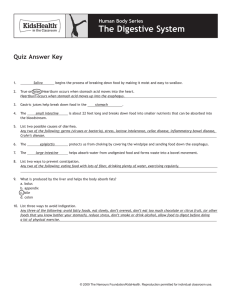
GASTROINTESTINAL DISEASES (PUD, GERD, GASTROENTERITIS, CROHN’S, ULCERATIVE COLITIS, HEMORRHOIDS) _______________________________________ A Seminar Manuscript Presented To the Faculty of the Nursing Department Mrs. Jocelyn A. Cataraja, RN, MN _______________________________________ In Partial Fulfillment of The requirements in SEM - 101 SEMINAR IN NURSING By Angkang, Gene Anthony Balug, Nova Mae Banasig, Trisha Mae Banggo, Farisa Jane Bangonon, Angel Shane Caburnay, Mylah Marie Caiña, Thea Marie Calipusan, Xylen May Casiple, Xynna Confesor, Gerald Vonn Coronel, Elmer Jr. BSN 4K - Group 1 March 07, 2023 TABLE OF CONTENTS INTRODUCTION…………………………………………………….…………………….………4 GOALS AND OBJECTIVES………………………………………….…………………..………5 I. PUD DEFINITION OF CASE………………………………………….………………………..………6 ANATOMY AND PHYSIOLOGY………………………………………….………………...……6 PATHOPHYSIOLOGY………………………………………….…………………………………10 SYMPTOMATOLOGY…………………………….………………………………......…10 ETIOLOGY………………………………………….…………………………………….11 SCHEMATIC DIAGRAM…………………………….…………………………….….…13 NARRATIVE…………………………….……………………………………………..…15 MANAGEMENT……………….………………………………………….……………………....16 DIAGNOSTIC EXAM………………………….…………………………………………16 MEDS…….………………………………………….……………………………..…..…20 TREATMENT…………………………………….…………………………………..…...31 SURGICAL MANAGEMENT…….………………………………………….………..…33 NURSING MANAGEMENT…….………………………………………….…..………..35 REVIEW OF RELATED LITERATURE…….………………………………………….……..…46 II. GERD DEFINITION OF CASE………………………………………….……………………….………50 ANATOMY AND PHYSIOLOGY………………………………………….………………..……50 PATHOPHYSIOLOGY………………………………………….……………………………...…53 SYMPTOMATOLOGY…………………………….……………………………………..53 ETIOLOGY………………………………………….………………………………...…..55 SCHEMATIC DIAGRAM…………………………….………………………………..…58 NARRATIVE…………………………….……………………………………………...…60 MANAGEMENT……………….………………………………………….…………………….…61 DIAGNOSTIC EXAM………………………….……………………………………….…61 MEDS…….………………………………………….………………………………….…66 TREATMENT…………………………………….……………………………………….81 SURGICAL MANAGEMENT…….………………………………………….………..…83 NURSING MANAGEMENT…….………………………………………….……………85 REVIEW OF RELATED LITERATURE…….………………………………………….…..……92 III. GASTROENTERITIS DEFINITION OF CASE………………………………………….………………………………95 ANATOMY AND PHYSIOLOGY………………………………………….………………….…95 PATHOPHYSIOLOGY………………………………………….……………………………..…97 SYMPTOMATOLOGY…………………………….………………………………….…97 1 ETIOLOGY………………………………………….…………………………………...99 SCHEMATIC DIAGRAM…………………………….…………………………………100 NARRATIVE…………………………….…………………………………………….…101 MANAGEMENT……………….………………………………………….…………………...…102 DIAGNOSTIC EXAM………………………….…………………………………..……102 MEDS…….………………………………………….……………………………...……104 TREATMENT…………………………………….……………………………………...115 SURGICAL MANAGEMENT…….………………………………………….…………117 NURSING MANAGEMENT…….………………………………………….…………..117 REVIEW OF RELATED LITERATURE…….…………………………………………….……125 IV. CROHN’S DISEASE DEFINITION OF CASE……………….………………………………………….………....…..127 ANATOMY AND PHYSIOLOGY……………….………………………………………………127 PATHOPHYSIOLOGY………………………………………….…………………………..…..128 SYMPTOMATOLOGY…………………………….……………………………………128 ETIOLOGY………………………………………….……………………………….….129 SCHEMATIC DIAGRAM…………………………….…………………………………132 NARRATIVE…………………………….……………………………………………….134 MANAGEMENT……………….………………………………………….………………..……136 DIAGNOSTIC EXAM………………………….……………………………….………136 MEDS…….………………………………………….………………………..…………146 TREATMENT…………………………………….………………………….………….162 SURGICAL MANAGEMENT…….………………………………………..………..…165 NURSING MANAGEMENT…….………………………………………..……………168 REVIEW OF RELATED LITERATURE…….………………………………….…….……..…176 V. ULCERATIVE COLITIS DEFINITION OF CASE……………….………………………………………….………...…..180 ANATOMY AND PHYSIOLOGY……………….………………………………………………180 PATHOPHYSIOLOGY………………………………………….…………………………..…..183 SYMPTOMATOLOGY…………………………….……………………………………183 ETIOLOGY………………………………………….……………………………….….185 SCHEMATIC DIAGRAM…………………………….…………………………………188 NARRATIVE…………………………….……………………………………………….191 MANAGEMENT……………….………………………………………….……...………………192 DIAGNOSTIC EXAM………………………….………………………...………………192 MEDS…….………………………………………….……………………………………204 TREATMENT…………………………………….……………………………………….232 SURGICAL MANAGEMENT…….………………………………………….………..…240 NURSING MANAGEMENT…….………………………………………….……………246 2 REVIEW OF RELATED LITERATURE…….………………………………………….……..…253 VI. HEMORRHOIDS DEFINITION OF CASE……………….………………………………………….………...…..256 ANATOMY AND PHYSIOLOGY……………….………………………………………………256 PATHOPHYSIOLOGY………………………………………….…………………………..…..257 SYMPTOMATOLOGY…………………………….……………………………………257 ETIOLOGY………………………………………….……………………………….….258 SCHEMATIC DIAGRAM…………………………….…………………………………260 NARRATIVE…………………………….……………………………………………….261 MANAGEMENT……………….………………………………………….……..………………262 DIAGNOSTIC EXAM………………………….…………………….…………………262 MEDS…….………………………………………….……………..……………………263 TREATMENT…………………………………….………………..…………………….277 SURGICAL MANAGEMENT…….……………………………..………….………..…282 NURSING MANAGEMENT…….…………………………..…………….……………283 REVIEW OF RELATED LITERATURE…….………………………..……………….……..…294 REFERENCES……………………………………………………….………………………….297 3 INTRODUCTION Digestion is essential for breaking down food into nutrients, which our body uses for energy, growth, and cell repair. The esophagus, stomach, large and small intestines, liver, pancreas, and gallbladder are all parts of the digestive tract, and disorders of the digestive tract, often known as the gastrointestinal (GI) tract, are known as digestive illnesses. Any health problem that occurs on it has a condition that may range from mild to severe. There are two types: functional and structural. Functional diseases are when the GI tract is checked, it appears normal, but it doesn't function as it should. They are the GI tract's most frequent health issues, including GERD. Structural gastrointestinal diseases are when your bowel looks abnormal upon examination and doesn't work properly, including hemorrhoids and diverticulitis. Sometimes surgery is required to repair the structural defect. In everyone's life, a little digestive distress will occur. Whether it's a meal that doesn't agree with us or a lingering gastrointestinal ailment requiring lifestyle changes and treatment, digestive problems are prevalent. The first sign of problems in the digestive tract often includes bleeding, bloating, constipation, diarrhea, heartburn, nausea and vomiting, pain in the belly, and weight loss or gain. Some digestive diseases include Peptic Ulcer disease, GERD, Gastroenteritis, Crohn's disease, Ulcerative Colitis, and Hemorrhoids. According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), over 60 to 70 million people worldwide suffer from the digestive disorder. It is estimated that 11% of the population in the United States suffers from a chronic digestive disease, with a prevalence rate as high as 35% of those 65 years and over. In a report published by the Philippine Statistics Authority in 2021, infections or complications of the digestive tract are among the top causes of death in the Philippines. The most common, among others, are liver cancer, colorectal cancer, peptic ulcer disease, diarrhea, and stomach ulcer. According to the latest WHO data published in 2020 Peptic Ulcer Disease Deaths in the Philippines reached 6,865 or 1.02% of total deaths. The age adjusted Death Rate is 9.95 per 100,000 of population ranks Philippines #12 in the world and as Peptic ulcer disease ranks 17th in leading cause of death in the philippines. With that, it was proclaimed under Proclamation 930 issued in 2020; President Rodrigo Roa Duterte declared the second week of March of every year as the "Philippine Digestive Health Week." This topic plays a significant role in nursing practice, research, and education, which are necessary to help the patient achieve holistic care. For nursing education, student nurses may acquire information about the condition and the process of learning about Gastrointestinal 4 disease. In addition, this could help health workers and medical students to obtain data and enhance their nursing and medical skills for a patient who has gastrointestinal problems. The data contributed can also be used to provide effective sufficient care; the study can also serve as related literature for further studies that could improve to impart more factual information about Gastrointestinal Disease. Moreover, it will benefit future nursing students encountering patients with similar cases. Furthermore, it could also impart data and recent updates regarding the said disease. Objectives At the end of the seminar conducted by the BSN 4K Group 1, the BSN participants will be able to acquire sufficient knowledge according to research-based information that can contribute to skill development; develop a positive attitude conducive to learning on providing holistic nursing care for patients suffering with gastrointestinal diseases. Specifically, the proponents aim to: a. discuss an overview about gastrointestinal disease and provide relevant statistic data; b. explain what is peptic ulcer disease, GERD, gastroenteritis, crohn's disease, ulcerative colitis, and hemorrhoids; c. indicate the anatomical structures that is correlated with the disease; d. discuss the predisposing and precipitating factors that contribute to the onset of the disease; e. identify the signs and symptoms of the disease; f. trace the pathophysiology of the disease through a schematic diagram; g. list the possible medical, surgical, and nursing management, including diagnostic, laboratory examinations, and interventions; h. present a summary on a related literature published not earlier than 5 years from conduct of this study; i. arrange an alphabetical list of references used in the study using APA format. 5 PEPTIC ULCER DISEASE I. DEFINITION A discontinuity characterizes peptic ulcer disease in the GI tract's inner lining due to pepsin or gastric acid secretion. Usually, the stomach and proximal duodenum are affected. It may involve the lower esophagus, distal duodenum, or jejunum. Patients with gastric ulcers typically have epigastric pain 15 to 30 minutes after eating; in contrast, patients with duodenal ulcers typically experience pain 2 to 3 hours after eating. (Malik et al., 2022). The two major causes of peptic ulcer disease are bacteria which are called helicobacter pylori (H.pylori). This can aggravate the digestive tract, increase acid production, and damage the mucus lining. While certain pain relievers, such as taking aspirin often and for a long time. NSAIDs prevent the body from producing a chemical that aids in protecting the interior walls of the stomach and small intestine from stomach acid. (Pathak, 2021). II. ANATOMY/ PHYSIOLOGY Mouth The digestive process starts in your mouth when you chew. Your salivary glands make saliva, a digestive juice, which moistens food so it moves more easily through your esophagus into your stomach. Saliva also has an enzyme that begins to break down starches in your food. The lips and cheeks help hold food in the mouth and keep it in place for chewing. They are also used in the formation of words for speech. The lips contain numerous sensory receptors that are useful for judging the temperature and texture of foods. The palate is the roof of the oral cavity. It separates the oral cavity from the nasal cavity. The anterior portion, the hard palate, is supported by bone. The posterior portion, the soft palate, is skeletal muscle and connective tissue. Posteriorly, the soft palate ends in a projection called the uvula. During swallowing, the soft palate and uvula move upward to direct food away from the nasal cavity and into the oropharynx. 6 The tongue manipulates food in the mouth and is used in speech. The surface is covered with papillae that provide friction and contain the taste buds. A complete set of deciduous (primary) teeth contains 20 teeth. There are 32 teeth in a complete permanent (secondary) set. The shape of each tooth type corresponds to the way it handles food. Pharynx & Esophagus Food is forced into the pharynx by the tongue. When food reaches the opening, sensory receptors around the fauces respond and initiate an involuntary swallowing reflex. This reflex action has several parts. The uvula is elevated to prevent food from entering the nasopharynx. The epiglottis drops downward to prevent food from entering the larynx and trachea in order to direct the food into the esophagus. Peristaltic movements propel the food from the pharynx into the esophagus. The Stomach The stomach is located in the upper part of the abdomen, just beneath the diaphragm. The stomach is distensible and on a free mesentery; therefore, the size, shape, and position may vary with posture and content. An empty stomach is roughly the size of an open hand and, when distended with food, can fill much of the upper abdomen and may descend into the lower abdomen or pelvis on standing. 7 The duodenum extends from the pylorus to the ligament of Treitz in a sharp curve that almost completes a circle. It is so named because it is about equal in length to the breadth of 12 fingers, or about 25 cm. It is mainly retroperitoneal, and its position is relatively fixed. The stomach and duodenum are closely related in function, pathogenesis, and disease manifestation. It takes in food from the esophagus (gullet or food pipe), mixes it, breaks it down, and then passes it on to the small intestine in small portions. It has three functions; to temporarily store food, contract and relax to mix and break down food, and produce enzymes and other specialized cells to digest food. In addition, it has a protective function because of the highly acidic medium due to the presence of HCl. Many of the micro-organisms die. Thereby it protects the GI tract from getting invaded by microorganisms. Structures Several layers of muscle and other tissues make up the stomach. 8 ● Mucosa is your stomach’s inner lining. When your stomach is empty, the mucosa has small ridges (rugae). When your stomach is full, the mucosa expands, and the ridges flatten. ● Submucosa contains connective tissue, blood vessels, lymph vessels (part of your lymphatic system) and nerve cells. It covers and protects the mucosa. ● Muscularis externa is the primary muscle of your stomach. It has three layers that contract and relax to break down food. ● Serosa is a layer of membrane that covers your stomach. 5 Distinct Sections The stomach may be divided into five major sections. The cardia is a 1–2 cm segment distal to the esophagogastric junction. The fundus refers to the superior portion of the stomach that lies above an imaginary horizontal plane that passes through the esophagogastric junction. The antrum is the smaller distal one-fourth to one-third of the stomach. The narrow 1–2 cm channel that connects the stomach and duodenum is the pylorus. The lesser curve refers to the medial shorter border of the stomach, whereas the opposite surface is the greater curve. The angularis is along the lesser curve of the stomach where the body and antrum meet, and is accentuated during peristalsis. The duodenum extends from the pylorus to the ligament of Treitz in a circle-like curve and is divided into four portions. The superior portion is approximately 5 cm in length, beginning at the pylorus, and passes beneath the liver to the neck of the gallbladder. The first part of the superior portion (2–3 cm) is the duodenal bulb. The descending or second part of the duodenum takes a sharp curve and goes down along the right margin of the head of the pancreas. The common bile duct and the pancreatic 9 duct enter the medial aspect of this portion of the duodenum at the major papilla either separately or together. The duodenum turns medially, becoming the horizontal portion, and passes across the spinal column, inclining upward for 5–8 cm. The ascending portion begins at the left of the spinal column, ascending left of the aorta for 2–3 cm, and ends at the ligament of Treitz, where the intestine angles forward and downward to become the jejunum. III. SIGNS AND SYMPTOMS SIGNS & SYMPTOMS RATIONALE Burning stomach pain The acid eats away the inner surface of the stomach or small intestine in the digestive system. It causes a painful open sore that can sometimes be alleviated by taking acid-reducing medicine or eating particular foods that buffer stomach acid, but it may return. (Mayo Clinic, 2022) Pain radiating at the back Pain radiating to the back may suggest that an ulcer has penetrated posteriorly, or the pain may be pancreatic in origin. (Malik et al., 2022) Feeling of fullness/bloating The infection is brought on by H infection. pylori, a common yet potentially harmful bacterium. Bloating from too much gas production might result from having too many bacteria in the small intestine. (Bakshis, 2021) Heartburn It occurs when stomach acid flows up into your esophagus. This leads to a burning discomfort below your breastbone or in your upper belly. (Digestive Health Associates Endoscopy, 2020) Nausea & Vomiting Peptic Ulcer can block the passage of food through the digestive tract, causing you to feel nauseous and 10 vomit. (Mayo Clinic, 2022) Appetite Change/Weight Loss Blockage in the digestive system caused by inflammation can prevent food from moving through the stomach, leading to weight loss and a decrease in appetite. (Prima Medicine, 2021) Dark Stool Dark stools and tarry may also result from unusual blood vessels or veins break in the esophagus, stomach, or duodenum. (Phillips & Dugdale, 2022) IV. ETIOLOGY Predisposing factors Age Rationale Age-related increases in Helicobacter pylori prevalence can have a significant impact on ulcer formation. Aging skin is more prone to pressure sores for a number of reasons. The skin loses some elasticity (stretchiness) in the elderly, making it more susceptible to damage. Blood Type According to a study, people with blood type O are more susceptible than people with other blood types to develop peptic and duodenal ulcers. Due to an increased epithelial cell colonization density and elevated inflammatory reactions to H. pylori. Precipitating factors Rationale Helicobacter Pylori infection A gram-negative bacillus called pylorus is present in the gastric epithelial cells. 