Secondary Hemostasis Lecture: Coagulation & Fibrinolysis
advertisement

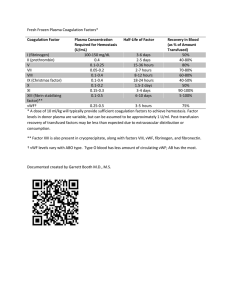
LECTURE 2 SECONDARY HEMOSTASIS Jahan Abdi | Clinical Science | Summer/Fall 2023 OVERVIEW • Coagulation proteins: synthesis, characteristics, clinical significance • • • • • • Coagulation cascade: proposed models Regulation of coagulation cascade Fibrinolysis: components and regulation Coagulation disorders Lab diagnosis and clinical correlation Case studies COAGULATION FACTORS: TERMINOLOGY/NOMENCLATURE • 8 factors (“F” for factor) are zymogens (circulating in plasma in an inactive form) • FII (prothrombin) • FVII (stable factor or proconvertin) • FIX (plasma thromboplastin component, Christmas factor) • FX (Stuart-Prower factor) • FXI (plasma thromboplastin antecedent) • FXII (Hageman factor) • FXIII (plasma transglutaminase, fibrin-stabilizing factor) • Prekalikrein () • All are serine proteases except FXIII COAGULATION FACTORS: TERMINOLOGY/NOMENCLATURE • 7 proteins are co-factors (stabilize and accelerate proteolytic reactions) • High molecular weight kininogen (HMWK, Fitzgerald) (co-factor for FXIIa and PK) • Tissue factor (FIII, tissue thromboplastin) (co-factor for FVIIa) • FV (labile factor, proaccelerin) (co-factor for FXa) • FVIII (labile factor, AHF A) (co-factor for FIXa) • Protein S (co-factor for activated protein C) • Thrombomodulin (co-factor for thrombin in protein C activation) • Protein Z (co-factor for protein Z-dependent protease inhibitor, ZPI) COAGULATION FACTORS: TERMINOLOGY/NOMENCLATURE/CLASSIFICATION • Regulatory proteins (inhibitors) • • • • Anti-thrombin Protein C Heparin co-factor II TFPI (tissue factor pathway inhibitor) Other coag factors: FI (fibrinogen), vWF, Ca+ (FIV), phospholipids (PF3) • • Suffix “a” after the factor indicates “active or activated”: e.g., VIIa, XIIa • Roman numerals are based on order of discovery or description of factors • We usually call factor I fibrinogen and factor II prothrombin • PK and HMWK never received a Roman numeral • Almost all coag factors are synthesized by liver except vWF which is made by ECs (stored in Weibel-Palade granules) or MKs (stored in PLT alpha granules) FUNCTION OF COAGULATION PROTEINS • Almost all coag factors are synthesized by liver except vWF which is made by ECs (stored in Weibel-Palade granules) and MKs (stored in PLT alpha granules) • vWF: heaviest cog factor (500 - 20000 kd) • VII: shortest half-life (3-6h), and HMWK the longest • VIII: is carried in plasma as bound to vWF to maintain 12 h halflife • Ionized calcium is crucial for coagulation complexes to bind to platelet or cell membrane phospholipids: FUNCTION OF COAGULATION PROTEINS • Coagulation proteins act on each other in a cascade reaction • Each factor (serine protease) activates the next, and this continues… • The outcome is conversion of fibrinogen (ultimate substrate) into stable fibrin clot FUNCTION OF COAGULATION PROTEINS • Vitamin K-dependent coag proteins • SCZ27910 (aka called prothrombin group) • They require vit K to become γcarboxylated (hence functional) • All have 10-12 glutamic acid residues at N terminal • Prothrombin group are important for assembly of coagulation complexes to generate thrombin COAGULATION COMPLEXES • Complex 1: extrinsic tenase • Tissue factor+VIIa +Ca2++ phospholipid • Activates X to Xa, and IX to IXa • Complex 2: intrinsic tenase • IXa+VIIIa+phospholipid (PLT surface)+Ca2+ • Activates X to Xa • Complex 3: prothrombinase • Xa+Va+phospholipid+Ca2+ • Activates prothrombin to thrombin FACTOR VIII AND VON WILLEBRAND FACTOR • • • • • • • • FVIII and vWF are the KEY factors in coagulation (severe bleeding in hemophilia A and vWD) FVIII and FIX are encoded by genes on X chromosome FVIII is degraded in stored plasma faster than other factors FVIII bounds to and carried by vWF in plasma vWF is multimeric, subunits of 240kd polymerized to 500-2000kd in MK and Ecs, degraded to smaller mulitmers by ADAMTS13 (a disintegrin