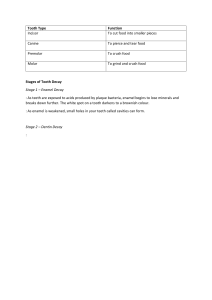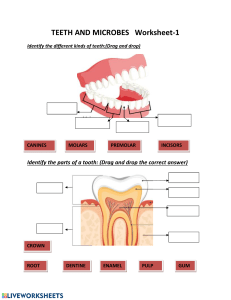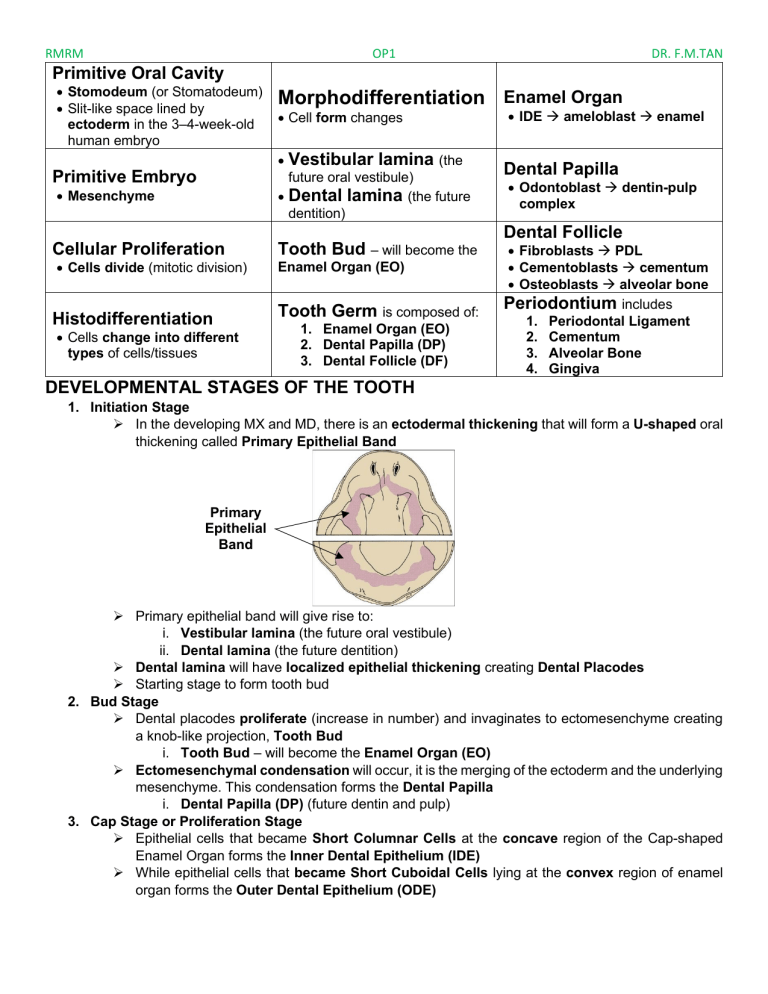
RMRM OP1 DR. F.M.TAN Primitive Oral Cavity • Stomodeum (or Stomatodeum) • Slit-like space lined by ectoderm in the 3–4-week-old human embryo Morphodifferentiation Enamel Organ • Cell form changes • Primitive Embryo Vestibular lamina (the future oral vestibule) • Dental lamina (the future dentition) • Mesenchyme • IDE → ameloblast → enamel Dental Papilla • Odontoblast → dentin-pulp complex Dental Follicle Cellular Proliferation • Cells divide (mitotic division) Histodifferentiation • Cells change into different types of cells/tissues Tooth Bud – will become the Enamel Organ (EO) Tooth Germ is composed of: 1. Enamel Organ (EO) 2. Dental Papilla (DP) 3. Dental Follicle (DF) • Fibroblasts → PDL • Cementoblasts → cementum • Osteoblasts → alveolar bone Periodontium includes 1. Periodontal Ligament 2. Cementum 3. Alveolar Bone 4. Gingiva DEVELOPMENTAL STAGES OF THE TOOTH 1. Initiation Stage ➢ In the developing MX and MD, there is an ectodermal thickening that will form a U-shaped oral thickening called Primary Epithelial Band Primary Epithelial Band ➢ Primary epithelial band will give rise to: i. Vestibular lamina (the future oral vestibule) ii. Dental lamina (the future dentition) ➢ Dental lamina will have localized epithelial thickening creating Dental Placodes ➢ Starting stage to form tooth bud 2. Bud Stage ➢ Dental placodes proliferate (increase in number) and invaginates to ectomesenchyme creating a knob-like projection, Tooth Bud i. Tooth Bud – will become the Enamel Organ (EO) ➢ Ectomesenchymal condensation will occur, it is the merging of the ectoderm and the underlying mesenchyme. This condensation forms the Dental Papilla i. Dental Papilla (DP) (future dentin and pulp) 3. Cap Stage or Proliferation Stage ➢ Epithelial cells that became Short Columnar Cells at the concave region of the Cap-shaped Enamel Organ forms the Inner Dental Epithelium (IDE) ➢ While epithelial cells that became Short Cuboidal Cells lying at the convex region of enamel organ forms the Outer Dental Epithelium (ODE) RMRM OP1 Outer Dental Epithelium (ODE) DR. F.M.TAN EO DP Inner Dental Epithelium (IDE) DF ➢ IDE and ODE secretes glycosaminoglycans into their extracellular compartment, where it pulls water from their surroundings into the enamel organ causing the cells to force apart that forms the star-shaped Stellate Reticulum ➢ Cells of the ectomesenchyme surrounding the EO and DP is the Dental Follicle (DF) or Dental Sac i. Dental Follicle (future periodontal tissues of the tooth) ➢ Tooth Germ is Composed of: i. Enamel Organ (EO) ii. Dental Papilla (DP) iii. Dental Follicle (DF) 4. Early Bell Stage ➢ Invagination deepens until the organ takes on a bell-like form. ➢ Histodifferentiation i. Dental papilla will differentiate to be odontoblast with cytoplasmic extensions • These cytoplasmic extensions will soon line the pulp and spreads to the dentin, making the dentin-pulp complex vital. ii. Short Columnar Cells of Inner Dental Epithelium (IDE) will differentiate into Long Columnar Cells of Ameloblasts • These ameloblasts will become the enamel ➢ Morphodifferentiation i. Dental crown form is determined as guided by the IDE space. EO DF DP 5. Late Bell Stage ➢ Initiation of mineralization will occur as odontoblasts forms the dentin along the future Dentinoenamel Junction (DEJ); ameloblasts, forming the enamel. 6. Root Formation ➢ Cervical Loop at the junction of IDE and ODE will form the Hertwig’s Epithelial Root Sheath (HERS) and it will continue to proliferate turning medially before it grows vertically, growing coronally for the root formation. Enamel and dentin will reach the future cementoenamel junction, and some cells will differentiate to become the future odontoblastic layer, dentin, cementum, and periodontal ligament fibers. 7. Tooth Eruption RMRM OP1 Intrinsic - DR. F.M.TAN Extrinsic Genetics, hereditary, systemic, congenital (not all congenital are inherited), metabolic dysfunction - Generalized (Anomalies) Due to infections, external factors - Usually hereditary (intrinsic) True DEVELOPMENTAL DISTURBANCES OF THE TEETH ALTERATIONS IN SIZE (usually Intrinsic) Anomaly Clinical Types Features 1. 1. Generalized microdontia 2. - More common than generalized macrodontia 3. - All teeth are smaller than normal Conditions Associated Clinical Management Significance 1. Down Syndrome (Pegshaped laterals) Microdontia 4. 5. 6. 7. 8. Tooth/teeth are smaller than the normal size 2. Focal microdontia 2. Ectodermal Dysplasia - One or group of teeth (regional but not all) - More common is one tooth only than group of teeth - Affects nails, enamel, etc. - Posterior teeth most commonly affected - E.g. MX 3rd molar, MX laterals 3. Disproportional microdontia - Relative generalized - Normal, but looks not because of disproportion - Bigger jaw (inherited) so there is spacing Orthodontic treatment Dental - Decreased restorations masticatory such as function crowns or - Esthetics bridges 3. Chondroectodermal Esthetic dysplasia (Ellis-van dentistry Creveld Syndrome) such as - Jaw develops from veneers Meckel’s cartilage RMRM OP1 1. Generalized macrodontia - Less common than generalized microdontia (rare) - All teeth are bigger than normal 2. Focal macrodontia - One or group of teeth (regional but not all) - More common is one tooth only than group of teeth - Posterior teeth most commonly affected, MX 3rd 1.Gigantism molar (Hyperpituitarism) - Generalized 2. Hemifacial hypertrophy Tooth/teeth – Focal Macrodontia are bigger (Megadontism) than the normal size 3. Disproportional macrodontia - Relative generalized - Normal, but looks not because of disproportion - Smaller jaw (inherited) so there is crowding DR. F.M.TAN - Esthetics - Occlusal issues, improper bite alignment Difficult dental treatments due to larger size of teeth (more complex) Orthodontic treatment - Selective tooth reduction Dental restorations such as veneers RMRM OP1 DR. F.M.TAN ALTERATIONS IN NUMBER AND ERUPTIONS Anomaly Clinical Features Types Conditions Associated Clinical Significance Management - They occupy space When impacted, they may block the eruption of other teeth - May cause delayed eruption of adj. teeth - May cause malalignment of the dentition Tooth extractions - Orthodontic treatment for teeth that became misaligned due to supernumerary teeth 9. 1. Mesiodens - Most common supernumerary tooth - Bet. two MX central incisors th 1. Cleidocranial Dysplasia 2. MX 4 molar 2nd most common - Extra tooth/teeth that supernumerary tooth can be found in any location in the oral cavity. - More on MX than MD 2. Gardner’s Syndrome 1. True Supernumerary 3. Peridens - Resembles like a tooth - Erupts outside the dental arch (in form and structure) (ANTERIORS) - Canine most common tooth 3. Down Syndrome (Trisomy 21) Supernumerary 2. False (Rudimentary) Supernumerary - Odd shaped, small 4. Mesiomolar or Distomolar - Found in molar region, like extra molar 5. Paramolars - Erupt on buccal, lingual, or proximal to one of the molars (POSTERIOR) - Usually, PMs not molars 4. Crouzon Syndrome (Craniofacial Dysostosis) RMRM OP1 DR. F.M.TAN 6. Paramolar tubercle - Fused with a permanent molar - Usually, found in molars not PMs 1. Generalized (Complete) Anodontia - Intrinsic, systemic (hereditary) - True anodontia, rare 1. Ectodermal Dysplasia Anodontia - Congenital absence of teeth - Caused by failure of tooth buds to develop - May involve both deciduous and permanent dentition - Hereditary (except false anodontia) 2. Focal/Localized (Partial) 2. Cleft Lip and Palate Anodontia - Regional, one or group of teeth - Hypodontia (1), or oligodontia (2 or more) Failure of Permanent Teeth Eruption causes - Loss of space - Overcrowding 3. Cleidocranial SuperDysplasia numerary and Frequency of Missing supplemental 3. Pseudoanodontia Teeth teeth - Tooth/teeth absent clinically 1. 