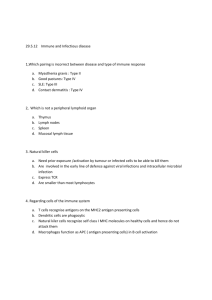
9/28/22 Inappropriate Immune Responses NURSING 304 PAT H O P H Y S I O L O G Y A LT E R AT I O N S I N IMMUNITY Allergy: an exaggerated response against an environmental antigen. Produces deleterious effects to environmental (exogenous) antigens Autoimmunity: a misdirected response against the host’s own cells. Is a disturbance in immunologic tolerance of self-antigens. Can cause autoimmune diseases Alloimmunity: directed against beneficial foreign tissues (e.g., transfusions, transplants) Is an immune reaction to tissues of another individual. Is also called isoimmunity Dr. Ghislaine Barry Immunodeficiency: Insufficient response to protect the host. All responses can be serious or life threatening Allergy, autoimmunity, & alloimmunity are collectively referred to as hypersensitivity reactions 1 2 Hypersensitivity Hypersensitivity Classifications Is an altered immunologic response to an antigen that results in disease or damage to the host. Type I: (IgE mediated) causes the release of histamine (the most potent mediator) & other inflammatory substances. Histamine release yields edema Reactions can be immediate (mins to hrs) or delayed (several hrs to days) Type II: (tissue specific) reactions caused by 5 possible mechanisms (complement mediated lysis, opsonization & phagocytosis, neutrophil mediated tissue damage, antibody dependent cell mediated cytotoxicity, modulation of cellular function) Anaphylaxis: the most immediate hypersensitivity reaction, is explosive. Occurs w/in mins of reexposure to the antigen and can lead to cardiovascular shock. Common offenders: beestings, peanuts, & fish. Clinical manifestations: itching, pain, swelling, redness, & dyspnea Type III: (immune complex mediated reactions) caused by the formation of immune complexes deposited in target tissues where they activate the complement cascade generating chemotactic fragments that attract neutrophils into the inflammatory site. Neutrophils release lysosomal enzymes resulting in tissue damage Categorized by the immune mechanisms classified as type I, II, III, IV Reactions require sensitization against a particular antigen that result in primary and secondary immune responses 3 Type IV: (cell mediated) caused by either cytotoxic T lymphs (TC cells) or lymphokine producing Th1 cells 4 Allergy Allergic Response Youtube Video Allergens are antigens that can cause allergic responses Typical allergens: pollen, mold/fungi, certain foods (milk/eggs/fish), animals (cat/dog), certain drugs (pcn), cigarette smoke, household dust Clinical manifestations of allergic reactions are usually confined to the areas of initial intake or contact. Ingested allergens induce GI symptoms, airborne allergens inhaled thru nose to lungs (portal of entry) induce respiratory tract or skin manifestations, contact allergens induce allergic responses at site of contact https://www.youtube.com/watch?v=KzIf8SYhh-8 Allergy Testing: food challenges, skin tests, IgE test 5 6 1 9/28/22 Type I Hypersensitivity Type I: Mast Cell Degranulation Is immunoglobulin E (IgE) mediated. Is against environmental antigens (allergens). IgE binds to crystalline fragment (Fc) receptors on the surface of mast cells; cross linking causes the release of histamine from mast cell degranulation. • H 1 and H 2 receptors • Increases chemotactic activity 7 8 Type I Hypersensitivity Type II Hypersensitivity Manifestations: Tissue specific From H1 Receptors: • Specific cell or tissue (tissue-specific antigens) is the target of an immune response. Bronchial constriction Five mechanisms 1. Cell is destroyed by antibodies and complement. Edema 2. Cell destruction occurs through phagocytosis. Vasodilation 3. Neutrophils release granules. From H2 Receptors: 4. Antibody-dependent cell-mediated cytotoxicity is present. Increases gastric secretions 5. Causes target cell malfunction Decreases the release of histamine from mast cells and basophils 9 10 Type II Hypersensitivity Mechanisms Phagocytosis: 11 Type II Hypersensitivity Mechanisms Cont. Neutrophil Cell Mediated Damage: Antibody Dependent Cell-Mediated Cytotoxicity: Induced Target Cell Malfunction: 12 2 9/28/22 Type III Hypersensitivity Is immune (antigen-antibody) complex mediated. Complexes are formed in the circulation and deposited later in vessel walls or extravascular tissues. Is not organ specific. Damage results from complement activation and neutrophil lysosomal enzymes. Immune complex clearance Type III Hypersensitivity Is characterized by a variety of symptoms. Periods of remission or exacerbation occur. Examples • Serum sickness Affected tissues are blood vessels, joints, and kidney. An example is Raynaud phenomenon • Arthus reaction Localized response causes increased vascular permeability, an accumulation of neutrophils, edema, hemorrhage, clotting, and tissue