Abstract on Disasters, Climate Change, and the the growing Population of Older Adults with Demnentia
advertisement

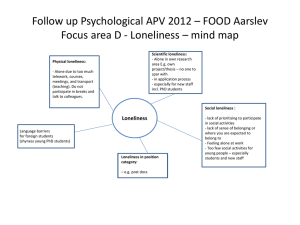
B166 Disasters, Climate Change, and the Growing Population of Older Adults with Dementia K. Ornstein, K. Ferreira, M. Husain, E. Bollens-Lund, B. Liu, A. Kelley. Geriatrics and Palliative Medicine, Icahn School of Medicine at Mount Sinai, New York, NY. Background: Recent years have seen a marked increase of climate-related disasters with potentially devastating consequences for individuals living in the community, particularly vulnerable older adults with dementia who are heavily reliant on caregivers for support. We aimed to estimate the population of older adults—and, among them, the population with dementia—who are living in areas at high risk of natural (including climate-related) disasters. Methods: We used data from the 2014 Health and Retirement Study (HRS), a nationally representative study of older adults merged with publicly available US Natural Hazards Index data from Columbia University’s National Center for Disaster Preparedness (NCDP). US Natural Hazards Index data include county-level hazards across multiple types of natural disasters—wildfire, volcano, tornado, snowfall, landslide, hurricane, heatwave, flood, long-term drought, earthquake, and avalanche—many of which are related to climate change. These data include hazards for each disaster type, as well as an aggregate estimate of hazard level (Multiple Hazard Index) across disaster types. We considered HRS participants to be at high risk of natural disaster if they reside in a county with a Multiple Hazards Index in the top quartile of counties. We then applied survey weights to obtain population-level estimates. Results: We estimated that 45.4% of people over age 65 in the contiguous US live in a county at high risk of a natural disaster, including an estimated 1.3 million people with dementia. Over 80% of older adults reside in a county with a high risk of at least one natural disaster, and 20% of those with dementia living in high risk counties rely on a formal caregiver. Conclusions: The estimated millions of older adults—including those with dementia—living in areas at high risk of climaterelated and other natural disasters highlight the urgency of addressing climate change and the importance of considering these populations in emergency planning efforts. Policy makers, emergency planners, and climate scientists should strongly consider the needs of those living at the intersection of older adulthood, dementia, and risk of climate-related disasters. These issues must be especially considered in light of recent trends towards non-institutional care, reliance on paid caregivers, and distance from family members. B167 Lonely older adults have higher benzodiazepine and opioid use in a nationally-representative sample A. Kotwal, M. A. Steinman, A. K. Smith. Medicine, University of California - San Francisco, San Francisco, CA. Background: Loneliness is associated with poor health outcomes, pain, and depression among older adults. We determine if, as a result, older adults with loneliness use more medications to cope with associated physical or psychological symptoms. Methods: We used data from the National Social life Health and Aging Project (NSHAP) Waves 1-3 (2005, 2010, 2015) an in-person nationally-representative survey including 10,872 community-dwelling older adults age >50. Loneliness was categorized as low, moderate, or high based on the UCLA 3-item loneliness scale. In-home medication logs were conducted where participants were asked to physically bring to the interviewer all medications they take “on a regular schedule, like every day or every week.” We focused on opioids, benzodiazepines, antidepressants, sleep medications, and the presence of polypharmacy (>5 medications). We used multivariate logistic regression to determine the cross-sectional association between loneliness and medication use after adjusting for age, gender, education, S144 AGS 2020 A nnual M eeting race/ethnicity, survey year, impairments in activities of daily living, a comorbidity index, social network size, and marital status. Results: The sample was 54% female, 28% moderately lonely, 17% highly lonely, and on average 70 years old (SD=9.9 years, Range: 50-96 years). The prevalence of medication use by loneliness level was: opioids (low: 5%, moderate: 6%, high: 10%, p<0.001), benzodiazepines (low: 5%, moderate: 7%, high: 11%, p<0.001), antidepressants (low: 13%, moderate: 17%, high: 23%, p<0.001), and polypharmacy (low: 46%, moderate: 48%, high: 52%, p<0.001). After adjustment, high loneliness was associated with increased use of opioids (aOR=1.28, 95% CI: 1.02-1.61, p=0.03), benzodiazepines (aOR=2.02, 95% CI: 1.62-2.54, p<0.001), antidepressants (aOR=1.80, 95% CI: 1.53-2.12, p<0.001), and polypharmacy (aOR=1.21, 95% CI: 1.06-1.36, p=0.004). Conclusion: Older adults who are lonely have higher use of opioids, antidepressants, benzodiazepines, and polypharmacy. These medications may not treat the underlying social experience of loneliness and could partly represent a coping strategy. Clinicians should consider social interventions for lonely older adults to help their symptoms while reducing problematic medications. B168 Distinct Patterns and Predictors of Loneliness and Social Isolation among Older Adults During the Last Years of Life A. Kotwal,1 I. Cenzer,1 L. Waite,2 C. Perissinotto,1 K. Covinsky,1 W. Dale,3 A. K. Smith.1 1. University of California San Francisco, San Francisco, CA; 2. University of Chicago, Chicago, IL; 3. City of Hope, Duarte, CA. Background: Loneliness and social isolation are distinct social risk factors critical to the health of older adults. While the last years of life have an intense focus on medical care, the prevalence and correlates of these two markers of social well-being have not been well described among older adults at the end of life. Methods: We used nationally-representative Health and Retirement Study data to examine adults age >50 who were interviewed once in the last four years of life (N=3,540). Loneliness was measured using the 3-item UCLA Loneliness Scale. Social isolation was determined using a 13-item scale describing whether an individual lived alone, was unmarried/unpartnered, had minimal interaction with children, family, or friends, and had minimal community engagement. We determined the prevalence of loneliness or social isolation overall and by the time in months prior to death. We then used multivariate logistic regression to identify sociodemographic, health, and functional status predictors of end-of-life loneliness or social isolation. Results: The mean age of our sample of decedents was 76 (SD=11.4), 50% were female, 11% black, and 6% Hispanic. The prevalence of loneliness was 69% and this rate was stable for four years prior to death. In contrast, social isolation occurred in 9% of respondents, and there was a non-significant trend indicating increased social isolation prior to death (8-10% at 6 months-4 years prior to death vs 15% at 0-6 months prior to death, p=0.06). Logistic regression revealed distinct risk factors for loneliness versus social isolation; cognitive impairment (Normal: 63%, CIND: 70%, Dementia: 76%), vision impairment (72% vs 66%), incontinence (73% vs 66%), and significant pain (72% vs 67%) were risk factors for loneliness (p<0.01), whereas race (White: 12% vs Non-White: 7%), low net worth (<$6,000: 22% vs ≥$239,000: 7%), and hearing impairment (14% vs 9%) were risk factors for social isolation (p<0.01). Conclusion: Loneliness is common among older adults for several years prior to death, whereas social isolation occurs in 1 in 10 of older adults with the highest prevalence in the months prior to death. Study results provide insight into the burden of and distinct populations at highest risk for end-of-life loneliness and social isolation. 15325415, 2020, S1, Downloaded from https://agsjournals.onlinelibrary.wiley.com/doi/10.1111/jgs.16431, Wiley Online Library on [04/10/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License Poster Abstracts