3rd molars - Retention of because of impaction/delayed 2. MD 2nd PM deciduous eruption 3. MX Laterals 4. Ellis-van Creveld predecessor - Hindered by adj. tooth, tissue, Syndrome 4. MD Centrals or bone 5. MD Laterals - Scarred tissue is hard to erode when tooth is extracted during childhood - Prosthodontics - Orthodontic treatment for partial anodontia RMRM OP1 DR. F.M.TAN 4. False Anodontia - Exfoliated/extracted teeth - Induced anodontia - Teeth are prevented from erupting by: adj. teeth or if crowded (lack of space); early extractions which forms scarred tissue - Tooth impaction have clinical significance: pain and discomfort, infection and inflammation, misalignment of teeth, cyst tumor formation - Dental management includes: surgical tooth extractions, orthodontic treatment, surgical exposure (for forced eruption) MANDIBULAR 3RD MOLAR IMPACTION Pell & Gregory Classification – Ramus Relationship (1st Name) Landmarks: • Point A - Distal of the 2nd molar • Point B - Anterior border of the ramus Impaction enough space Less than MD dia. Of 3rd molar crown 2/3s of the 3rd molar is located within the ramus 1. Class I - There is sufficient amount of space bet. the anterior border of the ramus and the distal portion of the 2nd molar for the accommodation of the MD dia. of the crown of the 3rd molar. 2. Class II - The space bet. the anterior border of the ramus and the distal portion of the 2nd molar is less than the MD dia. of the crown of the 3rd molar. 3. Class III - Tooth is located completely within the anterior border of the ramus - 2/3s is located within the ramus - Least accessible, most difficult to extract RMRM OP1 DR. F.M.TAN Pell & Gregory Classification – Impaction depth in bone (2nd Name) Landmarks: • Point A – Occlusal plane of the 2nd molar • Point B – Highest point of the impacted 3rd molar in level or above occlusal plane of 2nd M below the occlusal plane but above cervical line of 2nd M below cervical line of 2nd M 1. Position A - The highest point of the impacted 3rd molar is in the level or above the occlusal plane of the 2nd molar 2. Position B - The highest point of the impacted 3rd molar is below the occlusal plane but above the cervical line of the 2nd molar - The highest point of the impacted 3rd molar is bet. the occlusal plane of the 2nd molar and its cervical line 3. Position C - The highest point of the impacted 3rd molar is below the cervical line of the 2nd molar Winter’s Classification (3rd Name) - In relation to the long axis of the 2nd molar and impacted 3rd molar 1. Mesioangular 3. Vertical 2. Distoangular 4. Horizontal 7. Linguoangular - 3rd molar impaction where the crown is towards the lingual 5. Inverted 6. Buccoangular RMRM OP1 MAXILLARY 3 RD DR. F.M.TAN MOLAR IMPACTION Based on the relative depth in bone (1st Name) Landmarks: • Point A – Occlusal plane of the 2nd molar • Point B – Lowest point of the impacted 3rd molar in level or below occlusal plane of 2nd M above the occlusal plane but below cervical line of 2nd M above cervical line of 2nd M 1. Position A - The lowest point of the impacted 3rd molar is in the level or below the occlusal plane of the 2nd molar 2. Position B - The lowest point of the impacted 3rd molar is above the occlusal plane but below the cervical line of the 2nd molar - The lowest point of the impacted 3rd molar is bet. the occlusal plane of the 2nd molar and its cervical line. 3. Position C - The lowest point of the impacted 3rd molar is above the cervical line of the 2nd molar Winter’s Classification (2nd Name) - In relation to the long axis of the 2nd molar and impacted 3rd molar 1. Mesioangular 3. Vertical 2. Distoangular 4. Horizontal 7. Linguoangular - 3rd molar impaction where the crown is towards the lingual 5. Inverted 6. Buccoangular RMRM OP1 rd Proximity with the Floor of the Sinus (3 Name) Landmarks: Point A – Bone Point B – Floor of the sinus 1. No Sinus Approximation (NSA) - 3 mm or more bone is present bet. the sinus floor and the impacted 3rd molar bone present 2. Sinus Approximation (SA) - No bone or less than 3 mm of bone is present bet. the sinus floor and the impacted 3rd molar no bone present DR. F.M.TAN RMRM OP1 Identify the developmental anomaly (if present) and classify what type of 3rd molar impaction is shown (Both MX and MD). DR. F.M.TAN RMRM OP1 FURCATION - DR. F.M.TAN IMPERFECTA where roots of a multi-rooted tooth meet - OBLITERATE medical suffix used in naming conditions with abnormalities in structure or function of affected area - to destroy, wipe out DEVELOPMENTAL DISTURBANCES OF THE TEETH ALTERATIONS IN SHAPE AND FORM Anomaly Clinical Features Conditions Associated Etiology / Types Clinical Significance Management SHAPE OF THE CROWN Gemination (double teeth, double formations, joined teeth, fused teeth or dental twinning) Fusion etiology: nutritional, endocrine influences, infectious/inflammatory processes, ingestion of medicines, hereditary or congenital diseases, local - fusion of two teeth trauma, and ionizing radiation from a single enamel 1. Partial Cleavage organ - one tooth, 2 - appearance of two crowns that share the No specific same root canal crowns association - 2 teeth, one tooth germ – common MX anterior - joining of two developing tooth germs - union between dentin and enamel of two or more developing teeth more on deciduous dentition, anteriors - Root canals may also be separated or shared – etiology: local trauma 1. Complete (Total / True Fusion) - fusion begins before calcification stage - crown incorporates enamel, dentin, cementum and pulp of both the teeth No specific association crowding disease and alignment issues - orthodontic treatment, restorative procedures like bonding or veneers - orthodontic treatment crowding - restorative disease and options like alignment veneers or issues crowns might be considered RMRM - may involve the entire length of the teeth, or roots only, in which case cementum and dentin are shared OP1 2. Incomplete (Partial / Late Fusion) - occurs at a later stage - tooth have separate crowns and limited to root alone with fused or separate pulp canals DR. F.M.TAN - etiology: thought to be influenced by of genetic factors during tooth development Taurodontism (Bull Tooth) Talon’s Cusp failure appropriate invagination of Hertwig’s epithelial root sheath (HERS) - enlarged pulp chamber, apical displacement of the pulpal floor, and lack of constriction at the cementoenamel junction - elongated crowns or apically displaced furcations, resulting in pulp chambers that have increased apical-occlusal height 1. Hypotaurodontism - mild form, shorter roots - only the pulp chamber is enlarged 2. Mesotaurodontism - medium sized roots 1. Klinefelter syndrome 2. Tricho-DentoOsseous syndrome 3. Down syndrome 4. Van der Woude syndrome 5. Hypophosphatasia - difficulties in endodontic treatment - can affect occlusion and chewing efficiency - endodontic treatment - orthodontic evaluation - can cause problems with occlusion, increase the risk of - restorative procedures, oral hygiene, orthodontic consideration 3. Hypertaurodontism - root furcation occurs in close proximity to the root apices due to the disproportionately enlarged crown and pulp chamber - Anterior region 1. Rubinstein and lingual surface - etiology: developmental factors during Taybi - common in MX tooth formation 2. Berardinelli-Seip, laterals Mohr - “claw of bird of 1. Type 1: Talon 3. Ellis-van Creveld prey” 4. Sturge-Weber RMRM - Teeth may also exhibit extra small enamel projections called tubercles - excessive folding or invagination of the dental enamel organ OP1 - projects from the palatal (or facial) 5. Incontinentia surface of a primary or permanent pigmenti achromians anterior tooth - extends at least half the distance from CEJ to the incisal edge DR. F.M.TAN fractures, and complicate oral hygiene practices 2. Type 2: Semi talon - additional cusp of a millimeter or more - extending less than half the distance from CEJ to the incisal edge - may blend with the palatal surface or stand away from the rest of the crown 3. Type 3: Trace talon – an enlarged or prominent cingula and their variations, i.e. conical, bifid or tubercle-like Dens Evaginatus (tuberculated cusp, accessory tubercle, occlusal tuberculated premolar, Leong’s premolar, evaginatus - common than dens invaginatus - affects PMs formation of accessory cusp - often bilateral, anomalous tubercle, or cusp, located at the center of the occlusal surface - cusp is composed of normal enamel etiology: both environmental factors genetics and Location: 1. A cone-like enlargement of the lingual No specific cusp association - reducing the cusp's prominence, - can increase restoring with the risk of disease composite caries and material, or pulp even exposure extracting the affected tooth if necessary RMRM odontoma, and occlusal pearl) OP1 and dentin 2. A tubercle on the inclined plane of the containing varying lingual cusp extensions of pulp tissue - due to abrasion, it wears away causing accessory pulp exposure 3. A cone-like enlargement