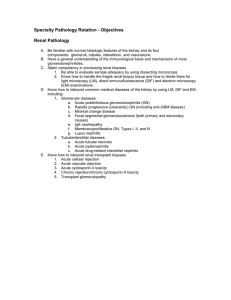
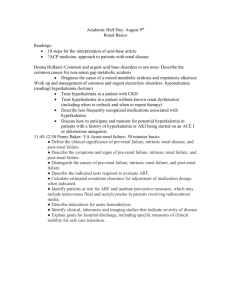
Acute Kidney Injury Workshop: Definition, Staging, and Treatment
advertisement

Acute Kidney Injury Workshop Joel M. Topf, MD FACP Nephrology @Kidney_Boy • Joel.Topf@gmail.com Acute Renal Failure Joel M. Topf, MD Introduction Acute renal failure is “The House Moment” of nephrology. The patients go from normal functioning kidneys to zero function and at that point they either recover with no significant sequelae or they die. At that branch point, between total recovery and death, is the nephrologist and she is selecting IV fluids, deploying dialysis, and determining the balance of atoms in order to nudge the patient toward recovery. Goals • Definition and staging of AKI • Intra-renal AKI • Etiologies of inpatient versus outpatient acute renal failure. • Understanding the Urinalysis • Pre-renal azotemia • Acute interstitial nephritis • BUN:Cr ratio • Ischemic versus toxic ATN • Hyperkalemia • FENa • EKG Changes • FEUrea • Treatment • Post-renal !2 Acute Renal Failure Joel M. Topf, MD Table of Contents History of acute kidney injury therapy .....................4 Definition of AKI ...........................................................4 Use KDIGO to stage the following cases of AKI ......6 Differential Diagnosis ..................................................7 Pre-renal azotemia ........................................................8 Diagnosing Pre-Renal ...................................................8 Questions on Pre-renal Azotemia ...............................11 Post-renal insufficiency ................................................13 Treating Post Renal AKI ...............................................14 Questions on Post-Renal AKI ......................................15 Intrarenal acute renal failure .......................................16 Diagnosis ........................................................................16 Clinical Syndromes .......................................................17 Questions on the Urinalysis ........................................18 Ischemic acute tubular necrosis .................................19 Toxic acute renal failure ...............................................19 Contrast Nephropathy .................................................20 Acute Interstitial Nephritis ..........................................21 Hyperkalemia ................................................................23 EKG Changes with hyperkalemia ..............................24 Treating hyperkalemia..................................................24 Question on hyperkalemia ..........................................25 !3 Acute Renal Failure Joel M. Topf, MD History of acute kidney C. 15 injury therapy In 1945, a 67-year-old woman in uremic coma presented to Dr Kolff. He initiated dialysis and she regained consciousness after 11 hours of therapy. This was his 17th patient after 16 consecutive treatment failures. She lived another 8 years and ultimately died of community acquired pneumonia. D. >20 Definition of AKI The study of AKI has been hampered by a proliferation of definitions for AKI. ! Dr. Haas in his laboratory with the first human dialysis machine in 1928. Extracorporeal dialysis for humans was first tested in the 1920’s by Dr. Haas. He treated 6 patients, all of whom died. In 1943, Willem Kolff, working in Nazi-occupied Holland, created the second human dialysis machine; and in 1943 he dialyzed his first patient. This young man with acute nephritis died during the therapy. Question: If you invented a novel and unproven technology for the treatment of a usually, but not universally, fatal condition, how many consecutive failures (patient dies during therapy) would you let occur before you considered the technique a failure? The classic text-book definition of acute renal failure is “ An acute and sustained decrease in renal function.” Unfortunately this accepted definition is hampered by ambiguity: How acute? How sustained? How should renal function be measured? Is the degree of renal impairment important? As clinical scientists studied AKI they needed specific case-definitions of AKI and each researcher created their own. At last count there were over 35 separate definitions of AKI. This created chaos where one study couldn’t be compared to another and has hampered progress in the field of AKI. KDIGO, the international nephrology guideline organization has established a consensus definition and staging system (1, 2, 3) for AKI. The KDIGO system replaces two other similar systems, the RIFLE criteria and AKIN system. A. 5 B. 10 !4 Acute Renal Failure Joel M. Topf, MD KDIGO Change in Cr Oliguria Definition ≥ 0.3 mg/dl within 48 h