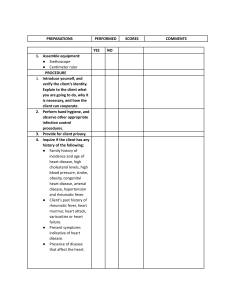
MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A 1 - SKIN, HAIR, AND NAILS ASSESSMENT Integumentary System Functions: 1. Protects the body against pathogens. 2. Regulates body temperature. 3. Synthesizes vitamin D. The examination begins with: A. Generalized inspection • Use a good source of light • Preferably indirect natural light ASSESSING THE SKIN Inspect and palpate skin for the following: • • • • • • • • • • • • • Color: Contrast with color of mucous of membrane Normal mucous membranes are pale pink to pale red Texture: Consistency of the skin Skin Turgor: lift a fold of skin and noted the ease which it moves (mobility) and the speed with which it returns into place. o NORMAL: less than 2 seconds o Note: Skin turgor is usually not examined among elderly over 65 years of age because skin is normally wrinkled. o The older client’s skin loses its turgor because of a decrease in elasticity and collagen fibers. Sagging or wrinkled skin appears in the facial, breast, and scrotal areas. Moisture: degree of water in the skin Pigmentation: coloring Lesions: change in skin integrity Hair distribution: amount and evenness of hair Warmth: feel with the back of your hand Jaundice Cyanosis Scars Edema CHECKLIST FOR ASSESSMENT OF THE SKIN Preparation 1. Assemble • Millimeter ruler equipment • Examination gloves • Magnifying glass Procedure 1. Introduce yourself and verify the client’s identity. 2. Perform hand hygiene and observe other appropriate infection control procedures. 3. Provide for client privacy. • Explain to the client what you are going to do, why it is necessary and how the client can cooperate. Rationale: to gain cooperation • Rationale: Hand hygiene is a great way to prevent infections. • Rationale: Privacy is important as it provides a secure environment for patients where they receive medical care and provide complete and accurate information, and to unnecessary prevent exposure of body parts. • • • • • • • • • 4. Inquire if client has any history of the following: 5. Inspect the skin for color. 1. 2. 3. Pain or itching Presence and spread of any lesions, bruises, abrasions, or pigmented spots. Skin problems Associated clinical signs Problems in other family members Related systemic conditions Use of medications, lotions, or home remedies Excessively dry or moist feel to the skin Tendency to bruise easily First, inspect the overall appearance of the skin. Inspect the skin for color. Assess skin color, skin tone. • Skin color can range from pinkish to dark brown. Some undertones include reddish, orange, yellow and olive. • People with dark brown skin tend to have a lighter pigmentation to the lips, palms of the hand and the fingernail. NORMAL FINDINGS: uniform in color, unblemished no presence of anu foul odor. o Varies from light to deep brown from ruddy pink to light pink. o From yellow overtones to olive. o Aging spots (irregularly pigmented melanocytes loss). DEVIATIONS FROM NORMAL: o Pallor, cyanosis, jaundice, erythema. 6. Inspect uniformity of skin color. • • Look to see if the patient’s skin tone is the same all over the body. Look for areas of hyperpigmentation and hypopigmentation. MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A NORMAL FINDINGS: o Generally uniform, except for areas exposed to the sun. o Areas of lighter pigmentation: palms, lips, nailbeds in dark skinned people. DEVIATIONS FROM NORMAL: o Areas of hyperpigmentation/hypopigmentation. NORMAL AREAS OF PIGMENTATION • Freckles - are patches of melanin pigmentation that occur normally or when the skin is exposed to the sun in some patients. These patches depend on the patient’s distribution of melanin. These patches are usually small and flat. • Moles - also are known as a nevus and are an excessive growth of melanocytes. They are usually small, smooth and symmetrical. Moles range in color from tan to dark brown. • Birthmarks - are flat areas of discoloration that are usually brown or tan. SKIN DISCOLORATIONS Pallor • result from inadequate circulating blood or hemoglobin and reduction in tissue oxygenation . CHARACTERIZED BY: • absence of underlying red tones in the skin , mostly seen in the buccal mucosa. • In brown – skinned clients skin appears as a yellowish brown tinged. • Black- skinned clients : skin appears ashen gray • pallor is usually most evident in areas with the least pigmentation conjunctiva, oral mucous membranes, nail beds, palms of the hands and soles of the feet. Cyanosis bluish tone to the skin. • • • • evident in : nail beds, lips, buccal mucosa Due to a decrease in the oxygenation to the tissue. Indicates hypoxemia (a low concentration of oxygen in the blood). Occurs in patients with shock and heart failure. Cyanosis can be: A. Centrally caused by problems with the heart and lungs B. peripherally due to exposure to cold temperatures. • Dark-skinned clients: conjunctiva, palms, nail beds, soles, mucous membranes. Jaundice (yellowish tinged) • • may be first evident : sclera of the eyes then mucous membranes and the skin. Due to increased levels of serum bilirubin in the blood. Increased bilirubin in the blood is most commonly due to liver inflammation. It is also seen in some newborns. Erythema (redness) • • • • reddish color of the skin. occurs when there is a rush of blood to the surface of the skin. associated with a fever or some type of localized inflammation. Inflammation can be assessed in a dark-skinned patient by touch. Their skin will be warm to the touch. Vitiligo 7. Assess edema if present (location, color, temperature, shape, and the degree). • • Patches of hypopigmented skin. Edema : accumulation of fluid in the intercellular spaces. 1. Check the areas that are normally dependent such as the feet and ankles. ▪ The skin will look puffy and tight. ▪ May be localized or generalized. Use your finger to lightly apply pressure for a minimum of 5 seconds. ▪ If there is no edema present, the skin will be smooth. ▪ Pitting edema is when you finger leaves an indentation when the pressure is released. Normal Findings: No edema Deviations from normal: Edema 2. ASSESSING EDEMA • Assess presence of edema, if present note the following : A. Location B. Color C. Temperature D. Shape E. Degree to which skin remains indented or pitted Scale for describing edema: 1+ barely detectable(2mm) 2+ indentation of 2-4mm 3+ indentation of 5-7mm 4+ Indentation of 7mm When pitting edema is present, use the following grading scale: 1+ Mild pitting, slight indentation, no perceptible swelling of the leg 2+ Moderate pitting, indentation subsides rapidly 3+ Deep pitting, the indentation remains for a short time, leg looks swollen 4+ Very deep pitting, indentation last a long time, the leg is very swollen 8. Inspect, palpate and describe skin lesions. • • Apply gloves if lesions are open or draining. Describe lesions according to location, distribution, color, configuration, size, shape, type, or structure. MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A • • Normal findings: few moles, and areas of •depigmentation can be encountered. Freckles, birthmarks, some flat raised nevi, no abrasions or other lesions. Various interruptions in skin integrity. Describing skin lesions: 1. Type or structure classification of lesions a. Primary lesions - are those which develop as a direct result of the disease process. b. Secondary lesions - are those which evolve from primary lesions or develop as a consequence of the patient's activities such as scales, crusts, excoriations, erosions, ulcers, fissures, scars, and keloids. 2. 3. 4. 5. Size, shape and texture (ABCDE) A= asymmetry ( two halves of the lesion do not look the same) B= border irregularity, poorly defined margins C= color variation D= diameter greater than 6mm E= elevation ( raised ) and enlargement Color Distribution Configuration PRIMARY LESIONS • macule, a flat, nonpalpable circumscribed area (up to 1 cm) of color change that's brown, red, white, or tan • patch, a flat, nonpalpable lesion with changes in skin color, 1 cm or larger • papule, an elevated, palpable, firm, circumscribed lesion up to 1 cm • plaque, an elevated, flat-topped, firm, rough, superficial lesion1 cm or larger • nodule, an elevated, firm, circumscribed, palpable area larger than 0.5 cm; it's typically deeper and firmer than a papule • cyst, a nodule filled with an expressible liquid or semisolid material • vesicle, a palpable, elevated, circumscribed, superficial, fluid-filled blister up to 1 cm • bulla, a vesicle 1 cm or larger, filled with serous fluid • pustule, which is elevated and superficial, similar to a vesicle, but is filled with pus • wheal, a relatively transient, elevated, irregularly shaped area of localized skin edema. Most wheals are red, pale pink, or white SECONDARY LESIONS caused by disease progression, overtreatment, excessive scratching, or infection of a primary lesion: • scale, a thin flake of dead exfoliated epidermis • crust, the dried residue of skin exudates such as serum, pus, or blood • lichenification, visible and palpable thickening of the epidermis and roughening of the skin with increased visibility of the normal skin furrows (often from chronic rubbing) • excoriation, linear or punctuate loss of epidermis, usually due to scratching. Look out for dry skin. 9. Observer and palpate skin moisture Assess for moisture: • Skin should not be overly moist or overly dry. 1. Inspect the amount of moisture in areas where perspiration is normally noted. 2. This includes the face, palms of the hands, and skin folds. 3. Profuse sweating (diaphoresis). This can occur during a fever, exertion or when a patient is in pain. Assessing dryness: 1. Dry skin will have a weathered look. 2. Sloughing of skin cells maybe noted. 3. Patients with dry skin may have pruritus. Pruritus is itchy skin. Normal findings: Moisture in skin folds and the axillae ( varies with environmental temperature and humidity, body temperature and activity) Deviations from normal : Excessive moisture, excessive dryness Assess for texture: 1. Palpation is used to assess for texture. 2. Use the palm (palmar surface) of the hand and the fingers to palpate for texture. 3. The skin should be smooth and firm. 4. Skin that is rough may indicate a problem with keratinization. This is when the epithelial cells lose their moisture and become dry. 5. Scar tissue will be depressed and feel smooth. Factors contribute to dry skin: o including a low-humidity environment ▪patient's personal habits (smoking, alcohol intake, and poor nutrition) o seasonal changes o chronic diseases o medications o skin cleaners o skin may be rough and scaly, with dryness occurring most often over the lower legs, hands, and forearms. Skin dryness is not associated with a dermatologic condition or systemic disease. o Scratching can cause excoriations, which can progress to secondary eczema or a skin infection. Assess skin thickness: • Palpation is used to assess for skin thickness. • Use the palm (palmar surface) of the hand and the fingers to palpate for thickness. • Skin is normally thin and firm over most of the body. MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A 10. Palpate skin temperature. Compare the two feet and two hands using the back of the fingers. • skin on the palm of the hands, the sole of the feet, knees, and elbows is normally thicker. • • Normal findings: Uniform within normal range. Deviations from normal: generalized hyperthermia (fever), hypothermia (shock), localized hyperthermia (infection), localized hypothermia (arteriosclerosis). Assess temperature: 1. Use the back of the hand (dorsal surface) to assess skin temperature. • The patient’s temperature should range from lightly warm to slightly cool. • Some patients’ hands and feet may be normally cooler. 2. Begin with the forehead and assess as you move from head-to-toe of your assessment. 3. Palpate down the body following your sequence for your head-to-toe assessment. 4. Compare the skin on the right and left sides as you move down to the feet. • The temperatures on both sides of the body should be equal. 11. Note skin turgor (fullness or elasticity) by lifting and pinching the skin on an extremity. 12. Document findings in the client record. Draw the location of skin lesions on body surface diagrams. • • Normal findings: good skin turgor ,when pinched skin springs back to previous state. With aging : texture and turgor changes. Loss of stretch and resilience. Tend to be dry. Deviations from normal: Skin stays pinched or tented or moves back slowly (i.e. dehydration). Poor skin turgor is inability of the large fold of skin to return to place promptly. May indicate dehydration. Sample documentation/charting for skin assessment: • Skin pink, warm, dry and elastic. • No lesions or excoriations noted. • Old appendectomy scar right lower abdomen 4 inches long, thin, and white. • Sprinkling of freckles noted across cheeks and nose. ABNORMAL FINDINGS: 1. Vitiligo – complete absence of melanin pigment in patchy area of white or light skin of the face, neck, hands, feet, body folds and around orifices. 2. Pigmented lesions with the following characteristics danger signs ABCDE: • Asymmetry ( two halves of the lesion do not look the same) • Border irregularity • Color variation • Diameter greater than 6mm • Elevation and enlargement 3. Seborrhea –oily skin 4. Xerosis – dry skin 5. Pruritus - itchiness 6. Alopecia – hair loss 7. Pallor- paleness of the skin due to inadequate oxygenation 8. Erythema- redness of the skin 9. Cyanosis- bluish discoloration of the skin due to inadequate oxygenation 10. Jaundice –yellowish discoloration of the skin. 11. Diaphoresis – profuse sweating ASSESSING HAIR Preparation 1. Assemble equipment: Procedure 1. Introduce yourself and verify the client’s identity. • Clean gloves Explain to the client what you are going to do, why it is necessary and how the client can cooperate. • Rationale: to gain cooperation 2. Perform hand hygiene and observe other appropriate infection control procedures. 3. Provide for client privacy • Rationale: Hand hygiene is a great way to prevent infections • Rationale: Privacy is important as it provides a secure environment for patients where they receive medical care and provide complete and accurate information, and to unnecessary prevent exposure of body parts. 4. Inquire if client has any history of the following: 5. Inspect the evenness of growth over the scalp. • • • • • Recent use of hair dyes, rinses, or curling or straightening preparations Recent chemotherapy Presence of disease Normal findings: Evenly distributed hair Deviations from normal: Patches of hair loss (i.e. alopecia) Observe the hair color: 1. Hair color is variable among patients. 2. Graying is normal depending on the patient’s age and genetics. Some patients may gray as early as their teens. Sometimes graying can be the result of a nutritional deficiency. Assess the distribution of the hair: 1. Check to see if there is even distribution of the hair throughout the scalp. 2. The thickness or thinness of the hair depend on the patient’s age, gender, and overall health. MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A 3. 