LOH & Aggressive Lymph Nodes in Papillary Thyroid Carcinoma
advertisement

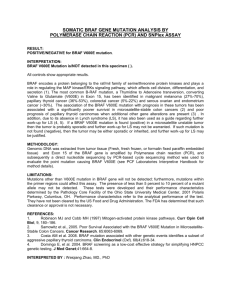
Pathology - Research and Practice 251 (2023) 154842 Contents lists available at ScienceDirect Pathology - Research and Practice journal homepage: www.elsevier.com/locate/prp Functional loss of tumor suppressor genes detected by loss of heterozygosity, but not driver mutations, predicts aggressive lymph node status in papillary thyroid carcinoma Sydney Finkelstein a, Venkata Arun Timmaraju a, Shabnam Samankan b, Quinn O’Malley c, Danielle Kapustin c, d, Sarah Spaulding c, Monica Xing c, Ammar Matloob b, John Beute c, Gabriella Seo c, Michael Saturno c, Lily Greenberg c, Lauren Wein c, Camilo Gonzalez-Velazquez c, Scott Doyle e, Jonathan Levine a, Mark Urken c, d, Margaret Brandwein-Weber b, * a Interpace Diagnostics, Interpace Biosciences, Pittsburgh, PA, United States Department of Pathology, Icahn School of Medicine, Mount Sinai Health System, New York, United States c THANC (Thyroid, Head and Neck Cancer) Foundation, 10 Union Square East, New York, NY 10003, United States d Department of Otolaryngology — Head and Neck Surgery, Icahn School of Medicine, Mount Sinai Health System, New York, NY, United State e Department of Pathology and Anatomical Sciences, University at Buffalo, Jacobs School of Medicine, Buffalo, NY, United States b A R T I C L E I N F O A B S T R A C T Keywords: Papillary thyroid carcinoma Loss of heterozygosity LOH ATA Aggressive lymph nodes Background: Recognizing aggressive tumor biology is essential to optimizing patient management for papillary thyroid carcinomas (PTC). Aggressive lymph node (ALN) status is one feature that influences decision-making. We evaluated genomic deletions in regions of tumor suppressor genes, detected by loss of heterozygosity (LOH) analysis, to understand causal alterations linked to thyroid cancer aggressiveness and to serve as a mo­ lecular diagnostic biomarker for ALN status. Methods: We analyzed 105 primary PTC enriched for patients with ALN (64% with, 36% without). We also analyzed 39 positive lymph nodes (79% with, 21% without ALN). LOH was determined using a panel of 25 polymorphic microsatellite alleles targeting 10 genomic loci harboring common tumor suppressor genes. Additionally, ThyGeNEXT® and ThyraMIR® assays were performed. Results: LOH was detected in 43/67 primary PTC from patients with ALN status, compared with only 5/38 primary PTC without ALN (minimal metastatic burden) (P=0.0000003). This is further supported by post hoc analyses of paired primary and metastatic samples. Paired samples from patients with ALN are more likely to harbor LOH, compared to the ALN negative group (P=0.0125). Additionally, 12/31 paired samples from patients with ALN demonstrated additional or different LOH loci in metastatic samples compared to the primary tumor samples. No association was seen between ALN and mutational, translocation, or microRNA data. Conclusions: LOH detected in primary PTC significantly predicts ALN status. Analysis of paired primary and metastatic samples from patients with / without ALN status further supports this relationship. The acquisition of LOH at additional loci is common in lymph nodes from patients with ALN status. Simple summary: A subset of patients with papillary thyroid carcinoma (PTC) will develop recurrent disease. One known predictor of recurrence is the American Thyroid Association category “Aggressive Lymph Node” (ALN) disease, considering metastatic burden. Loss of heterozygosity (LOH) — chromosomal loss in regions of tumor suppressor genes — has yet to be investigated as a possible mechanism driving ALN status in PTC. The ability to predict ALN status prior to surgery can guide the extent of surgery and postoperative treatment options. We found that paired samples from patients with ALN are more likely to harbor LOH, compared to patients without ALN disease. 38% of patients with ALN demonstrated additional or different LOH loci in metastatic samples compared to the primary tumor samples. LOH complements current molecular analysis of thyroid cancer when searching for evidence of aggressive biology. * Corresponding author. E-mail address: Margaret.brandwein@mountsinai.org (M. Brandwein-Weber). https://doi.org/10.1016/j.prp.2023.154842 Received 24 August 2023; Accepted 30 September 2023 Available online 4 October 2023 0344-0338/© 2023 Elsevier GmbH. All rights reserved. S. Finkelstein et al. Pathology - Research and Practice 251 (2023) 154842 lymph node (ALN) status and long-term follow-up, from 2010 onward. Aggressive lymph node (ALN) status considers metastatic burden and is a more meaningful indicator of aggressive behavior, as compared to binary lymph node status (negative or positive). It is defined as either more than five positive lymph nodes, one or more positive lymph node larger than 3 cm, or four or more positive lymph nodes with extranodal extension (ENE). Inclusion criteria included availability of all pathology slides and adequacy of tumor submission for histology. PTCs up to 4 cm were routinely submitted in entirety. Recuts from corresponding paraffin blocks were performed if slides were unavailable or the his­ tology was suboptimal. A cohort of 105 patient samples with known ALN status (positive ALN= 67, negative ALN= 38) were submitted for blin­ ded molecular analysis. Primary thyroid cancer tissue was manually microdissected from unstained 4-micron thick recut tissue sections of the formalin-fixed paraffin-embedded tissue blocks under stereomicro­ scopic guidance (SZ-PT, Olympus microscopes) using the hematoxylineosin stained tissue section. Sufficient nucleic acid for mutational, miRNA expression, and loss of heterozygosity (LOH) analysis was ob­ tained from manual microdissection of eight serial, four micron thick unstained recut tissue sections. Based on the results of the tumor pri­ mary molecular analysis, a subset of formalin-fixed paraffin-embedded positive lymph node samples from 39 patients (31 with ALN, 8 without ALN) were subsequently randomly selected for post-hoc molecular analysis. 1. Introduction An understanding of cancer biological aggressiveness can be clini­ cally impactful in optimizing patient management, especially at the outset of a cancer diagnosis, enabling more informed planning of sur­ gery and the use of other therapeutic modalities. A small subset of pa­ tients with well-differentiated thyroid carcinomas will pursue an aggressive clinical course [1]. Early diagnosis for patients facing recurrence and or metastatic spread is a critical means to achieve the best outcome. The American Thyroid Association (ATA) has developed the risk of recurrence (ROR) classification system for surgical and postoperative decision paradigms [2]. The ATA-ROR system describes aggressive lymph node (ALN) status in terms of the cumulative meta­ static burden, taking into account 1) the total number of positive lymph nodes, 2) metastatic lymph node size, and 3) presence of extranodal metastatic tumor invasion. Specifically, ALN status is defined as either more than five positive lymph nodes, one or more positive lymph node larger than 3 cm, or four or more positive lymph nodes with extranodal extension. The ATA-ROR designation of ALN status has been shown to be a more clinically meaningful indicator of aggressive behavior than designating lymph node status as either negative or positive [2,3]. We selected the ALN phenotype as the study outcome for two reasons. Firstly, it is generally challenging to correlate biomarkers with adverse outcome for PTC patients as initial local recurrence can develop decades after primary treatment. A large cohort size with a long mean follow-up is required to adequately power an outcome study. Therefore we framed our investigation by enriching the study cohort with a known surrogate for poor outcome, namely ALN status. Secondly, the finding of ALN impacts therapeutic options. We sought to better understand the mo­ lecular basis of ALN phenotypes and, more particularly, to better un­ derstand its role based on the molecular changes detected in the primary thyroid malignancy so this prognostic approach may be considered when planning initial oncologic therapy. Thyroid tumorigenesis involves the stepwise accumulation of mo­ lecular alterations that ultimately determine phenotypic expression including tumor biological aggressiveness [4]. Genomic as well as epi­ genomic changes have been shown to contribute to thyroid cancer development and progression [5]. While the greatest attention has centered on thyroid cancer-associated gene families and oncogenic translocations, we and others have shown that microRNA (miRNA) classification, an important epigenomic controller of phenotypic expression, together with defects in other cellular mechanisms play an important causative role in the development, progression and clinical expression of thyroid cancer [6–8]. Tumor suppressor gene (TSG) loss is an important alteration that has been reported in thyroid cancers, generally regarded to be a later event in cancer progression [9]. We and others have previously shown that loss of heterozygosity (LOH) is indicative of the second of the Knudsen’s two step inactivation of tumor suppressor gene function [10]. Published data support the notion that LOH tends to be associated with relatively greater thyroid cancer bio­ logical aggressiveness [9]. Here we explore the relationship between LOH and ALN, which supports the hypothesis that the role of LOH in chromosomal regions close to known tumor suppressor gene loci can be a biomarker of thyroid cancer aggressive etiology. More specifically, we show that detection of LOH in the primary thyroid malignancy is asso­ ciated with ALN status, in keeping with a causal role leading to aggressive biology in this important subset of thyroid cancer patients. 