or ≥ 1.5 times baseline, within seven days urine volume < 0.5 mL/kg / hr for 6 hours 1 1.5-1.9 times baseline or increase ≥ 0.3 mg/dL < 0.5 mL/kg/hr for 6-12 hours 2 2.0-2.9 times baseline < 0.5 mL/kg/hr for more than 12 hours 3 3.0 times baseline or Cr > 4 mg/dL or initiation of renal replacement therapy < 0.3 mL/kg/hr ≥ 24 hrs or anuria for > 12 hrs The KDIGO system has been validated: Validation means that as the AKI stage goes up the patient is sicker. This study shows an increase in both hospital mortality and length of stay with increasing AKI stage. Fujii T, Uchino S, Takinami M, Bellomo R. Validation of the Kidney Disease Improving Global Outcomes criteria for AKI and comparison of three criteria in hospitalized patients. Clin J Am Soc Nephrol. 2014;9(5):848-54. !5 Acute Renal Failure Joel M. Topf, MD Use KDIGO to stage the following cases of AKI A 32 year old African American hair model with a baseline creatinine of 1.4 receives a contrasted CT scan to determine the source of bleeding following a hysterectomy. Her creatinine 2 days later is 2.2. Her urine output over the last 8 hours is 640 mL. A 28 year old Asian bank employee is in a motor vehicle accident. He goes for emergency splenectomy and repair of a liver laceration. Despite aggressive use of blood products and crystalloids he has been anuric since a foley was placed 14 hours ago. A 62 year old white female who models for a national nursing home chain has a PMHx of arthritis and hypertension. She presents to her primary care doctor with symptoms of fatigue since starting ramipril for her blood pressure. Her medications include ibuprofen 800 mg three times a day, chlorthalidone 25 mg once a day, simvastatin 40 mg once a day and ramipril 10 mg once a day. Her labs show a creatinine of 3.2 (baseline 1.2) and a potassium of 6.6. She states she urinated a “normal amount” prior to coming to the office. A 55 year old Hispanic comedian is admitted for decompensated heart failure. His baseline creatinine is 1.4. On admission his creatinine is 2.2. He is given furosemide and responds well. His oxygen requirement decreases, most of his edema improves but his creatinine has gone up to 3.2. His urine output in the last 8 hours is 460 mL. A 82 year old nursing home resident with known diabetic nephropathy complains of an inability to walk. On exam he has an S3 gallop, rales in his lungs and pitting edema in both legs and back. Labs show a creatinine of 4.8, a potassium of 7.4 and a bicarbonate of 14. His baseline creatinine is 3.4. No urine output has been recorded and the patient is unable to estimate his recent urine output. !6 Acute Renal Failure Joel M. Topf, MD Differential Diagnosis Acute renal failure can be divided into three broad etiologies: Pre-renal azotemia, intrinsic renal failure and post-renal azotemia (obstructive uropathy). Using these categories one is able to quickly narrow the differential diagnosis of acute renal failure and determine the likely natural history of the condition. Pre- and post- renal AKI usually are quickly reversible and easy to treat. They are often obvious from the history. When the etiology of AKI is not obvious it is helpful to be aware of the incidence of the etiologies in various clinical settings. Multiple studies have shown that patients with AKI upon presentation to the hospital have different causes of AKI than patients who develop AKI while in the hospital. Another clue to the etiology can be the age of the patient. Pascual, et al. showed that as patients age post-renal etiologies and pre-renal etiologies of AKI become more common at the expense of decreasing intrarenal causes. Question: Why might the elderly have more pre-renal azotemia? Why do they have more post-renal failure? 100% 80% 17% 12% 11% 7% 56% 11% 20% 48% 39% 60% 40% 20% 29% 30% 65-79 >79 20% 0% <65 Prerenal Postrenal Inpatient/Hospital acquired AKI Intrarenal Unknown Outpatient acquired AKI 4% 38% 58% 17% 11% 72% Prerenal Intrarenal Postrenal !7 Acute Renal Failure Joel M. Topf, MD Pre-renal azotemia No BP; No pee pee. Volume depletion from any etiology decreases renal perfusion. If the body is unable to compensate this will decrease GFR. Heart failure and cirrhotic patients are both edematous. These patients have total body sodium excess but the amount of fluid in the arterial blood compartment, the “effective circulating volume” is decreased. This results in pre-renal azotemia. As perfusion falls the kidney compensates in an attempt to maintain a stable GFR. There are two primary strategies to maintain GFR: 1. The first is vasodilation of the afferent arteriole. Local prostaglandin production triggers this response. 