90% of duodenal ulcers and 70% to 90% of stomach ulcers are brought on by this bacterium. The pylori bacteria destroy the stomach and duodenum protective mucous lining, allowing acid 11 to enter the delicate lining underneath. The bacteria and the acid irritate the lining, leading to an ulcer or sore. NSAIDs The stomach prostaglandin mucosa is secretion. often protected by prevent the NSAIDs production of prostaglandins by inhibiting the COX-1 enzyme, which lowers the production of gastrointestinal mucus, bicarbonate, and mucosal blood flow. Smoking This increases the chance of Helicobacter pylori infection. Nicotine reduces the production of prostaglandins in a smoker's stomach mucosa, making the mucosa more sensitive to ulceration. Alcohol Excess take of alcohol can weaken and irritate the stomach lining, which can lead to inflammation. Also, this inflammation can exacerbate ulcers already present and inhibit the healing process. Zollinger-Ellison Syndrome Peptic ulcer disease can develop in people also with the rare disorder Zollinger-Ellison syndrome (gastrinoma). This disease forms a tumor of cells that produce acid in the digestive tract. These tumors may or may not be malignant. The acid that is produced excessively harms stomach tissue. 12 V. PATHOPHYSIOLOGY 13 14 Narrative Peptic ulcer is where the lining of the stomach, intestine, or esophagus develops sores. Predisposing factors such as age, blood type O, and precipitating factors like Helicobacter Pylori Infection, NSAIDs, Smoking, Alcohol, and Zollinger- Ellison Syndrome contribute to the development of peptic ulcer disease. The ingestion of infected utensils, food, and water in our mouth can eventually increase the spread of Helicobacter Pylori Infection in our body, it can bind to the mucosa, especially the foveolar cells, due to its adhesive capability. This would then stimulate the release of an enzyme called protease, which will then break down stomach tissues and also causes the release of more gastrin and a reduction in the generation of somatostatin. Together, they may induce burning stomach pain and bloating, in addition to gradually damaging the mucosal cells. Continuous intake or use of Alcohol, cigarette, and NSAIDs are the other factors that cause mucosal disruption. Nonsteroidal anti-inflammatory medications (NSAIDs) used over an extended period of time can harm the stomach mucosa. NSAIDs function by preventing the formation of inflammatory prostaglandins by the enzyme cyclooxygenase. The prostaglandin increases the production of mucus and the synthesis of bicarbonate, protecting the mucosa from gastric acid. A poor barrier to protect the mucosa layer from hydrochloric acid contact results from low mucus and bicarbonate synthesis. HCL irritates the mucosal layer because it is known for digesting or breaking down protein. Also, vagal stimulation stimulates the release of acid and pepsinogen, which increases gastric production and stimulates the production of gastric acid. This results in signs and symptoms like abdominal pain and heartburn. Those three factors irritate the mucosal layer and will lead to further damage and weakening of the mucosal barrier. Excessive production of stomach acid can irritate the mucosal layer and eventually lead to ulcerations as hyperacidity progresses. Ulcerations then progress to Peptic Ulcer Disease. When the breakdown of the mucosal barrier will then lead to painful sores appearing on the lower esophageal lining, which results in Esophageal Ulcers. Another type of peptic ulcer happens when there is a decline in the function of the stomach mucus and results in the formation of open sores in the stomach lining which will then lead to a Gastric Ulcer. Lastly, when the duodenum's surface mucosa is disrupted, duodenal lesions develop in the surface part of the duodenum lining, which results in what is known as a duodenal ulcer. Peptic ulcer disease is made up of duodenal, esophageal, and stomach ulcers. As these ulcers worsen, they gradually cause bleeding and hemorrhage, which lowers hemoglobin levels and the body's ability to carry oxygen. These combine to create generalized, distinctive signs and symptoms. The person will experience 15 pain when they have ulcers, which are characterized by epigastric or abdominal pain. Melena and hematemesis arise as a result of bleeding when the ulceration spreads to the layer of the stomach called the muscularis, which contains blood vessels and muscle tissues. Moreover, progressive bleeding leads to loss of appetite, a feeling of fullness, and unexplained weight loss. Scarring arises from tissues recovering from ulcerations; whether this scarring thickens, particularly on the pyloric sphincter, it may result in a blockage. If treated with certain medical management and complying with medication the tissue in the lining of the stomach, esophagus, or duodenum that causes peptic ulcers will restore and contributes to a good prognosis. However, if it is not treated immediately this will eventually progress to hemorrhage and further ulcerations which will then causes inflammation which decreases the tissue perfusion and leads to hypovolemic shock which will cause death to the patient and contributes to a bad prognosis. VI. MEDICAL MANAGEMENT A. DIAGNOSTIC EXAMS TEST RATIONALE NURSING RESPONSIBILITIES Esophagogastroduoden Upper GI Endoscopy is the golden Before the procedure: ● oscopy standard and remains the most (Upper Gastrointestinal accurate diagnostic test for PUD. A fast and restrict fluids Endoscopy) test to observe the lining of the for 6 to 8 hr prior to the esophagus, and procedure to reduce permits the risk of aspiration biopsies and cytology brushings in related to nausea and the presence of a gastric ulcer to vomiting. duodenum. stomach, This also distinguish a benign ulcer from a ● Instruct the patient to Instruct that the patient malignant one. Through this exam, may be required to be gastric ulcers can be seen as NPO after midnight. discrete mucosal holes with a ● The patient may be punched-out regular ulcer base, instructed to take a often covered with whitish fibrinoid laxative, an enema, or exudate. (Cleveland Clinic, 2021) a rectal laxative suppository. 16 ● Instruct to avoid taking natural products and medications with known anticoagulant, antiplatelet, or thrombolytic properties or to reduce dosage, as ordered, prior to the procedure. After the procedure: ● Observe the patient's vital signs for any unusualities. ● If sedated, advise to drink plenty of water to help eliminate sedative the more efficiently. ● Instruct to ingest soft foods and liquids such as broth can enable recovery with minimal soreness and easier swallowing. Barium Contrast Radiography Barium X-rays are used to diagnose Before the procedure: abnormalities of the GI tract, such as tumors, ulcers and ● Instruct the patient to other eat a low-residue diet inflammatory conditions, polyps, for several days before hernias, and strictures. Barium is a the dry, white, chalky powder that is consume only clear mixed with water to make barium liquids during the 24 hr procedure and 17 liquid. It is an X-ray absorber and appears white on X-ray film. When before the procedure. ● Advise to take instilled into the GI tract, barium laxative coats the before the exam to large excrete excess waste the inside esophagus, wall of stomach, intestine, and/or small intestine so the a night before the procedure. that the inside wall lining, size, shape, contour, and patency are After the procedure: visible on X-ray. (John Hopkins ● Medicine, 2023) Advise to drink water to cleanse the body after undergoing the procedure. ● Monitor for any casualties such as a sudden drop in blood pressure and fast respiratory rate. Testing for Helicobacter pylori: Stool antigen test Helicobacter pylori are a common cause of Peptic Ulcers. In this test, Before the procedure: a stool sample is collected from the ● patient to determine if H. pylori antigens are present in the GI Assess patient’s level of comfort to defecate. ● Encourage to drink system. The sample is sent to the plenty of liquids to laboratory and added with a specific facilitate chemical and color developer. A excretion. presence of a blue color indicates ● the presence of H. pylori antigens. easier Instruct to avoid eating red meat and having a diet high in residue. The breath test is a simple and safe test that detects active H. pylori infection Urea breath test enzymatic by testing activity of for the bacterial ● Instruct to maintain NPO at least 3 hours 18 urease. The test is done by drinking a special liquid substance called before the test. ● Advise that they may urea. The patient will be breathing brush their teeth and or exhaling into a bag and will be rinse, sent to the laboratory for testing. swallow water. but do not The rapid urease test (RUT), also known as the CLO test (Campylobacter-like organism test), is a popular diagnostic test that Rapid urease test ● Advise to not have a detects the presence of urease in or second on the gastric mucosa. Through breath test within 2 endoscopic days of your first test. mucosal biopsy, 14C urea presence of H. pylori may be obtained; the test involves After the procedures: incubating a gastric biopsy sample ● Encourage patient to in a urea broth that contains pH maintain indicator phenol red hygiene such as hand (Cleveland Clinic, 2021) washing. ● proper Drink plenty of water every after the procedure to replenish the body’s loss. Serology Serologic tests are blood tests that After the procedure: look for antibodies in the blood. The ● Advice to increase test has a high specificity and fluid intake sensitivity. The test relating to rehydrate the body. to peptic ulcer disease is useful in detecting a newly infected patient but not a reliable test for a follow-up test of treated patients because 19 results may not indicate recent infection of the bacteria. (Mayo Clinic, 2023) B. MEDS 1. Proton pump inhibitors (PPIs) - PPIs directly suppress gastric acid production by blocking the proton pumps of the gastric parietal cell that is responsible for acid secretion, and thereby promoting the ulcer healing. Their effect on suppressing gastric acid production is stronger than that of Histamine-2 receptor antagonists. GENERIC NAME Esomeprazole BRAND NAME Nexium, Prosome, Esoget, Esotaz-40 DRUG CLASSIFICATION Proton pump inhibitors, Anti-ulcers SUGGESTED DOSE Peptic Ulcer Disease (Helicobacter pylori) PO: Adult 40 mg b.i.d. for 2 wk in combination therapy for 10-14 d Duodenal Ulcer PO: Adult 15 mg/d for 4 wk ROUTE OF PO ADMINISTRATION MODE OF ACTION Esomeprazole works by binding irreversibly to the H+/K+ ATPase in the proton pump. Because the proton pump is the 20 final pathway for secretion of hydrochloric acid by the parietal cells in the stomach, its inhibition dramatically decreases the secretion of hydrochloric acid into the stomach and alters gastric pH. INDICATION Esomeprazole is indicated for the treatment of acid reflux disorders including healing and maintenance of erosive esophagitis, and symptomatic gastroesophageal reflux disease (GERD), peptic ulcer disease, and duodenal ulcer CONTRAINDICATION - Hypersensitive to esomeprazole magnesium or other protonpump inhibitors - Gastric Malignancy - Pregnant (Category B) - Lactating Mothers SIDE EFFECTS - Dry mouth and thirst, Nausea, Hiccups, Diarrhea, Constipation, Rash, Headache, Dizziness, Blurred vision, Fatigue ADVERSE EFFECTS - CNS: Headache, dizziness, vertigo, insomnia - GI: Nausea, vomiting, diarrhea, constipation, abdominal pain, flatulence, dry mouth. - Respiratory: Upper Respiratory Tract Infections, Cough - Others: Elevated AST, ALT DRUG INTERACTIONS Drug-Drug - May decrease theophylline levels; sucralfate decreases lansoprazole bioavailability; may interfere with absorption of ampicillin, ketoconazole, digoxin. Drug-Food - Food decreases peak levels (decreased absorption by up to 35%) NURSING RESPONSIBILITIES 1. Assess for the mentioned contraindications to this drug R: To prevent potential adverse effects. 21 2. Before initiating comprehensive pharmacological physical therapy, a should be examination performed. R: To determine effectiveness of therapy, and evaluate potential adverse effects. 3. Assess for the patients’ neurological status R: To determine potential CNS effects. 4. Assess for the cardiac status attentively R: To determine whether change in drug dose is essential 5. Monitor laboratory test results including complete blood count, renal and liver function tests R: Some medications such as digoxin can interfere the liver metabolism of esomeprazole. 6. Inspect and palpate the abdomen to determine potential underlying medical conditions; assess for changes in bowel elimination and GI upset R: To decrease the risk of developing GI adverse effects 7. Administer the drug before meals. Ensure that the patient swallows whole as indicated. R: To ensure the therapeutic effectiveness of the drug. 8. Provide comfort and safety measures R: To aid in patient’s well-being 9. Have emergency medications and equipment at the bedside R: To promote prompt treatment in cases of severe toxicity. 10. Monitor the patient for diarrhea or constipation R: To administer proper bowel interventions as needed 2. Antacids - Antacids are drugs that relieve heartburn and indigestion by reducing the amount of acid in your stomach. Antacids neutralize the acid in your stomach by stopping an enzyme that creates acid to break down food for digestion (pepsin). This drug can also help lessen the 22 symptoms of stomach lining infection or gastritis and help lessen the appearance of stomach ulcers. GENERIC NAME Aluminum Hydroxide BRAND NAME AlternaGEL, Amphojel, and Nephrox DRUG CLASSIFICATION Antacids SUGGESTED DOSE Oral suspension: 5-30 mL between meals and at bedtime or as directed Peptic Ulcer Disease 5-30 mL between meals and at bedtime or as directed Hyperphosphatemia Adult: 300-600 mg orally 3 times/day between meals and at bedtime ROUTE OF PO ADMINISTRATION MODE OF ACTION Acts by neutralizing hydrochloric acid in gastric secretions. Aluminum hydroxide is slowly solubilized in the stomach and reacts with hydrochloric acid to form aluminum chloride and water. It also inhibits the action of pepsin by increasing the pH and via adsorption. INDICATION - Relieves heartburn, acid indigestion, and upset stomach. They may be used to treat these symptoms in patients with peptic ulcer, gastritis, esophagitis, hiatal hernia, or too much acid in the stomach (gastric hyperacidity). 