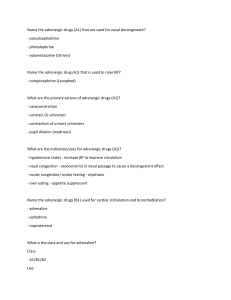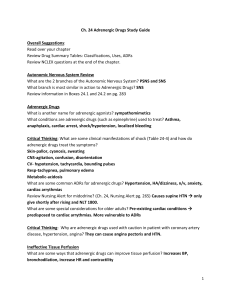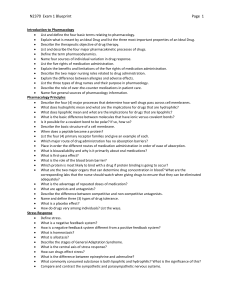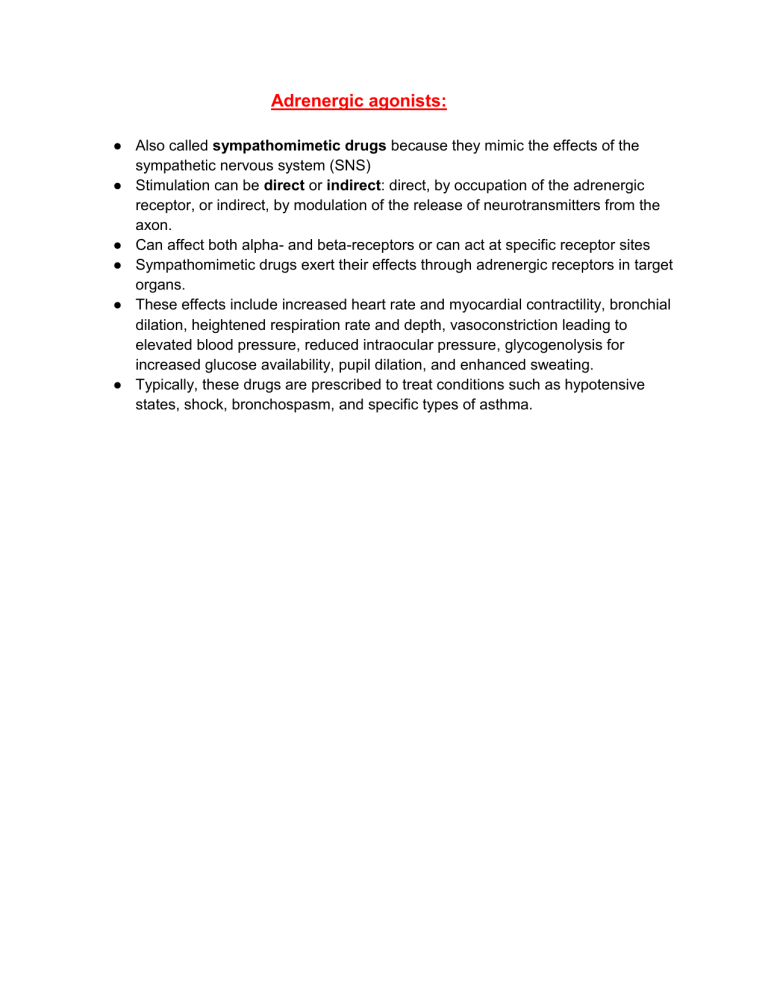
Adrenergic agonists: ● Also called sympathomimetic drugs because they mimic the effects of the sympathetic nervous system (SNS) ● Stimulation can be direct or indirect: direct, by occupation of the adrenergic receptor, or indirect, by modulation of the release of neurotransmitters from the axon. ● Can affect both alpha- and beta-receptors or can act at specific receptor sites ● Sympathomimetic drugs exert their effects through adrenergic receptors in target organs. ● These effects include increased heart rate and myocardial contractility, bronchial dilation, heightened respiration rate and depth, vasoconstriction leading to elevated blood pressure, reduced intraocular pressure, glycogenolysis for increased glucose availability, pupil dilation, and enhanced sweating. ● Typically, these drugs are prescribed to treat conditions such as hypotensive states, shock, bronchospasm, and specific types of asthma. Pharmacokinetics: ● These drugs are absorbed quickly through injection or mucous membranes. ● Metabolism of these drugs occurs in the liver. ● Excretion of these drugs happens through urine. ● In emergency situations, they are administered intravenously (IV) for a rapid onset of action. Contraindications and Cautions: ● ● ● ● ● Known hypersensitivity Pheochromocytoma Tachyarrhythmias or ventricular fibrillation Hypovolemia Halogenated hydrocarbon general anesthetics Adverse Effects: ● ● ● ● ● ● Adverse effects of alpha- and beta-adrenergic agonists are often linked to their impact on the sympathetic nervous system (SNS). Effects on the heart and cardiovascular system can result in arrhythmias, hypertension, palpitations, angina, and dyspnea. Depressant effects on the gastrointestinal (GI) tract may lead to nausea, vomiting, and constipation. Sympathetic stimulation can cause headaches, sweating, tension or anxiety, and piloerection (hair standing on end). Hypokalemia may occur due to aldosterone release with sympathetic stimulation, leading to potassium loss and muscle cramps. Vasoconstriction caused by these drugs necessitates caution to prevent extravasation, which can lead to tissue necrosis and cell death in the affected area. Alpha- and Beta-Adrenergic Agonists drug-drug interactions: ● Tricyclic antidepressants and MAOIs- Increased norepinephrine levels or receptor stimulation occur with these drugs. ● Other drugs that cause hypertension ● Adrenergic antagonists ● Halogenated hydrocarbon general anesthetics Alpha Agonist or Alpha- Selective Agonist: ● Drugs that specifically stimulates the alpha-receptors within the sympathetic nervous system, causing body responses seen when the alpha-receptors are stimulated Pharmacokinetics: ● These drugs exhibit excellent absorption regardless of the route of administration. ● IV and immediate-release oral formulations act rapidly, achieving peak levels quickly. ● They distribute widely throughout the body, undergo liver metabolism, and are mainly excreted via urine. ● Transdermal clonidine offers prolonged effects, lasting up to 7 days, requiring weekly replacement. ● Phenylephrine is versatile, administered intramuscularly (IM), subcutaneously, IV, orally, as well as in nasal or ophthalmic solutions. Contraindications and Cautions: ● ● Alpha-selective adrenergic agonists should be avoided in