2. The second strategy is efferent vasoconstriction via the action of angiotensin II. This increases intraglomerular pressure, forcing more RPF down the glomerular drain. Both of these strategies increase intraglomerular pressure to maintain GFR. If these strategies are successful, the GFR remains constant, the creatinine doesn’t rise and the patient is not pre-renal. They are prepre-renal. Question: What drugs antagonize the kidney’s ability for afferent vasodilation? For efferent Vasoconstriction? Diagnosing Pre-Renal There are three tests you need to be facile with to separate pre-renal azotemia from intrinsic AKI: 1. BUN:Cr ratio 2. Fractional excretion of sodium 3. Fractional excretion of urea. In volume depletion the kidneys become sodium avid and retain BUN out of proportion to creatinine. This allows physicians to make quantitative assessments of volume depletion and make an accurate diagnosis. BUN:Cr ratio A BUN to Cr ratio over twenty is a reasonably accurate indicator of volume depletion. This actually is an indication of the filtration fraction at the glomerulus. AT2 PGE Filtration fraction = GFR RPF The increased filtration fraction means that the plasma proteins that are not filtered by the glomerulus are diluted in less plasma (because more of that plasma went down the glomerular drain). This higher concentration of plasma proteins exert greater osmotic attraction in the proximal tubules bringing back more plasma water, sodium and urea. Creatinine is actively secreted in the proxi!8 Acute Renal Failure Joel M. Topf, MD mal tubule and is not affected by this osmotic movement of water. The net result is normal creatinine clearance and decreased urea clearance resulting in a rise in BUN out of proportion to the rise in creatinine. The calculation is easy to remember, doesn’t require a calculator and is surprisingly accurate; however the test has some important pitfalls. One can get a falsely elevated BUN:Cr ratio with a GI bleed or in catabolic patients due to steroids or sepsis. High protein tube feeds and recovery of ATN can also lead to false positive elevations in the BUN:Cr ratio. In some patients with pre-renal azotemia the BUN:Cr is falsely low due to either liver failure or malnutrition. This often is seen in alcoholics. Fractional Excretion of sodium (FENa) The fractional excretion of sodium is the excreted sodium divided by the amount of sodium filtered at the glomerulus. ! FENa ! In pre-renal azotemia less than 1% of the sodium is excreted. In intrinsic renal failure more than 1% of sodium is excreted. Calculating the FENa requires the simultaneous measurement of serum sodium and creatinine and the urine sodium and creatinine. FENa = Urine Na x Sr Cr Sr Na x Urine Cr X 100 FENa false negatives (High FENa in Pre-renal azotemia) The FENa is most accurate for patients who are oliguric. The equation is inaccurate in !9 Acute Renal Failure Joel M. Topf, MD patients who have recently received diuretics. FENa false positives (Low FENa in ATN) A low FENa can be found in conditions besides pre-renal azotemia. It also occurs with: • Contrast nephropathy • Rhabdomyolysis • Acute GN • Hepatorenal syndrome • ATN with CHF • ATN with cirrhosis • ATN with severe burns Remembering the FENa Equation The FENa is a small number (especially before you multiply it by 100. To remember the formula put all of the small numbers on the top and the big numbers on the bottom. FENa = small x small big x big Big or small? 1. Urine sodium big small 2. Urine creatinine big small 3. Serum sodium big small 4. Serum creatinine big small The Fractional Excretion of Urea The biggest weakness of the FENa is that it fails in the face of diuretics. Patients who are prone to pre-renal azotemia are often patients on diuretics. Think of CHF patients, or oliguric patients in the hospital. So in the very patients you would want to use the FENa it becomes inaccurate. Enter the FE Urea to solve this. The equation for the FE Urea is identical to the FENa except in everyplace there is a sodium you replace it with urea. Instead of 1% as the line between pre-renal and intrinsic renal failure use 35%. A FE Urea less than 35% indicates pre-renal azotemia, a FE Urea greater than 35% is indicative of intrinsic renal failure. FE Urea = Urine Urea x Sr Cr Sr Urea x Urine Cr X 100 Though the FE Urea was developed for use in patients with previous exposure to diuretics it is just as accurate as the FENa in patients without diuretic exposure. ! !10 Acute Renal Failure Joel M. Topf, MD Questions on Pre-renal Azotemia Calculate the BUN:Cr ratio, FENa and FEUrea for the following patients and then interpret each test as indicating a true positive, false positive, true negative, false negative. 