6. Inspect hair thickness or thinness. 7. Inspect hair texture and oiliness. • • • • Inspect the scalp for lesions. Normal findings: Thick, silky hair. Deviations from normal: Very thin hair (hypothyroidism) Normal findings: Silky, resilient hair Deviations from normal: Brittle hair ( hypothyroidism , oily/dry hair) Assessing the texture of the hair: 1. Take a few strands of hair between your thumb and finger and roll the hair. 2. Next, take a few strands of hair between the thumb and finger of one hand near the end and use the opposite hand to slide your fingers down the length of the hair. 3. The hair may have a texture that is thick or fine. The hair may also be straight, curly or wavy. 4. Patients that have a metabolic or nutritional problem may have hair that is coarse, dry, or brittle. 8. Note presence of infections or infestations by parting the hair in several areas and checking behind the ears and along the hairline at the neck. 9. Inspect the amount of body hair. 10. Document findings in the client record. • • Normal findings: No infection or infestations. Deviations from normal: flaking. Sores, lice, nits( louse eggs) and ringworm • • Normal findings: variable. Deviations from normal: Hirsutism ( abnormal in women) Sample documentation: • Hair brown, shoulder length, clean, shiny. • No infections and no signs of infestation. • Normal distribution of hair on scalp and perineum. • Hair has been removed form legs, axillae. ASSESSING NAILS Nails are inspected for : Procedure 1. Introduce yourself and verify the client’s identity. 2. Observe appropriate infection control procedures. 3. Provide for client privacy 4. Inquire if the client has any history of the following: 5. Inspect the fingernail plate shape to determine its curvature and angle. • • • • • Nail plate shape Angle between the nail and nail bed Nail texture Nail bed color Intactness of the surrounding tissues around the nails • Explain to the client what you are going to do, why it is necessary, and how the client can cooperate. • Rationale: to prevent the spread of microorganisms. • Rationale: Privacy is important as it provides a secure environment for patients where they receive medical care and provide complete and accurate information, and to unnecessary prevent exposure of body parts. • • • • Diabetes mellitus Peripheral circulatory disease Previous injury Severe illness Normal findings: • nail plate is normally colorless and convex curvature • angle between the nail and nail bed about 160 degrees. • Deviations from normal: • Spoon shaped nail (concave fingernails) ( nail curves upward from nail bed known as koilonychia, seen in clients with iron Deficiency anemia) • Clubbing of the nail (decreased blood oxygen levels and pulmonary pathology such as malignancy, interstitial lung disease, cystic fibrosis). Assess the nail for clubbing: 1. Clubbing is when the angle of the nail is greater than 160 degrees. 2. Occurs with hypoxia over a long period of time. 3. To assess the nail for clubbing, have the patient bring two nails on opposite hands with the dorsal side of the hand (top of the hands) facing each other to create a mirror image. • Normal nails should create a diamond shape opening at the nail beds. • When a patient has clubbing, the fingers will not create a diamond shaped opening but instead, create a V-shape as the distance between the fingertips is increased. • Lovibond angle – forms when the skin fold of the nail and the base of the nail when the nail is viewed from the side. Normally tis angle is less than 165 degrees. In clubbing, the angle is more than 180 degrees. • Schamroth sign in clubbing (diamond shaped window normally visible when dorsal surfaces of terminal phalanges of both fingers from opposite hands are placed together). MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A Assess the contour and shape of the nail: 1. The profile is the surface of the nail looking at the profile of the nail. 2. Nails may be flat and some may be slightly round. 3. The angle of the nail should be 160 degrees or less. NAIL ABNORMALITIES 1. Koilonychia : nail curves upward from nail bed, seen patients with iron deficiency anemia. 2. Clubbing : a condition in which the angle between the nail and nail bed is 180 degrees or greater. Caused by long termlack of oxygen. 3. Beau’s lines : are horizontal depressions in the nail caused by severe illness or injury 4. Onychomycosis : fungal infection of the nail, nails is seen as yellow nail, discoloration, thickening of nail, separation from nail bed. 6. Inspect fingernail and toenail texture. 7. Inspect fingernail and toenail bed color. 8. Inspect tissues surrounding nails. 9. Perform blanch test of capillary refill.(Press two or more nails between your thumb and index finger; look for blanching and return of pink color to nail bed.) 10. Document findings in the client record. Normal findings: Smooth texture. Deviations from normal: • Excessive thickness can be seen in elderly in the presence of poor circulation or fungal infection, or thinness (prolonged iron deficiency anemia). • Beau’s lines are horizontal depressions in the nail as a result of injury or severe illness. • Normal findings : Highly vascular and pink in light skinned clients; dark skinned clients may have brown or black pigmentation longitudinal streaks. • Deviations from normal : cyanosis or bluish or purplish tint, pallor may reflect poor arterial circulation. Normal findings: Intact epidermis. Deviations from normal: • Hangnails (a piece of torn skin at the root of a fingernail) • Paronychia ( inflammation of tissues known as an “ingrown nail” tissues appear inflamed and swollen and tender). • • Normal findings : Prompt return of pink or usual color(generally less than 4 seconds). Deviations from normal: o Delayed return of pink or usual color. o More than 3 seconds indicates impaired peripheral circulation. • • • • Nails form 160 degree angle at base, are hard, smooth, and immobile. Nailbeds pink without clubbing. Cuticles smooth, no detachment of nail plate. Hands well-manicured with clear enamel. Normal findings: • Nails: The client has light brown nails and has the shape of convex curve. • It is smooth and is intact with the epidermis. • When nails pressed between the fingers (Blanch Test), the nails return to usual color in less than 4 seconds. PHYSICAL ASSESSMENT OF THE SKIN, HAIR, AND NAILS Preparing the Client • Ask the client to remove all clothing and jewelry and put on an examination gown. • In addition, ask the client to remove nail enamel, artificial nails, wigs, toupees, or have the client sit comfortably on the examination table or bed. • The client may remain in a sitting position for most of the examination. However, to assess the skin on the buttocks and dorsal surfaces of the legs properly, the client may lie on her side or abdomen. • Provide privacy. Keep the room door closed or the bed curtain drawn to provide privacy as necessary. • Clients from conservative religious groups (e.g., Orthodox Jews or Muslims) may require that the nurse be the same sex as the client. Also, to respect the client’s modesty or desire for privacy, provide a long examination gown or robe. • Explain what you are going to do. • Make sure that the room is a comfortable temperature. • Sunlight is best for inspecting the skin. However, a bright light that can be focused on the client works just as well. • Wear gloves when palpating any lesions because you may be exposed to drainage. Equipment • Examination light • Penlight • Mirror for client’s self-examination of skin • Magnifying glass • Centimeter ruler • Gloves • Wood’s light • Examination gown • Braden Scale for Predicting Pressure Sore Risk • Pressure Ulcer Scale for Healing (PUSH) tool to measure pressure ulcer healing. MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A When preparing to examine the skin, hair, and nails, remember these key points: • • • • • Inspect skin color, temperature, moisture, texture. Check skin integrity. Evaluate hair condition; loss or unusual growth. Note nail bed condition and capillary refill. Be alert for skin lesions. 2 – HEAD AND FACE ASSESSMENT What to do: • • • • Inspect head size, shape and symmetry. Palpate skull for nodules, masses or depressions. Inspect facial features Note symmetry of facial movements. Note presence of headaches/injury. PROCEDURE 1. Introduce yourself and verify the client’s identity. Explain to the client what you are going to do, why it is necessary, and how the client can cooperate. 2. Perform hand hygiene and observe other appropriate infection control procedures. 3. Provide for client privacy. 4. Inquire if the client has any • Lumps or bumps, itching, scaling, or dandruff history of the following: • Loss of consciousness, dizziness, seizures, headache, facial pain, or injury If so, ascertain the following: • When and how any lumps occurred • Length of time any other problem existed • Any known cause of any problem • Associated symptoms, treatment, and recurrences. ASSESSMENT 5. Inspect the head for size, shape, and symmetry. Normal findings : • Rounded (normocephalic, symmetric head that is appropriate to body size, with frontal, parietal, occipital prominences; smooth head contour. • No tenderness upon palpation. Deviations from normal: • Lack of symmetry; increased head size with more prominent nose and forehead; longer mandible (may indicate excessive growth hormone or increased bone thickness). • Microcephaly (abnormally small head) • Macrocephaly ( abnormally large head) • Lumps, depressions, and protrusions. 6. Palpate the head for nodules or masses Use a gentle rotating motion with the fingertips. Begin at the front and palpate down the midline, then palpate each side of the head. 7. Inspect the facial features (e.g. symmetry of structures and distribution of hair) Normal findings: • Smooth, uniform consistency; absence of nodules or masses and depressions when palpated. Deviations from normal: • Sebaceous cysts; local deformities from trauma. Normal findings: • Symmetric or slightly asymmetric facial features; palpebral fissures, equal in size; symmetric nasolabial folds and sides of the mouth. Deviations from normal: • Increased facial hair, thinning of eyebrows; myxedema facies; moon face. • Hirsutism 8. Inspect the eyes for edema and hollowness Normal findings: • No signs of edema. 9. Note symmetry of facial movements. Deviations from normal: • Periorbital edema • Sunken eyes. Ask the client to elevate the eyebrows, frown, or lower the eyebrows, close the eyes tightly, puff the cheeks, and smile and show teeth. Normal findings: • Symmetrical facial movements. Deviations from normal: • Asymmetric facial movements( e.g. eye on affected side cannot close completely); drooping of lower eyelid and mouth; involuntary facial movements( i.e. tics or tremors). 10. Document findings in the client record. PALPATION • • • • Head symmetrically round, hard, and smooth without lesions or bumps. Face oval, smooth, and symmetrical. Temporal artery elastic and nontender. Temporomandibular joint palpated with full range of motion without tenderness. MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A Palpate the temporal artery then the temporo-mandibular joint as the patient opens and closes the mouth. Palpate maxillary sinuses for tenderness. • • The temporal artery is palpable between the eye and top of the ear. The temporomandibular joint ( below the temporal artery and anterior to the tragus) has smooth movement as the patient opens his/ her mouth, with no limitation and tenderness. Abnormal findings : • Temporal artery looks tortuous, feels hardened and tender with temporal arteritis. To palpate the maxillary sinuses, gently press your thumbs on each side of the nose just below the cheekbones. • No tenderness over the: o maxillary sinuses ( on each side of the face) o frontal sinuses ( above the eyebrows) 3 – ASSESSING THE NECK Assessment techniques used: Areas to be examined: a. Inspection b. Palpation c. Auscultation 1. The muscles a. Sternocleidomastoid muscle b. Trapezius muscle 2. Lymph nodes 3. Trachea 4. Thyroid gland 5. Carotid arteries 6. Jugular veins AREAS OF THE NECK I. THE MUSCLES Sternocleidomastoid muscles Trapezius muscle II. LYMPH NODES IN THE NECK A. Head • Divides each side of the neck into 2 triangles. a. Anterior triangle o Trachea o Thyroid gland o Anterior cervical nodes o Carotid artery b. Posterior angle o Posterior lymph nodes • Each sternocleidomastoid muscle extends from the upper sternum and the medial third of the clavicle to the mastoid process of the temporal bone behind the ear. These muscles turn and laterally flex the head. Each extends from the occipital bone of the skull to the lateral third of the clavicle. Functions: a. Draw the head to the side and back b. Elevate the chin c. Elevate the shoulders to shrug them • • • 1. 2. 3. B. Floor of the mouth 1. 2. C. Neck 1. 2. 3. 4. Occipital • located at posterior base of the skull. Post auricular (mastoid) • behind the auricle of the ear or in front of the mastoid process. Preauricular • in front of the tragus Submandibular ( submaxillary) • along the medial border of the lower jaw, halfway between the angle of the jaw and the chin. Submental • behind the tip of the mandible in the midline under the chin. Superficial (anterior) cervical chain • along the anterior to the sternocleidomastoid muscle Posterior cervical chain • along the anterior aspect of the trapezius mastoid muscle. Deep cervical • under the sternocleidomastoid muscle Supraclavicular • above the clavicles in the angle between the sternocleidomastoid muscle. PROCEDURE 1. Explain to the client what you are going do, why is it necessary, and how he or can cooperate. 2. Observe appropriate infection control procedures. 3. Provide for client privacy. MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A ASSESSMENT 4. Inspect the neck muscles (sternocleidomastoid and trapezius) for abnormal swellings or masses. Ask the client to hold head erect. Normal findings: • Muscles equal in size • Head centered. Deviations from normal: • Unilateral neck swelling • Head tilted to one side(indicate presence of masses, injury, muscle weakness, shortening of sternocleidomastoid muscle, scars). 5. Observe head movement. Normal findings: • there is coordinated, smooth movement with no discomfort. Deviations from normal: • Muscle tremor, spasm or stiffness. Ask client to: Move the chin to the chest (determines function of the sternocleidomastoid muscle). • • Normal findings: Head flexes 45 degrees Deviations from normal: Limited ROM, painful movements; involuntary movements (e.g, up and down nodding movements associated with Parkinson’s disease). Chin to Chest Test: • Bring head forward as far as possible. • Keep chin tucked. 