacy and safety of interleukin-1 inhibitors in familial Mediterranean fever patients complicated with amyloidosis. Mod Rheumatol. 2019;29:363–366. Cetin P, Sari I, Sozeri B, et al. Efficacy of interleukin-1 targeting treatments in patients with familial Mediterranean fever. Inflammation. 2015;38:27–31. Kidney International (2023) 103, 473–484 review 130. van der Hilst J, Moutschen M, Messiaen PE, et al. Efficacy of anti-IL-1 treatment in familial Mediterranean fever: a systematic review of the literature. Biologics. 2016;10:75–80. 131. Ugurlu S, Ergezen B, Egeli BH, et al. Safety and efficacy of antiinterleukin-1 treatment in 40 patients, followed in a single centre, with AA amyloidosis secondary to familial Mediterranean fever. Rheumatology (Oxford). 2020;59:3892–3899. 132. Leslie KS, Lachmann HJ, Bruning E, et al. Phenotype, genotype, and sustained response to anakinra in 22 patients with autoinflammatory disease associated with CIAS-1/NALP3 mutations. Arch Dermatol. 2006;142:1591–1597. 133. Srirangan S, Choy EH. The role of interleukin 6 in the pathophysiology of rheumatoid arthritis. Ther Adv Musculoskelet Dis. 2010;2:247–256. 134. Dayer JM, Choy E. Therapeutic targets in rheumatoid arthritis: the interleukin-6 receptor. Rheumatology (Oxford). 2010;49:15–24. 135. Waetzig GH, Rose-John S. Hitting a complex target: an update on interleukin-6 trans-signalling. Expert Opin Ther Targets. 2012;16:225– 236. 136. Mihara M, Kasutani K, Okazaki M, et al. Tocilizumab inhibits signal transduction mediated by both mIL-6R and sIL-6R, but not by the receptors of other members of IL-6 cytokine family. Int Immunopharmacol. 2005;5:1731–1740. 137. Hagihara K, Nishikawa T, Isobe T, et al. IL-6 plays a critical role in the synergistic induction of human serum amyloid A (SAA) gene when stimulated with proinflammatory cytokines as analyzed with an SAA isoform real-time quantitative RT-PCR assay system. Biochem Biophys Res Commun. 2004;314:363–369. 138. Ugurlu S, Hacioglu A, Adibnia Y, et al. Tocilizumab in the treatment of twelve cases with AA amyloidosis secondary to familial Mediterranean fever. Orphanet J Rare Dis. 2017;12:105. 139. Lane T, Gillmore JD, Wechalekar AD, et al. Therapeutic blockade of interleukin-6 by tocilizumab in the management of AA amyloidosis and chronic inflammatory disorders: a case series and review of the literature. Clin Exp Rheumatol. 2015;33(suppl 94):S46–S53. 140. Redondo-Pachon MD, Enriquez R, Sirvent AE, et al. Tocilizumab treatment for nephrotic syndrome due to amyloidosis in Behcet’s disease. Ren Fail. 2013;35:547–550. 141. Eriksson P, Molne J, Wirestam L, Sjowall C. Successful treatment of AA amyloidosis in ankylosing spondylitis using tocilizumab: report of two cases and review of the literature. Front Med (Lausanne). 2021;8: 661101. 142. Okuda Y. AA amyloidosis - benefits and prospects of IL-6 inhibitors. Mod Rheumatol. 2019;29:268–274. 143. Markham A, Patel T. Siltuximab: first global approval. Drugs. 2014;74: 1147–1152. 144. van Rhee F, Voorhees P, Dispenzieri A, et al. International, evidencebased consensus treatment guidelines for idiopathic multicentric Castleman disease. Blood. 2018;132:2115–2124. 145. Sitenga J, Aird G, Ahmed A, Silberstein PT. Impact of siltuximab on patient-related outcomes in multicentric Castleman’s disease. Patient Relat Outcome Meas. 2018;9:35–41. 146. Cunnane G. Amyloid precursors and amyloidosis in inflammatory arthritis. Curr Opin Rheumatol. 2001;13:67–73. 147. Elkayam O, Hawkins PN, Lachmann H, et al. Rapid and complete resolution of proteinuria due to renal amyloidosis in a patient with rheumatoid arthritis treated with infliximab. Arthritis Rheum. 2002;46: 2571–2573. 148. Gottenberg JE, Merle-Vincent F, Bentaberry F, et al. Anti-tumor necrosis factor alpha therapy in fifteen patients with AA amyloidosis secondary to inflammatory arthritides: a followup report of tolerability and efficacy. Arthritis Rheum. 2003;48:2019–2024. 149. Kuroda T, Wada Y, Kobayashi D, et al. Effective anti-TNF-alpha therapy can induce rapid resolution and sustained decrease of gastroduodenal mucosal amyloid deposits in reactive amyloidosis associated with rheumatoid arthritis. J Rheumatol. 