and metalloprotease with a thrombospondin type 1 motif, member 13), in blood vessels with higher shear rate vWF has receptors for PLTs and collagen (bridges PLTs to subendothelium during PLT adhesion) vWF level is associated with ABO groups, O group has lower level vWF and FVIII are acute phase reactants (APR) FACTOR XI AND THE CONTACT SYSTEM • FXII, PK, HMWK constitute the contact system (contact factors, contact factor complex) • Contact system is the basis of the aPTT test • FXII is activated by negatively charged surfaces, FXIIa converts PK (bound to HMWK) to K, K further activates FXII • Contact factor complex (HMWK+PK+FXIIa) activates FXI (in turn activates FIX) • The most important activator of FXI is thrombin generated by the extrinsic tenase • Deficiencies of the contact system factors do not cause bleeding BUT do prolong aPTT THROMBIN, FIBRINOGEN, FIBRIN CLOT, FXIII • Thrombin • Key serine protease in coagulation with multiple functions • Major function: cleaving fibrinopeptides A and B (FPA and FPB) from fibrinogen, triggering spontaneous polymerization, clot initiation • Thrombin activates FV, FVIII and FXI (positive feedback) • Thrombin bound to ………….. activates protein C • Thrombin triggers ……….. of PLTs • Thrombin activates TAFI (thrombin activatable fibrinolysis inhibitor) • Thrombin activates FXIII to stabilize the fibrin clot THROMBIN, FIBRINOGEN, FIBRIN CLOT, FXIII • Fibrinogen • • • • Primary substrate of thrombin RI in plasma 200-400mg/dL, an APR Essential for PLT………. through binding the ………. receptor PLTs absorb it and store in α granules • FXIII • Aka plasma transglutaminase • Deficiency does not affect PT or PTT but leads to clinical bleeding COAGULATION PATHWAYS: IN VITRO MODEL • Extrinsic pathway • • • TF:FVII primary initiator of in vivo coagulation Reaction order: VII, X, V, prothrombin, and fibrinogen Is assessed by prothrombin time (PT) test • Intrinsic pathway • • Reaction order: XII, pre-K, HMWK, XI, IX, VIII, X, V, prothrombin, and fibrinogen Is assessed by activated partial thromboplastin time (aPTT) test • Common pathway • • Includes X, V, prothrombin, and fibrinogen Both tests plus thrombin time (TT) COAGULATION PATHWAYS: IN VIVO MODEL • Initiation: • • • In vivo, extrinsic tenase complex is the main initiator of thrombin generation 1-2% FVIIa circulates but inert (requires TF) FVII:TF complex activates low level of FX and FIX, and small amount of thrombin (ignites more thrombin generation through positive feedback, max 3%) • Propagation: • • • >95% thrombin is generated Reactions are on PLT membrane Large PLT aggregates, intrinsic tenase activates FX 50-100 fold higher, prothrombinase complex generates burst of thrombin What is (are) missing in this model? REGULATION OF COAGULATION Name Tissue factor pathway inhibitor (TFPI) Thrombomodulin Protein C Protein S Antithrombin Heparin cofactor II Protein Z-dependent protease inhibitor Function With Xa, binds TF:VIIa EC surface receptor for thrombin Serine protease Cofactor Serpin Serpin Serpin Serpin: serine protease inhibitor FIBRINOLYSIS • Final stage of hemostatic activation (hours after) • Fibrinolytic proteins bind to fibrin as it is forming • • • • • Main substrate is plasminogen produced by the liver ECs secrete TPA (tissue plasminogen activator) and UPA (urokinase plasminogen activator), TPA is more effective TPA degrades fibrin-bound plasminogen to generate plasmin Plasmin degrades fibrin (and fibrinogen) into several fragments (X, Y, D, E, and D-D) D-D (D dimer) is fibrin-derived and a diagnostic test for thrombosis and fibrinolysis CONTROL OF FIBRINOLYSIS • Plasminogen activator inhibitor-1 (PAI-1) is the main inhibitor, binds to and inactivates TPA and UPA, it’s a serpin, produced mostly by ECs and MKs • α2-antiplasmin (α2-AP) produced by the liver, binds to and inactivates free plasmin (not plasmin bound to fibrin) • Thrombin activatable fibrinolysis inhibitor (TAFI) synthesized by the liver, activated