of the buccal DR. F.M.TAN cusp 4. A tubercle on the inclined plane of the buccal cusp 5. A tubercle arising from the occlusal surface obliterating the central groove. Dens Invaginatus uncommon compared to dens evaginatus - dens in dente or tooth within a tooth - etiology: genetic factors involved in No specific represents an some cases association exaggeration or accentuation of the lingual pit - permanent MX laterals, next are - cleaning and disinfecting increases the the invagination disease susceptibility followed by to caries and sealing it with infection a filling material to prevent decay RMRM OP1 DR. F.M.TAN endodontic treatment other anterior, bilateral commonly seen 1. Type I - enamel-lined minor form occurring within the confines of the crown - not extending beyond the CEJ 2. Type II - enamel-lined form which invades the root but remains confined as a blind sac - may or may not communicate with the dental pulp 3. Type III A - penetrates through the root and communicates laterally with PDL space through a pseudo-foramen. - no communication with the pulp, which lies compressed within the root 4. TYPE III B - penetrates through the root and perforating at the apical area through a pseudo-foramen. - invagination may be completely lined by enamel, but frequently cementum will be found lining the invagination Peg-shaped Lateral - undersized, - etiology: predominantly genetically tapered, maxillary determined and can also be caused due to lateral incisor endocrinal disturbances - conical in shape; broadest cervically 1. Tooth agenesis, 2. Canine transposition 3. Over retained deciduous teeth - can impact aesthetics and alignment cosmetic bonding, veneers, or crowns RMRM OP1 DR. F.M.TAN and tapers incisally to a blunt point - single lobe instead of four - etiology: systemic, from mother to fetus during the development of incisors - Central incisors are notched, smaller than normal - Widely spaced and shorter than lateral incisors - yellow-brown or amber coloration - enamel might be hypoplastic (thinner or less mineralized), leading to more translucent appearance 1. Congenital syphilis - can have implications for diagnosis and health assessment diagnosis and medical evaluation, oral hygiene, restorative treatment - Multiple rounded - etiology: systemic, from mother to fetus during the development affecting rudimentary molar formation enamel cusps - molars can also be discolored, often with a yellowishMulberry Molar 1. Congenital syphilis brown hue - enamel may be hypoplastic, leading to increased susceptibility to wear and decay - can have implications for diagnosis and health assessment diagnosis and medical evaluation, oral hygiene, restorative treatment Hutchinson’s Incisors RMRM OP1 DR. F.M.TAN SHAPE OF THE ROOT - etiology: space restriction during development, local trauma, excessive occlusal force, or local infection 1. True/developmental concrescence - occurs during tooth development - close proximity of developing roots of the adjacent teeth Concrescence Enamel Pearl - a form of fusion - cemental union - take place before or after eruption No specific and is believed to be association related to trauma or overcrowding 2. Acquired/post inflammatory - MX 2nd and 3rd concrescence molars - after root formation - may result from a chronic inflammatory response to a non-vital tooth - may occasionally be found on the - etiology: developmental factors during tooth formation, during root sheath roots of teeth - most commonly in differentiation and enamel deposition the bifurcation or trifurcation of teeth No specific but may appear on association single-rooted PM teeth as well MX molars commonly affected than MD molars - if problems arise, - can lead to extraction challenges might be during considered, disease extraction possibly and followed by orthodontic replacement treatment with a prosthetic option - can lead to challenges during disease extraction and orthodontic treatment surgical removal if not causing periodontal issues RMRM Dilaceration OP1 - extraordinary curving or angulation of tooth roots - apical 1/3 for anteriors - middle 1/3 for 1st molars - coronal 1/3 for 3rd molars - root dilacerations more common in posterior, permanent crown dilacerations common in permanent MX incisors the MD incisors (anteriors) - MX incisors show lingual deviation MD incisors incline labially DR. F.M.TAN - etiology: hereditary (few cases only), trauma during tooth development, mechanical trauma (E.g., laryngoscopy and 1. Smith Magenis endotracheal intubation in primary teeth) syndrome 2. Hypermobility type of Ehlers-Danlos syndrome 3. Axenfeld-Rieger syndrome 4. Congenital ichthyosis - etiology: hereditary, trauma, crowding, abnormal habits such as thumb sucking Flexion Ankylosis - can lead to difficulties in - orthodontic tooth treatment, eruption, extraction or alignment replacement issues No specific association - can lead to challenges during disease extraction and orthodontic treatment - orthodontic treatment might be used to align the affected tooth properly - fusion of the root - etiology: hereditary, trauma, idiopathic (dentin or causes cementum) of a No specific tooth to bone association - appears to be in lower level (height) than the other ones - can cause orthodontic disease and occlusal issues, and affect eruption - monitoring the affected tooth's growth and considering orthodontic treatment - deviation or bend of a tooth that is restricted to the root portion of a tooth RMRM OP1 DR. F.M.TAN MACANANG, RIZA MAE R. | DMD4F OP1 LEC Activity 2 DR. F.M.TAN ALTERATIONS OF ENAMEL AND DENTIN Anomaly Etiology / General Characteristics Types / Clinical Features Radiographic Features Histopathologic Features Clinical Significance Management - can result in enamel defects, causing teeth to be more prone to wear, sensitivity, and decay esthetic restorations like crowns, veneers, or bonding ENAMEL - etiology: hereditary patterns (cell mutation – DNA alteration) autosomal dominant or recessive to X-linked dominant or recessive AMELOGENESIS IMPERFECTA (AI) (Hereditary Enamel Dysplasia, Hereditary Brown Enamel, Hereditary Brown Opalescent Teeth) - affects both primary and secondary dentition enamel appears reduced in bulk, thin layer over occlusal and interproximal surfaces - although enamel is soft and irregular, teeth are not caries prone due to lack of interproximal contacts (wear) - dentin and pulp appear normal - Note: enamel: 9899% inorganic mineral and less than 2% organic matrix and water 1. ENAMEL HYPOPLASTIC AMELOGENESIS IMPERFECTA (QUANTITATIVE) - alteration occur during enamel matrix secretion - insufficient amounts of enamel - normal enamel - form pits and grooves (prone to staining as the stain can be absorbed easily) - rough or smooth and glossy, squareshaped crown - yellowish-brown color 1. ENAMEL HYPOPLASTIC AMELOGENESIS IMPERFECTA (QUANTITATIVE) - presence of thin radiopaque layer of enamel with normal radiodensity very thin enamel irregularly arranged enamel prisms - DEJ show some pits grooves exaggerated 2. ENAMEL HYPOCALCIFICATION 2. ENAMEL scalloping AMELOGENESIS IMPERFECTA HYPOCALCIFICATION areas of (QUALITATIVE) AMELOGENESIS homogeneous - alteration occur during calcification IMPERFECTA (QUALITATIVE) aprismatic stage - thickness of enamel is enamel or fused - weaker than hypomaturation AI normal but radiodensity of indistinct prisms, - enamel quantity = normal enamel is less than that of with “a reduction soft and friable, deficiently dentin in distance mineralized between enamel - fractures easily and wears readily rod incremental - white opaque to yellow to brown lines” - abnormal contour and absent interproximal contact points - “picket fence” appearance - teeth appear like crown preparations - sensitive Soft, “cheesy enamel” MACANANG, RIZA MAE R. | DMD4F OP1 LEC Activity 2 3. ENAMEL HYPOMATURATION 3. ENAMEL AMELOGENESIS IMPERFECTA HYPOMATURATION (QUALITATIVE) AMELOGENESIS - alteration occur during maturation IMPERFECTA (QUALITATIVE) stage - radiodensity of enamel is - mineralization begins but maturation similar to that of dentin into dense crystal structure - enamel quantity = normal - mottling, opaque white to brownish yellow discoloration (chalky) - primary teeth: ground glass opaque white appearance - permanent teeth: mottled yellow white, may be darkened with absorption - tight contact point - looks like fluorosis DR. F.M.TAN mottled enamel ENVIRONMENTAL ENAMEL HYPOPLASIA LOCALIZED ENAMEL HYPOPLASIA etiology: not