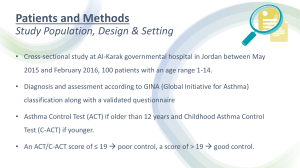
Asthma General Objective: After 1 hour of varied teaching-learning strategies, the BSN III students will be able to gain knowledge, develop skills and acquire positive attitude towards care of patients with asthma. Specifically, they will be able to: 1. define asthma. 2. identify the predisposing factors of asthma. 3. trace the pathophysiology of asthma. 4. identify the clinical manifestations of asthma. 5. discuss the assessment and diagnostic findings in asthma. 6. discuss the preventive measures of asthma. 7. identify the complications of asthma. 8. discuss the medical management of asthma. 9. appreciate the role of the nurse in caring for patients with asthma. Reader’s Theater: Will, Age 9 In your notebook… Note for significant data: ⚫ Predisposing/ contributing factors ⚫ History ⚫ Manifestations ⚫ Management Validate your notes’ accuracy as the discussion is going on. causes: 1. airway hyperresponsiveness 2. mucus production 3. mucosal edema Chemical mediators of inflammation allergy Common allergens: Seasonal: grass, tree, & weed pollens Perennial allergens: Molds Dust mite Animal Dander air pollutants, weather changes, hot, cod, strong odors, smoke, food (seafood, nuts), exercise, medications, stress, hormonal factors flu dust, fumes and vapors potent anti-inflammatory E.g. Symbicort SGA/ preterm allergic reactions Normal: 0.004% of the total Ig antibodies e.g. omalizumab bind Eosinophils Normal: 5% prevent the binding of IgE to the receptors of the receptors of Basophils basophils and mast cells block mast cell degranulation Chemical Mediators of Inflammation Slow-Reacting Substance of Anaphylaxis potent bronchoconstrictors Bronchoconstriction Inflammation - mucosal edema Mucus secretion e.g. montelukast Fluid leak from the vasculature (Singulair) Increased blood flow O2 sat decreased I PCO2 = acidosis O2 in blood block the effect of parasympathetic response (bronchoconstriction & e.g. aminophylline Cough theophylline If productive cough: -curschman spirals - epithelial and mucus cast -charcot-leydin crystals - broke down segments of eosinophils mucus production) Bronchodilation ABG - Arterial Blood Gas - acidosis or alkalosis pH (acid) 7.35 - 7.45 (alka) PCO2 35 - 45 mm Hg acid I CO2 = I acids = acidosis airway obstruction: asthma, COPD PCO2 - Partial pressure of CO2 FEV1 Forced Expiratory Volume in 1 sec HCO3 (bicarbonate) 22-26 mEq/L FVC Forced Vital Capacity O2 Saturation = 95% and up Normal at least 80% Marked respiratory effort: or methacholine challenge test(<20% = Asthma) - nasal flaring Pulmonary Function Test -use of accessory muscles - pursed-lip breathing - cyanosis (late) -acute, severe form of asthma; life-threatening If untreated: Respiratory or Cardiac Arrest Management: IV steroids; frequent administration of inhaled beta adrenergic agents (to prevent intubation & mechanical ventilation) - inflammation of the lung parenchyma lung collapse ASSESSMENT ⚫ Complete family, environmental, and occupational history ⚫ Comorbid conditions PREVENTION ⚫ Avoid causative agents: dust mites, roaches, pollens, molds ⚫ Client education MEDICAL MANAGEMENT Pharmacologic therapy 1. quick-relief medications 2. long-acting medications / short-acting ⚫ Route of choice: metered dose inhaler (MDI) p METERED-DOSE INHALER ⚫ pressurized device containing an aerosolized powder of medication Diskus Peak Flow Monitoring ⚫ Measures the highest airflow during a forced expiration ⚫ Daily monitoring ⚫ “personal best” is determined ⚫ ⚫ ⚫ Green zone: 80-100% of personal best Yellow zone: 60-80% Red zone: <60% Peak Flow Meter PHARMACOLOGIC THERAPY A. Quick-relief medications 1. Short-acting beta2-adrenergic agonist (SABA) ⚫ ⚫ Medication of choice for relief of acute symptoms & prevention of exercise-induced asthma Relaxes smooth muscle Ex: ⚫ Albuterol (Ventolin) ⚫ Levalbuterol (xopenex) ⚫ Pirbuterol (Maxair) 2. Anticholinergics inhibit muscarinic cholinergic receptors and reduce intrinsic vagal tone of the airway ⚫ For patients who cannot tolerate beta adrenergics agonists Ex: ipratropium bromide [Atrovent] ⚫ B. Long-acting: maintain control of persistent asthma ⚫ Corticosteroids ⚫ Most potent & effective anti-inflammatory ⚫ Use spacer and rinse mouth to