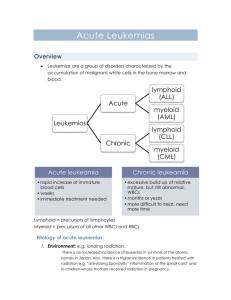
Leukemia Overview: Classification, Types, and Treatment
advertisement

LEUKEMIA abnormal, uncontrolled proliferation and accumulation of more than 1 hematopoietic cell; major signs are fever, weight loss, increased sweating o WBC normal value 4.5-11.5 x 109 L; RBC4.5-6.5 x 1012 L; Platelets 150-450 x 109 / L a generalized neoplastic proliferation or accumulation of leukopoietic cells a condition in which there is a growth of tissue that serves no physiological function with or without the involvement of peripheral blood INFILTRATION of NON - hematopoietic cells CLASSIFICATION: Classified regarding lineage and cell maturity 4 broad categories Acute Myeloid Leukemia (AML) Chronic Myeloid Leukemia (CML) Acute Lymphoblastic Leukemia (ALL) Chronic Lymphocytic Leukemia (CLL) ACCORDING TO ONSET Acute leukemia ✓ if no remission, it is fatal within 3 months ✓ Bone Marrow is packed with primitive cells ✓ Young cells are seen in the bone marrow (blast) Subacute leukemia ✓ involves a longer natural history of 3 - 12 months cells have intermediate differentiation ✓ There are some cells with differentiation Chronic leukemia ✓ survival is for more than 1-year cell types are more differentiated ✓ Cell counts are many ACUTE VS. CHRONIC LEUKEMIA (TABULAR LEUKEMIA) ACCORDING TO CYTOLOGICAL CHARACTERISTICS MYELOID (TABULAR) Organ involvement mostly in chronic leukemia ACCORDING TO CYTOLOGICAL CHARACTERISTICS LYMPHOID Lymphoblastic Leukemia (ALL) CLINICAL FEATURES Acute Myeloid Leukemia (AML) VS. Acute Lymphoblastic Leukemia (ALL) BLAST AML nucleoli( 2 or more) and ALL( 2 or less) LEUKEMIA Problem: Abnormal proliferation of stem cells (variable presentation, Leukocytosis, abnormal circulating cells, proliferation of tissue) Etiology: not completely understood(radiation, chemicals,virus and genetic disposition)MYELOID MYELOID DISORDERS Comprise a group of closely related syndromes characterized by self - perpetuating proliferation of Bone marrow cells Cells involved: Erythroid precursors, Granulocytes, Monocytes, Megakaryocytes proliferation is the ABNORMAL cause is UNKNOWN ALL cell line or a SINGLE cell line predominates(M3) Common Manifestation: Fever, malaise ACUTE MYELOID LEUKEMIA (AML) LEUKEMIA (AML) CLINICAL FEATURES: childhood & adolescent: RARE middle & later years: FREQUENT (MOST COMMON FORM OF ACUTE LEUKEMIA) onset resembles an acute infection or a septic condition granulocytic insufficiency w/ ulceration of mucous membranes (mouth & throat) fever, marked prostration (loss of strength), general malaise Initial Assessment: 500 cell count DIAGNOSIS: More than or equal to (>) 20% of the nucleated cells are blast and/or leukemic cells Usually affected are promyelocyte and promonocyte Distinct in AML: Auer Rods (cytoplasm; elongated and large crystalline) and Phi bodies CLASSIFICATION French-American-British (FAB) Cooperative Group (1976) o Morphology of cells in Romanowsky-stained blood and marrow films o Cytochemical reactions or serum lysozyme levels World Health Organization (WHO) (2001) (CURRENT) o Multilayered approach define morphology, cytogenetics, immunophenotyping o BASIS Recurrent Acquired Cytogenic Abnormalities History of Predisposing Factors/Multilineage AML ✓ Prior to cytotoxic therapy (CHEMOTHERAPY) ✓ Prior MDS (Myelodysplastic syndrome) Morphologic Stratification (FAB) otherwise categorized AML with Recurrent Genetic Abnormalities Affects children and young adults Involvement of a committed precursor High rate of complete remission (good response) with chemotherapy Formation of fusion gene - CHIMERIC PROTEIN (protein not present in the cell types in the body) Example: o AML with t(8:21) –1/3 of M2 cases( children and young adults; Myeloblast with dysplastic granular cytoplasm, Auer rods, hypo granulation, Pseudo-Pelger-Huët) o o o AML with invert (16) –M4 (younger children, extramedullary disease) Acute Promyelocytic Leukemia with t(15:17) – affect specific cell line(promyelocyte) causing hyper granularity and Auer rods; Release of primary granules of promyelocyte causes DIC; good prognosis AML with 11q23 abnormalities AML with Multilineage Dysplasia Arise from Myelodysplastic Syndrome (MDS) or arise de novo but with features of MDS occur in older people and poor prognosis (pancytopenia, hyper/hypo granular, Pseudo-Pelger-Huët