hereditary malnutrition, bacterial / viral infections, trauma, and other severe illnesses experienced during childhood regional or generalized etiology: not hereditary – local infection, trauma to a developing tooth, or disruptions during tooth formation - affects single tooth - more susceptible to decay - insufficient amounts of enamel - horizontal grooves located on middle linear radiolucencies third to incisal third of the tooth crossing the crown - pits, or lines on the tooth's surface, very due to interrupted enamel formation enamel - more caries susceptible - can indicate periods of thin severe physiological stress during tooth development esthetic restorations like crowns, veneers, or bonding - can provide insights into periods of thin localized stress or trauma during tooth development esthetic restorations like crowns, veneers, or bonding horizontal grooves - insufficient amounts of enamel - Turner’s Tooth - vary in size and shape - white, brown, or yellow spots Turner’s Tooth linear radiolucencies crossing the crown very enamel MACANANG, RIZA MAE R. | DMD4F OP1 LEC Activity 2 DR. F.M.TAN DENTIN 1. Type I - collagen gene mutation - syndrome-associated (osteogenesis imperfecta – OI – brittle bone disease) - normal dentin sialophosphoprotein etiology: gene (DSPP) mutations responsible - primary teeth more affected than permanent for dentin formation - roots may be short or blunted amber like - not sensitive - caries resistant appearance - yellowish to brown opalescent dentin - affects both primary and secondary 2. Type II dentition enamel looks - dentin sialophosphoprotein (DSPP) chemically normal gene mutation DENTINOGENESIS but fractures easily - dentin abnormality only but no bone disease IMPERFECTA due to wearing off (Hereditary tulip-shaped, - normal dentin collagen fibers Opalescent Dentin) bulbous crown - patients have only dentin abnormality constricted to but no bone disease - not sensitive cervical area - either too big or too - caries resistant small pulp chamber - Note: dentin: mineral (70%), organic matrix (20%), and water (10%) - organic matrix: collagen & dentin protein (dentin sialophosphoprotein) 1. Type I - partial or total obliteration of pulp chamber and root canals irregular shaped dentinal tubules filled with inorganic tulip-shaped crown substance obliterated pulp - some areas are sclerotic – completely 2. Type II - partial or total obliteration of obliterated by pulp chamber and root canals calcification - loss of enamel due to flat and smooth DEJ weak attachment of enamel to obliterated pulp dentin - bacteria has direct access to pulp due to thin dentin (shell opalescent teeth) for Type III 3. Type III 3. Type III - Brandywine Type - multiple pulp exposures, making prone to periapical - shell teeth periapical radiolucencies lesions - dentin sialophosphoprotein (DSPP) - large pulp chambers gene mutation - dentin abnormality only but no bone disease shell teeth large pulp chambers - can lead to weakened dentin, making teeth susceptible to fractures and wear - diagnosis and evaluation, restorative treatments, endodontic treatments MACANANG, RIZA MAE R. | DMD4F OP1 LEC Activity 2 1. Type I (Radicular Type) - roots are short and may be more pointed than normal - root canals and pulp chambers are absent 1. Type I (Radicular Type) - except for a chevron-shaped - rootless teeth remnants of pulp tissue – - both dentitions are of normal color - crowns appear to be normal in color horizontal radiolucencies and shape - premature exfoliation may occur due to short roots or periapical inflammatory short roots, lesions obliterated pulp - caries resistant 1. Type I (Radicular Type) - short and irregular 2. Type II (Coronal Type) dentinal mutation or deciduous roots are tubules normal color odontoblast has extremely short, pulps are - thin enamel abnormal almost completely obliterated characteristics - permanent dentition are 2. Type II 2. Type II (Coronal Type) - abnormal pulpal large pulp (Coronal Type) - dentin sialophosphoprotein (DSPP) abnormally morphology chambers in the coronal - normal root gene mutation portion of the teeth dentin - primary teeth: opalescent - exhibits a thistle tube pulp - permanent teeth: normal configuration with radiopaque globules of abnormal dentin - etiology: genetic, hereditary, autosomal dominant, or mutation DENTIN DYSPLASIA opalescent in primary short roots, pulp obliteration (primary) Thistle tube configuration (secondary) DR. F.M.TAN - weakened teeth that are more prone to decay and fractures regular dental check-ups restorative procedures or, in more severe cases, extraction and prosthetic options MACANANG, RIZA MAE R. | DMD4F OP1 LEC Activity 2 DR. F.M.TAN ENAMEL & DENTIN - small, and distorted - etiology: rare, local - soft on probing circulatory - irregular contour with surface pits and disorders, viral grooves infections, local - discolored, yellow or yellowish-brown trauma, - translucent or opaque with a mottled pharmacotherapy or pitted appearance REGIONAL during pregnancy, ODONTODYSPLASIA facial asymmetry or a (RO) combination of these (Odontogenic factors Dysplasia, - regional, not all Odontogenesis teeth Imperfecta, Ghost - generally, it is Teeth) localized in only one arch - delayed or failed eruption due to arrested root formation - disorganized or irregularly - ghostlike arranged - faint, fuzzy outline odontoblasts pulp chambers are - thin enamel, enlarged, and the roots dentin, and might be shorter cementum pulp may extend into the roots of the teeth in an irregular manner - in some cases, short roots, the affected large pulp teeth might chambers exhibit the presence of cellular fibrous tissue instead of normal dental pulp esthetic concerns, risk of infection, pain and discomfort - restorations, endodontic treatment, orthodontic treatment, regular dental check ups MACANANG, RIZA MAE R. | DMD4F OP1 LAB Activity 3 DR. F.M.TAN HARD TOOTH TISSUE REDUCTION Anomaly ATTRITION Tooth wear is an irreversible, non-carious, destructive process, which results in a functional loss of dental hard tissue. Radiographic / Conditions Clinical Etiology / Description Clinical Features Histopathologic Associated Significance Features Etiology: - Flat and smooth - flattened and shorter - Bruxism or - Tooth - Parafunctional activities - Shiny wear facet on amalgam contacts coronally with reduction night grinding sensitivity - Mastication (repetitive chewing) - Possible fracture of cusps or in the size of the pulp - Clenching - Changes in - Fibrous diet restorations chambers and canals due tooth shape - Tobacco and bettlenut chewing - Enamel and dentin wear at the same to deposition of - Fractures - Bruxism or night grinding time secondary dentin - Dentin may be yellow or brown stained - pulpal structures can Description: I. Anatomical Involvement become completely - Latin verb: attritum / atterere – 1. INCISAL ATTRITION obliterated (depends on action of rubbing against another - Lack of supporting occlusion as in the degree) surface absence of posterior teeth 1. INCISAL ATTRITION - Wearing away of a tooth as a - Surface of MD ant. teeth is worn result of tooth-to-tooth contact. obliquely - Occlusal, incisal, and proximal surfaces - Lingual surface of ant. MX teeth - Labial surface of ant. MD teeth - Deciduous and permanent 2. OCCLUSAL ATTRITION dentition 2. OCCLUSAL - Due to functional mastication - Usually, age-related process ATTRITION - Physiologic – aging - Pathologic – affects esthetic appearance and function - Factors accelerating destruction: fluorosis, environmental / hereditary enamel hypoplasia, 3. PROXIMAL ATTRITION premature contacts (edge-to-edge - Due to friction caused by tooth occlusion) 3. PROXIMAL movement during mastication - Shortening of length of dental arch and ATTRITION Bite Force Studies reduction in MD dia. ff the teeth - 58 lbs. of force during chewing - 68 lbs. during swallowing - 85 lbs. biting on anteriors - 150-175 lbs. biting on posteriors - 70-900 lbs. during sleep Management Orthodontic management - Restorative Management (crown replacement or onlays) Therapy (bite / night guard) MACANANG, RIZA MAE R. | DMD4F OP1 LAB Activity 3 II. Degree of Anatomical Involvement 1. FIRST DEGREE - Incisal edge / Cusp are worn out flat - No dentin exposure 2. SECOND DEGREE - Incisal edge / Cusp are worn out - Primary dentin are exposed 3. THIRD DEGREE - Ring of secondary dentin is visible 4. FOURTH DEGREE - Pulpal Involvement DR. F.M.TAN MACANANG, RIZA MAE R. | DMD4F Etiology: - Aggressive toothbrushing + abrasive toothpaste + heavy pressure + horizontal tooth brushing stroke - Pencils, toothpicks, pipe stems, bobby pins, tobacco chewing, cracking nuts, biting fingernails ABRASION (mechanical wear) Description: - Latin verb: abrasum / abradere – to scrape off, wear or partial removal through mechanical process - Pathologic wearing of teeth caused by an abnormal habit or abnormal use of abrasive substances orally - Location and pattern are directly dependent on the cause - Degree of lost is greatest on prominent teeth: cuspids, bicuspids, teeth adj. to edentulous area - Can be diffused or localized - More commonly seen on left side of right handed persons - Affects teeth in groups (often unilateral) OP1 LAB Activity 3 Toothbrush Abrasion (Horizontal Brushing Technique) - Horizontal cervical notches on buccal surface of exposed radicular cementum + dentin - Sharply defined margins - Hard smooth surface Thread Biting / Use of Bobby Pins - Rounded or V-shaped notches in incisal edges of anterior teeth Use of Pipe - Notching Cigar Chewing well-defined semicircular or semilunar shape radiolucent defects in cervical level of the tooth - borders are radiopaque - pulp chamber may be partially or fully sclerosed in severely affected teeth - Tooth sensitivity - Caries susceptibilit y DR. F.M.TAN - Composite restoration - Porcelain – buccal or labial up to incisal with metal at the back - Modified cleaning habits MACANANG, RIZA MAE R. | DMD4F OP1 LAB Activity 3 Etiology: Maxillary Anteriors - Multifactorial - Shallow spoon-shaped depressions in - External – work environment, cervical portion of crown e.g., battery manufacturing, competitive swimming, professional wine tasters; diet, e.g., citrus fruits, acid-containing soft drinks - Internal – regurgitation of gastric contents (involuntary or voluntary) - Dental Tetralogy EROSION (chemical erosion) Description: - Latin verb: erosum / eroder – to Posterior Teeth corrode, gradual destruction of - Extensive loss of occlusal surface surface by chemical or electrolytic process - Loss of tooth structure through a nonbacterial chemical process - Most commonly, acids are involved in the dissolution process from an external or internal source. - The pattern of erosion associated with vomiting – generalized tooth loss on lingual surfaces of MX teeth - All surfaces may be affected - Facial and palatal surfaces of MX ant. teeth - Facial and occlusal surfaces of MD post. teeth Erosion related to Acid in soft drinks - Affects teeth in groups (lingual uppers / buccal lowers) Note: - Critical pH of enamel – 5.5 pH - Any solution with a lower pH value may cause erosion (especially when repeated or long duration) - Saliva and the salivary pellicle counteract the acid attacks - Saucer shaped lesions have a smooth featureless surface as well as craters and dimples - First area to be affected is the peritubular dentin Progression makes dentinal tubules become enlarged but disruption is also seen in the intertubular areas - Bulimia – self-induced vomiting - Anorexia nervosa - GI disorders – peptic ulcers, gastritis - Chronic Alcoholism - Pregnancy (hyperemesis gravidarum) - Tooth sensitivity - Change in tooth color DR. F.M.TAN - Crowns (if dentin is not exposed) - Restorative managemen t - Less intake of acidic sources of food MACANANG, RIZA MAE R. | DMD4F Etiology: - Repeated tooth flexure with failure of enamel and dentin at a location away from point of loading - Occlusal forces are applied eccentrically to a tooth - Tensile stress concentration at cervical fulcrum (causing flexure) - Produce disruption in chemical bonds of enamel crystals in cervical areas Description: - Latin words: ab + fractio – away ABFRACTION + breaking - Latin verb: frangere – to break (stress - Loss of tooth structure from corrosion) occlusal stresses - The harder it is, the more prone to microfractures - Dentin is able to withstand greater tensile stress than enamel - Cracked enamel can be lost or more easily removed by erosion or abrasion - Predominantly affects: facial surfaces of bicuspids and molars - Affects single teeth (often upper PM first) OP1 LAB Activity 3 - Wedge-shaped defects limited to cervical area of teeth - Deep, narrow and V-shaped - Occasionally lesions are subgingival - Bruxism - Gum recession - Tooth sensitivity - Caries susceptibilit y DR. F.M.TAN - Composite restoration - Night guards Desensitizin g agents - Fluoride treatments - Dental bonding - Restorative Management (crown replacement or onlays) MACANANG, RIZA MAE R. | DMD4F OP1 LAB Activity 3 DR. F.M.TAN RMRM OP1 DR. F.M.TAN ABNORMALITIES OF THE DENTAL PULP ABNORMALITIES DESCRIPTION / ETIOLOGY • • PULP CALCIFICATION CLASSIFICATIONS BASED OF FORM (Radiographic / Naked eye) Calcified deposits form inside the pulp DENTICLES Etiology: Unknown, but (Pulp Stones / Endoliths) some conditions are • Globules, discrete rounded structures, rounded nodules, foci (more common) associated with pulp BASED ON COMPOSITION calcifications, no clear BASED ON LOCATION (Radiographically) (Histologically) pathophysiology 1. Free – floating, incorporated within the • Aging, 1. True Denticles – structures similar to pulp tissue inflammation, dentin 2. Attached – attached to the pulp cavity nutritional 2. False Denticles – calcified wall / dentin wall deficiency, substance only, not identifiable as 3. Embedded – incorporated within dentin, genetics, etc. dentin radiopaque than the surrounding dentin DENTICLES DIFFUSED CALCIFICATION DIFFUSED CALCIFICATIONS CLINICAL SIGNIFICANCE 1. Impediments / difficulty in endodontic treatment (may bara); endodontic treatment may not be done in some cases o Endodontic treatment difficulty still depends on the SIZE AND LOCATION of calcified tissue • Example: Located in pulp chamber, free floating – you can scoop it out, endo is possible Located in pulp chamber, attached – you can bur it out using endodontic burs o Hardest to treat – endodontic problems associated with pulp calcifications located in the root canal portion 2. Pain and sensitivity due to pulp inflammation o Because it is enclosed in a hard tissue cavity, it causes impingements of the nerve fibers, triggering slight to intense pain 3. Tooth fracture • Runs parallel to the long axis of the blood vessels in pulp canal RMRM OP1 • • • TOOTH RESORPTION Involves resorptive cells (-clast) May happen inside and outside the tooth WILL NOT OCCUR IN NON-VITAL PULP (necrotic pulp), as resorptive cells need nourishment from blood supply DR. F.M.TAN PHYSIOLOGIC PROCESS 1. Resorption in deciduous dentition for the eruption of permanent dentition 2. Orthodontic treatment where the teeth move, PRESSURE causes the resorption PATHOLOGIC PROCESS • It destroys the inside tooth and bone INTERNAL RESORPTION EXTERNAL RESORPTION • Within pulp chamber or root canal • Within the root portion (cementum / alveolar bone) • Odontoclasts • Osteoclasts, cementoclasts CLINICAL SIGNS AND SYMPTOMS WHAT AFFECTS TREATMENT OR PROGNOSIS OF EXTERNAL 1. Pain and discomfort RESORPTION? 2. Discoloration • Time when the process of resorption is discovered • Appears pink because dentin is resorbed • E.g., 3rd molar horizontal impaction that resorbs the root of 2nd making hard tissue to become soft tissues, attracting / molar forming abundant capillaries / blood vessels (granulation o Early detection, good prognosis (regardless of location) tissue) o Late detection, poor prognosis (regardless of location) • Area of resorption becomes highly vascular, and since it comes near with the enamel surface, it appears pink as it reflects the color of the inside tooth structure 3. Prone to fracture • Enamel is brittle, dentin gives the support for the enamel not to be fractured (shock absorber) WHAT AFFECTS TREATMENT OR PROGNOSIS OF INTERNAL RESORPTION? • TIME when the process of resorption is discovered, extent of damage depends on the time (routine radiographic examination is important o Early detection, good prognosis (regardless of location) TREATMENT o Late detection, poor prognosis (regardless of location) • Regardless of time, whether caused by age, trauma, systemic • LOCATION will determine if prognosis is good or bad, including disorders, or idiopathic, it has POOR PROGNOSIS the root canal area, or damage within the dentin 1. Extraction (poor prognosis) TREATMENT 1. Endodontic Treatment (good prognosis) 2. Extraction (poor prognosis) Poor Prognosis RMRM OP1 GENERALLY, WHICH HAS BETTER PROGNOSIS IF BOTH DISCOVERED