2.1. Molecular analysis Three molecular platforms were used for analysis in this study: 1) next-generation sequencing (NGS, Illumina) genomic mutational panel, detecting gene sequence variations and/or translocation mutations; 2) miRNA classifier, which includes biomarkers for malignancy risk strat­ ification [9]; and 3) fragment analysis by means of capillary electro­ phoresis of TSG-related LOH. All molecular testing was performed using standard clinical procedures for the ThyGeNEXT® mutation panel and ThyraMIR® miRNA risk classifier commercial tests, and for LOH anal­ ysis at Interpace Diagnostics as previously described [6–14]. The expanded mutation panel test (ThyGeNEXT) utilizes targeted NGS (Illumina) to detect DNA-based gene mutation variants and mRNA fusion transcripts, listed in Table 1. For a positive variant call, a spec­ imen was required to contain at least 3% BRAF V600E, 10% GNAS, or 5% other individual DNA variants in the panel. All samples required predominance of PAX8 and NKX2.1 messenger RNA (mRNA) expression to confirm thyroid follicular cell content. A minimum coverage of 1000 copies had to be met for each targeted genomic region or fusion product. All mutational testing was performed in duplicate with the specific sequence alteration confirmed in both replicates. Microdissected sam­ ples typically are composed of a chimeric mixture of cancers cells in Table 1 Genomic and microRNA Targets for ThyGeNEXT and ThyraMIR Testing. Expanded Mutation Panel (ThyGeNEXT) 2. Materials and methods This study was approved by the Mount Sinai Health System (MSHS) Institutional Review Board. Study inclusion criterion was patients treated at MSHS with primary surgery for PTC with curative intent. All eligible patients from 2017 onward were entered sequentially into this study. In addition, personal patient databases from one of the authors, MLU, were used to enrich this cohort for PTC patients with aggressive DNA variant Fusions (N) and mRNA microRNA Risk Classifier (ThyraMIR) miRNA BRAF† ALK GNAS HRAS KRAS NRAS PIK3CA PTEN RET‡ TERT promoter‡ BRAF (3)‡ ALK (2) NTRK (8) PPARg (5) RET (14)‡ THADA (5) NKX2.1 PAX8 TBP USP33 miR-31–5p miR-29b-1–5p miR-138–1–3p miR-139–5p miR-146b-5p miR-155 miR-204–5p miR-222–3p miR-375 miR-551b-3p BRAF V600E is a strong driver mutation, while BRAF K601E is a weak driver mutation ‡ Strong driver mutation mRNA (messenger RNA) † 2 S. Finkelstein et al. Pathology - Research and Practice 251 (2023) 154842 which a subset of microdissected cancer cells contain these mutations usually acquired later in tumorigenesis. Analytical validation of the ThyGeNEXT assay has been previously reported [13]. The miRNA risk classifier test (ThyraMIR) was performed using a validated panel of 10 specific miRNAs tested using quantitative reverse transcription poly­ merase chain reaction (RT-PCR) (QuantStudio) to evaluate miRNA expression levels in relation to one another. The panel of miRNAs tested is listed in Table 1. LOH analysis was carried out on an analytical and clinical validated panel of 25 polymorphic microsatellite alleles situated in close prox­ imity to common tumor suppressor genes (TSG) at 10 genomic loci [9]. LOH markers target the following genomic loci with corresponding cancer genes: 1p (LMYC), 3p (VHL, OGG1), 5q (APC), 9p (CDKN2A, CDKN2B), 10q (PTEN), 17p (TP53), 17q (RNF43), 18q (SMAD4, DCC), 21q (PSEN2) and 22q (NF2). LOH analysis was based on fragment analysis separated by length using capillary electrophoresis (Applied Biosystem) targeted polymorphic microsatellites located within or in proximity of well characterized tumor suppressor genes [9]. Micro­ satellites were PCR amplified using flanking fluorescent labeled oligo­ nucleotides (Integrated DNA Technologies) according to manufacturer’s recommendations (Applied Biosystems). LOH analysis utilized known homozygous microsatellite allele controls assembled to meet pre­ determined alleles admixtures [9]. Specimens consisted of unstained four-micron thick formalin-fixed paraffin-embedded tissue sections from 94 patients with primary carcinomas, and random subset of positive lymph nodes from 34 patients. All sample slides were microdissected under stereoscopic guidance followed by extraction of total nucleic acid as previously described [11–14]. Analytical validation of LOH analysis was based on known admixtures of polymorphic microsatellite alleles using blood samples of subjects with previously determined non­ informative single alleles. Laboratory staff performing the molecular analysis were performed blinded to ALN status and clinical patient outcome. 2.3. Statistics Chi-square tests (cell count ≥ 5) and Fisher’s exact tests (cell count < 5) were used to assess the relationship between categorical variables. The Freeman-Halton extension of Fisher’s exact test was used to compute two-tailed probabilities for distribution values in 2 × 3 con­ tingency tables. Kruskal–Wallis test and Wilcoxon rank-sum test were performed to compare the continuous variables among three groups and two groups, respectively. Kaplan–Meier outcome analyses, Log-rank tests and Cox proportional hazards analyses were performed for disease-free survival (DFS). All reported P values were two-sided; sta­ tistical significances were claimed at ≤ 0.05. 