by the thrombinthrombomodulin complex, blocks binding of TPA and plasminogen to fibrin and formation of plasmin BLEEDING DISORDERS AND LAB DIAGNOSIS Acquired • Trauma-induced: systemic shock leading to acute reduction in ADAMTS13, coag factor activation, TF release, and hyperfibrinolysis. • Liver disease: • Reduction in plasma level of SCZ27910 • At the beginning, FVII reduced (shortest half-life), PT is very sensitive to low FVII, so first PT is prolonged in mild liver disease, sensitive early maker • Vit K deficiency has the same effect on PT, FV level differentiates liver dx from vit K deficiency BLEEDING DISORDERS AND LAB DIAGNOSIS • Liver disease: • Thrombocytopenia due to high sequestration by enlarged spleen, abnormal PLT function (low aggregation in aggregometry) • DIC associated with liver dx due to low production of antithrombin or protein C and S, may be chronic compensated, or acute uncompensated • Acute DIC: prolonged PT, PTT, TT, low fibrinogen, increased D-dimer test • Chronic compensated DIC: only D-dimer is increased HEMOSTASIS LABORATORY TESTS IN LIVER DISEASE Assay Fibrinogen (FG) Thrombin time (TT) Reptilase time Prothrombin time (PT) Partial thromboplastin time (PTT) Factor V assay Platelet count Platelet aggregometry Quantitative D-dimer Interpretation >400 mg/dL (elevated) in early, mild liver disease; <200 mg/dL in moderate to severe liver disease, which causes dysfibrinogenemia and hypofibrinogenemia Prolonged in dysfibrinogenemia, hypofibrinogenemia, elevated fibrin degradation products, and unfractionated heparin therapy Prolonged in hypofibrinogenemia, significantly prolonged in dysfibrinogenemia; unaffected by heparin; assay rarely used Prolonged, even in mild liver disease, because of des-γ-carboxyl factors replacing normal factors II (prothrombin), VII, and X Mildly prolonged in severe liver disease because of disseminated intravascular coagulation (DIC) or des-γ-carboxyl factors II (prothrombin), IX, and X Factor V is reduced in liver disease but is unaffected by vitamin K deficiency, so the factor V level helps distinguish liver disease from vitamin K deficiency Mild thrombocytopenia, platelet count <150,000/μL Mild suppression of platelet aggregation and secretion in response to most agonists >240 ng/mL or >500 ng/mL fibrinogen equivalent units (FEUs) Reptilase time can sometimes be done instead of TT BLEEDING DISORDERS AND LAB DIAGNOSIS Acquired • Autoanti-factor VIII inhibitor and acquired hemophilia: • Some patients (older than 65) may develop an autoantibody against FVII which causes an “acquired hemophilia” condition (sudden bleeding into soft tissue or GI bleeding, …) • May develop in RA, IBD, SLE, or lymphoproliferative disease (e.g., CLL) • Could be fatal in 20% cases even if treated BLEEDING DISORDERS AND LAB DIAGNOSIS Laboratory investigation of FVIII inhibitors • PT, PTT, TT, for any patient experiencing sudden anatomic hemorrhage that mimics acquired hemophilia • PTT is prolonged but PT and TT are normal • FVIII level <40units/dL should be established by factor assay • Mixing studies to confirm presence of the inhibitor: • • • Patient’s plasma is mixed 1:1 with normal plasma (NP), prolonged PTT will be corrected initially but prolonged again after incubation in 370C, why?? If prolonged PTT remains prolonged even after 2h incubation, it indicates presence of lupus anticoagulants or patient is under heparin therapy 15% of inhibitors (called high avidity) immediately prolong the PTT’s mixture BLEEDING DISORDERS AND LAB DIAGNOSIS Congenital • vWD: • Autosomal dominant, affecting both sexes, females>males, qualitative or quantitative changes in vWF due to gene mutations • Most common inherited mucocutaneous bleeding disorder causing decreased PLT adhesion and impaired primary hemostasis • Severe quantitative vWF deficiency causes FVIII deficiency • In “low vWF” cases, vWF plasma level (30-50%) maintain sufficient FVIII BLEEDING DISORDERS AND LAB DIAGNOSIS