EARLY, INTERNAL RESORPTION OR EXTERNAL RESORPTION? • Internal resorption, because early detection problem can be resolved (endodontic treatment) • Prognosis of resorption is case to case basis, it depends on the TIMING AND LOCATION • RCT is feasible if you detected resorption early and it depends on the location DR. F.M.TAN RMRM OP1 DR. F.M.TAN PULP UNIQUE CHARACTERISTICS OF THE PULP 1. ENCLOSED WITHIN A RIGID / SOLID / HARD CAVITY ▪ Why pain in the pulp can be very intense? ▪ It does not allow / accommodate swelling caused by inflammation, no room for expansion, resulting to impingements of nerve fibers due to increased vascular pressure 2. HIGHLY VASCULAR soft tissue containing blood vessels, lymphatic vessels, and nerve fibers 3. Has TERMINAL BLOOD VESSELS ▪ Why pulp undergoes necrosis once it is damaged? ▪ It has only one main vessel (without collateral circulation) or backup blood supply; so, there will be no revascularization (e.g., trauma due to intrusion)—causing necrosis ▪ But if it is in the case of traumatized developing tooth with an open apex, revascularization is still feasible, there will be backup blood supply ▪ Fully developed tooth with closed apex is not feasible to be revascularized 4. Has FREE NERVE ENDINGS only ▪ Why pain is the only type of sensation felt in the pulp? ▪ Free nerve endings are pain receptors; all stimuli are interpreted / perceived as pain 5. Has NO PROPRIOCEPTORS, location detector ▪ Sometimes you cannot pinpoint where the pain is coming from ▪ Pain felt is diffused or referred pain (not localized) CAUSES OF PULP DISEASE 1. Physical (No bacteria on the first place) o Mechanical o Thermal o Electrical 2. Chemical (Erosion) (No bacteria on the first place) 3. Bacterial (Bacteria is the direct cause) • Type of pulpitis depends on the intensity of damage • Exposed dentin is prone to pulp diseases as odontoblastic processes are exposed and bacteria has a direct access up to the pulp due to the dentinal tubules. • Bacteria is not always the main cause, but this will intensify the severity of pulpitis INFLAMMATION OF THE PULP • As the bacteria / irritant has been detected by the defense cells, they go out of the circulation reacting with the irritant • The interaction between the defense cells and pulp irritant increases blood flow in the area, causing SWELLING • Swelling causes impingement of the nerve fibers present in the pulp, resulting to PAIN GOOD EFFECT OF INFLAMMATION (FUNCTIONAL) • We need inflammation TO ELIMINATE THE BACTERIA in our body • If there is no inflammation, there will be a rapid infection SIDE EFFECTS OF INFLAMMATION • Depends of the virulence or the extent of the irritation or inflammation • Cardinal signs of inflammation: o REDNESS (Rubor); HEAT (Calor); SWELLING (Tumor); PAIN (Dolor); Loss of function WHICH IS MORE PAINFUL, INFLAMMATION IN SKIN OR IN PULP? • Pulp, because there will be an increase pressure in the blood supply; and remember that the pulp is enclosed within a solid cavity, so there will be no room for expansion caused by the increased pulp volume which causes swelling, making the nerves of the vital pulp to be impinged, causing mild, moderate, to severe pain ▪ VIRULENCE OF BACTERIA / HOST RESISTANCE WILL DETERMINE IF THE DISEASE WILL BE REVERSIBLE OR NOT. ▪ Severity of inflammation is directly proportional to the intensity of pain • Prognosis is better if the area of inflammation is in the area where there is high vascularity Which will have more severe bacterial invasion, the fractured tooth with exposed dentin or pulp in the oral cavity, or exposed pulp due to wrong preparation done by the dentist (properly isolated, sterile burs are used)? • • Fractured tooth, because bacteria (from the saliva) will have a direct access up to the pulp (even if dentin is the only part the is exposed) due to open dentinal tubules. Thus, this will have more intense inflammation, so more intense pain. Bacterial invasion can be prevented in an exposed pulp caused by wrong tooth preparation by placing pulp medicaments as soon as possible. (Good prognosis) RMRM OP1 DR. F.M.TAN DISEASES OF THE PULP PULP DIAGNOSES 1. NORMAL PULP 2. REVERSIBLE PULPITIS - Bacteria has pulp access via open dentinal tubules - Tubules widens apically, bacteria spread faster 3. SYMPTOMATIC IRREVERSIBLE PULPITIS (Acute, rapid onset, dentin is not yet broken / opened) - Continues bacterial invasion, slow process - Host response, virulence of bacteria affects the process 4. ASYMPTOMATIC IRREVERSIBLE PULPITIS (Chronic, dentin is broken, opened, pulp exposed, pressure released) 5. PULP NECROSIS 6. PREVIOUSLY TREATED PULP 7. PREVIOUSLY INITIATED THERAPY DESCRIPTION / SIGNS / SYMPTOMS PULP TESTING (PULP VITALITY TEST) Electric, hot, cold test (+) Normal pulp, no problem Reaction for a few seconds, pain does not linger upon removal of stimulus Inflamed but can still be treated, can recover back to normal (also with the help of defense mechanism) (+) Inflamed and cannot be recovered due to severe inflammation (terminal stage) In symptomatic IP: Severity may progress into Hyperplastic (Pulp Polyp) Asymptomatic Irreversible Pulpitis or Pulp Necrosis Can be caused by the progression of irreversible pulpitis, or trauma, etc. Reaction for a minute or two, pain disappears after removal of stimulus (-) (still confined within the pulp) Pain lingers for a long time (provoked) even after removal of stimulus, or unprovoked pain without stimulus; intense, sharp, shooting, pulsating pain Response may be similar to acute apical periodontitis (+) (-) Parang brain dead na ito, pero buhay pa (still confined within the pulp) (-) May elicit pain, if there are remaining pulp that is not dead i.e., accessory canals May still elicit pain, if there are remaining pulp debris (not properly prepared canal) (-) RCT on going (-) (still confined within the pulp) PALPATION TEST To check swelling or tenderness on the tissue area (-) RADIOGRAPHIC FINDINGS No findings Radiograph: Normal, intact, no remarkable changes No findings Radiograph: Normal, intact, no remarkable changes No findings Radiograph: Normal, intact, no remarkable changes, restorations can be seen if with large caries No findings Radiograph: Normal, intact, no remarkable changes No findings Radiograph: Normal, intact, no remarkable changes No findings Radiograph: Normal, intact, no remarkable changes No findings Radiograph: Normal, intact, no remarkable changes (+) (-) RCT done PERCUSSION TEST (PERIAPICAL TISSUE TEST) Non-affected tooth first, so there will be basis for comparison (pain) May still elicit pain since ongoing treatment, if there are remaining pulp tissue Can be false positive (-) (-) (-) RMRM OP1 1. INTERNAL RESORPTION • • • DR. F.M.TAN ASYMPTOMATIC IRREVERSIBLE PULPITIS 2. HYPERPLASTIC PULPITIS (PULP POLYP) Starts from reversible pulpitis first, slow process Resorption may have pain or no pain No symptoms but pulp cannot be recovered • • • • • Starts from symptomatic irreversible pulpitis: mild, moderate, intense pain Long standing inflammation, inflammation is still on going PRESSURE is released, thus, asymptomatic (since there is no impingement of nerve fibers present) Inflammation causes hyperplastic reactions of pulp producing more fibers + dead bacteria + chronic inflammatory cells, forming granulation tissue Common in newly erupted 1st molar, open apex NOTE: • Subjective Symptoms – Varies (Depends on the patient’s pain threshold, immune system, etc.), not reliable source • Objective Symptoms – All the same, with the help of clinical tests • You cannot apply medicaments in pulp with disease, especially worse cases • Inflammation does not always mean that the site has bacteria. Sometimes it is just secondarily infected by bacteria. • Symptomatic = Acute, painful, intense • Asymptomatic = Chronic, not painful • Infection always finds a path with least resistance RMRM OP1 DR. F.M.TAN PERIAPICAL DISEASES (APICAL PERIODONTITIS) • • • • Untreated necrotic pulp / symptomatic / asymptomatic irreversible pulpitis can lead to periapical diseases May not always arise from a diseased pulp o E.g., due to trauma; normal tooth, with periodontal disease Periapical diseases do not eliminate the bacteria, they just confine it Bacteria continue to build up + dead tissue will drain to the root apex o Going to the thin layer of periodontal ligament tissue, reacting with the inflammation o Due to its thin / small area, few tissues, it cannot confine the infection, so the infection will