23 CONTRAINDICATION - Hypophosphatemia, Diarrhea, Neonates, renal disease, renal failure, renal impairment, Ascites, heart failure, hepatic disease, Geriatric, Pregnancy SIDE EFFECTS - Nausea, Vomiting, Rebound hyperacidity, Aluminum- intoxication, Hypophosphatemia, Chalky taste, Constipation (this could lead to hemorrhoids or bowel obstruction), Stomach cramps ADVERSE EFFECTS - Black/tarry stools, Mental/mood changes (e.g., confusion, deep sleep), Pain with urination, Stomach/abdominal pain, Vomit that looks like coffee grounds DRUG INTERACTIONS Drug-drug - Acetaminophen: Antacids can delay the oral absorption of acetaminophen - Allopurinol: Aluminum hydroxide decreases the oral bioavailability of allopurinol - Captopril: Antacids can decrease the GI absorption of captopril if administered simultaneously NURSING RESPONSIBILITIES 1. Assess vital signs before and after drug administration R: This is to watch out for any adverse effects that may occur 2. Educate to shake the suspension well before use R: To ensure proper dosage is administered 3. Advise to take medication after meals and at bedtime R: Intake on an empty stomach may cause stomach cramps 4. Encourage to intake drug with water R: To avoid the the chalky taste of the drug 5. Advise to not Aluminium Hydroxide drug along with other drugs R: This to ensure adequate absorption of other medications 6. Monitor periodic serum calcium and phosphorus levels R: Prolonged use may cause impaired renal function 7. Advise to increase phosphorus in diet if prolonged use 24 of drug occurs R: Hypophosphatemia can develop within 2 weeks of continuous use of these antacids. 8. Monitor number and consistency of stools. R: Constipation is common and dose related. Intestinal obstruction from fecal concretions may occur 9. Administer an appropriate bowel program R: Constipation and speckled or whitish stools may appear 10. Provide comfort measures and safety R: To ensure patient’s well-being 3. Histamine-2 receptor antagonists - Histamine-2 receptor antagonists, also known as H2-blockers, suppress the secretion of gastric acid by blocking the actions of histamine, a protein produced by the body that stimulates gastric acid secretion. They are also used to treat gastric ulcers and for some conditions, such as Zollinger-Ellison disease, in which the stomach produces too much acid. GENERIC NAME Ranitidine BRAND NAME Zantac DRUG CLASSIFICATION Antiulcer, Histamine H2 antagonists SUGGESTED DOSE Gastric Ulcer - Treatment: 150 mg orally every 6 hours or 50 mg intramuscular/intravenously every 6-8 hours intermittent bolus or infusion; 25 alternatively, 6.25 mg/hours intravenously by continuous infusion - Maintenance of healing: 150 mg orally every 12 hours ROUTE OF PO ADMINISTRATION MODE OF ACTION Inhibits the action of histamine at the H2 receptor site located primarily in gastric parietal cells resulting in inhibition of gastric acid secretion. In addition, healing and prevention of ulcers. INDICATION - Short term treatment of active duodenal ulcers and benign gastric ulcers. - Management of GERD - Treatment and prevention of heartburn, acid indigestion, and sour stomach - Management of gastric hypersecretory states CONTRAINDICATION - Hypersensitivity to ranitidine or other components of the drug. - Some products contain aspartame and should be avoided in patients with phenylketonuria. SIDE EFFECTS - Nausea, headache, abdominal pain, diarrhea, dizziness, hair loss, confusion, constipation, vomiting, anemia ADVERSE EFFECTS - CNS: drowsiness and hallucinations - CV: arrhythmias - GU: decreased sperm count, impotence - ENDO: gynecomastia - HEMATO: agranulocytosis, aplastic anemia, neutropenia, thrombocytopenia - LOCAL: Pain at IM site - Hypersensitivity reactions, vasculitis DRUG INTERACTIONS Drug-Drug 26 - Atazanavir and Delavirdine Drug absorption may be impaired - Gefitinib: Gefitinib exposure is reduced when used with ranitidine - Midazolam: Oral midazolam increases when used with ranitidine and may cause excessive and prolonged sedation. - Procainamide: Higher doses of ranitidine (> 300 milligrams/day) may increase plasma levels of this drug and in rare cases may cause toxicity. - Triazolam: Oral triazolam increases when used with ranitidine and may cause excessive or prolonged sedation. - Warfarin: Ranitidine may affect warfarin’s effectiveness. NURSING RESPONSIBILITIES 1. Assess heart rate, ECG, and heart sounds R: Any rhythm disturbances or symptoms of increased arrhythmias, should be reported right away 2. Monitor signs of hypersensitivity reactions, including pulmonary symptoms or skin reactions R: Notify the doctor immediately 3. Assess for side effects such as fatigue, weakness, muscle pain, numbness, fever, loss of appetite, and weight loss R: These could be adverse effects of the drug 4. Assess dizziness and drowsiness that might affect gait, balance, and other functional activities R: Report balance problems and functional limitations to the physician and nursing staff 5. Monitor other CNS symptoms such as confusion, hallucinations, and headache R: Excessive or prolonged CNS symptoms 27 may require a reduction in dose 6. Encourage adequate fluid intake R: Increased fluid intake helps improve bowel function 7. Advise increase in fiber intake R: Fiber intake helps with constipation 8. Advise patients to avoid alcohol. R: Alcohol in ranitidine may be contraindicated to some patients and may increase GI irritation. 9. Advise patient to avoid smoking or any exposure to tobacco chemicals R: Smoking interferes with the action of histamine antagonists 10. Educate family member to report any side effects immediately R: Immediate interventions helps reduce the risk for further complications 4. Cytoprotective agents - Cytoprotective agents stimulate mucus production and enhance blood flow throughout the lining of the gastrointestinal tract. These agents also work by forming a coating that protects the ulcerated tissue. Cytoprotective agents help protect the tissues that line your stomach and small intestine. GENERIC NAME Misoprostol BRAND NAME Cytotec DRUG CLASSIFICATION Prostaglandin, Antisecretory, gastric protectant 28 SUGGESTED DOSE For prophylaxis of NSAID-induced ulcers Adults: 200 mcg PO 2 to 4 times a day with food; if not tolerated, decrease to 100mcg PO q.i.d. For gastric and duodenal ulcers, NSAID associated ulceration Adults: 800mg daily in 2 to 4 divided doses for at least four weeks even if symptoms are relieved sooner. ROUTE OF PO ADMINISTRATION MODE OF ACTION Misoprostol is a synthetic prostaglandin E1 analog that inhibits basal and nocturnal gastric acid secretion through direct stimulation of prostaglandin E1 receptors on parietal cells in the stomach INDICATION - Ulcer - Prevents NSAID-induced gastric ulcer - For those at high risk for developing gastric ulcer/ gastric complications - Medical termination of intrauterine pregnancy - Cervical ripening - Labor induction - Treatment/prevention of postpartum hemorrhage - Treatment of incomplete or missed abortion CONTRAINDICATION - Hypersensitivity to prostaglandin - Pregnancy when used to reduce NSAID induced ulcers - Inflammatory bowel disease SIDE EFFECTS - Diarrhea, abdominal pain, vomiting, constipation, headache, nausea, flatulence, dyspepsia 29 ADVERSE EFFECTS - Tremor, seizures, dyspnea, palpitations, hypotension, bradycardia DRUG INTERACTIONS Drug-Drug - Antacids may increase concentration Drug-Food - Any food: May decrease the absorption rate of drug NURSING 1. Assess vital signs especially blood pressure for RESPONSIBILITIES hypotension R: When hypotension is severe, it may cause severe symptoms when taking the drug 2. Assess the female patient if pregnant or has plans to become pregnant. R: R: The drug induces uterine contractions, It may cause miscarriage, premature birth, or congenital disabilities if it is taken during pregnancy 3. Administer drug with or after meals. R: Intake with food will help prevent loose stools, diarrhea, and abdominal cramping, which is a common side effect of misoprostol 4. Advise to advise administering with magnesiumcontaining antacids R: This is to minimize the potential for diarrhea 5. Inform patient of taking the drug at the same time with NSAID R: To prevent NSAID-induced gastric ulcers, the drug must be continued as long as NSAIDs are taken 6. Inform the client about the common side effects of the medicine R: This is for the patient to anticipate the untoward symptoms and provide assurance 7. Monitor improvement of Gastrointestinal symptoms R: This is to know and help document if the drug effectively 30 prevents gastric damage or duodenal ulcers 8. Educate about using caution to the patient with kidney disease R: Since the effects may increase because of the slower removal of the medicine from the body 9. Instruct patient to avoid intake of alcohol. R: Some drinks and food may increase gastric irritation, worsening symptoms 10. Educate the patient about not taking for a longer time intended by the physician R: This is to achieve a safe and maximum effect of the medicine. Also, long term use of the drug may increase unwanted effects C. TREATMENT THERAPY Medications RATIONALE NURSING RESPONSIBILITIES Treatment will depend on the Before the procedure: underlying cause of your ulcer. ● Instruct patient to take the Several different medication proper dosage, and process therapies are available to help of reduce gastric acid and coat prescribed by their doctor or the ulcers. If tests show that physician. you have an H. pylori infection, ● the medications Educate to not take drugs all your doctor will prescribe a at once or together with combination other drugs as this may The of medication. medications include lessen the effect of the antibiotics to help kill infections prescribed drug or it may and cause proton pump inhibitors(PPIs) to help reduce stomach acid. Another severe adverse effects. is 31 Bismuth, this medication After the procedure: covers the ulcer and protects it ● Advice on proper bed rest from stomach acid. It can also after intake of help kill H. pylori infections medications (Rogers, 2020) proper absorption of the to the facilitate drug. Antisecretory therapy with a proton pump inhibitor (PPI) Proton pump inhibitors (PPIs) Before the procedure: effectively block gastric acid secretion by ● Instruct to take medication irreversibly before meals to ensure that binding to and inhibiting the the patient does not open, hydrogen-potassium ATPase chew, or crush capsules; pump that resides on the they should be swallowed luminal surface of the parietal whole cell membrane. PPIs are first- therapeutic effectiveness of line antisecretory therapy in the drug. to ensure the the treatment of peptic ulcer disease. (UpToDate, 2023) After the procedure: ● Monitor Vital signs especially cardiac rate for tachycardia and other unusualities. VII. SURGICAL MANAGEMENT PROCEDURE Vagotomy RATIONALE This surgical NURSING RESPONSIBILITIES procedure Before the procedure: requires removing a part or all of ● Educate client on the the vagus nerve. This is used to procedure itself to lessen aid in treating stomach ulcers anxiety and uncertainty. due to H. pylori infection and 32 erosion from stomach acid. The ● Instruct that abdominal hair procedure is usually done in is removed with clippers in conjunction the preoperative area. with procedures other such as pyloroplasty, where the pylorus After the procedure: is widened to help control the ● Keep the wound clean and movement of partially digested dry. The dressing should food and juiced into the small be removed and wounds intestine. covered (Cleveland Clinic, 2023) with adhesive bandages on the first or second day after surgery. Do not remove the paper strips or cut any of the visible sutures. ● Administer pain medications as ordered by the physician. ● Monitor patients vital signs for any unusualities Gastrectomy Gastrectomy may come in two Before the procedure: kinds: total and partial ● Advise to not eat or drink gastrectomy. Both gastrectomy anything after midnight the procedures are indicated for night before your surgery. patients with peptic ulcer ● Advise to not ingest any disease that have failed to drugs that make it difficult respond or for your blood to clot (ex. with gastric aspirin, ibuprofen, vitamin A partial E, warfarin. to individuals malignancies. therapy gastrectomy is mainly done since a small region of the After the procedure: stomach will be resected to remove the gastric ulcer. On the ● Administer killers until regular the pain patient 33 other hand, total gastrectomy is recovers the procedure where the entire discharged. stomach is removed, and the ● and will be Advise patients that they esophagus is directly connected are allowed to drink water 6 to the small intestine to continue hours after surgery. digestion. (Penn Medicine, ● 2023) Provide a relaxing and noise-free environment to aid in uninterrupted rest. Graham’s Omental Patch Graham patch is a technique Before the procedure: where a patch of omentum, a ● Educate the client on the fatty tissue that normally covers process of the surgery to the stomach and intestines, is lessen used to cover the perforation. uncertainty. The technique can be done with an open laparotomy ● their fear and Advice to maintain an NPO or after midnight before the laparoscopically. Three or four surgery to avoid any gastric interrupted sutures are inserted complications during the through and through the axis. procedure. Both approaches are within the standard of care, yet it still After the procedure: depends on the experience of ● Assess the operation site the surgeon and the condition of for any unusualities such the patient. (Cleveland Clinic, as swelling and pus. 2023) ● Instruct patient to take a few sips of water from time to time to replenish fluids lost during the surgery. ● Monitor for any adverse effects and and unusualities administer pain medication as prescribed VIII. NURSING MANAGEMENT 34 NURSING DIAGNOSIS GOAL INTERVENTION Acute pain related to the effect Within 1 hour of nursing 1. Administer prescribed of gastric acid secretion on intervention the patient will medications damaged tissue as evidenced demonstrate relief of pain as alleviate the symptoms by pain score of 8 out of 10, evidenced by: of heartburn/ stomach verbalization of chest pain or heartburn guarding after sign eating, on the abdomen. a. verbalization comfort decrease of and that pain. a Rationale: Antibiotics such as in the amoxicillin can kill H pylori. intensity level of pain Antacids are helpful in less than 2 to 4 on a neutralizing stomach acid. H2Rationale: occur Peptic when acid ulcers in inner surface receptor blockers reduce the the digestive tract eats away at the scale of 0 to 10. of the stomach or small intestine. production of stomach acid. b. Exhibit stable vital Proton- pump inhibitors work signs, and absence of by reducing the amount of guarding behavior. stomach acid. The acid can create a painful open sore that may bleed. 2. Assess the patient's Your digestive tract is coated vital signs and with a mucous layer that characteristics of pain normally protects against acid. at least 30 minutes after administration of Reference: (2020). Mayo Peptic Clinic Ulcer. medication. Rationale: To monitor of medical Retrieved on February 13, effectiveness 2022 treatment for the relief of from https://www.mayoclinic.org/di heartburn and stomach pain. seases- The time of monitoring of vital conditions/peptic- ulcer/symptoms- causes/syc- signs may depend on the peak time of the drug administered. 3. Teach the patient on 35 how to perform nonpharmacological pain relief methods such as deep breathing, massage, acupressure, biofeedback, distraction, music therapy. and guided imagery. Rationale: To reduce stress levels, thereby relieving the symptoms of peptic ulcer disease, especially stomach pain and heartburn. 4. Encourage the patient to assume a position of comfort Rationale: Reduces abdominal tension and promotes a sense of control 5. Encourage the patient to follow appropriate mealtimes and meal portions. Rationale: To ensure that the patient does not eat a huge meal, or that he/she does not eat late at night/ before bedtime as both of these may trigger nausea/vomiting. 36 6. Instruct the patient to avoid aspirin, ibuprofen, naproxen or any NSAIDS medication. Rationale: These medications irritation of may cause the gastric mucosa. 7. Encourage the patient to Increase oral fluid Intake unless contraindicated. Rationale: Fluid intake helps dilute the acid in the stomach which may aggravate the pain. 8. Inform the patient to avold spicy, fried, caffeinated, or acidic foods. Rationale: Gastric acid secretion may be stimulated by these types of food and may worsen the ulcerations in the stomach lining 9. Advice the patient to include probiotic in regular diet like yogurt, banana, watermelon,beans 37 carrots, cucumber, and green Rationale: to help restore the natural bacteria in the GI tract. 