58 year old white male admitted with an exacerbation of CHF. He is treated with IV diuretics and on the third hospital day the following labs are obtained: Serum ! Urine 136 111 88 3.4 3.4 19 Characteristic 55 123 59 ! Value Interpretation BUN:Cr FENa FEUrea An 82 year old nursing home resident presents to the ER with obvious dehydration. The patient has a blood pressure 80/50, is oliguric and has cloudy, foul smelling urine in a Foley bag. The following labs are collected: Serum ! Urine 136 111 93 3.4 5.4 19 Characteristic 10 ! Value 123 53 Interpretation BUN:Cr FENa FEUrea !11 Acute Renal Failure Joel M. Topf, MD A 44 year old alcoholic presents to the ED with hemetemesis. On initial labs the patient has a hemoglobin of 5 g/dL. The patient goes for emergency EGD and the bleeding is stopped. The next morning the patient has the following labs: Serum ! Urine 136 111 98 3.4 3.8 19 Characteristic 62 229 22 ! Value Interpretation BUN:Cr FENa FEUrea An elderly gentleman is shot multiple times. While planning the surgical approach the surgeons order a contrasted CT scan. One day later the patient’s creatinine begins to rise. The patient remains non-oliguric. The following labs are obtained: Serum ! Urine 136 111 64 3.4 3.4 Characteristic 19 Value ! 12 N/A 67 Interpretation BUN:Cr FENa FEUrea N/A !12 Acute Renal Failure Joel M. Topf, MD Post-renal insufficiency When the plumbing is clogged the kidneys fail. Post-renal AKI is immediately intuitive. When the urinary tract is blocked renal function falls. One of the most important aspects to understand is how unilateral obstruction placed after the patient attempts to urinate and the post-void residual is recorded. Post-Void Residual < 50 mL................normal Urinary obstruction review of systems: Do you have nocturia? Has it changed? Has the strength of your stream decreased? Do you have double voiding? Urinary frequency? Hesitancy? Do you need to strain (valsalva) to urinate? 100 mL .................Normal over 65 > 200 mL ..............very abnormal Ultrasound is the “gold-standard” for the diagnosis of obstructive uropathy. Ultrasound is quick, non-invasive and painless. It is also highly sensitive and specific for the correct diagnosis. Unfortunately there Do you have urinary incontinence or dribbling? works. In patients with two functioning kidneys, blocking a single kidney will not cause renal failure. Renal failure requires either bilateral obstruction or unilateral obstruction in a patient with a single functioning kidney. The most common cause of bilateral obstruction in males is prostatic hypertrophy. In women it is cervical cancer. When people think of obstruction it is easy to solely think of physical obstruction but a neurogenic bladder from neurologic disease (MS) metabolic derangements (diabetic neuropathy) or drugs can be occult sources of obstruction. Urine output is usually, but not always, decreased in obstructive uropathy. In some patients the primary symptom of obstruction is nocturia. Anuria is highly suggestive of bilateral obstruction. The diagnosis can almost always be made with a combination of a renal ultrasound and Foley’s Catheter. Make sure the Foley is a few situations where the ultrasound can give a false negative result (i.e. a normal renal ultrasound in the presence of clinically significant obstruction): 1. Concurrent volume depletion and obstructed may not show hydronephrosis on the ultrasound until after fluid resuscitation. !13 Acute Renal Failure 2. Patients early in the course of obstruction may not have developed hydronephrosis yet. 3. Large retroperitoneal tumors can encase the kidney and both cause the obstruction and prevent hydronephrosis. Joel M. Topf, MD Treating Post Renal AKI Treatment of post-renal acute renal failure is usually simple once the diagnosis has been made. Patients with neurogenic bladder will have brisk recovery after a Foley is placed. 4. Retroperitoneal fibrosis (idiopathic or post-radiation therapy) can prevent hydronephrosis. Also be careful of false positives. A dilated collecting system is a normal finding in pregnancy. Bladder scans can falsely report high residual bladder volume in patients with abdominal ascites. One last finding which can suggest obstructive uropathy is: hyperkalemia out of proportion to the degree of renal failure. Often patients with obstructive uropathy will have severe hyperkalemia with mild to modest renal failure. Physical Obstruction • Phimosis • Stricture • Prostatitis • Trauma • Blood clot • Stone • BPH • Prostate / bladder cancer • Cervical cancer • Colon cancer • Sarcoidosis • Tuberculosis • Pregnant Uterus Involve urology for more complex mechanical obstruction. Interventional radiology may be helpful by placing percutaneous nephrostomy tubes in patients with recalcitrant obstruction. Neurogenic