progress to the surrounding bone o Radiographically, it is seen as the widening of periodontal ligament space, as the bone is will be destructed / destructed already DISTINCT FEATURE OF PERIAPICAL DISEASE (RADIOGRAPHICALLY) • Periapical Radiolucency 1. Cyst 2. Granuloma 3. ABSCESS • ILL-DEFINED MARGIN, it blends with the surrounding tissue; spreads faster CHRONIC ASYMPTOMATIC LESIONS • Slow growing, long duration • Has SCLEROTIC MARGIN – WELL-DEFINED SCLEROTIC BORDER; represents new layer of bone, osteoblasts lay down new bone since the lesion is slow growing 1. CYST 2. GRANULOMA • To know if granuloma or cyst, do histologic examination IMPORTANCE • Confines the bacteria discharged from the root canal space • Prevents bacteria from spreading into adjacent bone marrow spaces and other surrounding tissues IN RETURN • Bone will be destroyed / resorbed, bone will sacrifice Cyst / Granuloma Abscess RMRM PERIAPICAL DISEASES (APICAL PERIODONTITIS) 1. SYMPTOMATIC APICAL PERIODONTITIS (ACUTE) Periodontal ligament tissue is only a thin layer so the spread of infection spreads faster to the adjacent bone structure • If it will confine bacteria, CAP • If not, AAA OP1 DESCRIPTION / SIGNS / SYMPTOMS Initial time of entry, inflammatory products has reached the apical tissue (PDL), Intense pain (No space in the periapical area, inflammation causes pressure) No bone destruction yet PULP TESTING (PULP VITALITY TEST) Electric, hot, cold test Can be false positive, not always (-) Response may be similar to symptomatic irreversible pulpitis (for early stage only of AP) DR. F.M.TAN PERCUSSION TEST (PERIAPICAL TISSUE TEST) Non-affected tooth first, so there will be basis for comparison (pain) PALPATION TEST To check swelling or tenderness on the tissue area RADIOGRAPHIC FINDINGS Normal (early stages), but there can be slight periodontal ligament space widening (for later stages) With or without slight periapical radiolucency (not well-defined) (+) (+) (pressure = pain) (apical) Cyst or Granuloma, well-defined sclerotic border, periapical radiolucency (hallmark of periapical disease) 2. ASYMPTOMATIC APICAL PERIODONTITIS (CHRONIC) Bone will be resorbed in return to bacterial confinement and infection spreading (- / +) Released Pressure = No Pain • Granuloma • Cyst (has thick lining) (Negative if progressed from necrotic pulp, positive if progressed from irreversible pulpitis) (-) (-) RMRM 3. ACUTE APICAL ABSCESS (SYMPTOMATIC) • Pus – degradation products of Can be secondarily infected inflammation, dead granuloma / cyst from bacteria and existing periodontal disease neutrophils (due to virulence of bacteria) Exacerbation of existing • Abscess – lesion, granuloma / cyst localized collection of pus • Cellulitis – not localized pus, spreads OP1 Presence of swelling (- / +) (Negative if progressed from necrotic pulp, positive if progressed from irreversible pulpitis) (+) (+) (apical) (pressure = pain) (-) 4. CHRONIC APICAL ABSCESS No Pain (there is drainage) Abscess will find and area with least resistance, creating sinus tract Fistula can appear on other areas (not adjacent to the infected tooth) (- / +) (Negative if progressed from necrotic pulp, positive if progressed from irreversible pulpitis) DR. F.M.TAN Periodontal ligament space widening, with radiolucency (well-defined) (-) Presence of fistula, draining sinus, gingival swelling, tenderness, redness Periodontal ligament space widening, with radiolucency (or mild pain) Well-defined periapical radiopacity, associated with carious tooth 5. CONDENSING OSTEITIS Forms bone instead of destructing, can be cementoblastoma or osteoblastoma (-) (+) (process of inflammation) (-) If intact (vital) tooth, not coming from a carious lesion, tumor (i.e., cementoblastoma) RMRM OP1 NOTE: • Granuloma can become cyst if it remains chronic, or directly become abscess (bacterial invasion) o Proliferation of epithelial cells, connective tissues, inflammatory cells can transform into cystic formation o Secondarily affected granuloma can become abscess • Cyst cannot become granuloma o Secondarily affected cyst can become abscess ADDITIONAL NOTES • • • • • The goal of infection is to find drainage, to be drained out. If left untreated, the virulence of bacteria will increase, causing more complex and severe damage (tissue destruction – consequence in defense mechanism; i.e., cyst / granuloma / blood clot (thrombus)). Infection will find its path of least resistance; it depends on: o Local Factors ▪ Thickness of the bone (e.g., in maxilla, buccal/facial is thinner compared to palatal bone) ▪ Anatomic location of the root ▪ Presence of Connective Tissue (CT) Barriers (i.e., muscle attachment) o Systemic Factors ▪ Host response ▪ Virulence of Bacteria If infection penetrates and destructs the cortical bone / plate and exits in: o ENCLOSED AREA (kulob) – ABSCESS (A lesion, localized infection of soft tissue, localized collection of pus) – Confined in area with CT BARRIERS (i.e., muscle attachments) o FASCIAL SPACES (kalat) – CELLULITIS (Not localized, widespread infection in fascial spaces) – E.g., posterior tooth infection (either MX / MD) spreading to buccal space ▪ -itis – acute, its onset signifies the entry of bacteria, INFLAMMATION ONLY, NOT INFECTION (E.g., Cellulitis) ▪ If infection spread in buccal space – Buccal Space Cellulitis (swelling of buccal space) ▪ Sublingual space and submandibular space are connected, divided by mylohyoid muscle ▪ If infection spread in sublingual and submandibular space – Ludwig’s Angina LUDWIG’S ANGINA - very common among young patients, cellulitis spreading in the floor of the mouth and neck o ENT first before dental department o Infection in Ludwig’s Angina spreads very fast as it spreads directly into the submandibular space (not through lymphatics); the roots of lower teeth are close to mylohyoid muscle which are located within submandibular space CAVERNOUS SINUS THROMBOSIS – defense mechanism forms blood clot (thrombus) containing bacteria (in response to infection) and reaches / trapped / occluded in the cavernous sinus (venous drainage of the brain, not a sinus) o During soft tissue infection, body forms blood clot to contain and prevent the spread of bacteria, circulating in the body DR. F.M.TAN RMRM OP1 DR. F.M.TAN RMRM OP1 DR. F.M.TAN OSTEOMYELITIS, CONDENSING OSTEITIS Disease Etiology / Description OSTEOMYELITIS Etiology: • Extension of periapical abscess • Physical Injury such as fracture or surgery • Bacteremia • Trauma Description: • Acute and chronic inflammatory process in the medullary cortical surfaces of bone that extends away from initial site of involvement CONDENSING OSTEITIS (Focal Sclerosing Osteomyelitis) Etiology: • Low grade focal bone irritation (e.g., pulpitis) Description: • Periapical lesion that is seen at the apex of a tooth with long standing pulpitis Pathophysiology / Tissue Damage Pathophysiology: • The periapical area infection is left untreated, causing the spread of infection into the adjacent cortical bone • The infection spreads in the medullary bone instead of making drainage (drainage will occur after) • Some parts of medullary bone are not destroyed Tissue Damage: • Bone destruction, resorption Clinical Signs and Symptoms • • • • • • Radiographic Features Histopathologic Feature • Opaque-lucent • Resorption of the lesion or demineralized bone over time diffuse radiolucent • Purulent Pain exudate changes begin to appear Pyrexia • Bony Painful lymph- • Islands / remnants of bone trabeculae (Sequestra – undestroyed adenopathy showing bone) Leukocytosis reduced Paresthesia of osteoblastic the lower lip activity Draining Sinus • Sequestrum Management • Antibiotics and Drainage • Sequestrect omy Pathophysiology: • Radiopaque mass usually at • Asymptomatic • The periapical area infection is the apex of the premolar or found on routine • Lymphocytes left untreated, causing bone molars dental and plasma calcification examination cells • Root Canal Tissue Damage: • Mild, persistent, • Sequestrum treatment • Bone calcification instead of and dull pain in • Fibrosis resorption the affected area. replacing fatty • Associated with carious • No systemic manners tooth (if not, can be symptoms like cementoblastoma) fever or chills. SUPERFICIAL INFECTION CELLULITIS Etiology: • Bacterial infection Description: • Acute inflammatory process that diffusely spread throughout the tissue rather than localized Pathophysiology: • From an untreated infection, the infection penetrates