3. Results 3.1. Patient cohort and outcome This cohort consists of 105 patients (38 men, 67 women), ages 16 – 82 (mean 44 years). As we are interested in predictive biomarkers of ALN status, the cohort was deliberately enriched for patients of interest. Thus, 67 patients (64%) were ALN positive, and 38 patients (36%) were negative for ALN status (including cNx patients) for a ratio of 2:1. By comparison, in our larger published cohort of 347 PTC patients, ALN status represented 32% of the total cohort for a ratio of 1:2 [15]. Post treatment disease status was known for 93 patients (mean follow-up 55 months): two patients manifested disease persistence in regional lymph nodes (2 and 3 months) and 10 patients developed recurrence in regional lymph nodes (12–60 months, mean 26). There were no cases of biochemical recurrence only. 3.2. Molecular analysis including LOH determination One or more TSG-related LOH mutations was detected in 48 of 105 patients (46%) (Table 2). All genomic loci tested (10 loci) were found to harbor at least one detectable LOH mutation. The number of LOH markers varied from one to four; 35 patients (73%) had one marker, nine patients (19%) had two markers, two patients (4%) had three markers, 2.2. Outcomes Patients were treated according to current American Thyroid Asso­ ciation (ATA) guidelines for extent of surgery and administration of adjuvant radioiodine therapy [2]. Patients were monitored post­ operatively with ultrasound and biochemical parameters, in line with ATA guidelines. Disease persistence is defined as newly recognized disease less than six months after a total thyroidectomy. This reflects the reality that suboptimal preoperative ultrasound or intraoperative eval­ uation may lead to incomplete surgery and therefore disease persistence. New disease manifesting six months or later after total thyroidectomy is classified as recurrence. For patients classified as recurrence-free, a minimum of six months follow-up was required; disease-free patients with fewer than six months of follow-up were excluded from outcome analysis. The last available serum thyroid stimulating hormone (TSH), thyroglobulin and thyroglobulin antibody titers were abstracted; pa­ tients with significantly elevated serum thyroid cancer markers, but no pathological/radiographic evidence of recurrent PTC, were classified as "biochemical recurrence." Kaplan–Meier analysis measured disease-free survival from date of surgery to either first date of disease progression, or last known disease-free date. Clinicopathologic, demographic, and outcome data were stored in a HIPAA (Health Insurance Portability and Accountability Act)-compliant Microsoft Access database. The following collected data is part of this analysis: gender, age, tumor size (centimeter (cm)), degree of extra­ thyroid extension (ETE: intrathyroidal, microscopic ETE, histologic spread to strap muscles, or pT4 disease), extranodal extension (ENE), ALN status, tumor multifocality, tumor necrosis, vascular invasion, perineural invasion, and lymphatic tumor emboli. Table 2 Summary of Molecular Data on 105 Primary Papillary Thyroid Carcinomas. Mutational Status None BRAF V600E BRAF V600E & TERT CCDC6::RET NCOA4::RET ETV6::NTRK3 AGK::BRAF KRAS Q61K BRAF V600E & PARG::BMS1 Failed MicroRNA expression level Level – 1 Level – 2 Level – 3 Specific chromosomal loci and associated TSG 3p (VHL, OGG1) 17q (RNF43, NMEI1) 1p (RUNX3, CMM1, LMYC) 10q (PTEN, MXI1) 22q (NF2) 5q (MCC, APC) 9p (CDKN2A, CDKN2B) 17p (TP53) 18q (SMAD4, DCC) 21q (TFF1, PSEN2) 3 n 13 62 15 6 2 2 1 1 1 Loss of Heterozygosity Status Primary PTC n No LOH Any LOH 57 48 1 LOH detected 2 LOH detected 3 LOH detected 4 LOH detected 35 9 2 2 2 1 1 103 Frequency (n) 18 12 9 6 5 4 4 4 3 1 S. Finkelstein et al. Pathology - Research and Practice 251 (2023) 154842 and two patients (4%) had four LOH markers (Table 2). Chromosomal locus 3p was the most commonly affected genomic site for LOH (single loss, n = 11, multiple losses, n = 7), followed by loss of 17q (single loss, n = 7, multiple losses, n = 5) (Table 2). No LOH was detected in 57 (54%) of primary tumors for this 105-patient cohort. Mutational change was frequent in this cohort enriched for aggres­ sive disease (Table 2). Not surprisingly, BRAF V600E-like, “strong” driver type mutations, dominated mutation genotypes in the thyroid follicular lining cell malignancies. BRAF V600E was the most common mutation detected, either as the sole mutation 62/102 (61%) or as BRAF V600E plus TERT promoter mutation (15/102, or 15%, Table 2). RET fusions were present in eight patients (CCDC6::RET = 6, NCOA4::RET = 2). Remaining cases showed a variety of mutational changes and mRNA fusions (AGK::BRAF, KRAS Q61K, NRAS, ETV6::NTRK3, and NTRK3 plus TERT) (Table 2). Only one cancer manifested “weak” (RAS-like) driver type mutations consisting of KRAS point mutations. Nine patients lacked detectable mutational change in their primary thyroid cancers. Muta­ tional analysis failed in two cases; these were still included in this cohort as LOH data is available for these patients. miRNA risk classification indicated positive status in all but two thyroid cancer samples (Table 2) in keeping with the neoplastic lesion having undergone malignant transformation. Positive overexpression recognizes two levels as previously described [6] consisting of a lower state of overexpression associated with greater sensitivity for detection of malignancy (Level-2) and a higher state of overexpression associated with greater specificity for detection of malignancy (Level-3). All pa­ tients with positive ALN status showed Level-3 strong positive over­ expression of miRNA. Of note, all mutation negative thyroid cancers in this series exhibited strong positive, Level-3 miRNA overexpression (Table 2). Table 3 demonstrates the relationship between LOH and phenotypic features of aggressive biological behavior. LOH was detected in the majority of primary tumors of patients with ALN status (43/67, 64%). In contrast, LOH was uncommonly detected in primary tumors of patients with non-ALN status (5/38, 13%). Therefore, LOH detected in primary thyroid cancers is strongly predictive of ALN status (P=0.0000003). The same was true for two components of ALN: extranodal extension (P=0.000007), and metastases involving more than five lymph nodes (P=0.000022). These data lead to post-hoc analysis of positive cervical lymph node samples from 39 randomly selected patients (31 with ALN, 8 negative ALN status). Table 4 summarizes the paired primary cancer and lymph node LOH and mutational data stratified for ALN status. Paired primary and lymph node samples from patients with ALN more commonly harbored LOH (19/31 or 61%), compared to ALN negative group samples (1/8 or 13%, P=0.0125, two-tailed Fisher exact test). Accumulation of additional or different LOH loci in positive lymph node samples, compared with primary tumors, is common in the ALN+ group. In contrast, the mutational driver status remained the same in paired primary and metastatic samples in all but one ALN positive patient (primary PTC no mutation, metastatic carcinoma BRAF V600E+, Table 4). No association was seen with LOH status and patient age (cutpoint 50 years), gender, tumor size, perineural invasion, lymphatic invasion, vascular invasion, tumor multifocality, necrosis, or degree of extrathyroid extension on Student t-test. BRAF V600E point mutation, with or without TERT promoter region mutational change was acquired by the majority of thyroid cancers in this series. Gene mutations were not associated with either LOH status, ALN status, or extrathyroid extension, with respect to BRAF V600E point mutation plus TERT promoter mutation versus BRAF V600E point mu­ tation alone, or versus other or no mutations. Positive status of the miRNA-risk classifier, a general indicator of thyroid nodule malignant transformation, did not associate with ALN status. With respect to outcome prognostication, Kaplan–Meier analysis was significant for decreased disease-free survival for BRAF V600E with TERT promoter mutation versus BRAF V600E, (P=0.002, HR 16.01, 95% CI 2.7, 92.9). Trends were seen for decreased disease-free survival and LOH (P=0.09, HR 3.1, 95% CI 0.8, 11.9) and also for ALN status (P=0.18, HR 2.6, 95% CI 0.64, 11.0) (Fig. 1). No associations wwere found between time to recurrence and gender, patient age (cut point age 50), tumor size, extranodal extension, degree of extrathyroid extension, or multifocal disease. Cox regression analysis was not significant. 4. Discussion Prior studies on loss of heterozygosity alterations support the idea that loss of tumor suppressor genes (TSG) are relatively late events in thyroid cancer progression and correlate with increased biological aggressiveness [9]. This is the first demonstration of the association between LOH and ALN status (P=0.0000003). Subgroup analysis confirmed that paired primary and positive lymph node samples from patients with ALN more commonly harbored LOH (19/31 or 61%), compared to ALN-negative (low metastatic burden) paired samples (1/8 or 13%, P=0.0125, two-tailed Fisher exact test). LOH is a marker of genomic instability that impacts tumor suppressor genes. These data support the role of LOH as a potential biological and prognostic marker to identify the subset of thyroid cancers that are likely to show aggres­ sive biology and worse outcomes. The BRAF V600E strong driver mutation is common in papillary thyroid carcinoma (PTC) [4]. A landmark multicenter study of over 1, 800 PTC patients demonstrated