damage. • Large: Macrophages • Small: Renal clearance • Intermediate: Deposited in tissues; causes problems 13 14 Type IV Hypersensitivity Autoimmunity Is mediated by T lymphocytes or is cell mediated. Autoimmunity is a breakdown of homeostasis Autoimmune diseases can be caused by exposure of a previously sequestered antigen, the development of a neo antigen, the complications of infectious disease, the emergence of forbidden clone of lymphocytes, or the consequence of ineffective peripheral tolerance (ex: RA, SLE) • Destruction of the tissue is usually caused by direct killing by toxins from cytotoxic T (Tc) cells Autoimmunity • Helper T (Th) 1 and Th 17 cells produce cytokines that recruit phagocytes, especially macrophages. • Is a breakdown of tolerance during which the body’s immune system begins to recognize self-antigens as foreign. • Genetic factor: Familial association Examples • Acute graft rejection, skin test for tuberculosis (TB), contact allergic reactions (poison ivy), and some autoimmune diseases 15 16 Autoimmune Disease Systemic lupus erythematosus (SLE) • Chronic multisystem inflammatory disease • Autoantibodies against: Nucleic acids, erythrocytes, coagulation proteins, phospholipids, lymphocytes, platelets, and many others • Deposition of circulating immune complexes containing antibody against the host’s deoxyribonucleic acid (DNA) • More common in females • Currently, there is no cure for SLE 17 Alloimmunity • Clinical manifestations Alloimmunity is the immune systems reaction against antigens on the tissues of other members of the same species (ex: transfusion reaction, transplant) A rthralg ias or arthr itis Vasculitis and rash R enal disease Alloimmunity H em atolog ic changes, especially anem ia • Individual’s immune system reacting against antigens on the tissues of other members of the same species C ardiovascular disease • Presence of at least four findings indicates SLE . • Transient neonatal alloimmunity Facial (m alar) rash, discoid rash, photosensitivity, oral or nasopharyngeal ulcers, nonerosive arthr itis, serositis, renal disorders, neurolog ic disorders, hem atolog ic disorders, im m unolog ic disorders, and presence of antinuclear antibodies (A N A s ) • Fetus expressing parental antigens not found in the mother, mom sensitized against fetus • Examples: transplant rejection and transfusion reactions Treatment: Nonsteriodal antiinflammatory drugs (NSAIDs), steroids, and immunosuppressive agents are administered 18 3 9/28/22 Transfusion Reactions • Two major carbohydrate antigens Are A and B co-dominant. Individuals have antibodies to the A and B antigens they lack. Anti-A and anti-B antibody production are induced by similar antigens on naturally occurring bacteria in the intestinal tract. Antibodies are usually of the IgM class (isohemagglutinins). O blood type: Is a universal donor. AB blood type: Is a universal recipient Graft Rejection • Is primarily expressed on erythrocytes. • Rh-positive: Expresses the D antigen on the RhD protein. Alloimmune reaction Matching the human leukocyte antigens (HLA)–DR locus: Is most critical for graft acceptance. Transplant rejection: Classified according to time. • Rh-negative: Does not express the D antigen. • Approximately 15% of North American white individuals are Rh-negative. • Rh-negative individuals can make anti-D if exposed to Rh-positive erythrocytes • Hemolytic disease of the newborn: Rh-negative mother gives birth to a Rh-positive infant Acute • Chronic Cell-mediated response against unmatched HLA antigens M onths or years; due to a weak cell-mediated reaction against minor HLA antigens 20 Deficiencies in Immunity Immune deficiency Diseases • DiGeorge syndrome (congenital thymic aplasia or hypoplasia) characterized by complete or partial lack of the thymus (resulting in depressed T cell immunity), parathyroid glands (resulting in hypocalcemia), and the Impaired function of T cells, B cells, phagocytes, and/or complement • Primary (congenital): Genetic defect that disrupts lymphocyte development presence of cardiac anomalies • Secondary (acquired): secondary to disease or other physiologic alteration 21 Hyperacute • Immediate and rare; preexisting antibody to graft antigens Ex: If patient A neg receives O pos blood, will see lysis & clumping of RBC’s 19 • • Hallmark: Recurrent, severe infections, often with opportunistic organisms • SCID a total lack of T cell function and a severe lack of B cell function • Type of infection: Can lead to a diagnosis of a type of deficiency Gonorrhea suggests complement deficiency. Viral infections suggest T-cell deficiency. Microorganisms requiring opsonization suggest B-cell and phagocyte deficiencies. • Acquired immune deficiencies Usual treatment is replacement therapy i.e. deficient antibody production, replace missing immunoglobulins for congenital acquired. 22 4