case of drug allergies, severe hypertension, or narrow-angle glaucoma. Alpha2-selective medications are not suitable for patients with hypotension or bradycardia. ● ● Limited data exists regarding pregnancy and lactation, so use should be carefully considered based on the risk-benefit assessment. Caution should be exercised in patients with cardiovascular disease, vasomotor spasm, thyrotoxicosis, diabetes, or renal/hepatic impairment due to potential exacerbation of these conditions and drug metabolism/excretion issues. Adverse Effects: ● ● ● ● ● ● ● ● Patients on these drugs often experience adverse effects due to sympathetic stimulation. CNS effects: anxiety, restlessness, depression, fatigue, strange dreams, and personality changes. Blurred vision and light sensitivity result from sympathetic-induced pupil dilation. CV effects: may involve arrhythmias, ECG changes, blood pressure fluctuations, and peripheral vascular issues. Nausea, vomiting, and anorexia can occur due to the SNS's inhibitory effects on the GI tract. GU effects: encompass reduced urinary output, urination difficulties, dysuria, and sexual function changes due to sympathetic stimulation. Avoid abrupt discontinuation as adrenergic receptors remain sensitive, potentially causing tachycardia, hypertension, arrhythmias, flushing, or death. Taper the drug over 2 to 4 days when discontinuing, if possible. When administering phenylephrine IV, take care to prevent extravasation, which can lead to necrosis and cell death in the affected area. Beta Agonist or Beta- Selective Agonist: ● ● ● Used to manage and treat bronchial spasm, asthma, and other obstructive pulmonary conditions Related to stimulation of the beta-adrenergic receptors Desired effects: increased heart rate, conductivity, and contractility; bronchodilation; increased blood flow to skeletal muscles and splanchnic beds; relaxation of uterus Pharmacokinetics: ● Isoproterenol is rapidly distributed after injection; it is metabolized in the liver and excreted in the urine. The half-life is relatively short—less than 1 hour. Contraindications and Cautions: ● ● Isoproterenol is contraindicated in cases of drug or component allergies to prevent hypersensitivity reactions. Avoid its use in pulmonary hypertension, tachyarrhythmias, digitalis intoxication-induced heart block, and angina pectoris due to potential worsening of clinical conditions. ● ● ● ● Do not administer during anesthesia with halogenated hydrocarbons, eclampsia, uterine hemorrhage, or intrauterine death, as it could complicate these situations. Exercise caution in patients with diabetes, thyroid disease, vasomotor problems, degenerative heart disease, or a history of stroke due to potential exacerbation by sympathomimetic effects. Use with care in cases of severe renal impairment, which could affect drug excretion. Avoid its use during pregnancy and lactation due to potential effects on the fetus or neonate. Adverse Effects: ● ● ● ● ● ● ● Drugs: Adverse effects of isoproterenol stem from sympathetic adrenergic receptor stimulation. CNS effects: restlessness, anxiety, fear, tremor, fatigue, and headache. CV effects: tachycardia, angina, myocardial infarction, and palpitations. Pulmonary effects: difficulty breathing, coughing, bronchospasm, and severe pulmonary edema. GI upset: nausea, vomiting, anorexia due to GI tract slowdown with SNS stimulation. Hypokalemia results from aldosterone release with sympathetic