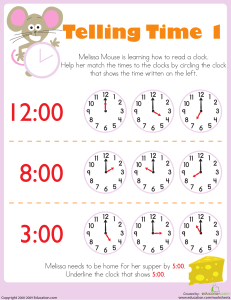
Introduction to Documentation and Informatics Information in the patient’s health record provides an account of their health in the past, is the place where new information about their health is documented, and can provide cues to what their health may be like in the future. Health professionals contribute to the patient’s health record by documenting assessments, identifying problems, prescribing treatment, and evaluating the individual’s response to treatment. Accurate documentation ensures continuity of care, saves time, and minimizes the risk of errors. By completing the documentation and informatics learning activities, you will gain the knowledge and skills needed to: Discuss the purpose of the health record. Explain the difference between the health record and the medical record. Discuss how informatics and technology have impacted documentation of, and access to, an individual’s health record. Adhere to legal guidelines, ethical principles, and nursing standards for documentation. Utilize the 24-hour clock when documenting. Purposes of the Health Record The medical record provides: a means of asynchronous communication for health professionals collaborating on the care of an individual; legal documentation of care encounters; a source to validate the costs of care for reimbursement; a source of information for auditing and monitoring the standards of care provided; data for research; and education. Additionally, most electronic health records (EHRs) provide patients with access to their complete health records, as well. Given the benefit of immediate and complete access to patient-specific information provided by electronic storage of the health record and the risks associated with storing personal information electronically, EHR standards have been developed. It is expected that EHRs will include the following attributes or components: EHR Standards provide a longitudinal or lifetime patient record by linking all patient data from previous healthcare encounters; include a problem list indicating current clinical problems for each healthcare encounter, the number of occurrences associated with all past and current problems, and the current status of each problem; require the use of accepted, standardized measures to evaluate and record health status and functional levels; provide a method for documenting the clinical reasoning or rationale for diagnoses and conclusions that allows clinical decision making to be tracked by all providers who access the record; support confidentiality, privacy, and audit trails; provide continuous access to authorized users at any time; allow multiple healthcare providers access to customized views of patient data at the same time; support links to local or remote information resources, such as databases using the internet or intranet resources based within an organization; support the use of decision analysis tools; support direct entry of patient data by physicians; include mechanisms for measuring the cost and quality of care; and support existing and evolving clinical needs by being flexible and expandable (Hebda et al., 2019). Interprofessional Communication Through Documentation Documentation is the foundation of the electronic health record (EHR)/electronic medical record (EMR) and a primary means of communication for health professionals working with the patient at different points in time. While all disciplines contribute, only the nursing-specific contributions will be discussed next. Charting By Exception (CBE) Many facilities use computer software for documentation as it contributes to the EHR database immediately, allowing anyone with access to the EHR to see the most up-to-date information. Electronic documentation often uses charting by exception. With CBE, normal standards of health have been predefined. This allows a checklist, or flowsheet, to be created with these norms listed. Nurses then place data on the flowsheet to record assessment findings, interventions, and other routine aspects of care. Note the “Legends” area near the bottom that provides clarity on what abbreviations should be used for each item assessed. Also, note the area for signatures used to identify which colleague records the information. When using an EHR, the legends and signature block are often not used. Instead, the documentation is done using a dropdown menu and the software notes which colleague was logged in when the charting was completed. (So log out when you are no longer using a computer and protect your password!) The only time “within normal limits” should be used when documenting is when a patient’s assessment findings meet the defined normal. When they do not, a narrative note is completed to describe how the assessment deviated from the defined norms. You can download a sample “Neurovascular Assessment Flowsheet” below the image to the right. Narrative Documentation Narrative nursing notes that are general in nature can be entered into the health record as free-form text to provide information that is not readily documented elsewhere. Two uses are seen in the example below. Date Time NURSING PROGRESS NOTE 08/08/20XX 14:15 Complete assessment on admission flowsheet. 