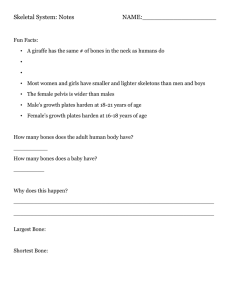
Skeletal System: Anatomy & Physiology Presentation
advertisement

SKELETAL SYSTEM Prepared by Red Steven Nillo,RMT LEARNING OBJECTIVES • Define Skeletal System • Explain how bones formed • Explain the physiology of skeletal system • Be familiar with the pathophysiology of some disorder associated with skeletal system. WHAT IS A SKELETAL SYSTEM Provides a structural framework in the body. There are 206 bones in the human body. More than just bones; it’s also ligaments and cartilage and the joints that make the whole assembly useful. 2 DIVISIONS OF SKELETAL SYSTEM AXIAL BODY Skull Ribcage Vertebral column Appendicular Body Arms and Legs Shoulder Pelvis Support FUNCTION OF SKELETAL SYSTEM Protection Mineral Storage Movement Blood cell production Five types of Bones according to shape A.Long bones B. Flat Bones C. Short Bones D.Irregular Bones E. Sesamoid Bones CARTILAGE Three major cartilage Hyaline cartilage- most important among the three. Elastic Cartilage Fibrocartilage HYALINE CARTILAGE • Chrondoblasts- produce extracellular matrix • Chrondocyte- cell that occupies the space of lacunae in the matrix • Lacunae- space within the chrondocyte • Perichondrium- Cover of the cartilage. Consist of two layers: Outer Lining: composed of dense irregular connective tissue. Inner Lining: consist of few fibers and chrondoblasts Articular Cartilage- A type of hyaline cartilage that covers the ends of bones where they come together to form joints. Articular cartilage does not have perichondrium, blood vessels and nerves. CARTILAGE GROWTH • Appositional Growth (takes place on the surface) Perichondrium add new cell cartilage to the outside edge of existing cartilage. Chrondoblast secretes new matrix and add new chrondocytes to the outside of the tissue. • Interstitial Growth Chrondocyte divide and become chrondoblast to add more matrix between existing cells within its lacuna. BONE COMPOSITION A. Bone Matrix Consist of inorganic substance (Hydroxyapatite) and organic substances (collagen and proteoglycans) If hydroxyapatite is absent= Bone will become FLEXIBLE. If Collagen and Proteoglycans are absent= Bone will become BRITTLE. B. Bone Cells Osteoblast, Osteocyte, Osteoclast OSTEOGENESIS IMPERFECTA • Also known as Brittle Bone Disorder • This connective tissue disease is caused by mutations that yield reduced or defective type I collagen. Type I collagen is the major collagen of bone, tendon, and skin. OSTEOBLAST • Known as bone- forming cells. • Responsible in collagen and proteoglycans production Matrix Vesicle- contain hydroxyapatite that once release it serve as the seed to form hydroxyapatite and mineralized the matrix. Ossification or Osteogenesis- process of osteoblast to form bone by means of appositional growth. Calcification- takes place during the ossification of bones it can also occur in other tissues. OSTEOCYTE • Inactive cell of the bone but capable to produce components to maintain the structure of the bone. OSTEOCLAST • Known as bone destroying Responsible in bone resorption or breakdown of hydroxyapatite to Calcium and Phosphate. Bone Resorption - process by which osteoclasts break down the tissue in bones and release the minerals, resulting in a transfer of calcium from bone tissue to the blood. SPONGY BONE VS COMPACT BONE SPONGY BONE Contains blood vessels and has less bone matrix. Trabeculae and bone marrow can be found in spongy bone. COMPACT BONE More dense than spongy bone due to more matrix. LONG BONES Long bones can be found in upper and lower limbs. Parts of a Long bone • Epiphysis • Diaphysis (primary ossification center) • Epiphyseal Line