stimulation, leading to potassium loss. Other effects: sweating, pupil dilation, rash, and muscle cramps due to potassium shift. Adrenergic Antagonists or Adrenergic blocking agents: ● Adrenergic antagonists, or sympatholytic drugs, block the effects of the Sympathetic Nervous System (SNS). ● Their therapeutic and adverse effects are linked to their specificity for adrenergic receptor sites. ● They interact with adrenergic receptors without activation, preventing typical SNS effects. ● By occupying adrenergic receptor sites, they block norepinephrine's activation of these receptors, thereby inhibiting SNS manifestations. Nonselective Adrenergic Blocking Agents: ● Block both alpha- and beta-adrenergic receptors ● Primarily used to treat cardiac-related conditions ● Adrenergic blocking agents competitively block alpha- and beta-receptors in the Sympathetic Nervous System (SNS), resulting in: ● Lower blood pressure via reduced alpha-receptor-mediated vasoconstriction. ● Slower pulse rate by inhibiting beta-receptor activation that increases heart rate. ● Improved renal perfusion, enhancing blood flow to the kidneys. ● Reduced renin levels, aiding blood pressure regulation by decreasing renin's vasoconstrictive effects. ● These drugs exhibit good oral absorption and widespread distribution when administered orally or intravenously. ● Metabolism primarily occurs in the liver, and elimination takes place through feces and urine. ● Adrenergic blocking drugs have variable half-lives depending on the specific drug and its formulation. Adverse effects of nonselective adrenergic blocking agents/cautions: Cautions: ● Diabetes, asthma, pregnancy Adverse effects: ● Usually associated with effects on SNS ● GI effects- such as vomiting ● CV effects- cardiac arrhythmias, hypotension, heart failure (HF), pulmonary edema, and stroke are associated with the lack of stimulatory effects and vascular tone loss in the CV system. ● Respiratory effects- bronchospasm, cough, rhinitis, and bronchial obstruction, ● Other effects ● CNS- dizziness, paresthesia, insomnia, depression, fatigue, and vertigo due to blocking norepinephrine's CNS effects. Nonselective Alpha-Adrenergic Blocking Agents: Phentolamine: Only nonselective alpha-adrenergic blocking agent ● Phentolamine prevents tissue damage from extravasation of IV norepinephrine or dopamine. ● It manages severe hypertension reactions during manipulation of pheochromocytoma before and during surgery. ● Aids in diagnosing pheochromocytoma, a tumor producing excessive catecholamines. ● It reverses soft tissue anesthesia, such as in Oraverse, by counteracting local anesthetic effects to restore normal sensation. Pharmacokinetics: ● Rapidly absorbed after injection ● Excreted in the urine Contraindications: ● Allergy ● CAD or MI Caution: ● Pregnancy or lactation Adverse Effects: ● Patients on phentolamine may experience extensions of therapeutic effects, including: ● Hypotension ● Orthostatic hypotension ● Angina ● Myocardial infarction (MI) ● Cerebrovascular accident ● Flushing ● Tachycardia ● Arrhythmia ● These effects result from vasodilation and reduced blood pressure. ● Common side effects include headache, weakness, dizziness (due to hypotension), and potential nausea, vomiting, and diarrhea. Alpha1-Selective Adrenergic Blocking Agents: ● Drugs that have a specific affinity for alpha1-receptors ● Well absorbed after oral administration and undergo extensive hepatic