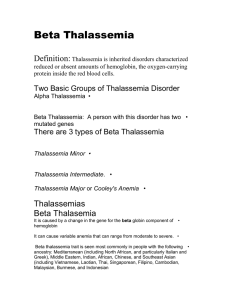
IDA: - Low MCV. High RDW. Low ferritin. High TIBC. High ZPP. Alpha Thalassemia Minor: - Low MCV. - Reticulocytosis; but remains in the normal range as the level of anemia is mild and the increased EPO production is just a slight. The increased RBC count signifies the reticulocyte count was slightly increased. - Normal RDW. - Normal ferritin. - Normal TIBC. - Normal ZPP. HbH disease: - Low MCV. - Reticulocytosis. - HbH in blood. - HbH inclusions. Hydrops Fetalis: - Hb Barts. - No HbA. Beta Thalassemia Minor: - Low MCV. - Normal MCH. - High HbA2 (differentiates from alpha thal minor, keep in mind a coexisting alpha thal or ID can decrease HbA2 levels then you’ll need iron study). Beta Thalassemia Major: - BM hyperplasia → bone deformities → chipmunk face. - Hemosiderosis. - High HbA2. - Low or absent HbA. - Nucleated RBCs in smears. Rx: transfusion/ deferoxamine/ vit C/ B9/ BM transplantation. Beta Thalassemia Intermedia: - Higher Hb levels than major making it less severe. - No transfusion needed. - Migh coexist with alpha thal or HPFH. Hemolytic Anemia: - High LDH. - Low haptoglobin. - Jaundice. - Haemoglobinuria. Low Hb is expected in all of them, it might be normal in alpha/beta thalassemia minor. It’s not a major thing to look at tho, focus on the parameters that will pinpoint the disease for you. Target cells are specific for thalassemia, stomatocytes and tear drop might also be present (not specific). In thalassemia minor, RBC increase and reticulocyte count increases as well, but remains in the normal range as the level of anemia is mild and the increased EPO production is just a slight. The increased RBC count signifies the reticulocyte count was slightly increased. In thalassemia major, both RBC and retic count increase. At the beginning of beta thalassemia major there will be reticulocytosis, but as the disease progresses folic acid gets depleted and having reticulocytopenia would be normal, thus daily folate is much needed.