10. Inform the patient to limit or avoid the aggravating factors of the pain such stress, as alcohol, smoking, etc. Rationale: increase The the factors risk for complications and may hinder the effectiveness of the drug therapy. Imbalanced than Nutrition: Body Less Within 8 hours of nursing 1. Create a daily weight Requirements intervention the patient will chart and a food and related to insufficient dietary demonstrate maintenance of fluid intake by nutritional requirements, and with the patient the pain, absence of complications as short term and long- burning as evidenced stomach chart. Discuss bloating, weight loss of 10 evidenced by: term pounds, nausea and vomiting, weight goals related to loss of appetite, heartburn. a. verbalization of nutrition and peptic ulcer disease. selection of foods or Rationale: To effectively Rationale: Many people with meals that will achieve monitor the patient's daily peptic a cessation of weight nutritional intake and progress ulcers particularly complain of pain on an empty loss. in weight goals. stomach. You may experience relief immediately after eating b. demonstrating healthy only to have pain return or eating worsen within an hour. This choices. patterns and 2. Help the patient to select dietary appropriate choices to 38 brief reprieve does not cause avoid spicy foods and people with ulcers to overeat, limit alcohol and coffee however, as frequent nausea intake. and discomfort can quash Rationale: To promote ulcer appetite or the desire to eat. healing Some people feel that certain habits. Caffeine is a stimulant foods (like high-fat choices) of gastric acid production. make peptic ulcer symptoms Decaffeinated coffee or tea worse, can still stimulate gastric acid while other foods soothe an ulcer. You can and healthy food secretion. become deficient in vitamins and minerals due to low food intake. Immune deficiencies, 3. Refer the patient to the dietitian. bone weakness, and skin Rationale: To provide a more fragility can all result from specialized care for the patient malnutrition, but may not be in terms of nutrition and diet in noticeable at first. relation to newly diagnosed peptic ulcer disease. Reference: Gillson, S. (2022, June 7). Stomach (Peptic) Ulcers: Symptoms Complications. and Verywell Health. 4. Administer the prescribed medications for peptic ulcer disease. https://www.verywellhealth.co Rationale: To reduce m/symptoms-of-peptic-ulcers- stomach acid production or 1741794 neutralize the stomach acid, relieving the burning stomach pain and helping the patient to have a better appetite. 5. Monitor values laboratory for serum albumin. 39 Rationale: This test indicates the degree of protein depletion (2.5 g/dL indicates severe depletion; 3.8 to 4.5 g/dL is normal). 6. Instruct in the importance of abstaining from excessive alcohol. Rationale: Alcohol causes gastric irritation and increases gastric pain 7. Encourage the client to limit the intake of caffeinated beverages such as tea and coffee. Rationale: Caffeine stimulates the secretion of gastric acid. Coffee, even if decaffeinated, contains a peptide that stimulates the release of gastrin and increases acid production. 8. Provide good oral hygiene and dentition. Rationale: Oral hygiene has a positive effect on appetite and on the taste of food. Dentures need to be clean, fit 40 comfortably, and be in the patient's mouth to encourage eating. 9. Provide a pleasant environment. Rationale: A atmosphere pleasing helps in decreasing stress and is more favorable to eating. 10. Teach about the importance of eating a balanced meals diet at with regular intervals. Rationale: Specific dietary restrictions are no longer part of the treatment for PUD. During the symptomatic phase of an ulcer the client may find benefit from meals at eating more small frequent intervals. Anxiety related to the nature of Within 8 hours of nursing the disease secondary peptic ulcer disease 1. Evaluate the client's to intervention the patient will will psychological and as demonstrate ways of reducing physiological status evidenced by verbal reports of anxiety level as evidenced by: fear and worry. and level of anxiety. Rationale: People suffering a. verbalize which from Peptic ulcer disease Rationale: Clients with peptic stressors most likely experience ulcers are anxious, but their affect them, anxiousness, and though the level of their 41 anxiety level is not visible. explore Mental health problems such habits can help them manifested. Encourage the as stress, depression, and to suicidal ideation were closely stressors. correlated with PUD. These what overcome daily anxiety is those client to not open usually up their thoughts and ensure to them b. exhibit coping patterns that we welcome them if they psychological problems were effectively with the do have any questions. Be found to be associated with modality of available patient in explaining to them PUD. Individuals under severe treatment, stress or with a depressed pharmacologic mood might be more likely to non-pharmacologic develop PUD. methods the important details because and they tend to be sensitive because of fear. 2. Recognize the Reference: Lee, Y. H., Yu, J., understanding of the Moon, J. H., Jeon, B., Kim, H., client's anxiety. Kim, S., Kim, S. W., Park, Y. Rationale: Recognize B., & Chae, H. S. (2020). The client's feelings, be attentive in association between peptic listening to what they share. It ulcer diseases and mental develops the feeling of trust health problems. Medicine, and acceptance between the 96(34), e7828. client and healthcare provider. https://doi.org/10.1097/md.00 This may help the client to 00000000007828 acknowledge anxiety and fear. 3. Give support the by allowing the client to verbalize their fears and concerns freely. Rationale: Sustain a trustful relationship with the client as they express themselves gives assurance that they can speak up openly It gives comfort and relieves 42 uneasiness that helps in reducing anxiety and stress levels. 4. Communicate simple using language, easily understood statements when giving direction to the client. Rationale: experiencing Clients moderate to severe anxiety may not be able to understand statements that are complex, vague, and even lengthy instructions. The right choice of words is also necessary so we can catch their interest and also avoid their thoughts being triggered. 5. Maintain a calm and quiet environment to minimize stressors and stimuli. Rationale: External stimuli may escalate anxiety to panic attacks such as a noisy environment. Avoid noise, too loud conversation, and equipment around the client. In dealing with clients, establishing a non-threatening 43 environment develops security and peace for them. It will help to put the client at ease. 6. Ensure emotional support to the client. Rationale: Extending emotional support to the client will provide relaxing a calm and feeling that may brighten up their mood and ease their stress and anxiety. Strong emotional support offers unconditional comfort measures. Promote wellness, keep them: reminded with the positive coping strategies, and refrain from triggers. 7. Help the patient in developing techniques that reduce anxiety and stress levels management strategies. These measures include biofeedback, positive imagery, and behavior modification. Rationale: Aside pharmacological from treatments, there are also nonchemical 44 ways that are effective in dealing with anxiety. Learning and with a regular habit of practicing these techniques provide confidence to the client in overcoming anxiety. 8. Explain reasons for planned treatment schedule, such as Pharmacotherapy, dietary restrictions, modification of activity levels, reduce or stop smoking. Rationale: Knowledge reduces anxiety appears to be a sense of ignorance. fear due Knowledge to can have a positive effect on behavior change. 9. Assess for the Influence of cultural beliefs, and the norms, values on a patient's perspective of a stressful situation. Rationale: What the patient considers stressful may be based on cultural perceptions. 45 IX. LITERATURE Medicinal Plants with Prospective Benefits in the Management of Peptic Ulcer Diseases in Ghana (Boakye-Yiadom et al., 2021) Boakye-Yiadom, M., Kumadoh, D., Adase, E., & Woode, E. (2021). Medicinal Plants with Prospective Benefits in the Management of Peptic Ulcer Diseases in Ghana. BioMed Research International, 2021, 1–14. https://doi.org/10.1155/2021/5574041 The growth or multiplication of harmful microorganisms in addition to harmful human activities has led to many disorders in humans. Consequently, there is a search for medications to treat these disorders. Interestingly, medicines of plant origin are known to be among the most attractive sources of new drugs and have shown promising results in the treatment of various diseases including peptic ulcers. This review, therefore, is aimed at obtaining knowledge on some Ghanaian ethnomedicinal plants used to treat peptic ulcers, their folkloric uses, their phytochemicals, and their antiulcer and related pharmacological activities as well as finding areas for prospective studies.Methods. Published peer-reviewed articles on ethnomedicinal plants used for the management of peptic ulcers in Ghana from 1967 to 2020 were sourced and used for the study. Results. In this review, 13 plants were identified which belong to 10 different families including Sapindaceae, Apocynaceae, and Bignoniaceae. The parts most often used for most preparations were the leaves (53%), followed by stem bark and roots (both having the same percentage of use of 17.6%), the whole plant (5.9%), and the rhizomes (5.9%). Azadirachta indica was the only plant that had undergone some patient studies in addition to animal studies. Conclusion. A discussion of various antiulcer activity studies using ulcer models carried out on selected medicinal plants used for the management of peptic ulcer disease in addition to brief information on their folkloric uses and their phytochemical and other pharmacological properties is presented. These medicinal plants may be used in developing herbal products for the management of peptic ulcer disease. Evidence-based clinical practice guidelines for peptic ulcer disease 2020 (Kamada et al., 2021) Kamada, T., Satoh, K., Itoh, T., Ito, M., Iwamoto, J., Okimoto, T., Kanno, T., Sugimoto, M., Chiba, T., Nomura, S., Mieda, M., Hiraishi, H., Yoshino, J., Takagi, A., Watanabe, S., & Koike, K. (2021). Evidence-based clinical practice guidelines for peptic ulcer disease 2020. Journal of Gastroenterology, 56(4), 303–322. https://doi.org/10.1007/s00535-02101769-0 46 The Japanese Society of Gastroenterology (JSGE) revised the third edition of evidencebased clinical practice guidelines for peptic ulcer disease in 2020 and created an English version. The revised guidelines consist of nine items: epidemiology, hemorrhagic gastric and duodenal ulcers, Helicobacter pylori (H. pylori) eradication therapy, non-eradication therapy, drug-induced ulcers, non-H. pylori, and nonsteroidal anti-inflammatory drug (NSAID) ulcers, remnant gastric ulcers, surgical treatment, and conservative therapy for perforation and stenosis. Therapeutic algorithms for the treatment of peptic ulcers differ based on ulcer complications. In patients with NSAID-induced ulcers, NSAIDs are discontinued and anti-ulcer therapy is administered. If NSAIDs cannot be discontinued, the ulcer is treated with proton pump inhibitors (PPIs). Vonoprazan (VPZ) with antibiotics is recommended as the first-line treatment for H. pylori eradication, and PPIs or VPZ with antibiotics is recommended as a second-line therapy. Patients who do not use NSAIDs and are H. pylori negative are considered to have idiopathic peptic ulcers. Algorithms for the prevention of NSAID- and low-dose aspirin (LDA)-related ulcers are presented in this guideline. These algorithms differ based on the concomitant use of LDA or NSAIDs and ulcer history or hemorrhagic ulcer history. In patients with a history of ulcers receiving NSAID therapy, PPIs with or without celecoxib are recommended and the administration of VPZ is suggested for the prevention of ulcer recurrence. In patients with a history of ulcers receiving LDA therapy, PPIs or VPZ are recommended and the administration of a histamine 2-receptor antagonist is suggested for the prevention of ulcer recurrence. Current Status and Future Perspective of Artificial Intelligence in the Management of Peptic Ulcer Bleeding: A Review of Recent Literature (Yen et al., 2021) Yen, H., Wu, P. Y., Chen, M., Lin, W., Tsai, C., & Lin, K. (2021). Current Status and Future Perspective of Artificial Intelligence in the Management of Peptic Ulcer Bleeding: A Review of Recent Literature. Journal of Clinical Medicine, 10(16), 3527. https://doi.org/10.3390/jcm10163527 [Original source: https://studycrumb.com/alphabetizer] With the decreasing incidence of peptic ulcer bleeding (PUB) over the past two decades, the clinician experience of managing patients with PUB has also declined, especially for young endoscopists. A patient with PUB management requires collaborative care involving the emergency department, gastroenterologist, radiologist, and surgeon, from initial assessment to hospital discharge. The application of artificial intelligence (AI) methods has remarkably improved 47 people’s lives. In particular, AI systems have shown great potential in many areas of gastroenterology to increase human performance. Colonoscopy polyp detection or diagnosis by an AI system was recently introduced for commercial use to improve endoscopist performance. Although PUB is a longstanding health problem, these newly introduced AI technologies may soon impact endoscopists’ clinical practice by improving the quality of care for these patients. To update the current status of AI application in PUB, we reviewed recent relevant literature and provided future perspectives that are required to integrate such AI tools into real-world practice. Patients with PUB, which is a longstanding health problem, may achieve improved care management through a new approach using AI techniques. However, with the declining PUB incidence and clinician experience, further research is needed to apply these techniques in daily treatment practice. 48 GASTROESOPHAGEAL REFLUX DISEASE I. DEFINITION The term “gastroesophageal” refers to stomach and esophagus. Reflux means to flow back or return. Gastroesophageal reflux is when what’s in your stomach flows back into your esophagus. In normal digestion, your lower esophageal sphincter (LES) opens to allow food into your stomach. Then it will close to stop food and acidic stomach juices from flowing back into your esophagus. Gastroesophageal reflux occurs when the LES is weak or relaxes when it shouldn’t. This lets the stomach's contents flow up into the esophagus (WebMD, 2022). It’s important to note that there’s a very real distinction between occasional heartburn (which may not need medical intervention), and GERD. Most people experience heartburn from time to time, and in general, occasional heartburn isn’t a cause for concern. But if you’ve been experiencing heartburn more than twice a week, and especially if you’ve also been experiencing a chronic cough and chest pain, you might be dealing with GERD (DiGiacinto, 2021). II. ANATOMY/ PHYSIOLOGY 49 The organs that take in food and liquids and break them down into substances that the body uses for energy, growth, and tissue repair. Waste products the body can’t use leaves the body through bowel movements. The digestive system consists of the mouth, pharynx (throat), esophagus, stomach, small intestine, large intestine, rectum, and anus. It also includes the salivary glands, liver, gallbladder, and pancreas, which create digestive juices and enzymes that help the body digest food and liquids. Also called gastrointestinal system. Mouth Mouth, also called buccal cavity or oral cavity, in human anatomy, orifice through which the food and air enter the body. The mouth opens to the outside at the lips and empties into the throat at the back; its borders are defined by the lips, cheeks, hard and soft palates, and glottis. It is divided into two sections: the vestibule, the part between the cheeks and the teeth, and the oral cavity proper. The latter section is mostly occupied by the tongue, a large muscle firmly anchored to the floor of the mouth by the frenulum linguae. In addition to its primary role in the intake and initial digestion of food, the mouth and its structures are important in humans to the formation of speech. If stomach acid goes into your esophagus, you may experience heartburn and belching. If it goes higher into your throat, you may experience hoarseness and sore throat. And if it gets into your mouth, you’ll notice a bitter taste in your mouth, and you may have a cough. If it happens a lot, it may wear down your tooth enamel or deteriorate the symptoms of asthma. 