metabolism and excreted in urine Contraindications/ Caution: ● Alpha1-selective adrenergic blocking agents are contraindicated in cases of drug allergies to prevent hypersensitivity reactions. ● Avoid use during lactation as these drugs can cross into breast milk, potentially affecting the neonate. ● Exercise caution in patients with heart failure (HF) or renal failure, as these drugs can exacerbate their conditions by lowering blood pressure. ● Hepatic impairment may affect drug metabolism, requiring cautious use. ● Be cautious during pregnancy due to the potential for adverse effects on the fetus. Adverse Effects: ● Adverse effects of these drugs are primarily linked to their blockage of the Sympathetic Nervous System (SNS). ● Central Nervous System (CNS) side effects encompass headache, dizziness, weakness, fatigue, drowsiness, and depression. ● Gastrointestinal (GI) symptoms like nausea, vomiting, abdominal pain, and diarrhea may occur due to direct effects on the GI tract and sympathetic blocking. ● Expected Cardiovascular (CV) effects include arrhythmias, hypotension, edema, heart failure (HF), and angina. ● Vasodilation caused by these drugs can lead to flushing, rhinitis, reddened eyes, nasal congestion, retrograde ejaculation, and priapism. Nonselective Beta-Adrenergic Blocking Agents: ● Used to treat migraine headaches and CV problems (hypertension, angina) and to prevent reinfarction after MI. Drugs: ● Carteolol (generic) ● Levobunolol (Akbeta, Betagan) ● Nadolol (Corgard) ● Nebivolol (Bystolic) Propranolol- variety of uses that range from prophylaxis of migraine headaches to treatment of arrhythmias. Sotalol (Betapace, Betapace AF, Sorine, Sotylize) Timolol (Betamol, Istalol, Timolol Maleate, Timoptic) Adverse Effects: ● Patients on these drugs often experience adverse effects related to beta-receptor blockage in the Sympathetic Nervous System (SNS). ● CNS effects encompass headache, fatigue, dizziness, depression, paresthesia, sleep disturbances, memory loss, and disorientation. ● CV effects may include bradycardia, heart block, heart failure (HF), hypotension, and peripheral vascular insufficiency. ● Pulmonary effects range from breathing difficulties, coughing, and bronchospasm to severe pulmonary edema and bronchial obstruction. ● GI upset, nausea, vomiting, diarrhea, gastric pain, and colitis can occur due to unchecked parasympathetic activity and sympathetic receptor blockage. ● Genitourinary (GU) effects may involve decreased libido, impotence, dysuria, and Peyronie's disease. ● Other possible effects include reduced exercise tolerance, hypoglycemia or hyperglycemia, and liver changes. ● Abrupt cessation of these drugs after long-term use can lead to angina, myocardial infarction (MI), hypertension, and stroke due to heightened catecholamine sensitivity after receptor blockage. Contraindications/ Caution: ● Nonselective beta-adrenergic blocking agents are contraindicated in cases of drug or component allergies to prevent hypersensitivity reactions. ● Avoid use with bradycardia, heart blocks, shock, or heart failure (HF) as these drugs can exacerbate cardiac suppression. ● Contraindicated in cases of bronchospasm or acute asthma due to potential worsening from sympathetic bronchodilation blockage. ● Avoid during pregnancy due to potential teratogenic effects and neonatal risks; also avoid during lactation due to potential neonatal effects. ● Use cautiously in diabetes and