prevent oral thrush IV⚫ Systemic form: to gain rapid control, manage severe asthma/ exacerbations, prevent recurrence 2. Mast cell stabilizer ⚫ Ex: Cromolyn sodium (Intal) nedocromil (Tilade) ⚫ Mild-moderate anti-inflammatory agent ⚫ Preventive treatment prior to exposure to exercise or known allergen ⚫ C/I in acute asthma exacerbations 3. Long-acting beta2-adrenergic agonists ⚫ For long-term control of asthma symptoms (esp. occurring at night) ⚫ Effective for prevention of exercise-induced asthma ⚫ Ex: salmeterol (serevent) formoterol (Foradil) 4. Methylxanthines ⚫ Ex: theophylline [Slo-bid, Theo-Dur] aminophylline ⚫ ⚫ Mild- moderate bronchodilators For relief of night-time asthma symptoms 5. Leukotriene modifier (inhibitors) ⚫ ⚫ Dilate blood vessels and alter permeability Ex: montelukast (Singulair) zileuton (Zyflo) 6. Immunomodulators ⚫ Prevent binding of IgE to the receptors of basophils and mast cells ⚫ Ex: omalizumab (Xolair) NURSING MANAGEMENT Assessment ⚫ Use calm approach ⚫ Assess for airway distress ⚫ History of allergic reactions to medications ⚫ Assess respiratory status: severity of symptoms, breath sounds, peak flow, pulse oximetry, vital signs ⚫ Current medication use ⚫ Fluid status insensible fluid loss is increased ==> dehydration ⚫ Ability to manage asthma & general adaptation ⚫ Presence of triggers Nursing Diagnoses, Outcomes & Interventions 1. Ineffective Airway Clearance related to production of mucus and spasm of the airway Goal: Establish an effective airway clearance as a. decreased abnormal breath sounds b. decreasing dry, non-productive cough ✔ ✔ ✔ ✔ ✔ ✔ ✔ evidenced by: Suctioning (for compromised airway) Assist in coughing effectively Encourage oral fluids to thin secretions Chest physiotherapy Expectorants Mucolytics first as prescribed before giving expectorants Frequent position changes Oral care every 2-4 hours to remove the taste of secretions 2. Ineffective Breathing Pattern related to airway spasm and edema Goal: Improved breathing patterns as evidenced by: a. RR with normal limits b. decreased dyspnea, less nasal flaring, and reduced use of accessory muscles c. decreased signs of anxiety d. a return of ABG levels to normal limits e. O2 saturation greater than 95% ✔ Assess frequently, observe RR & depth ✔ Assess: shortness of breath, pursed-lip breathing, nasal flaring, sternal and intercostal retractions, or prolonged expiratory phase ✔ Place on Fowler’s position to facilitate maximum lung expansion ✔ O2 as ordered ✔ Monitor ABG and O2 saturation levels 3. Impaired Gas Exchange related to trapped air in the alveoli and imbalance in O2 and CO2 Goal: Establish an adequate gas exchange as evidenced by: a. decreased abnormal breath sounds b. ABG levels within normal limits c. usual skin color d. decreasing dry, non-productive cough ✔ ✔ ✔ ✔ to help evaluate if there is adequate gas exchange Assess lung sounds every hour (acute episodes) Assess skin and mucous membranes for cyanosis Monitor pulse oximetry O2 as ordered 4. Anxiety 5. Activity Intolerance 6. Altered nutrition: Less than body requirements 7. Sleep Pattern Disturbance END ONE-SENTENCE SUMMARY In your notebooks, write a single sentence that sums up what should essentially be remembered about asthma. You have two (2) minutes to do this. 1. Pulmonary Function Tests (PFT) ⚫ include measurements of lung volumes, ventilatory function, and the mechanics of breathing, diffusion, and gas exchange ⚫ Spirometer – a volume-collecting device attached to a recorder that demonstrates volume and time simultaneously 2. Arterial Blood Gas Studies ⚫ Assesses ability of lungs to provide adequate oxygen and remove carbon dioxide and the ability of the kidneys to reabsorb or excrete bicarbonate ions to maintain normal body pH ⚫ pH ⚫ PaO2 ⚫ PaCO2 ⚫ HCO3 3. Pulse Oximetry ⚫ Continuous monitoring of the oxygen saturation of hemoglobin (SaO2), referred to as SpO2 ⚫ N = 95% - 100% ⚫ Less than 85% - indicate that the tissues are not receiving enough oxygen ⚫ Unreliable in states of low perfusion, hypothermia, nail polish 4. Cultures ⚫ Throat culture ⚫ Nasal swab 5. Sputum studies ⚫ To assess for pathogenic organisms, assess for hypersensitivity states, immunosuppressive medications ⚫ Early morning specimen - expectoration