GROSS ANATOMY OF TYPICAL LONG BONES BONE DEVELOPMENT • During fetal life our body consist of embryonic skeleton which are compost of fibrous membrane and hyaline cartilage Two types of bone development process a. IntramembranousOssification Endochondral Ossification INTRAMEMBRANOUS OSSIFICATION • During 8th week intramembranous ossification of the delicate connective tissue will start until 2 years of age. Central of ossification- location of the membrane where ossification begins. Fontanel is a large, membrane-covered spaces between the developing skull bones that have not yet been ossified. Example: Skull, mandible, diaphysis of collarbone , ENDOCHONDRAL OSSIFICATION • Formation of bone from hyaline cartilage. • All of the bones of the body except from flat bones of the skull, mandible and clavicles are formed by endochondral ossification. BONE GROWTH • Bones increase in size only by appositional growth, the formation of new bone on the surface of older bone or cartilage. Growth in Bone Length Growth at Articular Cartilage Growth in Bone Diameter GROWTH IN BONE LENGTH • Female stops growing at the age of 18 and males stops growing at the age of 21 in the process called epiphyseal plate closure. • Majority appendicular bones undergo bone growth. 4 ZONES IN THE EPIPHYSEAL PLATE a. ZONE OF RESTING- CELLS DO NOT DIVIDE b. ZONE OF PROLIFERATION- CHONDROCYTES BEGINS TO DIVIDE c. ZONE OF HYPERTROPHY- CHONDROCYTES BEGIN TO MATURE AND ENLARGE d. ZONE OF CALCIFICATION- HYPERTROPHIED CHONDROCYTES BEGINS TO CALCIFIED; CONSIST OF OLDER AND DYING CHRONDOCYTES. GROWTH IN ARTICULAR CARTILAGE • Epiphyses increase in size because of growth at the articular cartilage. • The process of growth in articular cartilage is similar to that occurring in the epiphyseal plate. • The chondrocytes near the surface of the articular cartilage are similar to those in the zone of resting cartilage of the epiphyseal plate. In the deepest part of the articular cartilage, nearer bone tissue, the cartilage is calcified and ossified to form new bone. GROWTH IN BONE DIAMETER • Long bones increase in width (diameter) and other bones increase in size or thickness because of appositional bone growth beneath the periosteum. FACTORS AFFECTING BONE GROWTH 1. Nutrition- Vitamin D, C, A are essential in creating a strong bone matrix. 2. Hereditary- genetic factors 3. Hormones- growth hormone, sex hormones 4. Mechanical Stress- stress on bone tissue can cause osteoblast to produce more matrix and make bone stronger. RICKETS • Insufficient vitamin D in children causes rickets, a disease resulting from reduced mineralization of the bone matrix. Children with rickets may have bowed bones and inflamed joints. • Osteomalecia- is the adult form of rickets. BONE REPAIR 1. Hematoma Formation- formed due to leakage of blood to outside tissue. 2. Callus Formation- callus is a mass of tissue that forms at a fracture site and connects the broken ends of the bone. 3. Callus ossification- the fibers and cartilage of the internal callus are replaced by woven spongy bone, which further stabilizes the broken bone. 4. Bone Remodeling- Filling the gap between bone fragments with an internal callus of woven bone is not the end of the repair process because woven bone is not as structurally strong as the original lamellar bone. BONE REMODELING • Replacement of old bones by new bones is called bone remodeling. • In this process, osteoclasts remove old bone and osteoblasts deposit new bone. Functions of Bone Remodeling 1. Bone growth 2. Changes in bone shape 3. Adjustment of the bone to stress, bone repair 4. Calcium ion (Ca2+) regulation in the body. BONE