Congenital • vWD types and subtypes: • • • • • • • Type 1: quantitative, 40-70% cases, mild to moderate Type 2: qualitative types Type 2A Type 2B Type 2M Type 2N Type 3: null phenotype, severe vWF deficiency, very low FVIII VWD LABORATORY DIAGNOSIS • Very helpful: history of mucocutaneous bleeding and decreased vWF concentration or activity (function) • CBC: to rule out thrombocytopenia • PT and PTT: to rule out factor deficiency other than vWF • Standard vWD test panel: • • • • • • vWF: Rco vWF: Ag VWF activity to VWF:Ag ratio RIPA FVIII activity vWF multimers VWD LABORATORY DIAGNOSIS Laboratory Test VWF:RCo Type 1 Subtype 2A Subtype 2B Subtype 2M Low Subtype 2N Type 3 Low Low Low Normal Normal to slightly decreased Decreased Normal Normal Very low or absent Very low or absent VWF:Ag Low Platelet count PTT Normal Normal to slightly decreased Normal Decreased Normal Normal Normal to slightly prolonged Decreased Slightly low Normal Normal Increased Normal Normal to slightly prolonged Normal Low Prolonged Decreased Normal Normal to slightly prolonged Decreased Normal Normal pattern Large and intermediate forms absent Large forms absent Normal pattern Normal pattern All forms absent (vWF activity) RIPA Factor VIII activity VWF multimers Absent <10 units/dL HEMOPHILIA A, B • Congenital, single-factor deficiencies • Marked by anatomic soft tissue bleeding • X-linked recessive (♂ have the disease, ♀are typically carriers) • Hemophilia A: FVIII deficiency (85% of patients) • Hemophilia B: FIX deficiency (14% of patients) • Hemophilia C: FXI deficiency (1% of patients) HEMOPHILIA A • FVIII protein translated from X chromosome • Various deletions, stop codons, nonsense and/or missense mutations result in quantitative deficiency of FVIII • FVIII deficiency significantly slows coagulation pathway production of Thrombin • Leads to bleeding • Clinical manifestations include: • • • • • Anatomic bleeds Deep muscle and joint hemorrhages Hematomas Wound oozing after trauma or surgery Bleeding into the central nervous system, peritoneum, gastrointestinal tract, and kidneys Results of Clot-Based Assays in Congenital Single-Factor Deficiencies Deficient Factor Fibrinogen Prothrombin V VII VIII IX X XI XIII PT Prolonged Prolonged Prolonged Prolonged Normal Normal Prolonged Normal Normal PTT Prolonged Prolonged Prolonged Normal Prolonged Prolonged Prolonged Prolonged Normal TT Prolonged Normal Normal Normal Normal Normal Normal Normal Normal Reflex Test Fibrinogen assay Prothrombin, V, VII, and X assays Prothrombin, V, VII, and X assays VII assay VIII, IX, and XI assays VIII, IX, and XI assays Prothrombin, V, VII, and X assays VIII, IX, and XI assays XIII quantitative assay What reflex tests do you suggest for a patient with normal PLT count and function, normal PT, PTT, TT tests, but with a bleeding history? LABORATORY INVESTIGATION OF BLEEDING Correction/Mixing Studies • • Mixing studies are performed on plasma used to distinguish factor deficiencies from factor inhibitors Therefore, to differentiate between: • Factor deficiencies (single or multiple) OR Specific Factor Antibodies or Inhibitors OR Non-specific Antibodies or Inhibitors Normal PT or APTT results require 50% of normal level of factors in circulation • Mixing studies help to determine the appropriate next steps to take in order to diagnose the cause of abnormal APTT and/or PT results PT and APTT 50:50 Mixing Studies Procedure: 1. Repeat PT and/or APTT using patient PPP 2. 3. 