6. Move head back so that the chin points upward. • Determines function of the trapezius muscle. Normal findings : o Head hyperextends 60 degrees. Deviations from normal: o Head hyperextends less than 60 degrees • • 7. Assess muscle strength. Move head so that the ear is moved toward the shoulder on each side. (Determines function of the sternocleidomastoid muscle.) Turn head to the right and to the left. (Determines function of the sternocleidomastoid muscle.) Ask the client to: • Turn head to one side against the resistance of your hand. Repeat with the other side. • Shrug shoulders against the resistance of your hands. LYMPH NODES 8. Palpate the entire neck for enlarged lymph nodes. TRACHEA 9. Palpate the trachea for lateral deviation. THYROID GLAND 10. Inspect the thyroid gland. • • • • • Place your fingertip or thumb on the trachea in the suprasternal notch. Then move your finger laterally to the left and the right in spaces bordered by the clavicle, the anterior aspect of the sternocleidomastoid muscle, and the trachea. Stand in front of the client. Observe the lower half of the neck overlying the thyroid gland for symmetry and visible masses. Ask the client to hyperextend head and swallow. If necessary, offer a glass of water to make it easier for the client to swallow. 11. Palpate the thyroid gland for smoothness. 12. If enlargement of the gland is suspected: • Note any areas of enlargement, masses, or nodules. • • • • Auscultate over the thyroid area for a bruit (vascular murmur). Use the bell-shaped diaphragm of the stethoscope. A thyroid bruit is described as a continuous sound that is heard over the thyroid mass. Thyroid bruit is seen in Grave's disease. 13. Document findings in the client record. • • • • Neck symmetric with centered head position and no bulging masses. Has smooth, controlled, full range of motion on the neck. Thyroid gland non-visible but palpable when swallowing. Trachea is midline. Lymph nodes nonpalpable. MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A 4 – ASSESSING THE EYES AND VISION Eyelid Palpebral fissure Eyelashes Conjunctiva Lacrimal apparatus Extraocular muscles of the eye Internal structures of the eye Sclera Cornea Iris Lens Choroid Retina Optic disc Eyeball Aqueous humor Visual Reflexes Accommodation • TARSAL PLATES contain MEIBOMIAN GLANDS secrete an oily substance that lubricates the eyelid • Eyelids join at two points: the lateral (outer) canthus and medial (inner) canthus • The medial canthus contains the puncta, two small openings that allow drainage of tears into the lacrimal system and the caruncle, a small fleshy mass that contains sebaceous glands • The width of the palpebral fissure is an important indicator for a number of pathologic changes in the eye • Projections of stiff hair curving outward along the margins of the eyelids that filter dust and dirt from air entering the eye • Thin, transparent, continuous membrane DIVISIONS OF CONJUNCTIVA: ✓ Palpebral conjunctiva lines the inside of the eyelids ✓ Bulbar conjunctiva (covers most of the anterior eye, merging with the cornea at the limbus) • Consists of glands and ducts that lubricate the eye • The lacrimal gland, located in the upper outer corner of the orbital cavity just above the eye, produces tears • As the lid blinks, tears wash across the eye then drain into the puncta, which are visible on the upper and lower lids at the inner canthus. Tears empty into the lacrimal canals and are then channeled into the nasolacrimal sac through the nasolacrimal duct. They drain into the nasal meatus • six muscles attached to the outer surface of each eyeball • control six different directions of eye movement • Four rectus muscles are responsible for straight movement, and two oblique muscles are responsible for diagonal movement • The eyeball is composed of three separate coats or layers. The external layer consists of the sclera and cornea. • The middle layer contains both an anterior portion, which includes the iris and the ciliary body, and a posterior layer, which includes the choroid. The ciliary body consists of muscle tissue that controls the thickness of the lens, which must be adapted to focus on objects near and far away • dense, protective, white covering that physically supports the internal structures of the eye • continuous anteriorly with the transparent cornea (the “window of the eye”) • permits the entrance of light, which passes through the lens to the retina • well supplied with nerve endings, making it responsive to pain and touch • circular disc of muscle containing pigments that determine eye color • pupil – central aperture of the iris • Muscles in the iris adjust to control the pupil’s size, which controls the amount of light entering the eye. • The muscle fibers of the iris also decrease the size of the pupil to accommodate for near vision and dilate the pupil when far vision is needed • biconvex, transparent, avascular, encapsulated structure located posterior to the iris. • The lens functions to refract (bend) light rays onto the retina. Adjustments must be made in refraction depending on the distance of the object being viewed. • Refractive ability of the lens can be changed by a change in shape of the lens (which is controlled by the ciliary body). • The lens bulges to focus on close objects and flattens to focus on far objects • contains the vascularity necessary to provide nourishment to the inner aspect of the eye and prevents light from reflecting internally. • innermost layer that extends only to the ciliary body anteriorly. • consists of nerve cells which is the rods and cones. • Photoreceptors – specialized nerve cells; responsive to light, regulate black-and-white vision, and function in dim light • Cones – bright light and are sensitive to color • Cream-colored, circular area located on the retina toward the medial or nasal side of the eye • Can be seen with the use of an ophthalmoscope and is normally round or oval in shape, with distinct margins • eyeball contains several chambers that maintain structure, protect against injury, and transmit light rays. • Anterior chamber - located between the cornea and iris; the posterior chamber is the area between the iris and the lens. • Clear liquid substance produced by the ciliary body • Helps to cleanse and nourish the cornea and lens as well as maintain intraocular pressure • Pupillary light reflex - immediately to constrict when exposed to bright light; bright reflex (constriction occurs in the eye exposed to the light) • Indirect or consensual reflex - exposure to light in one eye results in constriction of the pupil in the opposite eye • Functional reflex allowing the eyes to focus on near objects MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A Physical Examination 1. Inspect eyebrows for hair distribution and alignment, skin quality and movement 2. Inspect the eyelashes or evenness of Purpose of the eye and vision examination - To identify any changes in vision or signs of eye disorders in an effort to initiate early treatment or corrective procedures Physical Examination 1. Perform handwashing 2. Prepare and assemble the equipment 3. Check the client’s identity 4. Explain the procedure 5. Provide privacy Normal findings: • Hair is evenly intact • Eyebrows symmetrically aligned and showed equal movement when asked to raise and lower eyebrows Eyes • Evenly placed and inline with each other • Non protruding • Equal palpebral fissure Deviations from normal: Loss of hair, scaling and flakiness of skin. Unequal alignment and movement of eyebrows • Equally distributed, curled slightly outward Deviations from normal: a. Entropion: eyelid turned inward • Rub against the eyeball, causing discomfort MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A distribution and direction of curl 3. Inspect eyelids for surface characteristics Abnormalities of the eyelids 4. Inspect bulbar conjunctiva Abnormal Findings: Bulbar Conjunctiva 5. 6. 7. Inspect palpebral conjunctiva for color, texture and presence of lesions Inspect and palpate lacrimal glands and sacs, and nasolacrimal duct Inspect cornea for clarity and texture 8. Perform corneal sensitivity test (reflex) Abnormal Findings 9. Inspect pupil for color, shape and symmetry of size Deviations from Normal: Pupil 10. Assessing pupil reaction b. Ectropion: eyelids turn outward • This leaves the inner eyelid surface exposed and prone to irritation • Skin intact; no discharge; no discoloration • Lids close symmetrically w/o drooping • 15 to 20 involuntary blinks/ min; bilateral blinking • Redness, swelling, flaking, crusting, plaques, discharge, nodules, lesions • Lids close asymmetrically, absent or infrequent blinking • Ptosis • Ectropion • Entropion • Color • Texture and presence of lesions Normal findings: Transparent; capillaries sometimes evident dark-skinned clients • Jaundiced sclera • Reddened Sclera • Lesions/nodules on sclera Normal findings • Shiny, smooth and pink or red Deviations from normal • Extremely pale (Anemia) • Extremely red (inflammation) • Nodules or other lesions • Normally no edema or tearing • Use tip of your finger, palpate the lacrimal gland • Observe for edema between the lower lid and the nose and observe evidence of increased tearing Deviations from Normal • Evidence of increased tearing; regurgitation of fluid on palpation of lacrimal sac Normal findings • Cornea transparent and shiny, smooth; details of the iris are visible • Older people: a thin grayish white ring around the margin, called arcus senilis maybe evident Deviations from normal • Opaque; surface not smooth (results from injury or abrasion) • Arcus senilis in clients under age 40 is abnormal • Client blinks when the cornea is touched, indicating that the trigeminal nerve (CNV) is intact Deviations from normal: • One or both eyelids fail to respond Corneal Abnormalities Corneal scar – appears grayish white, usually is due to an old injury or inflammation Early pterygium – thickening of the bulbar conjunctiva that extends across the nasal side • Pupil is black in color; equal in size; normally 3 to 5 mm in diameter, round, smooth border and round Deviations from normal: • Cloudiness • Mydriasis – unusual dilatation of the pupils • Miosis – excessive constriction of the pupils 1. Reaction to light • Place the patient in an area with even lighting and instruct him to fix his gaze on a distant object. • Cover one eye and shine a flashlight in front of the exposed eye. • The pupil should constrict because of the light. • This response is called a direct reaction. The covered pupil should also contract. • This response is called a consensual reaction. 2. 11. Perform pupil reaction movement tests 12. Assess pupils’ reaction to accommodation (ability of the lens to adjust to objects at varying distances) Miosis Anisocoria Mydriasis PERRLA 13. Assessing visual fields Near point reaction • When the gaze is changed from a distant object to an object close at hand, the pupils should constrict a. Assess each pupil’s direct consensual reaction to light to determine function of the third (oculomotor) and fourth (trochlear) cranial Normal findings • Illuminated pupil constricts (direct response) • Nonilluminated pupil constricts (consensual response) Normal findings • Pupils constricts when looking at near objects dilate when looking at far objects; • Pupils converge (tend to meet at a point) when near object is moved toward the nose. Abnormal findings • One or both pupils fail to constrict, dilate or converge • Pinpoint pupils; constricted and fixed pupils- narcotic drugs or brain damage • Pupils of unequal size • Dilated or fixed pupils; CNS injury; circulatory collapse; deep anesthesia • Acronym for the pupil qualities • Pupils, Equal, Round, Reactive (to), Light, Accommodation Normal Findings • When looking straight ahead, client can see objects in the periphery. Deviations from Normal MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A • • Visual field smaller than normal ( possible glaucoma); one half vision in one or both eyes (indicates nerve damage Visual fields 14. Perform six ocular movement tests. Pseudostrabismus Strabismus (Tropia) 15. Assess Visual Acuity Snellen Eye Chart Recording Visual Acuity Test Papilledema Glaucoma Optic Atrophy 16. Perform Functional Vision Tests • Convergence - ability of the eye to turn or rotary movement of the eye. • Assess six ocular movements to determine eye alignment and coordination. Normal Findings • Both eyes coordinated, move in unison, with parallel alignment Abnormal Findings • Eye movements not coordinated or parallel, one or both eyes fail to follow a penlight in specific directions Nystagmus - involuntary rhythmic side-to-Pseduoside and up and down or circular motion of the eyes. • Normal in young children, the pupils will appear in the inner canthus • Constant misalignment of the eye axis • Esotropia (inward) • Exotropia (outward) a. Assess near vision Normal Findings • Able to read newsprint Deviations from normal: • Difficulty reading newsprint due to aging process b. Assessing Visual Acuity Normal findings • 20/20 vision on Snellen Chart Abnormal Findings • denominator of 40 or more on Snellen chart with corrective lenses. • used to measure the visual acuity. It has lines of letters arranged in decreasing size. • Position the patient 20 feet away from the chart. • Ask patient to cover one eye with opaque card. Test right eye first, then the left eye. • If patient wears eyeglasses or contact lenses, leave them on. Remove only reading glasses because they will blur distance vision. • Ask the patient to read through the chart to the smallest line possible. ✓ Use a Snellen picture chart for people who cannot read letters • Indicate if some of the letters were missed or if corrective lenses were worn. Ex. 20/20-2 with glasses (OD-right eye) Normal Findings • Normal result of the Snellen test is 20/20 (indicates normal vision) • The numerator indicates distance of the patient from the chart. • The denominator indicates the distance at which the normal eye can read the letter Abnormal Findings • If the denominator is increased or greater ( 20/30), the patient has myopia • If the denominator is decreased (20/15) or less), the patient has hyperopia • If the result is 20/200, the patient is legally blind. He is not allowed to drive. • Swollen optic disc • Blurred margins • Hyperemic appearance from accumulation of excess blood • Visible and numerous disc vessels • Lack of visible physiologic cup • Enlarged physiologic cup occupying more than half of the disc’s diameter • Pale base of enlarged physiologic cup • Obscured and/or displaced retinal vessels • White optic disc • Lack of disc vessels I. Light perception: How do you test LP? - If the patient can't see your hand waving, then shine a light in the patient’s eye. If the patients see the light record it as 'LP'(Light perception). If the patient can't see the light record it as 'NLP'(No light perception). Note: Light perception is different from light projection. II. Hand movements - hold hand 30cm ( 1 ft) from the patient’s face and move slowly back and forth, stopping it periodically. Ask client to tell you when your hand stops moving, if client knows when your hand stops moving, record the vision as ‘H/M 1 ft.” III. Counting Fingers - hold up some of your fingers 30cm(1ft) from the client’s face and ask the client to count your fingers. If the client can do so, note on the vision record “C/F 1 ft.” MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A 5 - ASSESSMENT OF THE EARS 3 Parts of the Ears Equipment 1. 