50 Esophagus The core functions of the esophagus are to transport food and fluids from the pharynx to the stomach, prevent the passive diffusion of substances from the food into the blood and to prevent the reflux of gastric contents into the esophagus. Food is transported starting from the pharynx to the stomach by a coordinated peristaltic contraction initiated in the upper esophagus, which temporally trails a descending wave of inhibition. The control of the LES is critical to esophageal function. Maintenance of sphincter tone is necessary to prevent the reflux of gastric contents, which are under positive pressure relative to the esophagus due to their position in the peritoneal cavity. Acid reflux happens because a valve at the end of your esophagus, the lower esophageal sphincter, doesn’t close properly when food arrives at your stomach. Acid backwash then flows back up through your esophagus into your throat and mouth, giving you a sour taste. Stomach The stomach is one of the important organs and the most dilated portion of the digestive system. The esophagus comes first, and the small intestine follows. It is a large, muscular, and hollow organ permitting for a capacity to hold food. It comprises 4 main regions, the cardia, fundus, body, and pylorus. The primary functions of the stomach include the temporary storing of food 51 and the partial chemical and mechanical digestion of food. The upper portions of the stomach (cardia, body, and fundus) relax as food enters to permit the stomach to hold increasing quantities of food. The lower portion of the stomach contracts in a rhythmic fashion (mechanical digestion) to aid with the breaking down of food and it mixes with stomach juices (chemical digestion) which also serve to break down food and prepare the mixture, termed chyme at this point of digestion, for further digestion. GERD happens when the digestive acids and enzymes in your stomach don’t want to stay in your stomach. Instead, they flow back up into your esophagus toward your mouth. This is due to a band of muscle around the base of your esophagus called the lower esophageal sphincter weakens and doesn’t seal properly. Large Intestine Your large intestine is around five feet or 1.5 meters long. The large intestine is much bigger than the small intestine and takes a much straighter path through your belly, or abdomen. The function of the large intestine is to absorb water and salts from the material that has not been digested as food, and get rid of any waste products left over. By the time the food mixed with digestive juices reaches your large intestine, most digestion and absorption has already taken place. Small Intestine The small intestine is made up of three parts, which form a passage from your stomach (the opening between your stomach and small intestine is called the pylorus) to your large intestine. It is the duodenum, jejunum, and ileum. By the time the food reaches your small intestine, it has already been broken up and mashed into a liquid form by your stomach. Each day, your small intestine obtains between one and three gallons or six to twelve liters of this liquid. The small intestine carries out most of the digestive process, absorbing almost all of the nutrients you get from the foods you’ve eaten into your bloodstream. The walls of the small intestine make digestive juices, or enzymes, that work together with enzymes from the liver and pancreas to do this. Rectum The rectum is a straight, 8-inch chamber that connects the colon to your anus. The rectum's job is to receive stool from the colon, let you know that there is stool to be evacuated (pooped out) and to hold the stool until evacuation happens. When anything such as gas or stool 52 comes into the rectum, sensors send a message to the brain. The brain then chooses and decides if the rectal contents can be released or not. III. SIGNS AND SYMPTOMS Signs and Symptoms Rationale Heartburn The feeling of acid reflux is heartburn: it is a mild burning sensation in the mid-chest, often happens after meals or when lying down. Gastroesophageal reflux disease (GERD) is a graver form of acid reflux. In GERD, the backflow of stomach acid happens chronically and causes damage to the body over time (Pfizer, 2023). Regurgitation Regurgitation is when food, liquid, or stomach acid comes up from the stomach into your mouth. This symptom is usually described as a sour taste in the mouth or a sense of fluid moving up and down in the chest. It occurs in 80% of people with GERD, which can be treated with over-the-counter and prescription medications (Buoy health, 2018). Coughing Many are surprised to know that the issue behind their chronic cough is not a cold, but rather due to gastroesophageal reflux or GERD. The U.S. Library of Medicine found that GERD was linked in 25% or more cases of chronic coughing. The GERD cough is a dry cough that gets worse at night and lasts longer than 8 weeks (Warf, 2021). Chest pain GERD causes chest pain that mimics a heart attack. Described as a squeezing pressure behind the breast bone, GERD-related chest pain lasts for hours. And like a heart attack, it can also radiate down from your 53 arm to your back (Larson, 2022). Swallowing problem Difficulty swallowing, also known as dysphagia, is the feeling of food “sticking” in your throat or chest and is one of the complications of acid reflux/GERD. When acid reflux occurs, acid flows back into your esophagus causing irritation and discomfort. With chronic acid reflux/GERD, this is happening frequently causing irritation to the esophagus, which can lead to other complications such as dysphagia (Endoscopy Center of Red Bank, 2023). Vomiting People who have acid reflux frequently experience a sour taste in their mouth from stomach acids. The taste, along with the frequent burping and coughing linked with reflux and GERD, can create nausea and even vomiting in some cases (Roth, 2019). Sore throat and hoarseness Gastroesophageal reflux is a condition in which some of the acid in the stomach travels backward out of the stomach and into the esophagus and throat. Reflux is usually worse when we are sleeping, but it can occur at any time. When we sleep the valve between the stomach and esophagus relaxes and opens. This lets acid in the stomach move backward into the esophagus and throat. This acid is irritating to the throat and can result in laryngitis, a condition of inflamed and irritated vocal cords or larynx (UMMC Health Care, 2020). IV. ETIOLOGY Predisposing factors Rationale 54 Age GERD can affect people of all ages, statistics show that the risk increases as the age Increases and tends to rise in the age after 40. (Scherer, 2022) Gender GERD tends to occur in both men and women. However, The prevalence of having a GERD is higher amongst men. (Sang, 2019) Race Studies show that older Caucasians and Europeans in particular are more likely to have serious GERD than other ethnicities and countries. African Americans and Asians appear to be at lower risk for the development of complicated GERD (Scherer, 2022) Genetics A pattern has been observed of GERD amongst Multigenerational members of a family. However, the gene responsible cannot be determined yet. (Scherer, 2022) Precipitating factors Rationale Diet Caffeinated food and drinks such as coffee, tea, and colas aggravated GERD. Caffeine can trigger GERD symptoms as it can relax the lower esophageal sphincter (LES) which is the ring of muscle between the esophagus and stomach. (Healthline, 2018) Sedentary Lifestyle Inactivity such as seating for a longer period of time aggravates GERD. In fact, the American College of Sports Medicine notes that regular light to moderate exercise can reduce the occurrence of GERD. Exercise may work by strengthening the sphincter that 55 keeps the lower end of the esophagus closed. (Miller, 2021) Alcohol Alcohol is a known trigger of GERD. Also, alcohol is a diuretic, which means it Causes to urinate more often.This can lead to dehydration, which makes acid reflux symptoms worse. In addition, alcohol can also cause the LES to malfunction, which leads to increased symptoms of acid reflux. (Healthline, 2018) Smoking Relaxing the lower esophageal sphincter. Nicotine tends to relax smooth muscle inside the body. One of the body's main defenses against GERD is the lower esophageal sphincter. (Healthline, 2018) Stress A person's emotions can increase the acid production in the stomach, aggravating GERD. In people with GERD, the lower esophageal sphincter muscle doesn’t work properly thus allowing the acid to rise up from the stomach then to the esophagus. (Golen, 2022) Existing GI abnormalities Medical problems such as hiatal hernia, peptic ulcer, and connective tissue diseases if left untreated for so long may lead to another condition called GERD. (Hollman, 2022) Medication Medications such as anticholinergics, barbiturates, antacids, and H2 antagonists if taken too much can cause GERD. In specific, the H2 antagonist reduces the amount of acid that the stomach produces and helps treat GERD and has been a go to treatment of choice for many acid-related stomach conditions. (Carter, 2020) Pregnancy Gastroesophageal reflux disease (GERD) is reported 56 in up to 80% of pregnancies. It is likely caused by a reduction in lower esophageal sphincter pressure due to an increase in maternal estrogen and progesterone during pregnancy. (Todd, 2022) Obesity The notion that obesity may be causal in GERD makes biologic sense. Obesity may increase intraabdominal pressure, impair gastric emptying, decrease lower esophageal sphincter (LES) pressure and possibly increase transient LES relaxation, all of which could lead to increased esophageal acid exposure. (Todd, 2022) V. PATHOPHYSIOLOGY 57 Narrative: 58 Gastroesophageal reflux disease (GERD) or chronic acid reflux is a condition in which the acids produced in the stomach passes to the lower esophageal sphincter and back flows to the esophagus. This back flow of acids irritates the esophageal linings that could cause. since a person is exposed to a multifactorial factor namely predisposing and precipitating, disease such as GERD happens. The etiology of the disease is still idiopathic but multifactorial factors are being taken into consider. First, are the factors that predisposes the person like gender, age, race and genetics. A person that is prone to having this disease are those men and a person aging 40 years old and above mainly living in the northern part of the world but to be more specific is a caucasian and having a family history of this problem. Then we have what we called precipitating factors which are those caused by the bad choices and habits by the patient. Having poor diet, sedentary lifestyle, alcoholism, smoking, existing GI abnormalities such as hiatal hernia, medication use, obesity and stress; as well as pregnancy, patients are at high risk of getting this disease. When a person has been constantly affected by the factors mentioned above, it will result in the following. First, there will be delayed gastric emptying. Signs and symptoms of it include constipation. Second, there is an accumulation of gastric contents in the herniated part of the stomach and for obese and pregnant women the stomach becomes distended. These three factors increase pressure in the intra abdominal causing a pressure lower esophageal sphincter. In pregnancy, relaxin is produced, which is a hormone secreted by the placenta that causes the cervix to dilate in preparation for labor. This activates the collagenase where it will be broken down, reducing muscle strength of the stomach leading to relaxation of the lower esophageal sphincter. If there is a pressure to the LES and decreased muscle strength the LES weakens and impairs LES motility allowing the gastric acids to flow back into the esophagus. The esophageal lining cannot withstand the acidic nature of the acid reflux causing the lining to be irritated resulting in signs and symptoms of heartburn, regurgitation and epigastric pain. If this backflow continues it further reaches the larynx and irritates the laryngopharyngeal tissue resulting in hoarseness of voice and belching. When there is a further irritation the laryngopharyngeal tissue becomes inflamed and causes signs and symptoms lymphadenopathy, tonsil irritation, sore throat, difficulty in swallowing, coughing and dysphagia. On the other hand the vagus nerve is stimulated resulting in constriction of the airway and shortness of breath occurs. Furthermore, the gastric acids travel to the pharynx and to the mouth the salivary glands are stimulated this will increase the production of saliva. When the gastric acid mixes with saliva in the mouth this results in dysgeusia and increases acidity in the mouth and causes the enamel to erode tooth decay. If persistent reflux continues the esophagus will have an erosion and causes. First, the mucosal defenses will be unable to counteract the damage leading to local inflammation such as ulcer formation and 59 esophagitis. Second, there will be a development of scar tissue and narrowing of esophagus then blockages that prevent smooth flow of food in the stomach. Lastly, the squamous cells are replaced with intestinal cells which complicates Barrett's esophagus and will result in bleeding. These three problems mentioned above lead to permanent damage of esophagus if not treated that could further lead to cancer then death which results in poor prognosis. The diagnostic procedures are done such as CBC, urinalysis, Serum Electrolytes, CBG, FBS, ultrasound in the abdomen, pylori determination and upper gastrointestinal determination. Medical management given such as antiemetic medication, antiulcer, calcium channel blocker, h2 receptor antagonist, antibiotic and antibacterial medications are given to a person with GERD. Fundoplication and linx device implantation are surgical managements. All management mentioned will result in a good prognosis. VI. MEDICAL MANAGEMENT A. DIAGNOSTIC EXAMS TEST Upper Endoscopy RATIONALE NURSING RESPONSIBILITIES An endoscopy can also be Before: used to collect a sample of ● Answer patient questions tissue (biopsy) to be tested for and complications such as Barrett concerns esophagus. In some instances, procedure. if a narrowing is seen in the ● address their regarding the Keep the patient informed esophagus, it can be stretched throughout the duration of or dilated during this procedure. the procedure. This is done to improve trouble ● Secure informed consent. swallowing (dysphagia). ● Change the patient's gown. ● Preparing the instruments, equipment, and supplies for the procedure. ● Sedating patient before the procedure. During: 60 ● Observe patients vital signs. ● Assist the surgeon throughout the procedure. After: ● Complete documentation of the procedure. ● Reassess vital signs. ● Check for complications bloating, any such cramping, as and sore throat. ● Make the patient comfortable. Ambulatory acid (pH) probe test This is generally considered the Before: diagnostic gold standard for ● Instruct patient not to eat use in patients with GERD. pH and/or drink before the test help determine the causes procedure is done. and severity of ● Instruct patient not to take gastroesophageal reflux with antacids 24 hours before higher degrees of accuracy and catheter placement. comfort.In this study, a pH monitor is placed in ● the During: esophagus above the lower ● esophageal sphincter, and the pH is recorded at Do medical handwashing. Assist the doctor in inserting the tube. given After: ● moments in time. Complete documentation of the procedure. ● Make the patient comfortable. X-Ray Of The Upper Digestive System An upper doctors GI X-ray helps Before: find the cause of ● Provide relevant 61 swallowing problems, information to the client to unexplained vomiting, nausea, abdominal discomfort, and ease anxiety. ● severe indigestion. It can detect signs of problems such as Secure consent for the procedure. ● Look for allergies. Assess ulcers, gastric reflux, hiatal for any history of allergies hernia, to or blockages or narrowing of the upper GI tract. iodinated dye or shellfish, if contrast media is to be used. ● Get health history Ask the patient about any recent illnesses or other medical conditions and current medications being taken. The specific type of CT scan determines the need for an oral or contrast recent I.V. in medium, some illnesses may contraindicate the procedure. ● Check for NPO status- Instruct the patient to