Bladder • Diabetes mellitus • Spinal cord disease • Multiple Sclerosis • Parkinsons disease • Anticholinergic drugs • diphenhydramine • Alpha-adrenergic agonists • ephedrine • pseudoephedrine • Calcium channel blockers • Opiates • Sedative hypnotics !14 Acute Renal Failure Joel M. Topf, MD Questions on Post-Renal AKI A 58 year old white female is admitted on a Friday evening from her Gyn’s office with a diagnosis of vaginal bleeding. Initial labs show: Serum 136 111 44 7.8 2.8 16 What is the likely diagnosis? What problems need to be addressed immediately? A 78 year old white male with a history of mild prostatism has been self treating for a “sinusitis” for the last few days with over the counter medications. He finally relents and comes to the doctor for “some antibiotics.” The PCP orders routine labs and sends him home. The patient receives a call that evening telling him to go straight to the ED. The initial labs are to the right: What’s going on? Serum 143 111 68 5.4 4.9 17 A 32 year old returns to the ED because the pain from his previously diagnosed kidney stone has gotten much worse and he has developed nausea and vomiting. A CT scan from earlier in the week revealed a 3 mm stone in the distal ureter and a 12 mm stone in the left renal pelvis. Before you arrive the ER gets a stat U/S which shows hydronephrosis on the left. ! Serum Urine 136 111 52 4.8 3.6 22 ! 31 156 29 !15 Acute Renal Failure Joel M. Topf, MD Intrarenal acute renal failure Intrinsic acute renal failure comes in a number of flavors but this guide will only examine diagnosis and three specific etiologies: ischemic ATN, contrast nephropathy and interstitial nephritis. Intrinsic acute renal failure is the most comThe concentrated urine is seen in pre-renal mon cause of acute renal failure among hosconditions. False positives are found in papitalized patients. Unlike pre- and post- retients with ATN in the background of CHF nal failure there is typically no direct and and cirrhosis and with pigmented nephropaeasy therapy. The role of the physician is relthy or acutely following contrast administraegated to supportive care as she waits for the tion. kidneys to recover on their own. However The isothenic urine is seen with non-oliguric the condition is quite severe with a high ATN (including recovery of ATN) and adhospital mortality. Among all hospitalized vanced CKD, including dialysis patients. patients it is usually around 30%. For septic Damaged tubules are unable to concentrate patients in the ICU it can be as high as 70% or dilute the urine. The tubules are on strike. hospital mortality. Protein: Proteinuria is characteristic of just Even survivors are not entirely off the hook. about any glomerular damage, from diabetes The development of AKI is a large risk facto lupus nephritis. The finding of proteinuria tor, and even may cause chronic kidney disis difficult to interpret because it is impossiease (CKD). Patients who survive AKI need ble to differentiate if it is pre-existing disease regular follow-up and screening for CKD. or associated with the AKI. The absence of proteinuria effectively rules out glomerulonephritis. Diagnosis The art of the Urinalysis The cheapest objective test available is the urinalysis. It is a liquid biopsy of the kidney and can be quite informative. Don’t forget to order the U/A! Don’t be the tool who orders a FENa, FEUrea, renal ultrasound, but forgets the U/A. The urinalysis is a two part analysis: a biochemical profile followed by a microscopic exam. Biochemical assessment Specific gravity: look for two extremes: the concentrated urine with specific gravity greater than 1.020 and the dilute isothenic urine (1.010). Hematuria is assessed in both components of the urinalysis. In the biochemical assessment, the assay measures heme and interprets this as blood. This will have false positives from myoglobulinuria from rhabdomyolysis or from hemoglobinuria associated with hemolysis. The biochemical assessment does not differentiate glomerular blood from lower tract blood. Glomerular blood and AKI are associated with acute GN, interstitial nephritis. Positive heme without RBC on microscopy indicates rhabdomyolysis or hemolysis. Microscopic analysis The microscopic analysis can identify a few enormously helpful findings: !16 Acute Renal Failure Dirty brown casts are pathognomonic for ATN. It is composed of dead tubular epithelial cells. Joel M. Topf, MD Hyaline casts are a normal finding. They are prominent in acidic urine as found with: loop diuretics and concentrated urine (first morning urine). Also found following vigorous exercise. Red cell casts are pathognomonic for glomerulonephritis and usually trigger a kidney biopsy. Red blood cells. Found