and destructs the cortical plate and exits in fascial spaces (not localized spread) Tissue Damage: • Bone destruction, tissue destruction • • • • Pain and tenderness Redness and inflammation Fever Abscess with pus • CT Scan shows a cobble stone appearance • Zone of liquefaction composed of proteinaceou • Antibiotics s exudate IV • Main bacteria • Surgical Streptococcu drainage s and Staphylococc us RMRM OP1 DR. F.M.TAN DEEP FACIAL INFECTION CAVERNOUS SINUS THROMBOSIS LUDWIG’S ANGINA Etiology: Pathophysiology: • Bacterial infection has • From an untreated infection, spread to the blood the defense mechanism of the stream body is to form a blood clot Description: (thrombus) • Very rare life- • The thrombus (containing threatening condition bacteria) circulates and that can affect adults and became occluded in the children, a blood clot cavernous sinus. blocks a vein that runs Tissue Damage: through a hollow • Swelling / redness in the space underneath the areas which are lined with the brain behind the eye venous drainage of the brain socket. The veins carry (cavernous sinus) blood from the face and head back to the heart. Pathophysiology: • From the untreated infection (e.g., apical abscess), the Etiology: infection spreads directly • Trauma to the floor of into the submandibular the mouth space and up to the floor of • Upper respiratory the mouth and neck. infection Tissue Damage: • Oral lacerations • Neck / face swelling • Endotracheal intubation. • Tongue piercing Description: • Soft tissue infection of the floor of the mouth which is bilateral and involves the submandibular and sublingual spaces • Unilateral periorbital edema • Headache, • Photophobia • Paralysis of cranial nerve • Proptosis (bulging of eyes) • CT scan reveals a bulging lateral margin of cavernous sinus • Staphylococc us and • Broad Staphylococc spectrum al antibiotics IV • Zone of liquefaction • Surgical composed of Drainage proteinaceou s Exudate • Radiopaque • • • • • • • • • • Fever Tachypnea Swelling Pain in the floor of the mouth Hoarseness of voice Difficulty swallowing (dysphagia) Difficulty speaking Drooling Respiratory disease (advanced stage) Pus drainage from the floor of the mouth or throat. • Antibiotics • Corticostero • Staphylococc ids us and • Endotrachea Staphylococc l intubation al • Tracheosto my RMRM [ADDITIONAL NOTES FROM CANVAS] OP1 DR. F.M.TAN CYSTS OF THE ORAL REGION ODONTOGENIC CYST Odontogenic Cysts are those cysts which derives from epithelium associated during the development of the dental apparatus. The tooth involved may be vital or non-vital and the pain may or may not be present. Asymmetrical appearance of the jaw may be evident as the cysts grows. Disease Etiology / Description Clinical Features Radiographic Features Histopathologic Feature Management • Radiolucency at the end of root of a nonEtiology: • Surgical vital tooth • Asymptomatic • An epithelial jaw cyst, caused by incision inflammatory activation of • Will not response to coupled RADICULAR • Lined with nonepithelial any standard pulp with CYST keratinized Description: testing procedures removal (Apical or epithelium of cause • Often found on tooth with deep • Invisible on intraoral Periapical Cyst) will cure carious lesion, deep restoration clinical examination the cyst and inadequate root canal filling • DENTIGROUS CYST (Follicular Cyst) Description: • A common epithelial lined jaw cyst • Surrounding the crown of an unerupted or impacted tooth • Common in mandibular 3rd molar and maxillary cuspid • May cause root resorption on adjacent tooth • Hollowing out in an unerupted mandibular 3rd molar of the entire ramus extending up to the coronoid process and condyle • • Solitary well defined radiolucent that surrounds the crown of an unerupted teeth or supernumerary teeth • Facial asymmetry – enlargement of jaw Displacement of tooth Radiographic Variations 1. Central Variety – cysts surrounding the crown of tooth and the crown projects into the cyst 2. Lateral Variety – usually associated with mesioangular impaction, cysts grow Complete surgical removal RMRM OP1 • PRIMORDIAL CYST Description: • Arises from a tooth germ that extend pushing a tooth adjacent into a cyst • Least common type of odontogenic cyst • Found in place of a tooth rather than clinically associated with one • • • • Associated with a missing tooth Mandible involved more frequent than the maxilla Enlargement of jaw Asymptomatic and may cause migration of erupted teeth All teeth in the area are vital DR. F.M.TAN laterally along the root surface and partially surrounds the crown 3. Circumferential – cysts surround the crown and extends for some distance along the root • Well determined radiolucency in place of normal tooth • Situated below the neck of teeth or root of adjacent teeth or near the crests of the ridge • • ODONTOGENIC KERATOCYST (Keratocyst or Keratinizing cyst) Description: • A jaw cyst of Dentigerous or Primordial origin • Common in the mandible • Mandibular 3rd molar is the common site Multilocular Appearing as a radiolucent around the crown of an unerupted tooth (dentigerous) or in a missing tooth (primordial) \ • Lined with keratinizing epithelium • Keratinized epithelium Actively proliferating epithelium Keratinize filter central cavity Thin cyst wall – epithelium and CT Flat epithelium – CT interfere Epithelium pouches – cul de sacs, scattered cyst • • • • • • Surgical removal with thorough curettage of the bone • Excision, but they tend to recur RMRM OP1 DR. F.M.TAN • • • LATERAL PERIODONTAL CYST Description: • Rare of unknown etiology • Found on interdental alveolar process between adjacent teeth • Associated tooth is vital Anterior region of mandible is commonly affected No clinical signs and symptoms may be only determined during routinely radiographic examination of teeth • Solitary small (1 cm in diameter) circumscribed radiolucency in the lateral surface of a tooth root Cystic border is surrounded by a thin layer of sclerotic bone • • RCT with enucleati on or extractio n Does not recur after removal NON-ODONTOGENIC CYST Non-Odontogenic Cysts develop from epithelium trapped during the development of the oral cavity. These cysts are not associated the dentition but may somehow affect the position of it as the cysts expands. • Fissural cysts are not related to teeth • Fusions of upper jaw bones and from epithelial trapped during development of the oral cavity and face • It does not arise in the mandible and is formed by the fusion of separate structures • Upward down pearDescription: shaped radiolucency • Arises from epithelial remnants • Non-keratinizing between the maxillary left during fusion of the globular • Enlargement and migration • Lines with canine and lateral of adjacent teeth and maxillary process of the stratified incisor GLOBULLOMAXIL embryonic face • Asymptomatic squamous non LARY CYST • Neck of the pear is • Seen between the root of • Teeth are vital keratinizing between the coronal maxillary lateral incisor and epithelium pars of these teeth canine • Root of canine and central incisor are • Enucleati on – removal of cyst RMRM OP1 DR. F.M.TAN spread apart by the radiolucency • • Description: • May arise from proliferation of epithelium trapped during the NASOLABIAL development of middle face CYST (lacrimal duct) (Nasoalveolar Cyst) • Rare soft tissue cyst appearing as a facial swelling • MEDIAN PALATAL CYST Description: • Situated in the midline of the palate • • Asymptomatic Lesion is confined solely to the soft tissue and are Swelling in the midline of the palate Covering mucosa is intact May cause problems during mastication and speech • Not visible in radiographs, it can only be seen by using intravenous dyes such as Barium • Circumscribed area in the midline of the hard palate Mistaken to nasopalatine cyst because of its site, which is in the anterior position • • Excision in the labial vestibule to avoid facial scar • Surgical excision RMRM OP1 DR. F.M.TAN • Description: • Most common of all nonodontogenic cyst NASOPALATINE CYST • Incisive Canal – located in the (Incisive Canal incisive papilla Cyst) • Cyst of Palatine Papilla – located within the nasopalatine canal • • • • Asymptomatic Elevation in the anterior part of the palate Covering mucosa is normal Teeth in the area are vital • Heart shaped radiolucency located midline just lingual to the maxillary central incisor Superimposition of the nasal spine on the radiolucent area • • • Excision Enucleati on Removal