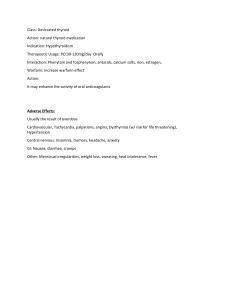
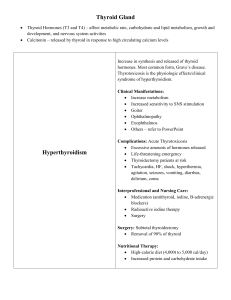
Week 4 Mini Case Study TS is a 48 year old female who presents to the ED via ambulance after falling at work. Since T.S. fell and appears to have hit her head I would ask her the following additional questions: How did you feel just before you blacked out? After? Any history of illness? LMP? Any symptoms of nausea, vomiting, or dizziness afterwards? Any neck pain? Visual disturbances? Able to move all extremities? Numbness or tingling in any of your extremities? Are you taking any medications? Any new medications? Cardiac history? Family history? I would focus on head and neck and neuro assessments. Check Blood sugar Inspect and palpate head. Auscultate the thyroid gland for bruit Check range of motion after xray and ct to clear c-collar Other tests indicated: Check blood sugar Labs including T3and T4 Xray of head Ct of head/neck r/o cervical spine fracture Ultrasound of thyroid EKG Cardiac monitor SOAP Subjective A co-worker who accompanies her states she “blacked out” for about 30 seconds and when she woke up “she didn’t know where she was.” Her co-worker was unsure if she hit her head; she only heard her fall in the break room. Her co-worker also states that TS has been agitated and moody lately. Complaining of an occipital headache. She denies previous fainting episodes but states that over the past two weeks, she has been dizzy and ‘jittery’. She complains of being tired but unable to sleep well. Pt felt dizzy afterwards. No history of illness. TS asks if the air conditioning could be turned on despite a cool temperature in the room. She denies any significant medical history. Pt complains of being consistently hungry and never being satisfied. No visual disturbances. AllergiesNKDA. Pt currently taking no medications. No family history of cardiac problems. Mother had thyroidectomy 2010 due to suspicious goiter that was benign in nature. Mother also had Graves’ disease. LMP: pt states “my periods have been irregular recently”. Objective Vital signs: VS temp 99.7 oral, HR 124 regular, BP 148/66 seated, RR 24, O2 sat on RA 93% FSBS: 85 General appearance: warm, moist skin, anxious, mucous membrane moist. Head: Swelling on her left occipital area, tenderness on palpation. Thinning hair with head tilted slightly to left. Point tenderness over the left occipital area Face: flush complexion. Eyes: Mild exophthalmos, staring unblinking appearance. Neck: mildly enlarged cervical lymph nodes-enlarged bilaterally firm, non-tender and mobile. Spasm in left cervical extensor muscles. Diffusely enlarged, multi-nodular, firm, non-tender thyroid. Presence of bruit auscultated over thyroid. Neuro: Glasgow: 15. A & O x 3. Able to move all extremities without resistance. No numbness or tingling. No difficulty swallowing. Fine tremor 1+ and brisk reflexes, PERRLA, photophobia, no visual changes. Cardiac: The cardiac examination is remarkable for a systolic murmur 2/6. EKG unremarkable. Cardiac monitor shows sinus tach without PVC’s. Respiratory: lungs clear bilaterally Labs: Serum T4 – 17 mcg/dL; TSH undetectable; CBC – wnl Xray and CT: Unremarkable Ultrasound: Impression: hypervascular, multinodular thyroid with large complex nodule measuring 3.5 x 2 x 2.9 cm. Recommend biopsy. Enlarged lymph nodes with normal appearance seen in lateral compartments bilaterally. Assessment: Hypothyroidism R/T lab results Knowledge deficit R/T disease process Plan: Pt most likely has hyperthyroidism. Given the exophthalmos and labs T.S. most closely relates to Graves disease. Graves disease is an “increased production of thyroid hormones causes an increased metabolic rate. This is manifested by goiter and exophthalmos (bulging eyeballs). Symptoms include nervousness, fatigue, weight loss, muscle cramps, and heat intolerance. Signs include forceful tachycardia; shortness of breath; excessive sweating; fine muscle tremors; thin silky hair, warm, moist skin; infrequent blinking; and staring appearance” (Jarvis, 2016, p. 277) My concern for this patient would be to treat symptoms and prevent thyroid storm. It is concerning that she has lost consciousness which is a sign of thyroid storm, close observation is warranted. Due to negative CT scan, c-collar removed. Advise pt to take beta blockers and follow up with endocrinologist to schedule thyroid biopsy and possible a radioactive iodine uptake. Endocrinologist consult. Prescribe anti-thyroid medication Prescribe muscle relaxant or benzodiazepine to help with muscle spasm. Ibuprofen for fever and swelling. Prescribe beta blocker. “Regardless of the cause of hyperthyroidism, the adrenergic symptoms are controlled by beta blockers” (Igor, 2016) Beta blockers would be given because “elevated thyroid hormone levels amplify catecholamine signaling through increased numbers of cell surface betaadrenergic symptoms (e.g. palpitations, heat intolerance, diaphoresis, tremor, stare)” (Igor, 2016). The most common cause of hyperthyroidism is Graves disease which is “an auto-immune disorder in which the thyroid-stimulating antibodies activate thyroid-stimulating hormone (TSH) receptors, triggering thyroid synthesis” (Igor, 2016). Jarvis, C. (2016). Physical Examination and Health Assessment. (7th ed.). St. Louis, MO: Elsevier Kravets, I., 2016. Hyperthyroidism: Diagnosis and Treatment. American Family Physician. Volume 93 (5), pages 363-70.