with glomerular disease, tubular disease, foley specimens, cystitis. Nonspecific finding that, like proteinuria, is more valuable when it is negative to rule out most types of kidney injury. Oval fat bodies: indicative of lipiduria found with nephrotic syndrome. Broad waxy casts are indicative of chronic kidney disease. Bacteria useful in the diagnosis of cystitis and pyelonephritis. WBC casts: found with pyelonephritis and acute interstitial nephritis. Clinical Syndromes There are two non-specific syndromes which are used to classify glomerular disease. These can usually be identified by the history and physical and the U/A. Nephrotic syndrome: A non inflammatory glomerular injury with massive proteinuria !17 Acute Renal Failure Joel M. Topf, MD (proteinuria > 10x the upper limit of normal). Patients are edematous but typically have normal blood pressure. Rarely associated with AKI. proteinuria (though not as much as with nephrotic syndrome) RBC casts (variable). Clinically the patients have renal failure and hypertension. This is an important cause of AKI. Nephritic syndrome: An inflammatory glomerular injury. Patients have hematuria, Questions on the Urinalysis Match the U/A to the patient to the diagnosis U/A 1 U/A 2 U/A 3 U/A 4 U/A 5 U/A 6 1.020 1.010 1.014 1.010 1.012 1.040 Protein neg 2+ 3+ 4+ 1+ neg Heme neg neg 3+ 1+ 2+ neg Micro hyaline casts waxy casts RBC Casts SpGrav oval fat bodies WBC casts nothing Patient Dx Patients A. 26 y.o. AA female with rash, joint pain, anemia and a Cr of 3.4. B. 64 y.o. white male who had a cardiac cath 6 hours ago. C. 40 y.o. white female with a diabetic foot ulcer. She is on cefazolin for osteomyelitis She develops a fever, rash and AKI. D. 38 y.o. with alcoholic cardiomyopathy. Patient is admitted for CHF. He develops hospital acquired AKI on hospital day 3. E. 37 y.o. black female with AIDS. She is poorly compliant with her HAART regimen and presents with lower extremity edema. !18 Acute Renal Failure Joel M. Topf, MD F. 62 y.o. white male with a 20 year history of diabetes, a Cr of 2.8 mg/dl and a 15 year history of proteinuria. Diagnosis 1. Collapsing focal segmental glomerulosclerosis (FSGS) 2. Contrast exposure 3. Pre-renal azotemia 4. Acute interstitial nephritis 5. Lupus nephritis 6. Chronic kidney disease Ischemic acute tubular necrosis Disruptions in blood supply to the kidney cause acute renal failure. The kidneys normally receive a rich blood Any insult that causes a de- crease in blood supply. In fact 20% of cardiac output, 1 liter pressure can cause ATN. Bleeding, sepsis, per minute, is devoted to perfusing the kidsevere volume depletion, ACEi and NSAIDs neys. Despite this abundance of perfusion, all can cause ATN. ATN will cause oliguria almost all of this blood goes solely to the rein about 70% of cases. The remainder will be nal cortex leaving the deep medullary tissue non-oliguric. Patients will remain in renal relatively devoid of oxygen. Much of the failure usually for 4-14 days, though longer medulla lives in continuous ischemia at the courses may occur. Loop diuretics can be very margin of viability. Brief interruptions used to increase urine output but they fail to of perfusion can push these marginal tissues shorten the duration of dialysis. Patients (the cells that line the renal tubules) into who do not have a good response to IV dioxygen debt and cause them to die and uretics have a much worse prognosis than slough into the urine. Once perfusion rethose with a good diuretic response. sumes the tissue regenerates and the kidney function is restored. Toxic acute renal failure A number of nephrotoxins can cause acute renal failure The very high renal blood flow means that • Acute interstitial nephritis the kidney is exposed to many toxins. These • crystallization in the renal tubules can disrupt normal renal function and cause • antagonize proximal tubule creatinine acute renal failure. secretion. Vancomycin and the aminoglycosides are Nephrotoxins often work in concert with famously nephrotoxic. Some agents like other renal insults such as dehydration to trimethoprim sulfamethoxazole can cause multiple types of renal failure: !19 Acute Renal Failure Joel M. Topf, MD increase toxicity. One of the most worrisome nephrotoxins is iodinated contrast. Contrast Nephropathy You were just trying to make a diagnosis and you boxed the kidneys. Iodinated contrast agents are responsible for • Avoid using contrast when imaging the 12-14% of hospital acquired acute renal failpatient. Make sure the contrast is absoure. Patients with pre-existing chronic kidlutely needed. Assessing an aortic ney disease and diabetes are at the highest aneurism? No need for contrast. Looking risk for this complication. for a