REMODELING • As a long bone increases in length and diameter, the size of the medullary cavity also increases, keeping the bone from becoming very heavy. • In addition, as the bone grows in diameter, the relative thickness of compact bone is maintained as osteoclasts remove bone on the inside and osteoblasts add bone to the outside CALCIUM HOMEOSTASIS • BONE IS THE MAJOR STORAGE SITE FOR CALCIUM IN THE BODY, AND MOVEMENT OF CA2+ INTO AND OUT OF BONE HELPS DETERMINE BLOOD CA2+ LEVELS. • HORMONES ASSOCIATED IN CALCIUM HOMEOSTASIS A. PTH( PARATHYROID HORMONE)- RELEASE FROM PARATHYROID GLAND WHEN LOW BLOOD CALCIUM LEVELS (HYPOCALCEMIA). IT STIMULATES OSTEOCLAST BONE RESORPTION ACTIVITY. B. CALCITONIN- RELEASE FROM THYROID GLAND WHEN HIGH BLOOD CALCIUM LEVELS(HYPERCALCEMIA). IT INHIBITS OSTEOCLAST FROM FURTHER BONE RESORPTION. OPEN FRACTURE (COMPOUND FRACTURE) Occurs when an open wound extends to the site of the fracture or when a fragment of bone protrudes through the skin CLOSED FRACTURE( SIMPLE FRACTURE) Fractured bones does not perforate the skin. INCOMPLETE FRACTURE An incomplete fracture does not extend completely across the bone, COMPLETE FRACTURE Complete fracture the bone is broken into at least two fragments GREENSTICK FRACTURE An incomplete fracture on the convex side of the curve of the bone. HAIRLINE OR STRESS FRACTURE Incomplete fractures in which the two sections of bone do not separate there is only a small crack on the bone. COMMINUTED FRACTURE Is a complete fracture in which the bone breaks into more than two pieces—usually two major fragments and a smaller fragment. IMPACTED FRACTURE One fragment is driven into the spongy portion of the other fragment. FRACTURES ARE ALSO CLASSIFIED ACCORDING TO THE DIRECTION OF THE FRACTURE WITHIN THE BONE Linear Fracture Linear fractures run parallel to the long axis of the bone FRACTURES ARE ALSO CLASSIFIED ACCORDING TO THE DIRECTION OF THE FRACTURE WITHIN THE BONE Transverse Fracture transverse fractures are at right angles to the long axis FRACTURES ARE ALSO CLASSIFIED ACCORDING TO THE DIRECTION OF THE FRACTURE WITHIN THE BONE Spiral Fracture Spiral fractures take a helical course around the bone Oblique FRACTURES ARE ALSO CLASSIFIED ACCORDING TO THE DIRECTION OF THE Fracture FRACTURE WITHIN THE BONE Spiral fractures take a helical course around the bone FRACTURES ARE ALSO CLASSIFIED ACCORDING TO THE DIRECTION OF THE FRACTURE WITHIN THE BONE Dentate Fracture Dentate fractures have rough, toothed, broken ends. FRACTURES ARE ALSO CLASSIFIED ACCORDING TO THE DIRECTION OF THE FRACTURE WITHIN THE BONE Stellate Fracture Stellate fractures have breakage lines radiating from a central point EFFECTS OF AGING TO SKELETAL SYSTEM • THE MOST SIGNIFICANT AGE-RELATED CHANGES IN THE SKELETAL SYSTEM AFFECT THE QUALITY AND QUANTITY OF BONE MATRIX. • ORGANIC MATERIALS IN THE MATRIX REDUCES AND BONES BECOME BRITTLE. • BONE MASS IS AT ITS HIGHEST AROUND AGE 30, AND MEN GENERALLY HAVE DENSER BONES THAN WOMEN BECAUSE OF THE EFFECTS OF TESTOSTERONE AND GREATER BODY WEIGHT. • A SLOW LOSS OF COMPACT BONE BEGINS ABOUT AGE 40 AND INCREASES AFTER AGE 45 EFFECTS OF AGING TO SKELETAL SYSTEM • The most effective preventive measure against the effects of aging on the skeletal system is the combination of increasing physical activity and taking dietary calcium and vitamin D supplements. Intensive exercise, especially weight-bearing exercise, can even reverse the loss of bone matrix. DISEASES ASSOCIATED WITH SKELETAL SYSTEM REFERENCES • Cinnamon Vanputte et al., Seeley’s Anatomy and Physiology 10th Edition • Scanlon Valerie et al., Essentials of Anatomy and Physiology Fifth Edition