2. 3. • • • External Ear Middle Ear Inner Ear Watch with a second hand for Romberg test Tuning fork (512 or 1024 Hz) Otoscope ASSESSMENT (INSPECTION) A. Inspect and 1. Ear position and alignment on head. palpate the external ✓ The top of the pinna should match an imaginary line extending from the corner of the eye to ear. the occiput. ✓ Infants: Low-set ears may indicate mental retardation or a genitourinary malformation. 2. Size and Shape ✓ The ears are of equal size bilaterally with no swelling or thickening. ✓ Ears of unusual size and shape may be a normal familial trait with no clinical significance. ▪ Assess for Microtia and Macrotia 3. Skin condition ✓ The skin color is consistent with the person’s facial skin color. ✓ Skin is intact, with no lumps or lesions. ✓ Darwin’s tubercle, a small painless nodule at the helix. 4. Tenderness • Move the pinna and push on the tragus. ✓ They should feel firm, movement should produce no pain. ✓ Pain with movement: otitis externa and furuncle (boil). • Palpate the mastoid process. ✓ No pain ✓ Pain: mastoiditis or lymphadenitis of the posterior auricular node. 5. The external auditory meatus (outer ear canal). • Note the size of the opening and there should be no swelling, redness, or discharge. □ Aural atresia (congenital deformity, ear canal is underdeveloped). □ A sticky yellow discharge = otitis externa or otitis media (if the drum has ruptured). • Some cerumen is usually present. □ Color: gray-yellow to light brown and black. □ Texture: moist and waxy to dry and desiccated. □ A large amount of cerumen obscures visualization of the canal and drum. □ Impacted cerumen is a common cause of conductive hearing loss. B. Inspect using the otoscope. 1. Note the size of the auditory meatus as you inspect the external ear. 2. Then choose the largest speculum that will fit comfortably in the ear canal, and attach it to the otoscope. 3. Tilt the person’s head slightly away from you toward the opposite shoulder. 4. Pull the pinna up and back on an adult or older child. Pull the pinna down on an infant and a child under 3 years of age. 5. Hold the pinna gently but firmly. Do not release traction on the ear until you have finished the examination and the otoscope is removed. 6. Hold the otoscope – upside down along your fingers and have the dorsa of your hand along the person’s cheek braced to steady the otoscope. INSPECT THE EXTERNAL CANAL 6. The external canal. • Note any redness, swelling, lesions, foreign bodies or discharge. ✓ If discharge is present, note the color and odor. ✓ For a person with a hearing aid, note any irritation on the canal wall from poorly fitting ear molds. • Redness and swelling occur with otitis externa. • Purulent otorrhea suggests otitis externa or otitis media if the drum has ruptured. • Frank blood or clear, watery discharge (CSF) following trauma suggests basal skull fracture and warrant immediate referral. ✓ CSF feels oily and is positive for glucose on TesTape. INSPECT THE TYMPANIC MEMBRANE 7. The tympanic membrane a. Color and characteristics • The normal eardrum is shiny and translucent, with a pearl-gray color. • Yellow-amber drum color occurs with serous otitis media. • Red color occurs with acute otitis media. • Air/fluid level of air bubbles behind drum indicate serous otitis media (Glue ear). b. Position • The eardrum is flat, slightly pulled in at the center, and flutters (move) when the person performs the Valsalva maneuver. • Avoid middle ear insufflations (blowing) in a person with URTI because it could propel infectious matter into the middle ear. 8. Integrity of membrane • Inspect the eardrum and the entire circumference for perforations. • The normal tympanic membrane is intact. MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A • ASSESSING HEARING ACUITY Some adults may show scarring, which is a dense white patch on the drum. This is a sequel of repeated ear infections. 9. Test hearing acuity • Nursing History: how well does the person hear conversational speech? • An audiometer gives a precise quantitative measure of hearing by assessing the person’s ability to hear sounds of varying frequency. ASSESSMENT: MECHANICAL TEST FOR HEARING 10. Voice (Whisper) • Test one ear at a time. Test • Place one finger on the tragus and rapidly push it in and out of the auditory meatus. • Shield lips; position 1-2 ft away from ear • Whisper 2 syllable words, e.g., Tuesday, baseball • Whisper a number or word approximately 60cm from the patient’s ear and ask the patient to repeat it. ✓ ✓ 11. Tuning fork tests. 12. The vestibular apparatus • • Tuning fork tests measure hearing by air conduction or by bone conduction. To activate the tuning fork, hold it by the stem and strike the tines softly on the back of your hand. a. Weber test: test for lateralization of vibration. • The Weber test is valuable when a person report hearing better with one ear than the other. • Place a vibrating tuning fork in the midline of a person’s skull and ask if the tone sounds the same in both ears or better in one. ✓ The person should hear the tone by bone conduction through the skull, and it should equally loud in both ears. b. Rinne test: compares air conduction and bone conduction sound. • Place the stem of the vibrating tuning fork on the person’s mastoid process and ask him or her to signal when the sound goes away. Quickly invert the fork so the vibrating end is near the ear canal; the person should still hear a sound. ✓ Normally the sound is heard twice as long as by air conduction (next to ear canal) as by bone conduction (through the mastoid process). ✓ A normal response is a positive Rinne test or – AC>BC. • • The Romberg test assesses the ability of the vestibular apparatus in the inner ear to help maintain standing balance. Romberg test is a test of the body’s sense of positioning (proprioception), which requires healthy functioning of the dorsal columns of the spinal cord. + Romberg test (abnormal) 1. 2. 3. Ask the patient to stand with their feet together (touching each other). Then ask the patient to close their eyes. Remain close at hand in case the patient begins to sway or fall. • • • • • • • • • • Otalgia – earache Otorrhea – ear discharge Presbycusis – hearing loss due to old age Tinnitus – ringing of the ear Vertigo – feels like room spins or person feels he/she spins Microtia – small ears, smaller than 4 cm vertically Macrotia – large ears, larger than 10 cm vertically Impacted cerumen – hardened ear wax Otitis media – infection of the middle ear Otitis externa – infection of the external ear • ABNORMAL FINDINGS Normally, the person repeats each word correctly after you say it. If the person is unable to hear whispered words, it is abnormal. A whisper is a highfrequency sound and is used to detect high-tone loss. 6 – ASSESSMENT OF THE NOSE Anatomy of the Nose External nose features: • Root • Dorsum (anterior border) • Tip • Lateral side • Nostrils (anterior nares) • Columella Normal anatomy: • Frontal sinus • Sphenoid sinus • Middle ear MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A • • • • • • • • Eardrum Eustachian tube Esophagus Palatine tonsil Trachea Upper turbinate Middle turbinate Lower turbinate ASSESSMENT Subjective Data A. External nose Nursing History: a. Allergies b. Difficulty breathing through the nose c. Sinus infection d.Injuries to nose or face d. Nosebleeds e. Any medications taken f. Any changes of smell • Nose is symmetric, in the midline, and in proportion to other facial features. • Newborn may have milia across the nose. • The nasal bridge may be flat in black and Asian children. Test the patency of the nostrils to R/O indicates obstruction (e.g., nasal polyps, rhinitis). • any deformity, asymmetry, inflammation or skin lesions. • Injury: palpate gently for any pain or break in contour. • nasal flaring. • wing with breathing. B. Nasal cavity • • • • C. Palpate the sinus area. • • View each nasal cavity with the person’s head erect, then with the head tilted back. Inspect the nasal mucosa, noting its normal red color and smooth moist surface. Note any swelling, discharge, bleeding, or foreign body. o In rhinitis, nasal mucosa is swollen and bright red with URTI. o Discharge is common with rhinitis and sinusitis, varying from watery and copious to thick, purulent, and green-yellow. o With chronic allergy, mucosa looks swollen, boggy, pale and gray. Inspect the turbinates, the bony ridges curving down from the lateral walls. o Middle and inferior turbinates appear the same light red color as the nasal mucosa. o Note any swelling. o Turbinates are quite vascular and tender if touched. • Note any polyps, which are benign growths that accompany chronic allergy, and distinguish them from the normal turbinates. o Polyps are smooth, pale gray, avascular, mobile and non-tender. Using your thumbs, press over the frontal sinuses. Take care not to press directly on the eyeballs. o The person should feel firm pressure but no pain. o Sinuses: frontal, ethmoid, maxillary ABNORMALITIES OF THE NOSE Choanal atresia • A bony or membranous septum between the nasal cavity and the pharynx of the newborn. Epistaxis • Nose bleeding, most common in the anterior septum. Foreign body • Children particularly are apt to put an object up the nose, producing unilateral mucopurulent drainage and foul odor. Perforated septum • A hole in the septum, usually in the cartilaginous part, may be caused by trauma from continual picking of crusts, chronic infection, sniffing. Furuncle • A small boil located in the skin or mucous membrane; appears red and swollen and is quite painful. o Avoid manipulation. • Cone-shaped infiltrate covered hyperemic skin on top of which is usually 3-4 days appears yellowish-white heat- the abscess. Inflammation extended to the upper lip, cheek and soft tissue. Acute rhinitis Sinusitis • • • • • • • Nasal polyps • Carcinoma • • • watery discharge, rhinorrhea Sneezing, swollen mucosa, Rhinorrhea, itching of nose and eyes, lacrimation, nasal congestion, and sneezing are present. Pale turbinates (although may appear violet), and their surface looks smooth and glistening. May be seasonal or perennial, depending on allergen. Facial pain, following URTI S/S: red swollen nasal mucosa, swollen turbinates, and purulent discharge. fever, chills, malaise. Smooth, pale gray nodules, which are overgrowths of mucosa, most commonly caused by chronic allergic rhinitis. This appears gray-white and nontender. It may produce slow bloody unilateral discharge. It is not a common lesion. MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A 7 – MOUTH & THROAT ASSESSMENT A. HISTORY (FROM REVIEW OF SYSTEMS) 1. a. Mouth pain b. Frequent sore throat c. bleeding gums d. toothache e. lesion in mouth or on tongue f. dysphagia g. hoarseness or voice change h. tonsillectomy i. altered taste 2. a. Pattern of daily dental care b. use of dentures c. bridges d. last dental checkup ASSESSING THE MOUTH & OROPHARYNX Lips and Buccal Mucosa 1. Inspect the outer ✓ color lips for: ✓ moisture ✓ cracking ✓ lesions 2. Inspect and palpate inner lips and buccal mucosa for: Ask patient to purse lips as if to whistle. Normal findings : • Uniform color ‘ pink’ • Soft, moist, smooth texture • Symmetry of contour • No masses, ulcerations, fissures • Able to purse lips. Deviations from normal • Pallor, cyanosis • Presence of blisters, swelling, fissures, crusts or scales • Unable to purse lips ( facial nerve damage) • color • moisture • texture • presence of lesions Normal findings: • Uniform pink color • Moist, smooth, soft, glistening and elastic texture( drier oral mucosa in elderly due to decreased salivation) Deviations from normal: • Pallor, white patches (leukoplakia) • Excessive dryness • Mucosal cysts; irritations from dentures; abrasions. • Ulcerations; nodules Teeth and Gums 3. Inspect for the following: a. Teeth/ Gums • Number • Arrangement • General condition b. Gums • Color • Texture • Discharge • Swelling or retraction c. Dentures ✓ Smooth, intact dentures • Normal findings: o Teeth ✓ 32 adult teeth ✓ Smooth, white shiny tooth enamel o Gums ✓ Pink gums, smooth, no swelling , no bleeding, no pus discharge ✓ Moist, firm texture of gums, no retraction of gums ( pulling away from the teeth) • Deviations from normal: ✓ Missing teeth ✓ ill-fitting dentures ✓ Excessively red gums ✓ No retraction of gums ✓ Spongy texture of gums, bleeding, tenderness ( periodontal disease) ✓ Receding atrophied gums, swelling partially covers the teeth. MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A Tongue/Floor of the Mouth 4. Inspect for the a. Surface of tongue for position, color and texture.( ask client to protrude tongue) following: b. Tongue movement c. Base of the tongue, mouth floor and the frenulum 5. Palpate a. Tongue b. Floor of the mouth for nodules, lumps and excoriated areas. Normal findings: Tongue o Midline , covered with papillae ✓ Pink color, moist; slightly rough; thin whitish coating ✓ Smooth, lateral margins; no lesions • Tongue movement ✓ Moves freely; no tenderness • Base of tongue ✓ Smooth with prominent veins ✓ Smooth with no palpable nodules Deviations from normal: Tongue • deviated from the center • Smooth red tongue ( iron, vitamin B12 or B6 deficiency) • Presence of nodules , ulcerations, discolorations • Dry, furry tongue ( fluid deficit) • Restricted mobility • Presence of ulcers , discolorations , tender • Restricted mobility • Swelling Salivary Glands 6. Inspect salivary duct openings for swelling or redness Normal findings: ✓ Same color of buccal mucosa and floor of mouth Deviations from normal: ✓ Inflammation ( redness and swelling) Palates and Uvula To check the uvula: ✓ a tongue blade is pressed down on the patient's tongue and the patient is asked to say "ah" ✓ the uvula should look like a pendant in the midline and rise along the soft palate. 7. Inspect the hard and soft palate for : Normal findings: ✓ color : • light pink, smooth, soft palate • lighter pink hard palate, more irregular texture ✓ Shape ✓ Texture ✓ Presence of bony prominences Deviations from normal: Hard and soft palates • Discoloration ( jaundice or pallor) • Irritations • Bony growths growing from the hard palate. • Leiomyoma of soft palate • blanching of soft palate • Blue grey lesion of palate 8. Inspect uvula for Uvula abnormal findings: position and mobility • Deviation to one side from tumor or trauma. Oropharynx and Tonsils 9. Inspect oropharynx • Color for: • texture • Inflammation • Masses ✓ Pink and smooth posterior wall Deviations from normal: • Reddened or edematous oropharynx • Presence of lesions, plaques, drainage 10. Inspect the tonsils for color, discharge and size. ✓ Pink and smooth ✓ Can be seen on the posterior portion of the tongue ✓ No discharge ✓ Of normal size Deviations from normal: • Inflamed tonsils • Presence of discharge MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A • Swollen 11. Inspect the posterior oropharynx by depressing the tongue and asking the patient to say "Ah." Note any tonsilar enlargement, redness, or discharge. 