76year-old male admitted from ED with a left femoral compound fracture resulting from hitting a stopped car while riding his bicycle. Approximate 10-minute loss of consciousness occurred at scene. Currently awake and cooperative. Left leg in traction pending surgical repair. Resting comfortably and denies pain at this time. Expresses concern over lost phone and damage to his bicycle. Patient stated, “I need to call my girlfriend. I may need her help getting up the stairs to my third floor apartment.” Phone provided with instructions on how to get an outside line and the direct number for people to reach him. ----------C. Simpson, RN 08/08/20XX 15:26 Assisted pt. to order dinner ----------L. Pallarino, UAP At 14:15, the RN noted information from the admission assessment, including some that may have been included on the admission assessment record. At 15:26, the UAP noted helping the patient order dinner. Though this may not seem like an activity that needs to be recorded, documenting the assistance allows others to know that the patient was oriented on how to order meals, so they can do that independently. SOAP Notes More often, narrative nursing documentation utilizes a standardized format by which information is organized. One of the most common is the SOAP note, described below. Subjective Data: Information shared by the patient, family member, or another individual; cannot be verified by the nurse. Objective Data: Information that can be assessed and verified by the nurse using their senses. Assessment: The nurse’s hypothesis, or evaluation, of what is happening, based on the cues from the data. Plan: The intended actions to be taken to support the patient’s health. Here is the 14:15 nursing progress note written using the SOAP format. Date Time NURSING PROGRESS NOTE 08/08/20XX 14:15 S: Pt stated “I need to call my girlfriend. I may need her help getting up the stairs to my third floor apartment.” O: Completed assessment on admission flowsheet; expresses concern over lost phone and damage to his bicycle; denies pain at this time. A: Resting comfortably pending surgical repair of leg. P: Maintain comfort; provide pre-op teaching after dinner; phone provided with instructions on how to get an outside line and the direct number for people to reach him. ---------- C. Simpson, RN 08/08/20XX 15:26 Assisted pt. to order dinner ---------- L. Pallarino, UAP Notice that information contained on the flowsheet has been omitted from the SOAP documentation, leaving only the reference to where the complete objective database can be located. When using narrative documentation, it is important to use correct medical terminology, spell correctly, and use only approved abbreviations. Though the main purpose of documentation is to create a record of the patient’s condition, the care provided, and the patient’s response to care, the EHR also serves as a legal account of the patient’s care. So clarity, timeliness, and accuracy matter. Also, notice that each line of text that did not reach the right margin has had a line added to prevent charting after the fact. The SOAP note could be written without starting each section on a new line to avoid leaving these blank spaces at the end of each line. Standards for Documentation The overarching goal when documenting patient care is to include information that is factual, accurate, complete, current, and organized. Using standardized forms to record routine information—such as vital signs, medications, and test results helps—as does using a computerized medical record. No matter how information is being recorded, here are some facts to keep in mind. Expand the tab below to review standards for all documentation. Standards for All Documentation Begin each entry with the date and time. Record all data factually and objectively. This includes observations of a patient’s behavior and the actions of another health professional. Use complete descriptions of assessments and care in an objective manner, avoiding generalizations. Use the patient’s words, in quotes, to record what they have said. This is most important when the patient is expressing emotions or thoughts of harming themselves or someone else. Document consultations with providers that seek to clarify a prescribed intervention. Document only what you have observed or done yourself. Document as care is provided, rather than waiting for the end of the shift. This increases the accuracy of documentation. If a late entry is needed, document the time the charting was completed, then note the time care was provided at the start of the note. Correct all errors when discovered. The process for making a correction in an EHR may vary by software. End each entry with your signature and role (RN; LVN; NA; MD; OT). This step is often completed by the EHR and is linked to your log-in credentials. First initial, last name, SN. (e.g., C. Simpson, RN) Document using correct medical terminology, spelled correctly. It is not necessary to use correct grammar and punctuation, though entries should be clear and concise. Be aware of who is around you when documenting in the electronic health record (EHR). Shield the monitor from the line of sight of others, including colleagues whose access may differ from yours. Do not leave the computer with the screen active, even for a short time. Finally, always protect your computer password. Standards for Written Documentation For written documentation: Draw a single line through any error, write the word error nearby, initial, and date. Record the correct information including the current date/time, then note “Correction to entry of date/time” followed by the correct information. Chart line by line, leaving no blanks. If a line is skipped, place a straight line through it to prevent someone from entering information out of order. If space is left at the end of an entry, draw a line through it, then sign the entry. Write legibly in black ink or as required by the facility. Do not use felt-tip pens or erasable ink. Date Time NURSING PROGRESS NOTE 08/08/20XX 14:15 Complete assessment on admission flowsheet. 