not to eat or drink for a period of time especially if a contrast material will be used. ● Encourage the patient to increase fluid intake (if a contrast is given). This is to promote excretion of the dye. ● Instruct the patient to 62 remove all metallic objects, including jewelry, hairpins, or watches. After: ● Encourage the patient to take plenty of water to excrete contrast medium in the urine. ● Make the patient comfortable. Esophageal Manometry This test measures the Before: rhythmic muscle contractions in ● your esophagus when you swallow. Esophageal Explain the procedure process to the patient. ● Make sure the patient has manometry also measures the been NPO for 8 hours and coordination and force exerted aware no sedation will be by given. the muscles of your esophagus. This is typically ● done in people who have trouble swallowing. Secure consent for the procedure. ● Assure no clothing is restricting the abdomen. During: ● While the patient is in the sitting position gently insert the probe into the patient's nares, down the back of the throat into the esophagus until the probe tip reaches the stomach. ● A topical anesthetic may be instilled into the nose to make passage of the 63 probe more comfortable. ● The patient may take sips of water to assist with probe placement. After: ● Document all the relevant data from the procedure. ● Make the patient comfortable. Transnasal Esophagoscopy Transnasal esophagoscopy Before: (TNE) is a minimally invasive outpatient procedure ● that Answer patient questions and address utilizes an ultra thin endoscope concerns inserted procedure. through passages esophagus patients to the nasal examine and the ● evaluate experiencing their regarding the Keep the patient informed throughout the duration of acid the procedure. chronic ● Secure informed consent. cough and globus sensation ● Change reflux, dysphagia, (the feeling of a lump in the throat). the patient's gown. ● Preparing the instruments, equipment, and supplies for the procedure. ● Sedating patient before the procedure. During: ● Observe patients vital signs. ● Assist the surgeon throughout the procedure. After: ● Complete documentation 64 of the procedure. ● Reassess vital signs. ● Check for complications bloating, any such cramping, as and sore throat. ● Make the patient comfortable. B. MEDS 1. Antacids - When the stomach contents back up into the esophagus, it causes heartburn because your esophagus is not built to withstand acidity, especially over a prolonged period of time. Antacids help neutralize these acids, so the esophageal lining is less exposed to gastric acids. GENERIC NAME Calcium Carbonate, Aluminum Hydroxide, Magnesium hydroxide, Simeticone BRAND NAME Kremil-S DRUG CLASSIFICATION Antacids with antiflatulents SUGGESTED DOSE To relieve heartburn in adults and children 12 years and older: 1 tablet as needed. Or, as directed by a doctor. Chew the tablet completely before swallowing. Do not use more than 2 chewable tablets in 24 hours. ROUTE OF ORAL, IV ADMINISTRATION MODE OF ACTION This product contains a combination of antacids, Aluminum Hydroxide and Magnesium Hydroxide, which effectively increase gastric pH by neutralizing the acid produced in the stomach. 65 INDICATION This medicine is used for the relief of heartburn associated with acid indigestion and hyperacidity. CONTRAINDICATION Contraindicated in patients with advanced kidney disease are at risk of Aluminum and Magnesium accumulation and toxicity. Do not use these products in such patients. SIDE EFFECTS ● CNS: Headache, dizziness, paresthesia, depression, anxiety, somnolence, insomnia, fever, seizures in renal disease CV: Dysrhythmias, QT prolongation (impaired renal functioning) ● EENT: Taste change, tinnitus, orbital edema GI: Constipation, nausea, vomiting, anorexia, cramps, abnormal hepatic enzymes, diarrhea INTEG: Rash, toxic epidermal necrolysis, Stevens-Johnson syndrome ● ADVERSE EFFECTS MS: Myalgia, arthralgia RESP: Pneumonia Famotidine: Famotidine is generally well tolerated. ● Undesirable effects involving stomach and intestines include: constipation, diarrhea, nausea, vomiting, abdominal and gas-related discomfort, decreased appetite, dry mouth, heartburn, and loss of taste. ● Famotidine may also cause the following skin reactions: acne, itching, red, itchy patches on the skin (hives), rash and dry skin. Headache, dizziness, weakness, fatigue, muscle weakness, seizures, insomnia, drowsiness, depression, confusion, disorientation, anxiety, decreased sexual desire, and hallucinations have been reported. ● Famotidine may also cause kidney problems (e.g., increased serum creatinine concentration and abnormal amounts of protein in the urine) and liver disease such as yellowing of the skin (jaundice). ● Other undesirable effects include: fever, hypertension, 66 flushing, muscle cramps, pain in the joints, ringing in the ears (tinnitus), and community-acquired pneumonia. Antacids: Flatulence from increased carbon dioxide may occur in some patients. ● Calcium carbonate can stimulate acid rebound in some people. Acid rebound causes the stomach to produce even more acid, making heartburn worse. This, however, is very rare. ● Excessive doses of calcium carbonate and magnesium hydroxide may result in high calcium and magnesium levels in the blood in patients with kidney impairment. ● Alkalosis (excess base in body fluids) may also occur with excessive doses of antacid. DRUG INTERACTIONS ● Food appears to slightly increase and antacids appear to slightly decrease the absorption of famotidine, but these effects do not appear to be clinically important. ● Unlike cimetidine, famotidine is considered to have little effect on the actions of other drugs such as warfarin, theophylline, phenytoin, diazepam, or procainamide. ● Antacids may interact with other drugs such as propranolol, isoniazid, prednisolone, diflunisal, and naproxen which may cause formation of complexes that are not absorbed. ● Antacids decrease the absorption of tetracycline and iron. Take tetracycline 1 hour before or 2 hours after antacids and 2 hours before or 3 hours after iron preparations and vitamin products that contain iron. NURSING RESPONSIBILITIES 1. Assess the patient for history of allergies, R: The antacids are contraindicated in the presence of any known allergy to antacid products or any component of the drug to prevent hypersensitivity reactions. 2. Instruct patient to take drug with food. 67 R: It's best to take antacids with food or soon after eating because this is when you're most likely to get indigestion or heartburn. The effect of the medicine may also last longer if taken with food. 3. Monitor the compliance with the regimen. R: To achieve maximum desired effect. 4. Teach patient to avoid taking other medications within 2 hours of taking the antacid. R: certain drugs may interact with the antacid and effectiveness may diminish. 5. Encourage the client to lie on the left side with the head of the bed elevated when complaints of chest discomfort arise after administering antacid. R: to relieve and make the client comfortable. 6. Assess for renal function. R: patients with decreased renal function are at risk for prolonged QT. 7. Instruct patient to avoid taking alcoholic beverages. R: May increase or worsen the condition. 8. Instruct patient to avoid smoking. R: It diminishes the effectiveness of the drug. 9. Instruct patient/watcher to avoid tasks requiring alertness. R: Dizziness and drowsiness may occur. 10. Teach the patient/ family that the product must be continued for prescribed time in the prescribed method. R: To achieve maximum effect. 2. Antiulcer - Both classes of antiulcer medications block the pathways of acid production or secretion, decreasing gastric acidity, improving symptoms and aiding in healing of acid-peptic diseases. 68 GENERIC NAME Famotidine (Pepcid) BRAND NAME Pepcid DRUG CLASSIFICATION Antiulcer agent (H2 antagonist) SUGGESTED DOSE Adult Dose: ● Duodenal ulcer: ○ 40 mg orally every night at bedtime for 4-8 weeks, then 20mg thereafter if needed for maintenance. ○ IV; 20mg every 12 hours if unable to tolerate PO ● Gastric Ulcer: ○ ● 40 mg orally every night at bedtime GERD: ○ PO 20 mg twice daily for up to 6 weeks; for esophagitis due to GERD, 20-40 mg twice daily for up to 12 weeks ● Hypersecretory conditions: ○ PO 20 mg every 6 hours; may give 160 mg every 6 hours if needed. ○ IV 20 mg every 12 hours if unable to tolerate PO ● Heartburn or acid indigestion: ○ PO 10mg twice daily; to prevent heartburn, 69 10mg 1 hour before meals ● Renal failure: ○ PO 20 mg at bedtime or increase dosing interval to 36-48 hours ROUTE OF ORAL, IV ADMINISTRATION MODE OF ACTION inhibit acid secretion by blocking H2 receptors on the parietal cell (figure 1). H2RAs are well absorbed after oral dosing; peak serum concentrations occur within one to three hours. INDICATION ● Short term and maintenance duodenal ulcer therapy ● Short term benign gastric ulcer therapy ● Pathological hypersecretory conditions (ZollingerEllison syndrome) ● Gastroesophageal disease (GERD) and esophagitis due to GERD CONTRAINDICATION Famotidine is contraindicated for use by patients with serious hypersensitivity to famotidine itself or any component of the formulation. Cross-sensitivity of H2RAs has been observed; therefore, famotidine should not be administered to patients with a history of hypersensitivity to cimetidine. SIDE EFFECTS ADVERSE EFFECTS headache, dizziness, constipation, and diarrhea. ● CNS: anxiety, depression, dizziness, fever, headache, insomnia, paresthesia, seizures, somnolence ● EENT: Orbital edema, taste change, tinnitus ● HEME: Thrombocytopenia ● RESP: Bronchospasm ● Arthralgia, myalgia, rash 70 DRUG INTERACTIONS ● Reduction of gastric acidity reduces absorption and introduces potential for therapeutic failure: ketoconazole, enoxacin, cefpodoxime, cefuroxime ● Increased absorption, potential for hypoglycemia: glipizide, glyburide ● NURSING RESPONSIBILITIES Increased concentrations: nifedipine, nisoldipine 1. Monitor renal function. R: Famotidine is substantially excreted by the kidneys. 2. Monitor patient's complete blood count (CBC), gastric pH and occult blood in patients with gastrointestinal (GI) bleeding. R: may cause serious adverse effects. 3. Monitor patient for any allergic reactions such as rash, itching/swelling (especially of the face/tongue/throat), severe dizziness, trouble breathing. R: This product may contain inactive ingredients, which can cause allergic reactions or other problems and provide immediate intervention. 4. Advise patient to administer drug at bedtime. R: Gastrointestinal reflux is most likely to occur during evening or nighttime hours. Because of this, famotidine may be most effective in controlling reflux when it is taken around the time of an evening meal. 5. Instruct patient to take drug one hour before eating. R: to prevent indigestion. 6. If headache occurs, adjust lights, temperature, and noise levels. R: to aid the side effect. 7. Instruct patient/watcher to avoid tasks requiring alertness. R: Dizziness and drowsiness may occur. 8. Instruct older adult patients to report any unusualities. 71 R: mental/ mood changes, seizure, and unusual tiredness may occur during treatment regimen. 9. Instruct patient to notify the health care provider if pregnancy is planned or suspected or if breastfeeding. R: drug is under pregnancy category B. 10. Instruct patient not to take more or less of it or take it more often or for a longer time than prescribed by the doctor. R: minimize adverse effects from happening. 3. Antiemetic - Prokinetic agents are used to induce gastric motility, whereas antiemetic agents are used to relieve symptoms of nausea and vomiting. GENERIC NAME Metoclopramide BRAND NAME Reglan DRUG CLASSIFICATION GI stimulant, Antiemetic, Dopaminergic blocker SUGGESTED DOSE Nausea/vomiting (chemotherapy) ● Adult: IV 1-2 mg/kg 30 min before administration of chemotherapy, then q2hr × 2 doses, then q3hr × 3 doses ● Child (unlabeled): IV 1-2 mg/kg/dose Facilitate small-bowel intubation for radiologic exams ● Adult and child >14 yr: IV 10 mg over 1-2 min ● Child <6 yr: IV 0.1 mg/kg ● Child 6-14 yr: IV 2.5-5 mg Diabetic gastroparesis ● Adult: PO 10 mg 30 min before meals, at bedtime × 2-8 wk ● Geriatric: PO 5 mg 30 min before meals, at bedtime, increase to 10 mg if needed Gastroesophageal reflux 72 ● Adult: PO 10-15 mg qid 30 min before meals and at bedtime ● Child: PO 0.4-0.8 mg/kg/day in 4 divided doses Renal dose ● Adult: PO CCr <60 mL/min, 5 mg qid, max 20 mg/day, or CCr 10-15 mL/min give 75% of normal dose; CCr <10 mL/min give 50% of normal dose. ROUTE OF PO, IM, IV ADMINISTRATION MODE OF ACTION Metoclopramide enhances the motility of the upper GI tract and increases gastric emptying without affecting gastric, biliary or pancreatic secretions. It increases duodenal peristalsis which decreases intestinal transit time, and increases lower esophageal sphincter tone. It is also a potent central dopaminereceptor antagonist and may also have serotonin-receptor (5HT3) antagonist properties. INDICATION Metoclopramide is used to treat the symptoms of slow stomach emptying (gastroparesis) in patients with diabetes. It works by increasing the movements or contractions of the stomach and intestines. It relieves symptoms such as nausea, vomiting, heartburn, a feeling of fullness after meals, and loss of appetite. Metoclopramide is also used to treat heartburn for patients with gastroesophageal reflux disease (GERD). GERD is esophageal irritation from the backward flow of gastric acid into the esophagus. CONTRAINDICATION H sensitivity to this product, procaine, or procainamide; seizure disorder, pheochromocytoma, GI obstruction Precautions: Pregnancy, disease, breastfeeding, breast cancer GI hemorrhage, (prolactin Parkinson’s dependent), abrupt discontinuation, cardiac disease, children, depression, diabetes 73 mellitus, G6PD hypertension, deficiency, infertility, geriatrics, malignant heart failure, hyperthermia, methemoglobinemia, procainamide/paraben hypersensitivity, renal impairment. SIDE EFFECTS ● CNS: Sedation, fatigue, restlessness, headache, sleeplessness, dystonia, dizziness, drowsiness ● CV: Hypotension, supraventricular tachycardia ● GI: Dry mouth, constipation, nausea, anorexia, vomiting, diarrhea ● GU: Decreased libido, prolactin secretion, amenorrhea, galactorrhea ADVERSE EFFECTS ● INTEG: Urticaria, rash ● CNS: suicidal ideation, seizures, EPS, neuroleptic malignant syndrome; tardive dyskinesia (>3 mo, high doses) DRUG INTERACTIONS ● HEMA: Neutropenia, agranulocytosis ● Avoid use with MAOIs; may increase hypertension in those patients Increase: sedation—alcohol, other CNS depressants; avoid concurrent use ● Increase: risk for EPS—haloperidol, phenothiazines; assess for EPS ● Decrease: action—anticholinergics, opiates; avoid using together or assess carefully Drug/Lab Test ● NURSING RESPONSIBILITIES Increase: prolactin, aldosterone, thyrotropin 1. Assess history to metoclopramide. R: to allow safe prescription and avoidance of the specific drug or drug class. 2. Monitor vital signs, especially BP. R: ECG may result in QT Prolongation. 3. Assess for mental status. 74 R: Drug effects may lead to depression, anxiety, and irritability. 4. Assess for involuntary movements often. R: Treatment with metoclopramide can cause tardive dyskinesia, a serious movement disorder that is often irreversible. The risk of developing tardive dyskinesia increases with duration of treatment and total cumulative dose. 5. Monitor the compliance with the regimen. R: To achieve maximum desired effect. 6. Instruct patient to intake the drug with food. R: GI irritation may occur. 7. Instruct patient/watcher to avoid tasks requiring alertness. R: Dizziness and drowsiness may occur. 8. Instruct patient to avoid alcohol intake. R: can cause extrapyramidal effects. 9. Instruct patient to take this drug exactly as prescribed. R: to achieve maximal effect and avoid unwanted side effects. 10. Teach the patient/ family that the product must be continued for prescribed time in the prescribed method. R: To achieve maximum effect. 4. Proton Pump Inhibitor - Many people take PPIs for gastroesophageal reflux disease (GERD). By lowering stomach acid levels, they reduce acid reflux into the esophagus and the resulting heartburn symptoms. GENERIC NAME BRAND NAME Esomeprazole Nexium 75 DRUG CLASSIFICATION Proton Pump Inhibitor SUGGESTED DOSE Gastro-oesophageal reflux disease ● ORAL ○ Adult: Erosive reflux oesophagitis: 20 mg or 40 mg once daily for 4-8 weeks, may extend for an additional 4-8 weeks if necessary. Maintenance (to prevent relapse of erosive oesophagitis): 20 mg once daily for up to 6 months. Symptomatic treatment of GERD (without oesophagitis): 20 mg once daily for 4 weeks, may extend for an additional 4 weeks if necessary. ○ Child: As granules for oral susp: 1 month to <1 year Erosive reflux oesophagitis: 3-5 kg: 2.5 mg once daily for up to 6 weeks; >5-7.5 kg: 5 mg once daily for up to 6 weeks; >7.5-12 kg: 10 mg once daily for up to 6 weeks. 