that BRAF V600E was significantly related to disease-specific mortality and synergistic with other adverse features (older age, Stage IV, distant metastasis) [15]. High-risk sec­ ondary TERT promoter mutations can be present in a subgroup of papillary thyroid carcinoma and are known predictors of lower disease-free survival rates [16]. Here we demonstrate that LOH is strongly associated with ALN status (Table 3), a known surrogate for the outcome of disease progression. A variety of BRAF V600E-like, strong driver mutations, were seen in this series, which was enriched for aggressive thyroid malignancies (Table 2, Table 4). However, there was no exclusive driver mutation that correlated with ALN. This supports the idea that tumor suppressor gene loss is an additional event, independent of driver mutation, associated with a surrogate marker of increased thyroid cancer biological aggressiveness (ALN status). We also demon­ strate that the accumulation of additional or different LOH loci in Table 3 Papillary Thyroid Carcinoma With/Without Aggressive Lymph Node Status (N = 105): LOH Status Within the Primary PTC. LOH ≥ 2 LOH 1 locus No LOH Total ALN No ALN p ENE No ENE p > 5 +LN ≤ 5 LN 12 31 24 67 1 4 33 38 0.000003 11 22 13 46 1 10 36 47 0.000007 12 30 24 6 4 31 37 N = Number of patients in each cell LOH: Loss of heterozygosity PTC: Papillary thyroid carcinoma ALN: Aggressive lymph node status ENE: Extranodal extension LN: Lymph node 4 p 0.000022 S. Finkelstein et al. Pathology - Research and Practice 251 (2023) 154842 Table 4 LOH and Mutational Analysis on Paired Primary Tumor and Positive Lymph Node Samples per ALN Category. Aggressive Lymph Node Status (N = 31) Primary PTC LOH status 10q 10q 17q 17q 17q 17q 17q 18q 1p 10q 17p 17q 1p, 3p 1p10q 1p17q 22q 3p 3p 3p 3p 5q 9q No LOH No LOH No LOH No LOH No LOH No LOH No LOH No LOH No LOH No LOH No LOH No LOH Limited metastatic burden (N = 8) + LN Driver Mutation BRAF V600E BRAF V600E ETV6: :NTRK3 BRAF V600E BRAF V600E BRAF V600E None BRAF V600E TERT C228T LOH status BRAF V600E TERT C228T BRAF V600E TERT C228T BRAF V600E TERT C228T CCDC6: :RET BRAF V600E CCDC6: :RET BRAF V600E CCDC6: :RET BRAF V600E BRAF V600E BRAF V600E BRAF V600E BRAF V600E BRAF V600E TERT C228T None None None BRAF V600E BRAF V600E BRAF V600E BRAF V600E BRAF V600E BRAF V600E 1p 10q 17p 17q 5q 22q * 1p10q 1p17q 7p9p10q18q* 3p10q17q* 3p 17q * 17q 22q* 17q 22q* 17q 17q 18q 22q 9p17q* 3p17q* 3p 5q* 3p 5q 10q* 9p 17q* 17q* No LOH No LOH No LOH No LOH No LOH No LOH No LOH No LOH No LOH No LOH Primary PTC Driver Mutation BRAF V600E BRAF V600E ETV6: :NTRK3 BRAF V600E BRAF V600E BRAF V600E None BRAF V600E TERT C228T LOH status + LN LOH status No LOH No LOH No LOH Driver Mutation None None BRAF V600E No LOH No LOH No LOH No LOH 17q BRAF BRAF BRAF BRAF BRAF No LOH No LOH No LOH No LOH 1p17q* V600E V600E V600E V600E V600E TERT C228T BRAF V600E TERT C228T BRAF V600E TERT C228T BRAF V600E TERT C228T CCDC6: :RET BRAF V600E CCDC6: :RET BRAF V600E CCDC6: :RET BRAF V600E BRAF V600E BRAF V600E BRAF V600E BRAF V600E BRAF V600E TERT C228T None None BRAF V600E* BRAF V600E BRAF V600E BRAF V600E BRAF V600E BRAF V600E BRAF V600E No LOH No LOH No LOH Driver Mutation None None BRAF V600E BRAF V600E BRAF V600E BRAF V600E BRAF V600E BRAF V600E TERT C228T Legend Metastatic carcinoma has acquired additional or different chromosomal losses, as compared to the primary carcinoma LOH: Loss of heterozygosity. PTC: Papillary thyroid carcinoma ALN: Aggressive lymph node status +LN: Positive lymph node positive lymph node samples is common in the ALN+ group, as compared with primary tumors, further supporting that these are later events of cancer progression. In contrast, the mutational driver status remained stable in paired primary and metastatic samples, for all but one ALN positive patient (primary PTC no mutation, metastatic carci­ noma BRAF V600E+, Table 4). The acquisition of LOH appears to differentially favor certain genomic loci suggesting specific tumor suppressor genes that are pref­ erentially responsible for increased cancer aggressiveness (Table 2). Chromosome 3p loss was the single most observed genomic locus showing LOH. The interrogated region, 3p24, harbors several common tumor suppressor genes including von Hippel Lindau (VHL) and 8-oxo­ guanine DNA Glycosylase (OGG1) genes. The former has been described in thyroid malignancies [17] and the latter in head and neck cancer; thus both are suitable candidates for potential driver mutations responsible for increased biological aggressiveness. However our data also supports the role of other cancer genes including those situated at 17q, 1p, 10q and other genomic loci. By expanding future molecular analysis to search in more detail, we hope to address the presence, range and specific genomic changes regarding this important issue. A study limitation is the relatively small number of patients with known outcome (93 patients, mean follow-up 