12. Elicit the gag ✓ Present gag reflex reflex by pressing ✓ Absent may indicate problems with glossopharyngeal or vagus nerves. tongue with a tongue blade. • Pharyngeal ‘gag’ reflex – subsumed in the swallowing reflex, being elicited by momentary & artificial stimulation of the oropharynx (in contrast with food or drink which produce sustained, familiar stimulation). o Gently touch posterior oropharynx with sterile swab. o Look for abnormal deviation away from side of lesion. o Two key features: -inhibition of respiration -relaxing of the soft palate. 13. Document findings. 8 – ASSESSING THORAX AND LUNGS 1. Preparing the Client 2. Equipment 3. During examination of the client Inspection Palpation • Have the client remove all clothing from the waist up and • put on an examination gown or drape. • The gown should open down the back, and is used to limit exposure. Examination of a female client’s chest may create anxiety because of embarrassment related to breast exposure. • Explain that exposure of the entire chest is necessary during some parts of the examination. To further ease client anxiety. • Ask the client to sit in an upright position with arms relaxed at the sides. • Examination gown and drape • Gloves • Stethoscope • Light source • Mask • Skin marker • Metric ruler • Provide privacy • Keep your hands warm • Remain nonjudgmental regarding the client’s habits and lifestyle particularly smoking. At the same time educate and inform about risks such as lung CA, COPD and related habits • Inspect for nasal flaring and pursed lip breathing • Nasal flaring is seen with labored respirations (especially in small children) and is indicative of hypoxia. • Pursed lip breathing may be seen in asthma, emphysema, or CHF as a physiologic response to help slow down expiration and keep alveoli open longer • Pursed lip breathing - slowly inhale through your nose and gently exhale through pursed lips. • Observe color of face, lips, and chest • • The client has evenly colored skin tone, without unusual or prominent discoloration • Ruddy to purple complexion may be seen in clients with COPD or CHF as a result of polycythemia. Cyanosis may be seen if client is cold or hypoxic. • Inspect color and shape of nails. • Pink tones should be seen in the nailbeds. • There is normally a 160-degree angle between the nail base and the skin. • Inspect configuration. While the client sits with arms at the sides, stand behind the client and observe the position of scapulae and the shape and configuration of the chest wall • Scapulae are symmetric and nonprotruding • Shoulders and scapulae are at equal horizontal positions. The ratio of anteroposterior to transverse diameter is 1:2. • Spinous processes appear straight, and thorax appears symmetric, with ribs sloping downward at approximately a 45-degree angle in relation to the spine • Observe use of accessory muscles. Watch as the client breathes and note use of muscles • The size of the thorax, which affects pulmonary function, differs by race. Compared with African Americans, Asians and Native Americans, adult Caucasians have a larger thorax and greater lung capacity • The client does not use accessory (trapezius/shoulder) muscles to assist breathing. The diaphragm is the major muscle at work. This is evidenced by expansion of the lower chest during inspiration • Inspect the client’s positioning. Note the client’s posture and ability to support weight while breathing comfortably • Client should be sitting up and relaxed, breathing easily with arms at sides or in lap. • Palpate for tenderness and sensation. Palpation may be performed with one or both hands, but the sequence of palpation is established. • Use your fingers to palpate for tenderness, warmth, pain, or other sensations. • Start toward the midline at the level of the left scapula (over the apex of the left lung) and move your hand left to right, comparing findings bilaterally. Move systematically downward and out to cover the lateral portions of the lungs at the bases. • Palpate for crepitus. Crepitus, also called subcutaneous emphysema, is a crackling sensation (like bones or hairs rubbing against each other) that occurs when air passes through fluid or exudate. MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A 9 - ASSESSING THE BREAST Preparing the Client • • • • • • Equipment Key points for PA • • • • • • • • • The actual hands-on physical examination of the breast may create client anxiety. ✓ The client may be embarrassed about exposing his or her breasts and may be anxious. Explain in detail what is happening throughout the assessment Provide the client with as much privacy as possible during the examination. Prepare for the breast examination by having the client sit in an upright position. Explain that it will be necessary to expose both breasts to compare for symmetry during inspection. One breast may be draped while the other breast is palpated. Be sensitive to the fact that many women may feel embarrassed to have their breasts examined. The breasts are first inspected in the sitting position while the client is asked to hold arms in different positions. The breasts are then palpated while the client assumes a supine position The final part of the examination involves: teaching clients how to perform BSE and asking them to demonstrate then ask the client to demonstrate how is it done Centimeter ruler Small pillow Gloves Client handout for BSE Slide for specimen Explain to the client what the steps of the examination and the rationale. Warm your hands. Observe and inspect breast skin, areolas, and nipples for size, shape, rashes, dimpling, swelling, discoloration, retraction, asymmetry and other unusual findings. Palpate breasts and axillary lymph nodes for swelling, lumps, masses, warmth or inflammation, tenderness, and other abnormalities. MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A • ASS PROCEDURE (INSPECTION) • • • • • • Palpation The Axillae (Inspection and Palpation) The Male Breasts (Inspection and Palpation) Palpating the Breasts BSE STEPS Peau D’orange Paget’s Disease Retracted Nipple Dimpling Retracted Breast Tissue Cancerous Tumors Fibroadenomas Benign Breast Disease • • • • Remember it is important to carefully perform the breast examination on male as well as female clients. Inspect size and symmetry. Have the client disrobe and sit with arms hanging freely. Explain what you are observing to help ease client anxiety Inspect color and texture. Note any lesions Inspect superficial venous pattern. Observe visibility and pattern of breast veins Inspect the areolas. Note the color, size, shape, and texture of the areolas of both the breasts Inspect the nipples. Note the size and direction of the nipples of both breast. Note dryness, lesions, bleeding, or discharge Finally ask the client to lean forward from the waist. The nurse should support the client by the hands or forearms. This is a good position to use in women who have large, pendulous breasts Palpate texture and elasticity Palpate for tenderness and temperature Inspect and palpate the axillae. Ask the client to sit up. Inspect the axillary skin for rashes or infection. Hold the client’s elbow with one hand, and use the three finger pads of your other hand to palpate firmly the axillary lymph nodes. First palpate high into the axillae, moving downward against the ribs to feel for the central nodes. Continue to move down the posterior axillar to feel for the posterior nodes. Use bimanual palpation to feel for the anterior axillary nodes. Finally palpate down the inner aspect of the upper arm. Inspect and palpate the breasts, areolas, nipples, and axillae. Note any swelling, nodules, or ulceration. Palpate the flat disc of underdeveloped breast tissue under the nipple. 1. Ask the client to lie down and to place overhead the arm on the same side as the breast being palpated. Place a small pillow or a rolled towel under the breast being palpated. 2. Use the flat pads of three fingers to palpate the client’s breasts 3. Palpate the breasts using one of three different patterns. Choose one that is most comfortable for you, but be consistent and thorough with the method chosen. 4. Be sure to palpate every square inch of the breast, from the nipple and areola to the periphery of the breast tissue and up into the tail of Spence. Vary the levels of pressure as you palpate. Light – superficial Medium – mid-level tissue Firm – to the ribs 5. Use the bimanual technique if the client has large breasts. Support the breast with your nondominant hand and use your dominant hand to palpate. Stand in front of a mirror and look for any changes in the look, feel or size of the breast, breast swelling, dimpling or puckering of the skin change in the look or feel of the nipple or discharge from the nipple 1. Do once a month, a week after your period 2. Look in the mirror for any asymmetries 3. Touch all portions of your breasts-up and down and left to right 4. Start feeling for lumps or masses 5. Check from the underarm area to the chest wall and sternum 6. Conduct the self-exam standing up or lying down Resulting from edema, an orange peel appearance of the breast is associated with cancer Redness, mild-scarring, and flaking of the nipple may be seen early in Paget’s disease of the nipple and then disappear. However, this does not mean that the disease is gone. Tingling, itching, increased sensitivity, burning, discharge and pain in the nipple are late signs of Paget’s disease Malignancy Malignancy malignancy Irregular, firm, hard, and not defined masses that may be fixed or mobile. They are not usually under and usually occur after age 50 Lobular, ovoid, or round. They are firm, well-defined, seldom tender, and usually singular and mobile. Common between puberty and menopause Also called fibrocystic breast disease, benign breast disease is marked by round, elastic, defined, tender and mobile cysts; 30 to menopause 10 - ASSESSING THE RESPIRATORY SYSTEM Techniques Preparing the Client 1. 2. 3. 4. • • • Equipment • • • • Inspection Palpation ✓ Many breathing difficulties can be seen during this step ✓ Systemic problems can be detected during the assessment Percussion Auscultation Have the client remove all clothing from the waist up and put on an examination gown or drape. The gown should open down the back, and is used to limit exposure. Examination of a female client’s chest may create anxiety because of embarrassment related to breast exposure. Explain that exposure of the entire chest is necessary during some parts of the examination to further ease client anxiety. Ask the client to SIT IN AN UPRIGHT POSITION with arms relaxed at the sides Examination gown and drape Gloves Stethoscope MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A Key Points Inspection • • • • • • • • • • • • • • • Posterior Thorax: Inspection 5. Inspect Spinal alignment for deformities Deformities of the Thorax 6. Posterior Thorax: Palpation Chest Excursion 7. Palpate chest for vocal fremitus - faintly perceptible vibration felt through the chest well when the client speaks. Light Source Mask Skin Marker Metric Ruler Provide privacy Keep your hands warm Remain nonjudgmental regarding the client’s habits and lifestyle particularly smoking. At the same time educate and inform about risks such as lung CA, COPD and related habits Inspect for nasal flaring and pursed lip breathing o Nasal flaring is seen with labored respirations (especially in small children) and is indicative of hypoxia. Pursed lip breathing may be seen in asthma, emphysema, or CHF as a physiologic response to help slow down expiration and keep alveoli open longer Pursed lip breathing - slowly inhale through your nose and gently exhale through pursed lips. Observe color of face, lips, and chest The client has evenly colored skin tone, without unusual or prominent discoloration Ruddy to purple complexion may be seen in clients with COPD or CHF as a result of polycythemia. Cyanosis may be seen if client is cold or hypoxic. Inspect color and shape of nails. Pink tones should be seen in the nailbeds. • Inspect ✓mucous membranes for pallor in patients with respiratory distress as in asthma ✓ The shape and symmetry of the thorax from posterior and lateral views • Compare the anteroposterior diameter to the transverse diameter Normal findings: AP diameter is > Transverse Diameter • Anteroposterior to transverse diameter in ration of 1:2. • Adult thorax is oval. • Chest is symmetric. Deviations from Normal: ✓ Barrel chest ✓ Increased anteroposterior to transverse diameter ✓ Chest asymmetric ✓ Have the client stand ✓ From a lateral position, observe the three normal curvatures: cervical, thoracic, and lumbar ✓ To assess for lateral deviation of the spine (scoliosis) observe the standing client ✓ Have the client bend forward at the waist and observe from behind Normal Findings ✓ Spinous process should be aligned ✓ Thorax symmetrical with no deformities Deviations ✓ Exaggerated spinal Curvatures (kyphosis, lordosis) • Barrel chest : chest appears to be partially inflated all the time, with the rib cage broadened as if in the middle of a deep breath. • Pectus carinatum : is a genetic disorder of the chest wall. It makes the chest jut out. • Pectus excavatum: a congenital deformity of the chest wall that causes several ribs and the breastbone (sternum) to grow in an inward direction. • Scoliosis : abnormal lateral curvature of the spine. It is most often diagnosed in childhood or early adolescence • Kyphosis : is an exaggerated, forward rounding of the back 1. Temperature and integrity of all chest skin 2. Chest areas for bulges, tenderness, or abnormal movements • Avoid deep palpation for painful areas, especially if a fractured rib is suspected. Normally intact, uniform temperature Deviations from normal: • Skin lesions • Areas of Hyperthermia Palpate the posterior chest for respiratory excursion (thoracic expansion) • Place the palms of both hands over the lower thorax, with thumbs adjacent to the spine and fingers stretched laterally. • Ask the client to take a deep breath while observing the movement of your hands and any lag in movement NF: • Full and symmetric chest expansion. • Thumbs move apart an equal distance and at the same time; • Normally thumb separate 3 to 5 cm ( 1-½ to 2 in.) during deep inspiration Deviations from Normal: • Asymmetric/ or decreased chest expansion • Place the palmar surfaces of fingertips or the ulnar aspect of hand or closed fist on the posterior chest, staring near the apex of the lungs • Ask the client to repeat such words as “blue moon” or “one, two, three” • Repeat the two steps, moving hands sequentially to the base of the lungs • Compare the fremitus on both lungs and between the apex and the base of each lung 1) Using one hand and moving it from one side of the client to the corresponding area on the other side. 2) Using two hands that are placed simultaneously on the corresponding areas of each side of the chest. MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A Percussing the posterior chest 7. Percuss the posterior thorax