1-11 years Erosive reflux oesophagitis: <20 kg: 10 mg once daily for 8 weeks; ≥20 kg: 10 mg or 20 mg once daily for 8 weeks. Symptomatic treatment of GERD: 10 mg once daily for up to 8 weeks. As tab, cap, or granules for oral susp: 12-17 years Erosive reflux oesophagitis: 20 mg or 40 mg once daily for 4-8 weeks. Symptomatic treatment of GERD (without oesophagitis): 20 mg once daily for 4 weeks. ● IV ○ Adult: Erosive reflux oesophagitis: 40 mg once daily. Symptomatic treatment: 20 mg once daily. Doses are given via slow inj over at least 3 minutes or infusion over 10-30 minutes. Treatment duration: Up to 10 days. Switch to oral therapy as soon as possible. 76 ○ Child: 1-11 years Erosive reflux oesophagitis: <20 kg: 10 mg once daily; ≥20 kg: 10 mg or 20 mg once daily. Symptomatic treatment of GERD: 10 mg once daily. 12-18 years Same as adult dose. Doses are given via slow inj over at least 3 minutes or infusion over 10-30 minutes. Switch to oral therapy as soon as possible. Dosage recommendations may vary among countries and individual products (refer to specific product guidelines). ROUTE OF PO, IV, PARENTERAL ADMINISTRATION MODE OF ACTION Suppress gastric actions by inhibiting hydrogen/potassium ATPase enzyme system in gastric parietal cell; characterized as gastric acid pump inhibitor because it blocks the final step of acid production. INDICATION ● Relieve symptoms of acid reflux, or gastroesophageal reflux disease (GERD). This is a condition in which food or liquid moves up from the stomach to the esophagus (the tube from the mouth to the stomach). ● Treat a duodenal or stomach (gastric) ulcer. ● Treat damage to the lower esophagus caused by acid reflux. CONTRAINDICATION Hypersensitivity to proton pump inhibitors (PPIs) Precautions: Pregnancy, breastfeeding, children, geriatric patients, hypomagnesemia, osteoporosis. SIDE EFFECTS ● headache ● nausea ● diarrhea 77 ADVERSE EFFECTS ● gas ● constipation ● dry mouth ● drowsiness ● blisters, peeling, or bleeding skin; sores on the lips, nose, mouth, or genitals; swollen glands; shortness of breath; fever; or flu-like symptoms ● rash; hives; itching; swelling of the eyes, face, lips, mouth, throat, or tongue; difficulty breathing or swallowing; or hoarseness ● irregular, fast, or pounding heartbeat; muscle spasms; uncontrollable shaking of a part of the body; excessive tiredness; lightheadedness; dizziness; or seizures ● severe diarrhea with watery stools, stomach pain, or fever that does not go away ● new or worsening joint pain; rash on cheeks or arms that is sensitive to sunlight ● increased or decreased urination, blood in urine, fatigue, nausea, loss of appetite, fever, rash, or joint pain. DRUG INTERACTIONS ● Increase: effect, toxicity of diazePAM, digoxin, penicillins, saquinavir, cilostazol, cloZAPine, those drugs metabolized by CYP2C19 ● Increase: effect of methotrexate, tacrolimus, warfarin ● Decrease: effect—atazanavir, nelfinavir, dapsone, iron, itraconazole, carbonate, ketoconazole, vit B12 , indinavir, clopidogrel, iron calcium salts, mycophenolate Drug/Lab Test ● Interference: sodium, Hgb, WBC, platelets, magnesium False-positive CgA 78 NURSING RESPONSIBILITIES 1. Monitor improvements in GI symptoms (gastritis, heartburn, and so forth). R: to help determine if drug therapy is successful. 2. Monitor the compliance with the regimen. R: To achieve maximum desired effect. 3. Instruct patient/ watcher to avoid hazardous activities. R: dizziness may occur. 4. Instruct patient to report any severe GI symptoms. R: to immediately provide immediate intervention or have the drug discontinued. 5. Instruct patient to take drug one hour before meal. R: Esomeprazole should be taken in the morning on an empty stomach to optimize benefits/ maximum absorption. 6. Instruct patient not to crush and chew drug. R: to get the maximum absorption of the drug. 7. Instruct patient to take drug as soon as remembered if missed. Do not double dose. R: To avoid double dosing and getting your disease worse. 8. Instruct patient/ watcher to notify health care provider if pregnancy is planned or suspected or if breastfeeding. R: drug is under pregnancy category C. 9. Advise patient to discontinue/ avoid St. John’s wort herb while taking esomeprazole. R: It may stop esomeprazole working as well as it should. 10. Advise patient to avoid alcohol and foods that may cause an increase in GI irritation. C. TREATMENT 79 TREATMENT RATIONALE NURSING RESPONSIBILITIES Lifestyle and dietary Dietary and lifestyle changes changes are the first step in treating low residue diet to relieve GERD. Certain foods make abdominal the reflux worse. diarrhea. ● ● Instruct patient to follow a pain and If the patient experiences strictures, instruct them to avoid eating nuts, seeds, beans and kernels. ● Instruct to avoid foods that may increase stool output such as fresh fruits and vegetables, prunes and caffeinated beverages. Medication If lifestyle and dietary changes ● Instruct patient to take do not work, the doctor may medication on the prescribe certain medications. prescribed time and There are two categories of amount. medicines for reflux. One ● decreases the level of acid in your stomach, and one Instruct patient not to double dose. ● Encourage patient to report increases the level of motility any adverse effects of the (movement) drug administered. in the gastrointestinal tract. upper ● Instruct patient to take full course of the drug. VII. SURGICAL MANAGEMENT Surgery for GERD is known as antireflux surgery and involves a procedure called a fundoplication. The goal of a fundoplication is to reinforce the LES to recreate the barrier that stops reflux from occurring. 80 PROCEDURE Nissen fundoplication RATIONALE NURSING RESPONSIBILITIES The Nissen fundoplication is Preoperative: almost always chosen to control GERD. This wrapping a is done portion of by regarding the procedure. ● Instruct patient not to the esophagus in an effort to smoke or take any NSAIDS strengthen, or or Aspirin products up to 1 recreate the LES valve. The week prior to surgery date. most augment, common type fundoplication is a fundoplication in which stomach wrapped degrees is around of Transoral ● Nissen the 2-3 miles a day prior to surgery to get in the best 360 shape possible for surgery. lower ● Obtain informed consent. ● Change the patient's gown. ● Preparing the instruments, incisionless equipment, and supplies fundoplication is a minimally invasive procedure for GERD. Unlike the fundoplication incisions in the transoral fundoplication for the procedure. ● laparoscopic that requires abdomen, Intraoperative: ● Instruct patient not to eat or drink performed anything after midnight the night prior to through the mouth, without incisions. Sedating patient before the procedure. incisionless is Encourage patient to walk the esophagus. fundoplication Answer patient questions and address their concerns the stomach around the bottom of Transoral incisionless ● surgery. ● Observe patients vital signs. ● Assist the surgeon throughout the procedure. Postoperative: ● Complete documentation of the procedure. 81 ● Reassess vital signs. ● Check for complications bloating, any such cramping, as and sore throat. ● Make the patient comfortable. VIII. NURSING MANAGEMENT NURSING DIAGNOSIS GOAL INTERVENTION Imbalanced Nutrition: Less After 8 hours of nursing 1. Accurately measure the Than Body Requirements care, the patient will be able patient’s related to inability to intake to: height. enough food because of reflux as evidenced by a. ingest daily nutritional weight loss. requirements 2. Obtain a nutritional history. accordance activity common cause is food that's and Rationale: For baseline data. inadequate food intake and Rationale: The most weight in Rationale: to level Determining the his feeding habits of the client can and provide a basis for establishing a metabolic needs. nutritional plan. b. demonstrating acidic or high in fat—like healthy eating 3. Encourage small frequent citrus fruits, tomatoes, patterns and choices. meals of high calories and onions, chocolate, coffee, c. verbalization of high-protein foods. cheese, and peppermint. selection of foods or Rationale: Small and frequent Spicy foods or large meals meals can also be the root of achieve a cessation distress. Other sources of of weight loss. heartburn include aspirin or that will meals are easier to digest. 4. Provide a pleasant environment. ibuprofen, as well as some Rationale: sedatives and blood atmosphere helps in decreasing A pleasing 82 pressure medications.They stress and is more favorable to may experience nausea and eating. difficulty or pain when they swallow. Over time, the 5. Instruct to remain in an condition may lead to a loss upright position at least 2 of appetite and persistent hours after meals; avoid vomiting, indicating eating complications of GERD. bedtime. 3 hours before Rationale: Helps control reflux and causes less irritation from Reference: MediLexicon reflux action in the esophagus. International. (n.d.). Acid reflux and weight loss: 6. Instruct the patient to eat Causes, dangers, slowly and masticate foods management. Medical News well. Today. Retrieved from Rationale: Helps prevent reflux. https://www.medicalnewstod ay.com/articles/acid-refluxweight-loss 7. Provide oral hygiene. Rationale: A clean mouth can enhance the taste of food. 8. Instruct in the importance of abstaining from excessive alcohol. Rationale: Alcohol causes gastric irritation and increases gastric pain 9. Encourage the client to limit the caffeinated intake of beverages such as tea and coffee. Rationale: Caffeine stimulates the 83 secretion of gastric acid. It contains a peptide that stimulates the release of gastrin and increases acid production. 10. Prepare the patient for CBC procedure. Rationale: To identify the presence of anemia that must be ruled out. Acute Pain related to After 1 hour of nursing care, 1. Perform a comprehensive aspiration as evidenced by the patient will be able to: assessment pain scale of 7 out of 10. Determine a. report pain is relieved Rationale: to 0 out of 10 Aspiration of large amounts b. demonstrate the use the pain. location, characteristics, duration, onset, frequency, quality, and severity of of gastric acid will result in of the induction of a chemical diversional activities Rationale: It helps the nurse in injury to the airways and lung and relaxation skills. parenchyma. The initial insult triggers a cascade of inflammatory responses with the recruitment of appropriate of c. Display improvement pain via assessment. planning optimal pain management strategies. in mood, coping. 2. Determine the client’s perception of pain. inflammatory cells and the Rationale: Provide an opportunity release for the client to express in their of various inflammatory mediators own words how they view the pain Stomach acid can break and the situation to gain an down understanding of what the pain tissue esophagus, in the causing means to the client. inflammation, bleeding, and sometimes an open sore. 3. Pain assessments must be initiated by the nurse. 84 Reference: Sullivan, Hunt, E. B., J., unique for each person, and some MacSharry, J., & Murphy, D. clients may be reluctant to report M. (n.d.). Gastric aspiration or voice out their pain unless and asked about it. its A., role inflammation. Galvin, Rationale: Pain responses are in The airway open respiratory medicine journal. Retrieved from 4. Determine the patient’s anticipation for pain relief. https://www.ncbi.nlm.nih.gov Rationale: This influences the /pmc/articles/PMC5806178/ perceptions of the effectiveness of the treatment modality and their eagerness to engage in further treatments. 5. Assess the patient’s willingness or ability to explore a range of techniques to control pain. Rationale: A combination of both therapies may be more effective, and the nurse has the duty to inform the patient of the different methods to manage pain. 6. Determine factors that alleviate pain. Rationale: Ask clients to describe anything they have done to alleviate the pain. 7. Evaluate response the to patient’s pain and management strategies. 85 Rationale: It is essential to assist patients to express as factually as possible the effect of pain relief measures. 8. Provide ample time and effort regarding the patient’s report of their pain experience. Rationale: Patients may be reluctant to report their pain as they may perceive staff to be very busy and have competing demands on their time from other nurses. 9. Provide measures to relieve pain such as deep breathing exercises before it becomes severe. Rationale: It is preferable to provide an analgesic before the onset of pain or before it becomes severe when a larger dose may be required. 10. Acknowledge and accept the client’s pain. Rationale: Nurses have the duty to ask their clients about their pain and believe their reports of pain. Deficient Knowledge related After 8 hours of nursing 1. Identify the learner: the 86 to lack of information care, the patient will be able patient, regarding the condition as to: significant evidenced by verbalization of problems and questions. family, other, or caregiver. a. express comprehension R: Some patients, especially older regarding the signs and adults or the terminally ill view symptoms of GERD. themselves as dependent on the Rationale: Identifying a lack caregiver, therefore will not allow of cognitive information or b. recognize factors that themselves to be part of the psychomotor ability required may worsen GERD and educational process. for restoring, maintaining, or cause its symptoms to promoting health is referred intensify. 2. Assess ability to learn or to as a knowledge deficit. Knowledge is a crucial factor in a patient's recovery and daily life. I The nurse has the responsibility to work with perform desired healthc. demonstrate understanding of the therapeutic regimen for treating GERD. related care. R: Cognitive impairments must be recognized so an appropriate teaching plan can be outlined. the patient to determine what to teach, when to teach, and 3. Assess the motivation and how to teach matters related willingness of the patient to to learn. health. The teaching- learning process is guided by R: principles of adult learning. Patients must see a need or Learning requires energy. purpose for learning. They also have Reference: Wagner, M. the right to refuse educational services. (2023, January 9). Knowledge deficit nursing 4. Determine priority of diagnosis & care plan. learning needs within the NurseTogether. Retrieved overall care plan. from R: This is to know what needs to https://www.nursetogether.c be discussed especially if the om/knowledge-deficit- patient already has a background about the situation. Knowing what 87 nursing-diagnosis-care-plan/ to prioritize will help prevent wasting valuable time. 5. Allow the patient to open up about experience previous and health teaching. R: Older patients often share life experiences at each learning session. They learn best when teaching builds on previous knowledge and experience. 6. Observe and note existing misconceptions regarding material to be taught. R: Assessment important provides starting point an in education. Knowledge serves to correct faulty ideas. 7. Acknowledge racial/ethnic differences at the onset of care. R: Acknowledgement racial/ethnicity enhance issues of will communication, establish rapport, and promote treatment outcomes. 8. Identify cultural influences on health teaching. R: Interventions need to be 88 specific to considering each their patient individual differences and backgrounds. 9. Consider the patient’s learning style, especially if the patient has learned and retained new information in the past. R: Every individual has his or her learning style, which must be a factor in planning an educational program. Matching the learner’s preferred style with the educational method will facilitate success in mastery of knowledge. 