55 months). On Kaplan–Meier analyses, significance was seen only for the acquisition of TERT promoter mutation with BRAF V600E, as compared to BRAF V600E driver mutation alone. We were unable to achieve significance for DFS and LOH or ALN status. In contrast, we were able to demonstrate a strong association between ALN and decreased DFS (P=0.0001, HR 1.7, 95% CI 1.3, 2.2) by Kaplan–Meier analysis in a larger cohort of 347 patients with similar follow-up (mean 40.8 months) [18]. It is generally challenging to correlate biomarkers with adverse outcome for PTC pa­ tients. First local recurrence can develop decades after primary treat­ ment. This justifies framing our investigation by enriching the study cohort with a known surrogate for poor outcome, namely ALN status. Future validation studies will test the hypothesis that LOH detection in preoperative PTC specimensin addition to an expanded mutational panel that includes known important events such as BRAF V600E and TERT promoter mutations–can enhance the ability to predict disease recurrence. This novel association requires additional study in an increased patient cohort that is powered to query the impact of LOH detection on outcome for patients with primary PTC. In conclusion, the presence of LOH in primary PTC strongly predicts ALN status, a known surrogate for aggressive behavior. The accumula­ tion of additional LOH hits is common within regional metastases of patients with ALN status, while driver mutational status remains stable. 5 S. Finkelstein et al. Pathology - Research and Practice 251 (2023) 154842 Fig. 1. Kaplan–Meier Curves. Y axis: Probability of locoregional recurrence-free survival. X axis: Time in months. Left – ALN status, P=0.18. Right – BRAF V600E plus TERT promoter mutation versus BRAF V600E, P= 0.002. Bottom – LOH status, P= 0.09. Levine, Mark Urken and Margaret Brandwein-Weber; Software, Venkata Arun Timmaraju and Jonathan Levine; Supervision, Mark Urken and Margaret Brandwein-Weber; Validation, Sydney Finkelstein, Venkata Arun Timmaraju and Jonathan Levine; Writing – original draft, Sydney Finkelstein, Mark Urken and Margaret Brandwein-Weber; Writing – re­ view & editing, Shabnam Samankan, Camilo Gonzalez-Velazquez, Scott Doyle and Jonathan Levine. Molecular diagnostics designed to show the presence or absence of LOH mutational change could potentially predict ALN status and overall aggressive biology of thyroid cancer based on sampling and analysis of the primary malignancy. However, further work is necessary. Ethics approval The study was conducted according to the guidelines of the Decla­ ration of Helsinki and was approved by the Institutional Review Board of Mount Sinai (IRB STUDY-18–01236: Molecular markers predictive of aggressive and metastatic thyroid cancer). Last approval: 5/5/2023. Declaration of Competing Interest SDF, JL and VAT are employees of Interpace Diagnostics and own limited stock in the company. Consent to participate Data Availability Exempt from patient consent due to retrospective nature. Upon request. Consent for publication References All authors have reviewed the manuscript and approve the content. [1] M.J. Griffin, F.M. Baik, M. Brandwein-Weber, M. Qazi, L.E. Yue, M. Osorio, M. L. Urken, Positive lymph node counts in american thyroid association low-risk papillary thyroid carcinoma patients, World J. Surg. 44 (6) (2020) 1892–1897, https://doi.org/10.1007/s00268-020-05399-0. [2] B.R. Haugen, E.K. Alexander, K.C. Bible, G.M. Doherty, S.J. Mandel, Y.E. Nikiforov, F. Pacini, G.W. Randolph, A.M. Sawka, M. Schlumberger, K.G. Schuff, S.I. Sherman, J.A. Sosa, D.L. Steward, R.M. Tuttle, L. Wartofsky, 2015 American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association Guidelines Task Force on thyroid nodules and differentiated thyroid cancer, Thyroid 26 (1) (2016) 1–133, https://doi.org/10.1089/thy.2015.0020. PMID: 26462967; PMCID: PMC4739132. [3] S. Leboulleux, C. Rubino, E. Baudin, B. Caillou, D.M. Hartl, J.M. Bidart, J. P. Travagli, M. Schlumberger, Prognostic factors for persistent or recurrent disease of papillary thyroid carcinoma with neck lymph node metastases and/or tumor extension beyond the thyroid capsule at initial diagnosis, J. Clin. Endocrinol. Metab. 90 (10) (2005) 5723–5729, https://doi.org/10.1210/jc.2005-0285. [4] A. Singh, J. Ham, J.W. Po, N. Niles, T. Roberts, C.S. Lee, The genomic landscape of thyroid cancer tumourigenesis and implications for immunotherapy, Cells 10 (5) Funding This research received no funding. CRediT authorship contribution statement Conceptualization, Sydney Finkelstein, Scott Doyle, Jonathan Lev­ ine, Mark Urken and Margaret Brandwein-Weber; Data curation, Sydney Finkelstein and Margaret Brandwein-Weber; Formal analysis, Sydney Finkelstein and Margaret Brandwein-Weber; Investigation, Shabnam Samankan, Quinn O’Malley, Danielle Kapustin, Sarah Spaulding, Mon­ ica Xing, Ammar Matloob, John Beute, Gabriella Seo, Michael Saturno, Lily Greenberg and Lauren Wein; Methodology, Sydney Finkelstein, Venkata Arun Timmaraju and Jonathan Levine; Resources, Jonathan 6 S. Finkelstein et al. [5] [6] [7] [8] [9] [10] [11] Pathology - Research and Practice 251 (2023) 154842 [12] X. Lin, S.D. Finkelstein, B. Zhu, J.F. Silverman, Molecular analysis of multifocal papillary thyroid carcinoma, J. Mol. Endocrinol. 