cells) > 20% blasts in blood and/or marrow Dysplasia in >50% of cells of at least 2 lineages, Therapy Related AML, Therapy Related Alkylating Agent - Related AML o Chlorambucil, Cyclophosphamide or radiation o Occur 5-10 years after exposure o Poor response to therapy Topoisomerase II Inhibitor - Related AML o After 1-5 years of exposure AML Not Otherwise Classified FAB Classification o based on morphology and cytochemical reaction o requires presence of > 20% blasts in the blood and/or marrow o ¼ of the AML cases are under this classification FAB CLASSIFICATION FAB CLASSIFICATION M0 Acute myeloblastic leukemia, minimally differentiated o o o o CLASSIFICATION Common myeloblst ≥ 20% ALL NUCLEATED CELLS (ANC) are blasts < 3% of blasts are Myeloperoxidase and SBB positive ≥ 20% of blasts are positive for myeloid-associated antigens (CD13 specific for myeloblast, CD33, CD117) M1 Acute myeloblastic leukemia, without maturation o ≥ 20% ANC are blasts o ≥ 90% of (non-erythroid cells) NEC are myeloblasts o ≤ 10% of leukocytes show maturation o ≥ 3% of blasts are positive for peroxidase and SBB o Positive for chloroacetate esterase o M1 is similar to L2 hence, cytochemical differentiation is important M2 Acute myeloblastic leukemia, with maturation o ≥ 20% ANC are myeloblasts o ≥ 10% NEC are promyelocytes or more mature granulocytes o < 20% are of monocytic lineage o Myeloblast represents 20% to 89% of total marrow cells o Usually, > 85% of leukemic cells are positive for peroxidase, SBB and Chloroacetate Esterase (CAE) M3 Acute Promyelocytic Leukemia o > 20% blasts and abnormal granular Promyelocytes o Auer rods and faggot cells (promyelocytes with a cluster of Auer rods in the cytoplasm) o Usually,>85% of leukemic cells are positive for SBB/MPX/CAE o Translocation of 15 and 17 affecting Retinoic Acid Receptor Alpha (RARA) gene is affected o Associated with DIC o Common in Males M4 Acute myelomonocytic leukemia o AKA Naegili’s type of Leukemia o Inversion 16 o ≥ 20% of ANC are myeloblast o Granulocytic series represent 30-80% of NEC o sum of monoblasts, promonocytes and monocytes is more than 20% less than 80% of NECs o ≥ 20% of blasts are positive for SBB/PX/CAE/PAS o positive for aNAE and aNBE M4e Acute Myelomonocytic Leukemia with Eosinophilia o Presence of eosinophilia o Large basophilic granules mixed with smaller eosinophilic granules o There is inversion or dilution of the long arm of chromosome 16 M5a Acute monoblastic leukemia, poorly differentiated o AKA Schilling’s Type of Leukemia o Translocation in 9 and 11(mostly affected) o > 80% of NEC are monoblasts, promonocytes or monocyteS o Negative for SBB/MPO and specific esterase o Strongly positive for nonspecific esterase o Highest incidence of organ involvement M5b Acute monoblastic leukemia, differentiated o > 80% of NEC are monoblasts, promonocytes or monocytes o < 80% of monocytic cells are monoblasts o Negative for SBB/MP and specific esterase o Strongly positive for nonspecific esterase o Reduced number of monoblast o Associated with diffused erythematous rashes M6 Erythroleukemia o > 50% of ANC are erythroblasts o AKA Di Guglielmo syndrome or Erythema Myelosis o Many erythroid precursors are PAS-positive o Affects Chromosome 5 and 7 M7 Acute Megakaryoblastic Leukemia o > 20% of NEC are megakaryoblasts or leukemic cells o platelet peroxidase positive on electron microscopy o positive for glycoproteins Ib or IIb/IIIa o Positive for ANAE but negative with ANBE o Affects Chromosome 21(cytopenia and thrombosis) CHEMOTHERAPY Phases( AML and ALL treatment are similar except M3) 1. Induction of Complete Remission 2. Consolidation 3. Maintenance Remission REMISSION INDUCTION Goal: get rid of all visible leukemia Drugs: 1. Cytosine arabinoside (ara-C) 2. Anthracycline (Daunorubicin) 3. Amsacrine( Resistant AML) Administered in a week Requires hospitalization Target: <5% blast in the marrow after 1-2 week (40- 80% success rate) CONSOLIDATION THERAPY Goal: destroy any remaining leukemia cells and prevent relapse High dose Cytarabine in 5 days 15-40% success rate STEM CELL TRANSPLANT After successful induction 1. Allogenic 2. Autologous Factors considered More intensive induction Availability of tissue match Presence of 1 or more adverse prognostic factors (ex. prior MDS) Young patients Patient’s wish