hypoglycemia patients, as these drugs can mask signs and symptoms. ● Be cautious in patients with chronic obstructive pulmonary disease (COPD) and asthma, which may worsen due to blocked sympathetic bronchodilation. ● Use with care in patients with renal or hepatic dysfunction, as it may interfere with drug excretion and metabolism. Beta1-Selective Adrenergic Blocking Agents: ● Preferred for patients who smoke or who have asthma ● At lower doses it doesn't usually block beta receptor sites; they do not block sympathetic bronchodilation that is important for patients with lung diseases or allergic rhinitis. ● Also treats hypertension, angina, and some cardiac arrhythmias. ● The therapeutic effects of these drugs stem from their selective blocking of beta1-receptors in the Sympathetic Nervous System (SNS) at therapeutic doses. ● They do not block beta2-receptors, preserving sympathetic bronchodilation, but this selectivity diminishes with higher doses. ● Blockade of beta1-receptors in the heart and juxtaglomerular apparatus contributes to therapeutic benefits. ● Actions include reduced heart rate, contractility, excitability, and a membranestabilizing effect, resulting in decreased arrhythmias, cardiac workload, and oxygen consumption. ● Inhibition of renin release from juxtaglomerular cells further lowers blood pressure. ● These drugs are used to treat cardiac arrhythmias, hypertension, chronic angina, and can help prevent reinfarction post-MI by reducing cardiac workload and oxygen consumption. Contraindications/ Caution: ● Beta1-selective adrenergic blockers are contraindicated in cases of drug or component allergies to prevent hypersensitivity reactions. ● Avoid use with sinus bradycardia, heart block, cardiogenic shock, heart failure requiring inotropic support, or hypotension, as these conditions can worsen due to cardiac depression and blood pressure lowering. ● Contraindicated during lactation due to potential adverse neonatal effects. ● Exercise caution in patients with diabetes, thyroid disease, or chronic obstructive pulmonary disease (COPD) due to potential adverse effects on these conditions with sympathetic blockade. ● Be cautious in pregnancy due to potential adverse effects on the fetus. ● Safety and efficacy in children have not been established. Adverse Effects: ● Patients on these drugs may experience adverse effects stemming from beta1receptor blockade in the Sympathetic Nervous System (SNS). ● CNS effects include headache, fatigue, dizziness, depression, paresthesia, sleep disturbances, memory loss, and disorientation. ● CV effects may involve bradycardia, heart block, heart failure (HF), hypotension, and peripheral vascular insufficiency. ● Pulmonary effects range from rhinitis to bronchospasm and dyspnea, although they are less likely than with nonselective beta-blockers. ● GI upset, including nausea, vomiting, diarrhea, gastric pain, and colitis, can occur due to unchecked parasympathetic activity and sympathetic receptor blockade. ● GU effects may encompass decreased libido, impotence, dysuria, and Peyronie's disease. ● Other potential effects include reduced exercise tolerance, hypoglycemia or hyperglycemia, and liver changes reflected in increased liver enzyme concentrations. ● Abrupt cessation of these drugs after long-term use can lead to severe hypertension, angina, myocardial infarction (MI), and stroke due to heightened catecholamine sensitivity after receptor blockage.