76-yearold male admitted from ED with a right (error, cs 08/08/20XX) left femoral compound fracture resulting from hitting a stopped car while riding his bicycle. Approximate 10-minute loss Date Time NURSING PROGRESS NOTE of consciousness occurred at scene. Currently awake and cooperative. Left leg in traction pending surgical repair. Resting comfortably and denies pain at this time. Expresses concern over lost phone and damage to his bicycle. Patient stated, “I need to call my girlfriend. I may need her help getting up the stairs to my third floor apartment.” Phone provided with instructions on how to get an outside line and the direct number for people to reach him. ---------- C. Simpson, RN 08/08/20XX 15:26 Assisted pt. to order dinner --------- L. Pallarino, UAP Confidentiality and Sharing Information Because not all health records are stored electronically, and those that are may not be readily accessible outside of a healthcare system or geographical area, the need to share Health Insurance Portability and Accountability Act (HIPAA) protected Personal Medical Information (PMI) with others caring for an individual exists. Data may only be shared with permission from the patient or legal guardian. Steps to Assure Confidentiality of Shared PMI: Emailing Confirm the email address before sending. Ask for an email reply confirming the information was received. Only send encrypted email. Faxing Place fax machines in a secure area and limit machine access to designated individuals. Use the encryption feature on the fax machine. Encoding transmissions makes it impossible to read confidential information without the encryption key. Confirm the fax number is correct. Use the cover sheet to list the intended recipient(s), the sender, and the phone and fax numbers. Use programmed speed-dial keys to eliminate the chance of a dialing error and misdirected information. Verify the fax number on the transmittal confirmation sheet. Log fax transmissions, if not completed electronically on the machine (Potter et al., 2016). Time at a Glance This table shows the relationship between the time of day and how it is recorded using the 12-hour clock and the 24-hour clock. Time of Day 12-Hour Clock 24-Hour Clock 12 o’clock midnight 12:00 a.m. 00:00 1 o’clock in the morning 1:00 a.m. 01:00 2 o’clock in the morning 2:00 a.m. 02:00 3 o’clock in the morning 3:00 a.m. 03:00 Time of Day 12-Hour Clock 24-Hour Clock 4 o’clock in the morning 4:00 a.m. 04:00 5 o’clock in the morning 5:00 a.m. 05:00 6 o’clock in the morning 6:00 a.m. 06:00 7 o’clock in the morning 7:00 a.m. 07:00 8 o’clock in the morning 8:00 a.m. 08:00 9 o’clock in the morning 9:00 a.m. 09:00 10 o’clock in the morning 10:00 a.m. 10:00 11 o’clock in the morning 11:00 a.m. 11:00 12 o’clock noon 12:00 p.m. 12:00 1 o’clock in the afternoon 1:00 p.m. 13:00 2 o’clock in the afternoon 2:00 p.m. 14:00 3 o’clock in the afternoon 3:00 p.m. 15:00 4 o’clock in the afternoon 4:00 p.m. 16:00 5 o’clock in the afternoon 5:00 p.m. 17:00 6 o’clock in the evening 6:00 p.m. 18:00 Time of Day 12-Hour Clock 24-Hour Clock 7 o’clock in the evening 7:00 p.m. 19:00 8 o’clock in the evening 8:00 p.m. 20:00 9 o’clock in the evening 9:00 p.m. 21:00 10 o’clock in the evening 10:00 p.m. 22:00 11 o’clock in the evening 11:00 p.m. 23:00 Informatics and Data During a Pandemic While the use of informatics and technology has enabled public health officials, government leaders, and the general public to remain informed during the recent global pandemic, the same technology has slowed the testing results for thousands of people in the United States (Barone, 2020). Just as healthcare systems and healthcare providers may use different electronic health record (EHR) software, laboratories have equipment that uses different software to run the same tests. Barone (2020) recently noted that patients in the United States were waiting anywhere from 24 hours to 24 days to receive their COVID-19 test results. The longer wait times were often associated with high demand at some of the laboratories completing testing for areas with increased testing needs. Although labs that were testing under their capacity offered to assist, results were further delayed because the software used by the two labs could not communicate directly. This meant that results were manually entered, which increased the risk of results being reported inaccurately. Because progress tends to result from identified needs, the future of healthcare informatics and data sharing is sure to move forward as this pandemic resolves, putting the world in a stronger position to handle the next global health crisis by giving health professionals the tools needed to work smarter together. Objective data includes: admitted from ED alert and oriented moderately short of breath T 98.4° F (36.9° C) HR 102 RR 23 BP 140/92; SaO2 92% on RA skin warm/dry, no lesions