retroperitoneal hematoma? No need for contrast. Kidney stone? No contrast. Contrast nephropathy is usually defined as a Oral contrast is safe. Angiograms can 0.5 mg/dL or 25% increase in serum creatisometimes be done with CO2 rather than nine within 48 hours of administration of iodinated contrast agents. contrast. The creatinine usually starts rising immediately after contrast is given and peaks on day 4. Typically, the creatinine remains above baseline 10 days after contrast administration. The acute renal failure is typically non-oliguric and has a low FENa. People with contrast nephropathy have poor prognosis. The rise in hospital mortality occurs even when patients do not require dialysis. In patients with the need for dialysis the condition becomes truly devastating. Mortality 62% 34% 31% • Use isoosmolar or low osmolar contrast agents. Some contrasts are more nephrotoxic than others. These two are the safest. • Minimize the dose of contrast. If the patient is going for a left heart catheterization, get the echo first so there is no need for a ventriculogram to asses cardiac function • Make sure the patient is not volume depleted. IV saline is the most effective weapon to reduce contrast nephropathy. 0.9 NS is more effective than 0.45 NS. To maximize the benefit give as much hydration as the patient can tolerate. • Stop drugs associated with increased risk of contrast nephropathy: 7% CN, +HD CN CN, no HD ! No CN • Diuretics There are some precautions one can take to reduce the risk of contrast nephropathy: • Mannitol • ACEi/ARB • NSAIDs. • N-acetyl cysteine and sodium bicarbonate are no better than placebo and normal saline respectively. !20 Acute Renal Failure Joel M. Topf, MD Acute Interstitial Nephritis A drug induced allergic reaction that takes the kidneys down. In most cases, the cause of acute renal failure is obvious: • The patient received contrast • Patient develops hypotension • The patient passes a liter and a half of urine after someone thinks to place a Foley • Creatinine falls after a night of IV fluids Then there are the exceptions, the patients whose renal function declines day after day with no obvious source of renal failure. They don’t respond to IV fluids. The patient Most common drugs associated with AIN • NSAIDs • Selective COX-2 inhibitors • Penicillins • Cephalosporins • Rifampin • Sulfonamides (Bactrim) • Furosemide, bumetanide • Thiazide-type diuretics • Ciprofloxacin and other quinolones • Cimetidine • Allopurinol • Omeprazole and lansoprazole • Indinavir • Mesalamine !21 Acute Renal Failure doesn’t have a history of contrast exposure, no gentamicin on the MAR. These are the cases where a cagey nephrologist is needed. The differential diagnosis of occult AKI is long and complex and beyond the scope of this workshop. One etiology I would like to highlight is acute interstitial nephritis (AIN). AIN is an allergic reaction, typically to a drug which results in acute renal failure. Patients need prolonged exposure to the drug to develop their first case of AIN but the renal failure can recur within days on subsequent exposures to the drug. Joel M. Topf, MD The classic presentation is renal failure in the presence of hematuria, pyuria, fever and rash. The patients are almost always nonoliguric and serum potassium tends to be low rather than high. The classic drug-class responsible for AIN is ß-lactam antibiotics but the list of drugs associated with AIN is long and varied (see box). Therapy focuses on stopping the offending drug. Some retrospective data suggests that high dose steroids are beneficial. The steroids should be used early to be most effective. (Gonzalez E, Et al. Kidney International (2008) 73, 940–946) !22 Acute Renal Failure Joel M. Topf, MD Hyperkalemia One of the most concerning causes of morbidity with AKI is hyperkalemia. Hyperkalemia is a particular problem with obstructive uropathy, tumor lysis syndrome and rhabdomyolysis. Hyperkalemia can occur from three primary sources: 1. Increased intake. This can be either enteral through potassium supplements and diet or enteral as found in potassium infusions, blood transfusions and TPN. 2. Movement of potassium from inside cells to the outside of cells. The concentration of potassium inside cells is about 140 mEq/L so tissue death releases a tremendous amount of potassium. This occurs in tumor lysis syndrome, crush injuries, and rhabdomyolysis. 