4. Run Normal Pooled Plasma alone • Ensure normal results or 100% of factor level Run patient PPP mixed 1:1 with NPP Compare results • Initial testing is compared to mix • Did mix correct? Did mix not correct? PT and APTT 50:50 Mixing Studies Interpretation: • If the time of the 1:1 mixture result is still ≥ 10% of the pooled normal plasma result (or outside the reference interval), no correction has occurred and a circulating inhibitor such as lupus anticoagulant is suspected • If the time of the 1:1 mixture result is within ≤ 10% of the pooled normal plasma result (or within reference intervals), a correction has occurred and a factor deficiency or specific factor antibody may be suspected as the cause for the cause of the originally prolonged test(s) Example: Patient plasma PT = 12s APTT = 49s (Normal) (Prolonged) Normal Pooled Plasma APTT = 27s (Normal) MIX APTT 1:1 (Patient:NPP) APTT = 30s (slightly more prolonged than NPP) • Patient’s plasma was “Corrected” by the NPP • NPP provided a factor that was lacking in the patient’s sample • “Correction” rules out a non-specific inhibitor • Could be an antibody to a factor (rule out by incubation) • Could be Factor deficiency • Further testing is then needed to identify the factor deficiency (Factor Assay) 5 M UREA SOLUBILITY TEST Principle: • Performed to specifically assess FXIII deficiency or inhibition • FXIII is insoluble in urea • In the absence of FXIII, fibrin clot will dissolve rapidly in presence of urea • Positive results should be confirmed by FXIII assay • Quantitative FXIII activity assay THROMBIN TIME (TT) • Commercially available bovine thrombin reagent transforms plasma fibrinogen to a detectable fibrin polymer • Thrombin reagent and patient’s plasma (100uL) are pre-warmed at 370C for 3 min • 200 uL of thrombin is added to patient’s plasma and chronometer is started, clot formation is recorded • RI: 15-20 s • TT is prolonged when there is hypofibrinogenemia (<100mg/dL) or afibrinogenemia or dysfibrinogenemia • TT may be replaced by Reptilase time test (SOP the same) PROTHROMBIN TIME (PT) Test Procedure 1. PT reagent is warmed to 37ºC 2. PPP aliquot is warmed to 37ºC for 3-10 min - Aliquots that are incubated longer than 10 minutes become prolonged o Coagulation factors begin to deteriorate or are affected by evaporation and pH change 3. A premeasured volume of reagent is added (speedily) to the plasma aliquot and a timer is started 4. As clot forms, timer stops, and elapsed time is recorded 5. Fibrin clot is detectable visually or by optical or electromechanical sensors PROTHROMBIN TIME (PT) & INR • Due to inherent variations in Thromboplastin reagents from lab to lab and in an effort to standardize inter-laboratory PT reporting, the International Normalized Ratio (INR) was developed • INR standardizes PT results and reporting, to allow for monitoring of Vitamin K antagonist therapy (such as, Coumadin/Warfarin) across different labs • INR is reported along with PT result PROTHROMBIN TIME (PT) • PT (in seconds) and ISI are used to calculate the INR ‒ISI = International Sensitivity Index • Commercial suppliers of Thromboplastin reagent preparations supply ISI with each reagent lot • ISI indicates how sensitive the reagent is to deficiencies in Vitamin K dependent factors compared to the WHO (World Health Organization) reference standard PROTHROMBIN TIME (PT) & INR ISI INR = Patient PT Mean Normal PT Mean Normal PT= The geometric mean normal PT is determined from at least 20 fresh plasma specimens obtained from healthy individuals PROTHROMBIN TIME (PT) & INR • Reference Intervals • Manual PT: 10.6 – 14.6 s • Automated PT: could be a bit different (e.g., 9.5 13.5 s) • INR: 0.9 - 1.2 • • • • Varies from lab to lab Must be re-established once a year Report PT in Seconds & calculate INR (manual) Automated analyzers automatically calculate INR ACTIVATED PARTIAL THROMBOPLASTIN TIME (APTT/PTT) APTT – clot-based routine coagulation test APTT is used to assess deficiencies or inhibitors of the factors in the intrinsic and common pathway: • Factors XII, XI, IX, VIII, X, V, II (prothrombin), I (fibrinogen) – all factors except FVII To monitor standard (unfractionated) Heparin anticoagulant therapy ACTIVATED PARTIAL THROMBOPLASTIN TIME (APTT/PTT) Test Procedure 1. Equal volumes of PPP and 1st reagent- contact activator + PL are combined and incubated for 3 minutes 2. 