Posterior thorax: Auscultation Anterior Thorax (Inspection) Auscultate anterior chest Auscultation of anterior chest NF: ✓Bilateral symmetry of vocal fremitus. ✓Fremitus heard most clearly at the apex of the lungs. Deviations from normal: • Decreased or absent fremitus (pneumothorax) • Increased fremitus in vocal fremitus indicates denser lung tissue, which can be caused by consolidation in diseases like pneumonia. • Keep the middle finger firmly over the chest wall along intercostal space and tap chest over distal interphalangeal joint with middle finger of the opposite hand. • Tap 2-3 times in a row. Ask the patient to exhale and hold it. ▪ Percuss the chest on both sides, down their back in the intercostal margins (bone will be dull), starting below the scapula, until sounds change from resonant to dull (lungs are resonant, solid organs should be dull). • Percussion performed over most of the lung area produces • A resonant sound, which is a low pitched, hollow sound. • Any dullness or hyper-resonance is indicative of lung pathology, such as pleural effusion ( fluid in the layers of the pleura outside the lungs) or pneumothorax(collapsed lung) Deviations from normal • Asymmetry in percussion • Areas of dullness or flatness over lung tissue or mass • When the posterior thorax is examined, the patient's arms should be crossed anteriorly to move the scapula's laterally as much as possible. • Comparing one side to the other is a helpful maneuver to identify the patient's "normal” 1. Inspect breathing patterns (respiratory rate and rhythm) 2. Palpate the anterior chest for respiratory excursion ✓ Place the palms of both your hands on the lower thorax, with your fingers laterally along the lower rib cage and your thumbs along the coastal margins ✓ Ask the client to take a deep breath while you observe the movement of your hands To auscultate anterior chest: ✓ When the posterior thorax is examined, the patient's arms should be crossed anteriorly to move the scapula's laterally as much as possible. ✓ Comparing one side to the other is a helpful maneuver to identify the patient's "normal. ✓ Listen at each point to the breath sounds during a complete inspiration and expiration ✓ Compare findings at each point with the corresponding point on the opposite side of the chest NF: 1. Vesicular breath sounds – low, pitched, normal breath sounds, heard in the periphery of the lungs 2. Bronchovesicular breath sounds – medium pitched sounds, commonly heard over upper 3rd of the anterior chest 3. Bronchial breath sounds – arise from the tracheobronchial tree, Has a higher pitch, louder, inspiration and expiration are equal. Deviations from normal: • Adventitious breath sounds • Absence of breath sounds (collapsed and surgically removed lung lobes) Inspecting breathing pattern Normal Breath sounds Adventitious Breath Sounds 4 Most Common Abnormal Breath Sounds Anterior Chest: Palpation NF: Quiet, rhythmic and effortless respirations Deviations: Labored breathing, use of accessory muscles 1. Bronchial breaths sounds – heard over the tracheobronchial tree 2. Vesicular breath sounds – heard over the lung tissue 1. Rales (or crackles) • Small clicking, bubbling, or rattling sounds in the lungs. • Produced by bubbling air through the alveoli, bronchioles bronchi • Generated from small airways. a. Fine rales – terminal bronchioles and alveoli, sounds like hair being rubbed between fingers b. Medium rales – larger air passages, bubbling sound of opening a carbonated beverage c. Coarse rales – louder and lower-pitched from larger passages 2. Rhonchi • Sounds that resemble snoring. • Produced by air travelling through narrowed passages or through mucus in the passages a. Fine R b. Coarse R c. Sibilant rhonchi (wheezes) due to constricted airways 3. Friction rub • Coarse grating sound • Inflamed surfaces of the pleura rub together during respirations 1. Rales – Small clicking, bubbling, or rattling sounds in the lungs. They are heard when a person breathes in (inhales). 2. Rhonchi: Coarse loud sounds, that resemble snoring. Originates from upper airways. 3. Stridor: Wheeze-like sound heard when a person breathes Originates from upper airways. 4. Wheezing. High-pitched sounds produced by narrowed airways • • Palpate tactile fremitus Same manner as in posterior chest MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A NF: Anterior Chest: percussion ✓ Same as posterior vocal fremitus ✓ Fremitus is normally decreased over heart and breast tissues Deviations from Normal: Same as posterior fremitus NF: • Percussion note resonate down to the sixth rib at the level of the diaphragm • Flat over areas of heavy muscle and bone • Dull on areas over the heart liver and tympanic over the underlying stomach Deviations from Normal: Asymmetry in percussion notes. Areas of dullness or flatness over lung tissue 11 - ASSESSING THE CARDIOVASCULAR SYSTEM 5 AREAS FOR LISTENING Assessing the Heart and Blood Vessels • Aortic - right 2nd ICS • Pulmonic – left 2nd ICS • ERBS Point – left 3rd ICS • Tricuspid – lower left 4th ICS • Mitral – left 5th ICS MCL Includes: • Inspection and palpation of precordium • Auscultation of the heart in four anatomic sites • Palpation and auscultation of the carotid artery • Inspection of the jugular veins ASSESSING THE HEART & CENTRAL BLOOD VESSELS 1. Inspect and palpate precordium for presence of abnormal pulsations. ✓ Palpation is performed to evaluate the characteristics of the right and left ventricles. NORMAL FINDINGS: 1. Aortic and pulmonic areas: ✓ No pulsations. 2. Tricuspid area: ✓ No pulsations 3. Apical area: ✓ Pulsations visible over the apical area in 50% of adult’s Epigastric area: DEVIATIONS FROM NORMAL: o Presence of pulsations o Presence of pulsations in tricuspid area (enlarged right ventricle) o PMI displaced laterally or lower (indicates enlarged heart) o Bounding abdominal pulsations (e.g., aortic aneurysm) Point of Maximal Impulse (PMI) • • 2. Auscultate heart in four anatomic sites. is at the fifth intercostal space at the midclavicular line. when dilated cardiomyopathy is present, this can be shifted laterally. Two normal heart sounds that should be elicited in auscultation: • • • • S1 (lub) 1st heart sound marks the beginning of systole). Closure of the mitral and tricuspid valves. Best heard at the tricuspid (Left lower sternal border & Cardiac apex) S2 (dub). 2ndheart sound marks end of systole beginning of diastole. Closure of the aortic and pulmonic valve. ANY ABNORMAL SOUND OUTSIDE FROM S1 AND S2 WILL PRODUCE S3 AND S4 WHICH IS YOUR GALLOP SOUND HEART SOUNDS S1 - TRICUSPID & MITRAL CLOSE = “LUBB” S2 - AORTIC & PUMNONIC CLOSE = “DUBB” GALLOP SOUNDS S3 (VENTRICULAR GALLOP) S4 (ATRIAL GALLOP) NORMAL FINDINGS: o Heart sounds heard at all sites. o Usually louder at apical area MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A o o o S2 usually heard at all sites. Usually louder at base of heart S3 in children and young adults DEVIATIONS FROM NORMAL o Increased or decreased intensity. o Varying intensity with different beats o Increased intensity at aortic area and pulmonic area o S3 in older adults o S4 may be a sign of hypertension 3. Assess apical pulse. 4. Auscultate the carotid artery to determine the presence of a bruit. 5. Palpate and auscultate the carotid artery Apical pulse: • Normal pulse rate: 60 to 100 beats/ min • pulse site on the left side of the chest over the pointed end, or apex, of the heart. ✓ No sound heard on auscultation. DEVIATIONS FROM NORMAL: o Presence of bruit in one or both arteries (suggests occlusive artery disease) o Bruit –a murmur, an audible vascular sound associated with turbulent blood flow. Palpate the carotid artery, using extreme caution. 1. Palpate one side at a time. 2. Gently tilt the head to relax the sternomastoid muscle. 3. Palpate the carotid artery by placing your fingers near the upper neck between the sternomastoid and trachea roughly at the level of cricoid cartilage. 4. Repeat the procedure on the opposite side. NORMAL FINDINGS: o Symmetric pulse volumes o Full pulsations, thrusting quality. o Quality remains same when client breathes, turns head, and changes from sitting to supine position. o Elastic arterial wall DEVIATIONS FROM NORMAL: o Asymmetric volumes (possible stenosis or thrombosis) o Decreased pulsations (impaired left cardiac output) o Increased pulsations JUGULAR VEINS 1. Inspect jugular veins for distention while: Client is placed in a semifowler’s position (30 to 45 degrees angle with head supported on a small pillow. NORMAL FINDINGS: o Veins not visible (indicating right side of heart is functioning normally) DEVIATIONS FROM NORMAL: o Veins visibly distended (advanced cardiopulmonary disease) If jugular vein distention is present, assess the jugular venous pressure (JVP) • Locate the highest visible point of distention of the internal jugular vein. • Measure the vertical height of this point in centimeters from the sternal angle, the point at which the clavicles meet. Repeat on the other side. DEVIATIONS: o Bilateral measurements above 3 to 4cm, are considered elevated (indicate right-sided heart failure) o Unilateral distention (indicates local obstruction) 12 - ASSESSING THE PERIPHERAL-VASCULAR SYSTEM ASSESSING THE UPPER EXTREMITIES(ARMS) 1. Inspection: • Observe skin over extremities for: ✓ Color ✓ Pallor ✓ rubor (redness) ✓ hair distribution • Inspect the arms for any superficial vessels. MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A NORMAL FINDINGS: o Extremities symmetrical, even in color o Skin is warm and moist. • • 2. Palpation • Note temperature of skin over extremities, comparing one side to the other. Palpate pulses-radial then brachial for: ✓ Symmetry Test ROM ✓ Full ROM ✓ normal muscle strength ✓ Arms symmetric in size NORMAL FINDINGS: O O Radial pulses on both arms present and equal. Normal pulse rate per minute: 60 to 100 beats per minute Qualities of pulse Amplitude(force) of pulses 3+ increased, full, bounding. 2+ normal (regular rhythm, equal intervals between pulsations) 1+ weak 0 absent ASSESSING THE PULSE • • Methods in assessing the pulse. Data Collected when Assessing the Pulse 1. 2. 3. 4. 5. Palpation. The three fingers are used to assess all peripheral sites except the apical pulse. Auscultation. Health care provider uses a stethoscope or Doppler Ultrasound Stethoscope (DUS). DUS is used for pulses that are difficult to assess. Pulse Rate Pulse Rhythm Pulse Volume o Full or Bounding Pulse o Weak, feeble, or thready Pulse Elasticity of the arterial wall Presence or absence of bilateral equality PERIPHERAL PULSES: SITES IN ASSESSING THE PULSE Determine symmetry of pulse volume SITES IN ASSESSING THE PULSE 1. 2. 3. 4. Femoral (groin), Popliteal (back of the knee), Posterior tibial (ankle), Dorsalis pedis (foot) areas. Other pulses 5. Radial (wrist), 6. Brachial (forearm) Radial Pulse • • • Location: Where the radial artery runs along the radial bone, on the thumb side of the inner aspect of the wrist Position the client’s arm alongside the body, palm downward. Curl 2 to 3 fingers around the wrist on the thumb side and palpate gently. Readily accessible. Temporal Pulse • • • Location: Where the temporal artery passes over the temporal bone of the head. The site is above and away from the midline of the eye. The superficial temporal artery passes upward just in front of the ear Palpate gently, using the tips of 2 to 3 fingers. Used when radial pulse is not accessible. Carotid Pulse • • • At the side of the neck where the carotid artery runs between the trachea and the sternocleidomastoid muscle. Locate the larynx or voice box and slide 2 to 3 fingers off into the groove beside it. Never press both carotids at the same time or press it too hard or too long because this can cause a reflex drop in blood pressure or pulse rate. Used in case of cardiac arrest. Used to determine circulation of the brain. Apical Pulse • At the apex of the heart MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A • • In an Adult, this located on the left side of the chest just about 3 inches to the left of the sternum and at the 4th, 5th or 6th intercostal space (between the ribs). For a child 7 to 9 years old, it is located at the 4th or 5th intercostal space. Before 4 years of age, it is left of the midclavicular line. between 4 and 6 years old, it is at the midclavicular line. Routinely used for infants and children up to 3 years of age. Used to determine discrepancies with radial pulse. Used in conjunction with some medications. Brachial Pulse • • • At inner aspects of the biceps muscle of the arm or medially in the antecubital space. Have the patient rest the arm with palm upward and locate the pulse located near the center of the antecubital space toward the little finger. Used to measure blood pressure. Used during cardiac arrest in infants. Femoral Pulse • • • Where the femoral artery passes alongside the inguinal ligament. You may need to press harder to locate the femoral pulse found about halfway between the anterior superior iliac spine and symphysis pubis, below the inguinal ligament. Respect the client’s privacy when attempting to locate this pulse. Used in case of cardiac arrest. Used for infants and children. Used to determine circulation of a leg. Posterior Tibial Pulse • • • On the medial surface of the ankle where the posterior tibial artery passes behind the medial malleolus Feel for this pulse by curving your finger behind and a little below the medial malleolus of the ankle. Often difficult to feel in obese or edematous clients. Used to determine circulation to the foot Pedal (Dorsalis Pedis) • • • Where the dorsalis pedis artery passes over the bones of the foot, on an imaginary line draw from the middle of the ankle to the space between the big and second toe. Feel the pedal pulse on the dorsum (top) of the foot with foot plantar flexed if possible. Feel gently as this pulse is easily obliterated. You may find the pulse between the middle of the client’s ankle and the space between the big and the second toe. Used to determine circulation to the foot. ABNORMAL FINDINGS: UPPER EXTREMITIES • • • • Cold, clammy, and pale hands and arms. ✓ Indicate vasoconstriction and decreased cardiac output. Edema of upper extremities, ✓ indicate poor venous return or obstruction of lymphatic drainage. Full, bounding pulse (3+) ✓ can occur with exercise, anxiety, fever. Anemia, hyperthyroidism. Weak, thready pulse. ✓ Occurs with shock and peripheral disease. ASSESSING THE LOWER EXTREMITIES Inspection • • • Expose legs, in supine position, keep genitalia covered. Inspect both legs, note skin color, hair distribution, temperature, venous pattern, size (swelling or muscle atrophy) Measure calf circumference with tape measure (if lower leg appear asymmetrical) NORMAL FINDINGS: o o o Hair covers the legs. Venous pattern in legs normally flat and barely visible. Legs symmetric in size, no swelling or atrophy. ABNORMAL FINDINGS: o Legs appear pale (vasoconstriction), reddish with vasodilation; cyanotic(poor oxygenation ). o Skin thin, pallor, cold, loss of hair, ulcers, gangrene in legs (arterial insufficiency) o