3. Inability of the kidneys to excrete potassium. This could be due to generalized renal failure or a specific inability to excrete potassium. The later occurs with medications, diabetes, or obstructive uropathy. In general the first two causes result in transient hyperkalemia, as healthy kidneys are able to up-regulate clearance of potassium and excrete almost any dietary or endogenous load. Persistent, clinically significant hyperkalemia always has at least a component of excretion failure. Drug induced hyperkalemia • ACEi • ARB • Aldosterone antagonists • Digoxin • Beta-blockers • Heparin • Triamterene • Amiloride • Trimethoprim • Potassium supplements • Ringer’s solution • Penicillin G • Amicar • Succinylcholine • NSAID • Pentamidine • Cyclosporine • Tarolimus !23 Acute Renal Failure Joel M. Topf, MD EKG Changes with hyperkalemia Normal EKG Initial finding is peaked T waves Widening of the QRS complex and shortened ST interval A sinusoidal EKG Treating hyperkalemia. Treatment of hyperkalemia follows the same conceptual framework as the differential diagnosis: intake, distribution and excretion. The treatment of hyperkalemia needs to be fastidious and follow-up is critical. Patients with potassiums greater than 6 mmol/L should have an EKG to look for typical EKG changes. Patients with these changes should be given calcium to stabilize the cardiac membranes. Hyperkalemia orders • Stop all sources of potassium • Stat EKG • Consider transfer to telemetry • Calcium gluconate 1g IVPB or IVP • Calcium chloride 1g IVPB or IVP in patients with central access • Insulin 10 units IVP (note not subQ) followed by 1 amp of D50 IVP follow serial blood glucose to avoid hypo- and hyperglycemia • Calcium chloride if the patient have central access • Calcium gluconate if they only have peripheral access This can be repeated every 5 minutes in order to correct EKG changes. Calcium should • Albuterol 10-20 mg by nebulizer • Sodium polystyrene 15-30g po • avoid if sick GI tract • Furosemide IV and saline. Use twenty times the serum creatinine as the dose in mg (max. 80 mg) • Call or consult nephrology • Assess and correct any causes of hyperkalemia !24 Acute Renal Failure Joel M. Topf, MD be used with caution in cases of digoxin toxicity. 0.0 0 Intake 15 30 45 60 To start lowering the potassium stop any source of additional potassium. Review all of the medications and make sure all IVs are potassium free. Stop TPN. Change in K -0.3 -0.6 -0.9 Transcellular shift This is the mainstay of acute management of hyperkalemia. Beta-agonists (albuterol) and insulin are the primary drugs which shift potassium into cells. These drugs stimulate the Na-K-ATPase and can lower the potassium by about 1 mEq/L in about in an hour. Sodium bicarbonate is sometimes used to lower the potassium. Multiple studies have shown that this is ineffective and there are theoretical concerns that it maybe harmful. A banana has about one mEq of potassium per inch. -1.2 -1.5 Time (min) Insulin Albuterol Combination Excretion from the body Final correction of hyperkalemia requires getting rid of excess potassium either through the GI tract or via the kidneys. In patients with functioning kidneys, a dose or two of furosemide along with a generous dollop of saline is usually enough to correct the hyperkalemia. In patients with severe chronic kidney disease or on dialysis use of a cation exchange resin like Kayexylate is required to use the GI tract to excrete excess potassium. If hyperkalemia occurs in a dialysis patient the nephrologist needs to be notified so a prompt decision regarding dialysis can be made. Question on hyperkalemia A 71 year old Asian man presents with acute renal failure due to dehydration. Initial labs show a potassium of 6.7. The EKG shows a QRS complex of 123 msec. A Previous EKG showed a QRS of 110 msec. !25 Acute Renal Failure How would you handle Joel M. Topf, MD this situation? Answers KDIGO 1 KDIGO stage 3 Obstruction due to cervical Ca, Address hyperkalemia Obstruction due to OTC cold medicine on top of BPH KDIGO stage 2 KDIGO stage 2 KDIGO stage 3 Question: Elderly with more pre-renal azotemia? Increased CKD decreases the ability to concentrate urine predisposing to fluid loss. Co-morbidities require diuretics Why do they have more post-renal failure? Increased BPH, increased risk of Cx Ca. BUN:Cr 14.4, FENa 2.8%, FEUrea 37%, ATN due to NSAIDS, obstruction is not the cause b/c it is unilateral. Questions on urinalysis U/A 1: patient D, diagnosis 3 U/A 2: patient F, diagnosis 6 U/A 3: Patient A, diagnosis 5 U/A 4: Patient E, diagnosis 1 U/A 5: Patient C, diagnosis 4 U/A 6: Patient B, diagnosis 2 Question: What drugs antagonize afferent vasodilation? NSAIDS Efferent Vasoconstriction? ACEi & ARB Remember the FENa Eq. small, big, big, small BUN:Cr 25.9, FENa 2.2%, FEUrea 8%, use of diuretics causes the false (–) FENa BUN:Cr 17.2, FENa 0.7%, FEUrea 13%, malnutrition causes false (–) BUN:Cr BUN:Cr 25.8, FENa 7.9%, FEUrea 40%, GI bleed causes false (+) BUN:Cr BUN:Cr 18.8, FENa 0.4%, false (+) FENa due to contrast !26