2nd reagent- CaCl2 is then added, the sample is mixed while kept at 37ºC, and then timing is started 3. Timing is stopped when first signs of a fibrin strands are seen 4. Fibrin clot is detectable visually or by optical or electromechanical sensors 5. RI: 25-35 s, could vary from lab to lab, must be established once a year NCS: can be silica, kaolin, ellagic acid, or celite COAGULATION SAMPLE COLLECTION Frequency of Errors Pre-analytical Analytical Post-analytical 68,2 13,3 18,5 The distribution of mistakes was: preanalytical 68.2%, analytical 13.3%, and postanalytical 18.5%. Most of the laboratory mistakes (74%) did not affect patients’ outcome. However, in 37 patients (19%), laboratory mistakes were associated with further inappropriate investigations, thus resulting in an unjustifiable increase in costs. Moreover, in 12 patients (6.4%) laboratory mistakes were associated with inappropriate care or inappropriate modification of therapy (Plebani and Carraro, Clinical Chemistry. 1997;43:8:1348 –1351). COAGULATION SAMPLE COLLECTION • • • • • • Acceptable anticoagulant: 3.2% buffered Sodium Citrate, Sodium Citrate leaves all clotting factors available except Calcium, Citrate binds the calcium in the plasma and therefore prevents coagulation, but not as strongly as EDTA Plasma (contains coagulation factors) is separated from platelets (phospholipid source) by centrifugation = PlateletPoor Plasma (PPP- platelet count <10x109/L) Centrifugation at 3000 RPM for 15 minutes at room temperature 9:1 blood-to-anticoagulant ratio is required for optimum results (9 parts whole blood to 1 part sodium citrate) High Hematocrit (≥ 55%) affects ratio Whole blood: Anticoagulant Ratio Adjustment for high hematocrit: C = (1.85x10-3)(100-H) x V C = volume of sodium citrate (mL) V = volume of whole blood-sodium citrate solution (mL) H = hematocrit (%) Example: To collect 3mL of blood and anti-coagulant mixture from a patient who’s HCT is 65%, calculate the volume of sodium citrate as follows: C = (1.85x10-3)(100-65 %) x 3.0mL C = (1.85x10-3)(35 %) x 3.0mL C= 0.19 mL of 3.2% sodium citrate CASE 1 A 55-year-old man comes to the emergency department with epistaxis. He reports that he has “bleeder’s disease” and has had multiple episodes of inflammatory hemarthroses. Physical examination reveals swollen, immobilized knees; mild jaundice; and an enlarged liver and spleen. Complete blood count results indicate that the patient is anemic and has thrombocytopenia with a platelet count of 74,400/μL. PT is within reference range and aPTT is 43 seconds. 1. What is the most likely diagnosis? 2. What treatment (s) does the patient need? 3. What reflex test (s) would you suggest? 4. What would be the result of mixing studies? CASE 2 A 28-year-old female patient presents with excessive bleeding after a dental extraction. She claims to suffer from very heavy menstruation, bleeding gums and recurrent nose bleeds throughout her life. Coagulation screen results are as follows: PT: 12.8s APTT: 42.9s PLT: 208 x109/L Questions: 1. As the next step, you do mixing studies and find mix aPTT to be 35.1s, what is your interpretation? 2. Can this be due to a lupus anticoagulant? 3. Considering the laboratory results, history, and patient’s gender, suggest the most likely clinical condition 4. List any investigation studies used to detect this suggested clinical condition and their respective results CASE 3 A 35-year-old female patient is in the ICU with sepsis after a cesarean section. CBC • WBC: 2.3 x109/L • RBC: 3.2 x1012/L • HGB: 100 g/L • HCT: 0.30 L/L Questions: • MCV: 93 fL 1. • MCH: 32 pg 2. 3. Describe the peripheral blood findings What additional tests should be performed and list the expected results? Based on all the data provided, what clinical condition is most likely? • MCHC: 345 g/L • RDW: 17.9 % • PLT: 10 x109/L Manual Differential: • Neutrophils: 90 • Lymphocytes:10 • Monocytes: 0 • Eocinophils: 0 • Basophils: 0 NRBCs- 9/100 Many Band cells seen Marked toxic granulation RBC Morph: • Many schistocytes