2009;36:2409–2415. 150. Nakamura T, Higashi S, Tomoda K, et al. Etanercept can induce resolution of renal deterioration in patients with amyloid A amyloidosis secondary to rheumatoid arthritis. Clin Rheumatol. 2010;29:1395–1401. 151. Fernandez-Nebro A, Olive A, Castro MC, et al. Long-term TNF-alpha blockade in patients with amyloid A amyloidosis complicating rheumatic diseases. Am J Med. 2010;123:454–461. 483 review 152. Denis MA, Cosyns JP, Persu A, et al. Control of AA amyloidosis complicating Crohn’s disease: a clinico-pathological study. Eur J Clin Invest. 2013;43:292–301. 153. Kuroda T, Otaki Y, Sato H, et al. A case of AA amyloidosis associated with rheumatoid arthritis effectively treated with infliximab. Rheumatol Int. 2008;28:1155–1159. 154. Nakamura T, Higashi S, Tomoda K, et al. Effectiveness of etanercept vs cyclophosphamide as treatment for patients with amyloid A amyloidosis secondary to rheumatoid arthritis. Rheumatology (Oxford). 2012;51:2064–2069. 155. Okuda Y, Ohnishi M, Matoba K, et al. Comparison of the clinical utility of tocilizumab and anti-TNF therapy in AA amyloidosis complicating rheumatic diseases. Mod Rheumatol. 2014;24:137–143. 156. Nedjai B, Hitman GA, Yousaf N, et al. Abnormal tumor necrosis factor receptor I cell surface expression and NF-kappaB activation in tumor necrosis factor receptor-associated periodic syndrome. Arthritis Rheum. 2008;58:273–283. 157. Nedjai B, Hitman GA, Quillinan N, et al. Proinflammatory action of the antiinflammatory drug infliximab in tumor necrosis factor receptor-associated periodic syndrome. Arthritis Rheum. 2009;60: 619–625. 158. Rubbert-Roth A, Finckh A. Treatment options in patients with rheumatoid arthritis failing initial TNF inhibitor therapy: a critical review. Arthritis Res Ther. 2009;11(suppl 1):S1. 159. Narvaez J, Hernandez MV, Ruiz JM, et al. Rituximab therapy for AAamyloidosis secondary to rheumatoid arthritis. Joint Bone Spine. 2011;78:101–103. 484 S Karam et al.: Renal AA amyloidosis: diagnosis and management 160. Pamuk ON, Donmez S, Pamuk GE, et al. Turkish experience in rheumatoid arthritis patients with clinical apparent amyloid deposition. Amyloid. 2013;20:245–250. 161. Kilic L, Erden A, Sener YZ, et al. Rituximab therapy in renal amyloidosis secondary to rheumatoid arthritis. Biomolecules. 2018;8:136. 162. Soriano A, Verecchia E, Afeltra A, et al. IL-1beta biological treatment of familial Mediterranean fever. Clin Rev Allergy Immunol. 2013;45:117–130. 163. Trabulus S, Korkmaz M, Kaya E, Seyahi N. Canakinumab treatment in kidney transplant recipients with AA amyloidosis due to familial Mediterranean fever. Clin Transplant. 2018;32:e13345. 164. Yilmaz S, Cinar M, Simsek I, et al. Tocilizumab in the treatment of patients with AA amyloidosis secondary to familial Mediterranean fever. Rheumatology (Oxford). 2015;54:564–565. 165. Kuroda T, Tanabe N, Nozawa Y, et al. Effects of biologic agents in patients with rheumatoid arthritis and amyloidosis treated with hemodialysis. Intern Med. 2016;55:2777–2783. 166. Bollee G, Guery B, Joly D, et al. Presentation and outcome of patients with systemic amyloidosis undergoing dialysis. Clin J Am Soc Nephrol. 2008;3:375–381. 167. Kofman T, Grimbert P, Canoui-Poitrine F, et al. Renal transplantation in patients with AA amyloidosis nephropathy: results from a French multicenter study. Am J Transplant. 2011;11:2423–2431. 168. Law S, Cohen O, Lachmann HJ, et al. Renal transplant outcomes in amyloidosis. Nephrol Dial Transplant. 2021;36:355–365. 169. Ozcakar ZB, Ozdel S, Yilmaz S, et al. Anti-IL-1 treatment in familial Mediterranean fever and related amyloidosis. Clin Rheumatol. 2016;35: 441–446. Kidney International (2023) 103, 473–484

![Anti-Apolipoprotein A I antibody [1405] ab20735 Product datasheet Overview Product name](http://s2.studylib.net/store/data/013572528_1-4a321b1d50b8bcc44ab392bbbdd347d2-300x300.png)

![Anti-Apolipoprotein A I antibody [1402] ab20411 Product datasheet Overview Product name](http://s2.studylib.net/store/data/013572527_1-7106be9823f653a7d46ace3d2c577bec-300x300.png)