PERRLA bilateral crackles in lungs; heart rate/rhythm regular with occasional irregular beat JVD present bilateral pedal edema abdomen soft, bowel sounds active Subjective data, which can be a bit trickier, includes: stating they are “moderately diabetic” lives alone in assisted living pain level and that it occurs with deep respiration and last bowel movement Why is subjective data tricky? The medical record can reveal if a health provider has diagnosed the client with pre-diabetes and a family member could verify living arrangements. However, until verified, it remains subjective data. It is important to not get distracted by classifying information “correctly” when documenting. Instead, focus on getting information recorded as factually as possible. Factual information consists of the observations the nurse sees, hears, smells, or touches related to the client’s current state of health. Within this documentation, the facts include: the observed burn to the right hand unable to walk a straight line people at the bedside (seen) the client’s statement about pain (heard) the fruity smell to the breath (smelled) the laughter (heard and seen) The statements related to how the injury was sustained (probably shooting off fireworks) and the client’s state of sobriety (obviously drunk) are assumptions based on the facts that it is late on July 4th—a time when many in the U.S. celebrate by lighting fireworks—and the client’s inappropriate laughter, inability to walk a straight line, and the fruity smell of the breath. While it seems logical to make both assumptions, the statements are hypotheses based on the identified cues. Instead of documenting the hypotheses, the nurse uses the cues to question the client about how the hand was injured and inquire if they have used alcohol recently. The answers provided will either confirm the facts (“Yes, I have been drinking”) or negate the hypothesis (“I can’t believe I tripped on a chair and fell into the campfire”). 1 = Risk Present: The fax machine is located in an open hallway that is accessible to anyone on the floor. It should be moved to a more secure location. 2 = Risk Present: Although it is not apparent if the fax was addressed to one or both of these colleagues, the fact that another colleague overheard their conversation and was able to identify the client means a risk is present that others may overhear, as well. 3 = Risk Present: These colleagues are also close enough to overhear the conversation. Although they may have a right to information contained within the shared medical record, it should be accessed in a way that minimizes the risk of breaching confidentiality. In this example, prevention would involve double-checking that the correct fax number of the recipient is correctly placed on the fax cover sheet and double-checking the number typed into the fax machine before hitting the send button. Use of the cover sheet will not prevent mistyping the recipient’s fax number, though it can get the fax to the correct recipient more quickly. Programmed speed-dial keys are helpful for frequently dialed numbers, though that may not have applied in this example. Checking the transmittal confirmation sheet to compare the fax number may have meant the error would be discovered sooner, but it would not have prevented it from being sent to the incorrect number. The entry on 12/13/20XX at 23:30 is out of chronological order. When a narrative entry is needed to reflect care given prior to the most recent timed entry, enter the date and time when the documentation is done, then start the narrative noting that the entry refers to care provided earlier. See correct documentation below for an example. 12/14/20xx 07:10 Refused breakfast due to nausea. Insulin withheld and antiemetic administered.---------J. Collins RN 12/14/20xx 23:30 On 12/13/20xx at 23:30 pt experiencing nausea not relieved by prescribed antiemetic. D. Long, ANP notified and new medication prescribed. --------- S Peters RN Note that the entry on 12/14/20xx at 00:45 contained an error that was properly crossed out and marked with the word error and the writer’s initials. 10 hours is the correct answer. At 22:37 on 8/13, the client’s temperature was 97.8º F (36.6º C), and the last temperature below 98.6º F (37º C) was normal. The most recent temperature was taken the next day at 08:37, which is 10 hours later. The quickest way to “count” hours between days is to add the hours before and after midnight represented by the two times. 22:00 is 2 hours before midnight and 08:00 is 8 hours after midnight. 2 + 8 = 10 hours. Note that no adjustment was needed for the minutes, as they were the same. Although all options represent advantages realized with an EHR, only continuity of care and increased safety directly benefit the client. Healthcare providers benefit from having complete data available when assessing and treating clients whose information is stored in an EHR and the decreased liability realized by the checks and balances of an electronic documentation system. The availability of audit trails and accessible data for research within an electronic record directly benefits auditors and researchers responsible for collecting this data. In the long run, however, clients and health professionals benefit from audits (cost of care covered, systems improvement) and research (deeper knowledge of illness and the human response).