41 (4) (2008) 195–203, https:// doi.org/10.1677/JME-08-0063. Epub 2008 Jul 15. PMID: 18628356. [13] X. Lin, S.D. Finkelstein, J.F. Silverman, Loss of Heterozygosity (LOH) at 17p13 and 22q13 are shared by breast and thyroid carcinomas for metastasis, Appl. Immunohistochem. Mol. Morphol. 27 (2) (2019), https://doi.org/10.1097/ PAI.0000000000000630 e16-e19. [14] K.K. Ablordeppey, V.A. Timmaraju, J.W. Song-Yang, S. Yaqoob, C. Narick, A. Mireskandari, S.D. Finkelstein, G. Kumar, Development and analytical validation of an expanded mutation detection panel for next-generation sequencing of thyroid nodule aspirates, J. Mol. Diagn. 22 (3) (2020) 355–367, https://doi.org/ 10.1016/j.jmoldx.2019.11.003. Epub 2019 Dec 19. PMID: 31866571. [15] M. Xing, A.S. Alzahrani, K.A. Carson, D. Viola, R. Elisei, B. Bendlova, L. Yip, C. Mian, F. Vianello, R.M. Tuttle, E. Robenshtok, J.A. Fagin, E. Puxeddu, L. Fugazzola, A. Czarniecka, B. Jarzab, C.J. O’Neill, M.S. Sywak, A.K. Lam, G. Riesco-Eizaguirre, P. Santisteban, H. Nakayama, R.P. Tufano, S.I. Pai, M. A. Zeiger, W.H. Westra, D.P. Clark, R. Clifton-Bligh, D. Sidransky, P.W. Ladenson, V. Sykorova, Association between BRAF V600E mutation and mortality in patients with papillary thyroid cancer, JAMA 309 (14) (2013 10) 1493–1501, https://doi. org/10.1001/jama.2013.3190. PMID: 23571588; PMCID: PMC3791140. [16] B.A. McKelvey, C.B. Umbricht, M.A. Zeiger, Telomerase Reverse Transcriptase (TERT) regulation in thyroid cancer: a review, Front Endocrinol. 11 (2020) 485, https://doi.org/10.3389/fendo.2020.00485. PMID: 32849278; PMCID: PMC7412884. [17] L. Todorović, B. Stanojević, V. Mandušić, N. Petrović, V. Živaljević, I. Paunović, A. Diklić, V. Saenko, S. Yamashita, Expression of VHL tumor suppressor mRNA and miR-92a in papillary thyroid carcinoma and their correlation with clinical and pathological parameters, Med. Oncol. 35 (2) (2018) 17, https://doi.org/10.1007/ s12032-017-1066-3. [18] S. Samankan, L. Militello, G. Seo, S. Everest, Q. O’Malley, S.L. Spaulding, M. Xing, A. Matloob, J. Beute, R. Chai, S. Doyle, M.L. Urken, M. Brandwein-Weber, Tall cell variant papillary thyroid carcinoma impacts disease-free survival at the 10% cutpoint on multivariate analysis, Pathol. Res. Pr. 236 (2022), 154012, https://doi. org/10.1016/j.prp.2022.154012. Epub 2022 Jul 2. PMID: 35834884. (2021) 1082, https://doi.org/10.3390/cells10051082. PMID: 34062862; PMCID: PMC8147376. V. Costa, R. Esposito, P. Pallante, A. Ciccodicola, A. Fusco, The "next-generation" knowledge of papillary thyroid carcinoma, Cell Cycle 14 (13) (2015) 2018–2021, https://doi.org/10.1080/15384101.2015.1049786. PMID: 26030480; PMCID: PMC4614799. M.A. Lupo, A.E. Walts, J.W. Sistrunk, T.J. Giordano, P.M. Sadow, N. Massoll, R. Campbell, S.A. Jackson, N. Toney, C.M. Narick, G. Kumar, A. Mireskandari, S. D. Finkelstein, S. Bose, Multiplatform molecular test performance in indeterminate thyroid nodules, Diagn. Cytopathol. 48 (12) (2020) 1254–1264, https://doi.org/ 10.1002/dc.24564. Epub 2020 Aug 7. PMID: 32767735; PMCID: PMC7754490. S. Jackson, G. Kumar, A.B. Banizs, N. Toney, J.F. Silverman, C.M. Narick, S. D. Finkelstein, Incremental utility of expanded mutation panel when used in combination with microRNA classification in indeterminate thyroid nodules, Diagn. Cytopathol. 48 (1) (2020) 43–52, https://doi.org/10.1002/dc.24328. Epub 2019 Nov 1. PMID: 31675178; PMCID: PMC6972518. N. Kumar, R. Gupta, S. Gupta, Molecular testing in diagnosis of indeterminate thyroid cytology: Trends and drivers, Diagn. Cytopathol. 48 (11) (2020) 1144–1151, https://doi.org/10.1002/dc.24522. Epub 2020 Jun 5. PMID: 32501611. J.L. Hunt, M. Fowler, D. Lomago, L. Niehouse, E. Sasatomi, P. Swalsky, S. Finkelstein, Tumor suppressor gene allelic loss profiles of the variants of papillary thyroid carcinoma, Diagn. Mol. Pathol. 13 (1) (2004) 41–46, https://doi. org/10.1097/00019606-200403000-00007. M. Migdalska-Sęk, K.H. Czarnecka, M. Kusiński, D. Pastuszak-Lewandoska, E. Nawrot, K. Kuzdak, E. Brzeziańska-Lasota, Clinicopathological significance of Overall Frequency of Allelic Loss (OFAL) in lesions derived from thyroid follicular cell, Mol. Diagn. Ther. 23 (3) (2019) 369–382, https://doi.org/10.1007/s40291019-00387-0. PMID: 30747408; PMCID: PMC6548761. G. Kumar, V.A. Timmaraju, J.W. Song-Yang, B. Repko, C. Narick, A. Mireskandari, S. Finkelstein, Utility of microdissected cytology smears for molecular analysis of thyroid malignancy, Diagn. Cytopathol. 47 (4) (2019) 289–296, https://doi.org/ 10.1002/dc.24100. Epub 2018 Dec 8. PMID: 30548138; PMCID: PMC6587978. 7