Bilateral edema in legs (deep vein thrombosis) may indicate systemic illnesses affecting heart or kidneys. o Acute, unilateral painful swelling in the legs indicate deep vein thrombosis. o Brown discoloration in legs * chronic venous stasis due to hemosiderin deposits (a protein compound that stores iron in tissues) from red blood cell degradation. o Venous ulcers (poor venous return) MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A o Palpate peripheral pulses Arterial ulcers on tip of toes, metatarsal heads, and lateral malleoli. To determine symmetry of pulse volume 1. Femoral (groin), 2. Popliteal (back of the knee), 3. Posterior tibial (ankle), 4. Dorsalis pedis (foot) areas NORMAL FINDINGS: o o Inspect the peripheral veins in the arms and legs for: Symmetric pulse volumes Full pulsations DEVIATIONS FROM NORMAL: o Asymmetric volumes o Absence of pulsation o Decreased, weak, thready pulsations (impaired cardiac output) o Thready pulse (a scarcely perceptible and rapid pulse that feels like a fine mobile thread under a palpating finger). o Increased pulse volume (hypertension, high CO, circulatory overload) • presence / appearance of superficial veins when limbs are dependent and when limbs are elevated. NORMAL FINDINGS: o Dependent position: presence of distention and nodular bulges at calves o Limbs elevated: veins collapse. ABNORMAL FINDINGS: Inadequate perfusion to the extremities refers to decreased arterial blood flow to the extremities. Inspect the skin of the hands and feet for color, temperature, edema, and skin changes. Assess the adequacy of arterial flow if arterial insufficiency is suspected. o o o o o Distended veins Tenderness on palpation Pain in calf muscles with forceful dorsiflexion (Positive Homan’s sign) Warm and redness over vein (phlebitis) Swelling of one calf or leg • • Homans's sign is often used in the diagnosis of deep venous thrombosis of the leg. A positive Homans's sign (calf pain at dorsiflexion of the foot) is thought to be associated with the presence of thrombosis. NORMAL FINDINGS: o Skin color pink o Skin temperature not excessively warm o No edema DEVIATIONS FROM NORMAL: o Cyanotic (venous insufficiency) o Pallor that increases with limb elevation o Dusky red color when limb is lowered (arterial insufficiency) o Skin cool (arterial insufficiency} o Marked edema. o Delayed color return NORMAL FINDINGS: skin color pink • Buerger’s test: original color returns in 10 seconds; veins in feet or hands fill in about 15 seconds. • Capillary refill test: immediate return of color DEVIATIONS FROM NORMAL: o Delayed color return or mottled appearance; delayed venous filling; marked redness of arms or legs (indicates arterial insufficiency). 13 - ASSESSING THE ABDOMEN Assessing Abdomen the abdominal assessment sequence: 1. Inspection 2. Auscultation 3. Percuss 4. Palpation MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A Preparation: • Ask patient to void, to promote comfort during the procedure. • Position patient in a supine position, arms on side, bends the knees slightly. • Bending the knees will help to relax the abdomen and make palpation easier. • Expose abdomen, nurse’s hands and diaphragm of the stethoscope must be warm. • Sequence: Inspection, Auscultation, Percussion, Palpation (IAPePa) SEQUENCE OF EXAMINATIONS OF THE QUADRANTS • Inspection of the abdomen: have Patient lie on his back. Right Lower quadrant, right upper quadrant, Left upper quadrant, Left lower quadrant (RLQ, RUQ, LUQ, LLQ) Skin integrity. • unblemished skin, uniform color, striae, surgical scars DEVIATIONS: o presence of rash, lesions, tense glistening skin (ascites, edema) Contour and symmetry: • flat, rounded(convex) scaphoid(concave), symmetric contour. DEVIATIONS: o distended, asymmetric. O Asymmetric contour Observe abdominal movements • symmetric movements caused respiration, • visible peristalsis in very lean people • aortic pulsations in thin persons at epigastric area DEVIATIONS: o limited movement due to pain or disease o Visible peristalsis marked aortic pulsations. Vascular patterns ✓ No visible visual pattern DEVIATIONS: o Visible venous pattern (dilated veins) Auscultate abdomen for: 1. Bowel sounds: • audible bowel sounds heard in 4 quadrants high pitched occurs 5-30 times per minute. • Listen for full 5 minutes if no bowel sounds are heard. DEVIATIONS: absent, hypoactive, or hyperactive bowel sounds 2. Vascular sounds: absence arterial bruits DEVIATIONS: loud bruit over aortic area(aneurysm) 3. Peritoneal friction rubs: absence of friction rubs DEVIATIONS: bruit or renal or iliac arteries Palpate abdomen to detect areas of tenderness. a. Light palpation (depress about 1cm) NORMAL FINDINGS: • No tenderness; relaxed abdomen with smooth, consistent tension DEVIATIONS FROM NORMAL: o tenderness and hypersensitivity o Superficial masses o Localized areas of increased tension b. Deep palpation (1.5 to 2 inches deep) • • • • It is the indentation of the abdomen performed by pressing the distal half of the palmar surfaces of the fingers into the abdominal wall. The abdominal wall may slide back and forth while the fingers move back and forth over the organ being examined. Deeper structures, like the liver, and retro peritoneal organs, like the kidneys, or masses may be felt with this method. In the absence of disease, pressure produced by deep palpation may produce tenderness over the cecum, the sigmoid colon, and the aorta. MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A LIVER PALPATION There are two types of bi manual palpation recommended for palpation of the liver. The first one is the superimposition of the right hand over the left hand. • • • Ask the patient to take 3 normal breaths. Then ask the client to breathe deeply and hold. This would push the liver down to facilitate palpation. Press hand deeply over the RUQ. the second method: • • • • • Palpation of the liver Palpate the liver to detect enlargement and tenderness. Palpate for the liver with one or two hands palm down moving upward 2-3 cm at a time towards the lower costal margin (medial margin of the 7thto 10thribs). Palpate bladder for possible urinary retention Normal Findings: Inspection The examiner’s left hand is placed beneath the client at the level of the right 11th and 12th ribs. Place the examiner’s right hands parallel to the costal margin or the RUQ. An upward pressure is placed beneath the client to push the liver towards the examining right hand, while the right hand is pressing into the abdominal wall. Ask the client to breathe deeply. As the client inspires, the liver maybe felt to slip beneath the examining fingers. NORMAL FINDINGS: • The liver usually cannot be palpated in a normal adult. However, in extremely thin but otherwise well individuals, it may be felt the costal margins. • When the normal liver margin is palpated, it must be smooth, regular in contour, firm, and nontender. • May be palpable, border feels smooth. • No tenderness DEVIATIONS: o Enlarged, smooth but tender. o Nodular (growth of abnormal tissue) or hard o Liver span >12cm or <6cm indicate. o hepatomegaly or cirrhosis (scarring or fibrosis) Have the patient take a deep breath. • • • The liver will move downward due to the downward movement of the diaphragm. Feel for the liver to hit the caudal (tail) aspect of your palpating hand. Palpate area above the pubic symphysis • Not palpable DEVIATIONS FROM NORMAL: o Distended and palpable as smooth, round, tense (indicates urinary retention) • Skin color is uniform, no lesions. • Some clients may have striae or scar. • No venous engorgement. • Contour may be flat, rounded or scaphoid. • Thin clients may have visible peristalsis. • Aortic pulsation maybe visible on thin clients. 14 – ASSESSING THE MUSCULOSKELETAL SYSTEM • • • • • • • • • Inspect the muscles for size. Inspect the muscles and tendons for contractures. Inspect the muscles for tremors. Palpate muscles at rest to determine muscle tonicity. Palpate muscles while the client is active and passive for flaccidity, spasticity, and smoothness of movement. Test muscle strength. Compare the right side with left side. Inspect the skeleton for normal structure and deformities. Palpate the bones to locate any areas of edema or tenderness. Inspect and palpate joints. ASSESSMENT A. Muscles 1. Inspect muscles for: a. Size and Contour • Compare muscles on one side of the body: o Arm, thigh and calf. MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A o Measure muscles with a tape ✓Muscles equal size on sides of the body. Normal findings: ✓Equal size on both sides of the body. 2. Inspect the muscles and tendons for contractures (shortening). 3. Fasciculations (muscle twitching) and tremors 4. Palpate muscles at rest to determine muscle tonicity. 5. Palpate muscles while the client is active and passive for flaccidity, spasticity and smoothness of movement. Deviations from normal: • Atrophy • Hypertrophy Normal findings: ✓No contractures (hardening of muscles) Deviations from normal: • Malposition of body parts ( foot drop ( foot flexed downward) • Inspect any tremors of the hands and arms by having the client hold arms out in front of the body. Normal findings : • No fasciculations or tremors. Deviations from normal: • Presence of fasciculation or tremor. ✓Normally firm. Deviations from normal : • Atonic (lack of muscle tone, limp) Normal findings: ✓Smooth coordinated movements. Deviations from normal: • Flaccidity/ flaccid muscles ( lacking firmness, hanging limply) • Spasticity (abnormal increase in muscle tone / stiffness of muscle) Testing for spasticity in the arms: • While still supporting the elbow, passively flex and extend the elbow. • Use same technique on both arms. • If tone is normal, there will be no resistant to these movements. • 6. Test muscle strength. • • Compare the right side with left side. ✓Normally equal strength on each body. Test the strength of each muscle groups for each joint. Ask client to flex and hold while applying opposing force. Normal findings: o Muscle strength is equal bilaterally and fully resists opposing force. MRC MUSCLE POWER SCALE Assessing the power of the upper and lower limb muscles is a crucial component of the neurological exam. The MRC muscle power scale is an important tool that helps in communication our examination findings. Score 0 1 2 3 4 5 Description No contraction Flicker or trace of contraction Active movement only with gravity eliminated Active movement against gravity Active movement against gravity and resistance Normal power B. Bones 1. Inspect the skeleton for normal structure and deformities. 2. Palpate the bones to locate any Normal: areas of edema or tenderness. ✓No deformities Deviations from normal: • Bones misaligned. C. Joints 1. Inspect and palpate joint for swelling, tenderness, smoothness of movement, crepitation( crackling or rattling sound) and presence of nodules. ✓Normally no swelling, redness, masses or deformities in the joints. Deviations: • One or more swollen joints (excess joint fluid). • Presence of tenderness, swelling, crepitation, and presence of nodules. ABNORMAL FINDINGS: JOINTS • • • • • • Swelling in the joints ( excess joint fluid effusion ) Deformities Dislocation – complete displacement of a joint. Subluxation- partial displacement of a joint. Contracture- shortening of a muscle leading to a limited ROM of joint. Ankylosis – stiffness or fixation of a joint. MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A • 2. Assess joint range of motion. Ask the client to move selected body parts ( ROM). If available, use a goniometer to measure the angle of the joint in degrees. ✓Normally joints move smoothly, no tenderness, pain and crepitation. Deviations: • Limited ROM in one or more joints • Limitations in ROM may suggest articular disease or injury. 15 - ASSESSING THE NEUROLOGICAL SYSTEM ASSESSING THE NEUROLOGICAL SYSTEM • • Also called a neuro exam, is an evaluation of a person's nervous system that can be done in the healthcare provider's office. It may be done with instruments, such as lights and reflex hammers. It usually does not cause any pain to the patient. PREPARATION • Assemble equipment: ✓ Sugar, salt, lemon juice, quinine flavors ✓ Percussion hammer ✓ Tongue depressors (for testing pain sensation) ✓ Wisps of cotton, to assess light touch sensation. ✓ Test tubes of hot and cold water, for skin temperature assessment (optional) • Pins or needles for tactile discrimination PROCEDURE • Introduce yourself and verify the client’s identity. Explain to the client what you are going to do, why it is necessary, and how the client can cooperate. • Perform hand hygiene and observe other appropriate infection control procedures. • Provide for client privacy. • Inquire if the client has any history of the following: ✓ Presence of pain in the head, back, or extremities, as well as onset and aggravating and alleviating factors • Disorientation to time, place, or person ✓ Speech disorders ✓ Any history of loss of consciousness, fainting, convulsions, trauma, tingling or numbness, tremors or tics, limping, paralysis, uncontrolled muscle movements, loss of memory, or mood swings ✓ Problems with smell, vision, taste, touch, or hearing INSPECTION • Assess patient’s overall neurological status by observing there: ✓ general appearance ✓ posture ✓ ability to walk. ✓ personal hygiene • Level of orientation is assessed and other standardized tools to evaluate a patient’s mental status may be used. ✓ Glasgow Coma Scale (GCS) • Patient’s cerebellar function is assessed by observing their gait and balance. 1. Mental Status Current mental capacity: • Through evaluation of general appearance (age, ethnicity. Height, weight, any physical deformities) ✓ Unusual behavior ✓ Mood ✓ Unusual, bizarre beliefs (perceptions and hallucinations) ✓ All aspects of cognition (attention, orientation, memory). a. Language If the client displays difficulty speaking: • Point to common objects and ask the client to name them. • Ask the client to read some words and to match the printed and written words with pictures. b. Memory Divided into three abilities: 1. IMMEDIATE MEMORY • Assess immediate memory by giving the patient three unrelated words to remember such as: pencil, grape, and car. • Have him repeat the words and ask him to remember them. • After 5 minutes ask him to repeat the words back to you. 2. RECENT MEMORY • Ask patient to describe something that happened in the last few days. • Ask how what he had breakfast. MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A 3. 4. Attention Span and Calculation • • 5. Level of Consciousness ✓ ✓ ✓ ✓ ✓ ✓ REMOTE MEMORY • Requires verification from another party. • Birthdates of children • Events Test the ability to concentrate or attention span by asking the client to recite the alphabet or to count backward from 100. Test the ability to calculate by asking the client to subtract 7 or 3 progressively from 100—i.e., 100, 93, 86, 79, or 100, 97, 94. Apply the Glasgow Coma Scale: Standardized, objective assessment that describes level of consciousness by giving a numeric value. Scale is divided into 3 areas: Eye opening Verbal response Motor response DECEREBRATE VS DECORTICATE POSTURING • Signs of DECEREBRATE POSTURING ✓ Head and neck are arched. ✓ Legs are straight. ✓ Toes are pointed downwards. ✓ Arms are straight, extended and hands are curled. • Signs of DECORTICATE POSTURING ✓ closed hands. ✓ legs are internally rotated. ✓ feet turned inward. ✓ arms are adducted and flexed against the chest. GLASGOW COMA SCALE • • • • ABOVE 7: NORMAL GCS BELOW 7: SEMI COMA 5-6: COMA 3-4: DEEP COMA CRANIAL NERVE ASSESSMENT (CN I-XII) CRANIAL NERVE I— OLFACTORY NERVE • • Test sense of smell. Ask client to close eyes and identify different mild aromas, such as coffee and vanilla. NORMAL FINDING: o Can identify an odor on each side of the nose. ABNORMAL FINDINGS: o Anosmia –loss of sense of smell. CRANIAL NERVE II— OPTIC NERVE CRANIAL NERVE III— OCULOMOTOR o Unilateral loss of sense of smell in the absence of nasal disease is neurogenic anosmia. • • Test visual acuity test of the visual field. Ask the client to read Snellen’s chart; check visual fields by confrontation and conduct an ophthalmoscopic examination. o o ABNORMAL FINDINGS: Patient unable to see the pencil or finger of examiner (loss of visual field) Papilledema (Choked disc) Increase ICP • Assess six ocular movements and pupil reaction. MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A CRANIAL NERVE IV— TROCHLEAR CRANIAL NERVE V— TRIGEMINAL • O NORMAL FINDING: PERRLA (PUPILS EQUAL, ROUND, REACTIVE TO LIGHT AND ACCOMMODATION) o o o o o o ABNORMAL FINDINGS: Dilated pupils. Dilated fixed pupils. Constricted/ pinpoint pupils. Unequal response or no response to light Absence of constriction or convergence Asymmetric response • Assess six ocular movements by the six cardinal positions of gaze. o ABNORMAL FINDINGS: nystagmus, ptosis, strabismus motor function: Muscles of mastication (Ask client to clench teeth) palpate temporal and masseter muscles) • While client looks upward, lightly touch the lateral sclera of the eye to elicit the blink reflex. • To test light sensation, have the client close eyes, and wipe a wisp of cotton over client’s forehead and paranasal sinuses. • To test deep sensation, use alternating blunt and sharp ends of a safety pin over same area o o o • CRANIAL NERVE VI— ABDUCENS • CRANIAL NERVE VII— FACIAL NERVE • • ABNORMAL FINDINGS: Decreased strength on one side or both. Asymmetry in the jaw movement Pain when clenching teeth. Assess directions of gaze (Test for accommodation: distant/far object ( to dilate the pupils) then ask patient to shift gaze to gaze at near object examiner’s finger held at 7 to 8 cm (3 inches) from nose. Motor function (observe for movement and facial symmetry) Ask the client to smile, raise the eyebrows, frown, puff out cheeks, and close eyes tightly. Ask the client to identify various tastes placed on the tip and sides of tongue—sugar, salt— and to identify areas of taste. ABNORMAL FINDINGS: muscle weakness of facial muscles. CRANIAL NERVE VIII— AUDITORY (HEARING ACUITY) CRANIAL NERVE IX— GLOSSOPHARYNGEAL (S: taste M: swallowing, gag reflex) • Assess the client’s ability to hear the spoken word and the vibrations of a tuning fork. • The acoustic nerve has two divisions: cochlear and vestibular. 1. The cochlear division is involved in hearing – Do Weber and Rinne Test The vestibular division is involved in the sense of balance, which includes equilibrium, coordination and orientation is space --- First, examine the patients ear canals for obvious blockages or malformation. • Apply tastes on the posterior tongue for identification. Ask the client to move tongue from side to side and up and down. CRANIAL NERVE X— VAGUS (S: Throat sensation M: vocal cords, peristalsis) • Assessed with CN IX; assess the client’s speech for hoarseness. CRANIAL NERVE XI— SPINAL ACCESSORY NERVE (Head and shoulder movement) • Ask the client to shrug shoulders against resistance from your hands and to turn head to the side against resistance from your hand. Repeat for the other side. Cranial Nerve XII— CRANIAL NERVE XII – HYPOGLOSSAL NERVE (Tongue movement) • Ask the client to protrude tongue at midline, then move it side to side. MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A 16 – FEMALE GENITAL & INGUINAL ASSESSMENT Order to be followed • • • • Examination of pubic hair Inspection and palpation of the vulva Examination in the speculum. Pap smear Vaginal examination Preparing the client • The patient should be in the supine position, with the legs apart and supported in the corresponding stirrups, with the buttocks a few centimeters outside the table (also lithotomy position) It is necessary that the patient is properly covered. She has previously emptied her bladder. Ideally, should dress in a backless gown. Ensured that the necessary material is available. The light source and the bench to support a foot must be located in the corresponding place. The examiner’s hands and the speculum will be at an appropriate temperature • • • • • PREPARATION 1. Assemble equipment. PROCEDURE 1. Introduce yourself and verify the client’s identity. 2. Perform hand hygiene, apply gloves, and observe other appropriate infection control procedures. 3. Provide for client privacy. Request the presence of another woman, if desired, required by agency policy, or requested by the client. 4. Determine the client history. • age of onset of menstruation, last menstrual period, regularity of cycle, duration, amount of daily flow, and whether menstruation is painful • incidence of pain during intercourse • vaginal discharge, number of pregnancies; number of live births; labor or delivery complications • urgency and frequency of urination at night; blood in urine, painful urination, incontinence; history of sexually transmitted disease, past and present. 5. Cover the pelvic area with a sheet, or drape at all times when not actually being examined • Position the client supine, with feet elevated on the stirrups of an examination table. • Alternately, assist the client into the dorsal recumbent position with knees flexed and thighs externally rotated. ASSESSMENT 6. Inspect the distribution, amount, and characteristics of the pubic hair. Normal findings: • wide variations; generally kinky in menstruating adult, thinner and straighter after menopause Deviation from normal: • Scant pubic hair (may indicate hormonal problem) • Hair growth should not extend over abdomen. 7. Inspect the skin of the pubic area for parasites, inflammation, swelling, and lesions. 8. Inspect the clitoris, urethral orifice, and vaginal orifice when separating the labia minora. To assess pubic skin adequately, separate the labia majora and labia minora. Deviation from normal • Lice, lesions, scars, fissures, swelling, erythema, excoriations, scars from episiotomies, varicosities or leukoplakia Normal Finding • Clitoris does not exceed 1cm and 2cm length • Urethral orifice appears small slit and is the same color as surrounding tissue • No inflammation or swelling Deviation from normal • Presence of lesions, inflammation swelling or discharge 9. Palpate the inguinal lymph nodes Normal Finding • No enlargement or tenderness Deviation from normal • Enlargement and tenderness 10. Document findings in the client record. CONSIDERATIONS • most practice settings, only inspection of external genitals and palpation of inguinal lymph nodes are performed • If there is an abnormal vaginal discharge, specimens should be taken to check for sexually transmitted disease . • lithotomy position can cause embarrassment - ensure privacy;/ left lateral or Sims’ position with buttocks near edge of bed with right knee flexed. • Empty bladder before the procedure MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A 17 – MALE GENITAL & INGUINAL ASSESSMENT PREPARATION 1. Assemble equipment. PROCEDURE 1. Introduce yourself and verify the client’s identity. Explain to the client what you are going to do, why it is necessary, and how she can cooperate. 2. Perform hand hygiene, apply gloves, and observe other appropriate infection control procedures. 3. Provide for client privacy. Request the presence of another man, if desired, required by agency policy, or requested by client. 4. Determine the client history. o Usual voiding patterns and any changes, bladder control, urinary incontinence, frequency, or urgency. o Abdominal pain o Symptoms of sexually transmitted disease o Swellings that could indicate the presence of a hernia o Family history of nephritis, malignancy of the prostate, or malignancy of the kidney o Done with the patient lying down and then in the standing position. Purpose: To look for hernias and the presence of a varicocele. o Rubber gloves are used, and if not, manual hygiene before and after the exam is a good habit. 5. 6. Cover the pelvic area with a sheet, or drape at all times when not actually being examined. Inspect the distribution, amount, and characteristics of pubic hair. Observe characteristics of the penis : o Skin o Shape o Size 7. Inspect the penile shaft and glans penis for lesions, nodules, swellings, and inflammation. 8. Inspect the urethral meatus for swelling, inflammation, and discharge. ASSESSING THE PENIS Ask client to retract the foreskin: • Smegma: o in case of poor hygiene o a creamy, yellowish-white material will be observed in the balanopreputial sulcus. ✓ The glans must be compressed to produce the opening of the urethral orifice, from which no secretion should flow. EXAMINATIONOF THE PENIS • Gently retract foreskin to expose the glans (the patient may wish to do this themselves) • The foreskin should be supple allowing smooth and painless retraction • Observe the glans penis for any abnormalities • An odorless, curd-like smegma often underlies the foreskin • Inspect both ventral and dorsal surfaces of the shaft of the penis for any abnormalities PENIS Normal findings: • Inspection : ✓The skin normally looks wrinkled, ✓hairless and without lesions. ✓The dorsal vein may be apparent Abnormal findings: • • • • • • Inflammation – appears reddish and swollen. Lesions - nodules, solitary ulcer ( chancre), wartlike papules. Phimosis - foreskin too tight to be pulled over head of the penis) Paraphimosis – foreskin cannot be returned to its original position after being retracted causing swelling and stuck at the tip of the penis. Hypospadias: opening of urethra is on the underside of penis. Epispadias : urethra opens in top of penis rather than the tip. GLANS PENIS • Smooth without lesions. • if male is uncircumcised, ask him to retract the foreskin or you retract it. It should move easily. • Some cheesy smegma may have collected under the foreskin. • After inspection, slide the foreskin back to the original position. • The urethral meatus is positioned centrally, at the tip off the penis . • At the base of the penis, pubic hair distribution is consistent with age. Hair is without lice. • Compress or ask the client to compress the glans slightly to open the urethral meatus to inspect it for discharge. • If the client has reported a discharge, instruct the client to strip the penis from the base to the urethra. 9. Palpate the penis for tenderness, thickening, and nodules. INSPECTION OF THE SCROTUM • Inspect the scrotal skin for: a. Color b. Texture MARCHAN – SALATAN – TANGENTE – MASONG HEALTH ASSESSMENT TRANSES BSN-1A • • Palpate: o Testicles o Epididymis ➢ (with the thumb, index, and middle finger.) Assess the: o Shape o Size o Surface o Consistency Note: it is normal for this palpation to produce visceral pain. • The spermatic cords will also be palpated. In order to confirm the normality of the testicles, transillumination can be used, for which, in a dark environment, a powerful light beam is directed through the scrotum. • Under normal conditions the content allows transillumination. Transillumination of the scrotum: • Performed if a mass or swelling is being assessed. • Turn off light in the room . Shine a strong flashlight from behind the scrotal contents. • Normal scrotal contents do not transilluminate. • Serous fluid transilluminates and shows a red glow, e.g. hydrocele, spermatocele. 10. Inspect the scrotum for appearance, general size, and symmetry. To facilitate inspection of the scrotum during a physical examination, ask the client to hold the penis out of the way. • Inspect all skin surfaces by spreading the rugated surface skin and lifting the scrotum as needed to observe posterior surfaces. Palpate the scrotum to assess the status of underlying testes, epididymis, and spermatic cord. • 11 .Palpate both testes simultaneously for comparative purposes. SCROTUM • Scrotal contents should slide easily during palpation. • Testes normally feels oval, firm and rubbery, smooth and equal bilaterally. Freely movable and slightly tender to moderate pressure. • Each epididymis normally feels discrete, softer than the testis, smooth non tender. • Spermatic cord feel smooth to touch and non-tender. Abnormal findings: scrotum 12. Inspect both inguinal areas for bulges while the client is standing, if possible. 13. Palpate hernias. RECTAL EXAMINATION • • • • • • • • • • Scrotal swelling, may indicate heart failure, renal failure or local inflammation. Lesions are present Cryptorchidism/ undescended testis) Atrophied testis- small and soft Fixed testis Nodules on testis or epididymis. Marked tenderness Thickened spermatic cord, soft swollen and tortuous cord First, have the client remain at rest. Next, have the client hold his breath and strain or bear down, as though having a bowel movement. Men over 40 years of age. The objective of the maneuver must be explained to the patient and in this way he will only experience slight discomfort. RECTAL DIGITAL EXAM DIGITAL RECTAL EXAMINATION (DRE) Position: 1. Left lateral decubitus - with the left leg partially flexed and the right leg frankly flexed , the left arm crossed under the chest and the right arm hanging over the table. 2. Knee-shoulder position, in which the patient rests both knees separately on the examining table and the left shoulder, with the left arm underneath, also leans on the table explorer; the ankles and feet extend off the table • • • • Performed with the patient in a standing position. At the edge of the bed. the patient, rests his hands or elbows on the bed. The region must be well lit to properly view the anal area The examiner, with the gloved right hand, inserts the lubricated index finger through the anal sphincter, while the left hand separates the buttock The anal sphincter closes around the explorer finger and begins by palpating the lateral and posterior aspects of the rectum, which should have a smooth surface and may contain fecal matter Then the anterior wall of the rectum is palpated to evaluate the characteristics of the prostate, its shape, lobes, size, surface, consistency and sensitivity. Taking into account that its palpation can arouse the desire to void. The examiner finger should be gently withdrawn, observing the remains of material to look for the presence of blood in the stool. The patient is offered gauze to remove excess petroleum jelly. • • • • 14. Document findings in the client record.