10. Assess barriers to learning (e.g., perceived change in lifestyle, financial concerns, cultural patterns, lack of acceptance by peers or coworkers). R: The patient brings to the learning situation a unique personality, established social interaction patterns. IX. LITERATURE New Research could change How Clinicians diagnose, Treat Unmanaged Heartburn (Robinson, 2019) 89 Robinson, E. (2019. New research could change how clinicians diagnose, treat Unmanaged Heartburn. OHSU News. Retrieved from https://news.ohsu.edu/2019/10/23/new-research-could-change-how-clinicians-diagnosetreat-unmanaged-heartburn Gastroesophageal reflux disease (GERD) is a prevalent digestive disorder that affects a significant percentage of the US adult population, with a higher prevalence in individuals aged 40 years or older. However, GERD is not limited to adults, as babies and children may also experience chronic acid reflux, with about a quarter of children displaying GERD symptoms. The underlying issue causing heartburn and reflux is a weakened muscle at the top of the stomach that is meant to remain closed between swallowing to keep stomach acid in check, which does not function optimally in patients with GERD, leading to acid reflux. Recent research has demonstrated that a substantial number of individuals who continue to experience heartburn symptoms despite taking proton pump inhibitors (PPIs) may not actually have GERD as the root cause of their discomfort. Instead, they may be suffering from a range of other conditions that cause a similar burning sensation in the chest, which can be difficult to differentiate from heartburn caused by GERD. To ascertain the underlying cause of persistent heartburn, the study utilized a comprehensive battery of tests that were specifically designed to identify conditions other than GERD that could be contributing to heartburn symptoms. This allowed the researchers to determine whether the heartburn was linked to reflux of stomach contents into the esophagus prior to considering surgical intervention as a treatment option. A New Device is Helping Treat Acid Reflux and Heartburn (Dickson, 2022) Dickson, D. (2022). A new device is helping treat acid reflux and Heartburn ahead of the holidays. 25 News KXXV and KRHD. Retrieved from www.kxxv.com/brazos/a-newdevice-is-helping-treat-acid-reflux-and-heartburn-ahead-of-the-holidays A novel medical device has been developed in 2022 to address acid reflux and heartburn. The LINX Reflux Management System utilizes metal beads and is employed in a minimally invasive surgical procedure where a flexible ring of small magnets is positioned around the esophagus, just above the stomach. This procedure is designed to assist in the prevention of reflux. The LINX system is suitable for individuals who have been diagnosed with GERD through pH testing and desire an alternative to continuous acid suppression therapy. Testimonies have conveyed 90 immediate results and have expressed their satisfaction and relief with the said new device as medication to GERD. However, prospective LINX recipients should be healthy enough for surgery, at least 21 years of age, and have successfully managed their weight. Before undergoing antireflux surgery, a gastroenterologist will conduct pre-operative esophageal testing to determine its efficacy. Two surgeries for Chronic GERD yield Similar Long-term Outcomes (Hamza, 2022) Hamza, Z. (2022). Two surgeries for chronic GERD yield similar long-term outcomes. Medical News. Retrieved from https://www.medpagetoday.com/gastroenterology/gerd/98325 GERD has been a persistent condition affecting a significant portion of the global population for many years. Its prevalence ranged from 18.1% to 27.8% in North America, 8.8% to 25.9% in Europe, 2.5% to 7.8% in East Asia, 8.7% to 33.1% in the Middle East, 11.6% in Australia, and 23.0% in South America. Moreover, there are various surgical and non-surgical methods for treating GERD. A recent randomized trial conducted in Sweden found that laparoscopic partial or total fundoplication was similarly effective in improving the ability to swallow solid and liquid foods, controlling reflux, and enhancing the quality of life in patients with chronic GERD. The trial recruited 456 patients with GERD from 2001 to 2006, and the present analysis included 301 of the 407 patients who completed follow-up questionnaires after 16 years. The study found no significant differences in daily proton pump inhibitor use or additional surgery for recurrent GERD between the two groups. This suggests that laparoscopic partial or total fundoplication could be a valuable surgical option for patients with chronic GERD who seek long-term symptom relief. GASTROENTERITIS I. DEFINITION The term "gastroenteritis" also refers to the stomach or intestinal flu that is brought on by a virus, chemical, medication, bacteria, or parasite. It comes in four different forms: bacterial gastroenteritis, bacillary dysentery, amebic gastroenteritis, and viral gastroenteritis. The most typical form of gastroenteritis is viral, and the rotavirus is the virus that mostly causes it. It affects and irritates the digestive system, especially the stomach and intestines, or both, which frequently causes diarrhea, abdominal cramps, nausea, and vomiting. Gastroenteritis can be transmitted 91 from person to person by viruses, bacteria, and parasites. When contacting an object with the germs on it and then touching their eyes, mouth, or nose, they could become infected. II. ANATOMY/ PHYSIOLOGY The alimentary canal, commonly known as the gastrointestinal tract, and the accessory organs are the two main parts of the digestive system. Essentially, it serves two purposes. Two things happen during digestion: first, food and liquids are converted into simple chemicals that may be taken into the bloodstream and carried throughout the body; and second, wastes are expelled through the stools. The person's general health will be significantly impacted if this system fails, making it crucial. A muscular hollow tube called the alimentary canal extends from the mouth to the anus. The pharynx, esophagus, stomach, small intestine, and large intestine are also included. The liver, biliary duct system, and pancreas are examples of auxiliary organs in contrast. Mouth It focuses mostly on swallowing, salivating, and chewing food. The sensation of taste is provided by the tongue, and saliva moistens the food as it is being chewed. The parotid, submandibular, and sublingual salivary glands generate saliva. Pharynx or Throat It is a cavity that connects the esophagus to the mouth cavity. In addition to accelerating the meal toward the esophagus, it aids in swallowing. Esophagus 92 It is a muscular tube that connects the throat to the stomach by passing through the mediastinum. The cricopharyngeal sphincter relaxes as food is swallowed, allowing it to pass into the esophagus. After that, peristalsis forces food and water into the stomach from the esophagus. Stomach It is a collapsible, pouch-like structure in the left upper region of the belly, right below the diaphragm, and it serves as the body's food storage. Its top border is joined to the esophagus' lower end. The cardiac and pyloric sphincters are located in the stomach. The stomach converts food into chime, a semifluid material, creates the intrinsic factor required for vitamin B12 absorption, and transports the contents of the stomach to the small intestine. Small Intestine It is roughly 6 meters long, and it is where the majority of digestion and nutritional absorption happens. It also has to do with the hormones' production, which regulates the release of bile, pancreatic juice, and intestinal juice. There are three sections: the duodenum, jejunum, and ileum. The villi, which are finger-like projections on the mucosa, the microvilli, which are tiny projections on the surface of epithelial cells, and the plicae circulars, which are circular folds on the mucosa, are some of the structures in the small intestine that aid in absorption. Large Intestine or Colon It retains food scraps, absorbs extra water and electrolytes, and excretes waste in the form of feces. Cecum, ascending colon, transverse colon, descending colon, sigmoid colon, and rectum are the six segments that make up this organ. Liver It has four lobes: the left, right, caudate, and quadrate. It is situated in the right upper quadrant of the abdomen beneath the diaphragm. It is made up of hepatic cells that extend outward from a central vein. Bile is secreted by the hepatic cells, which also perform numerous metabolic, endocrine, and secretory tasks. The liver detoxifies numerous pollutants in the plasma in addition to metabolizing proteins, lipids, and carbs. In addition, it produces plasma proteins, vital amino acids, and vitamin A, controls blood glucose levels, and secretes bile. It also converts ammonia to urea. Gallbladder 93 It is a little, pear-shaped structure that lies midway beneath the right liver lobe. The liver produces bile, which it stores and concentrates before releasing it into the common bile duct for transportation to the duodenum. Bile, a greenish liquid, emulsifies fat and aids in the absorption of fatty acids, cholesterol, and lipids through the intestinal wall. Pancreas It is visible in the horizontal abdomen, behind the stomach. Its tail rests on the spleen, while its head and neck touch the duodenal curvature. Exocrine and endocrine functions are under its control. Its exocrine function is carried out by dispersed cells, which daily produce a large number of digesting enzymes. The pancreatic duct receives secretions from clustered lobules and lobes before running through the pancreas and joining the bile duct from the gallbladder to enter the duodenum. Blood glucose levels trigger the release of the islets of Langerhans, which have an endocrine function and are made up of beta cells that secrete insulin and alpha cells that emit glucagon. III. SIGNS AND SYMPTOMS Signs and Symptoms Rationale Abnormal flatulence Flatulence occurs in gastroenteritis due to bacterial or viral overgrowth and infection which causes buildup of gas. Nausea and vomiting It is unknown why some people with gastroenteritis vomit and get nauseous, however it is hypothesized that this is because of peripheral sensations coming from the gastrointestinal system, primarily through the vagus nerve or by serotonin stimulation of the gut's 5hydroxytryptamine 3 (5HT3 receptors). 94 Diarrhea Several viral activities cause diarrhea when the GI tract becomes infected during gastroenteritis. Enterocytes, a type of gut cell, are destroyed as a result of malabsorption. The virus can also cause secretory diarrhea, which causes the loose, watery stools, and interfere with the body's ability to absorb water. Abdominal pain and cramps Inflammation and irritation of intestines occurs as well as malabsorption which causes pain. Gastroenteritis is caused by viruses and bacteria which could result in bacterial or viral tummy bugs and inflicts pain and cramps to patients. Low grade fever Inflammation and infection in the GI tract are present thus fever is an indicative sign that the body is fighting and infection. Dehydration Due to diarrhea and vomiting dehydration occurs and the body excretes a lot of water into the system out because of malabsorption and dysfunction of the GI tract. Weight loss Diarrhea and vomiting lessen the body fluid in a short time. Having gastroenteritis also leads to poor absorption of nutrients and leads to weight loss. IV. ETIOLOGY Predisposing factors Rationale Age (Young children and older Due to their underdeveloped immune systems, infants adults) and young children are more vulnerable than adults, who are vulnerable due to compromised immune 95 systems. As for older adults, their immune systems. Environment Viral, bacterial, or parasitic infections can result in infectious gastroenteritis. In each instance, the infection starts when the agent is swallowed typically through food and drink. Moreover, it can spread through tainted food, drinks and environmental factors like things we touch. Precipitating factors Rationale Rotavirus The most typical cause of viral gastroenteritis. Rotavirus is most often spread through a fecal-oral route. This is often because a child does not wash their hands properly or often enough. It can also be caused by eating or drinking contaminated food or water. The virus may live on surfaces such as doorknobs, toys, and other hard objects for a long time. Norovirus The majority of norovirus outbreaks occur when infected individuals directly contact uninfected individuals, such as by caring for them, sharing food, or using the same eating utensils. Norovirus outbreaks can also be sparked by contaminated food, water, and surfaces. Poor personal hygiene The Gastroenteritis virus can spread when people dont thoroughly wash their hands after coming into contact with feces and vomit. Moreover, it is possible to contract it by breathing vomit droplets hanging in the air. (Mayo Clinic 2023) Poor food preparation Foodborne acute gastroenteritis is linked to poor food handling practices in the home. The two most important risk factors for foodborne acute gastroenteritis are 96 inappropriate food storage and infrequent thorough heating (Mayo Clinic,2023) I. PATHOPHYSIOLOGY 97 Narrative: “Gastro” refers to the stomach, “Enter” refers to the small intestine, and “itis” refers to inflammation. So there are really two different types of gastroenteritis. There's acute gastroenteritis, and there's chronic gastroenteritis. acute gastroenteritis doesn't last very long. It's usually about a few days to a week. Chronic gastroenteritis, on the other hand, is persistent and lasts for a pretty long period of time. We're gonna mostly be talking about acute gastroenteritis. So people have acute gastroenteritis, they don't usually say you know, like, I have acute gastroenteritis, they usually say something like, you know, I have the stomach flu, or the stomach bug, or a stomach virus. So anyone who said they've had this is kind of familiar with some of the symptoms associated with it. So to look at those symptoms, why don't we actually look at the gastrointestinal tract over here? So here's the stomach, and here's the small intestine in green. So after you consume a meal, you know, you'll have some stuff in your stomach that your digestive system is really trying to digest and then absorb. But when you have gastroenteritis, your digestive tract can't do that. So now you have all this stuff that your body is going to want to expel. So how's it going to do that? Well, it can either come out this way right through your esophagus, and that's really why you experienced some vomiting and nausea. It can also come out from the other end as well, right? And that's why a lot of people may experience diarrhea. So there's a lot of nutrients and a lot of water that you've consumed, but your body isn't taking it because you're vomiting and excreting a lot of water out. You're not getting that water into your system, so you'll be pretty badly dehydrated as well. Some other symptoms could include things like abdominal pain, and a fever. And usually an acute gastroenteritis. These symptoms last for about a few days to a week. So what's causing all these symptoms? to occur? What causes gastroenteritis? We know sometimes people call it the stomach flu and I think that can be a bit misleading. The ordinary flu is caused by the influenza virus, but this virus has absolutely nothing to do with gastroenteritis. There are a number of different infectious pathogens that can cause this instead. So you may have some different viruses or some different bacteria. So a few examples, right. Some really common examples of the many different pathogens would be you know, like the rotavirus, the norovirus. So these are examples of viruses that could cause the disease. An example of a bacteria would be something called intero toxigenic E. Coli. So this is just a really fancy name for some bacteria that can cause a disease but all in all, there are a lot of other types of pathogens 98 that could cause it as well. So how do these pathogens get into your system to begin with? It's usually through fecal to oral transmission. So your feces is the stuff that gets undigested and doesn't get absorbed into your system and gets excreted as waste. That feces can contain the pathogen. So it's contaminated and oral just refers to someone's mouth. So maybe someone with gastroenteritis uses the bathroom and they wash their hands but not well enough. So their hands might actually be contaminated with some of the pathogen and they may go on to touch other objects, right surfaces and foods and water that you may touch. And then if you touch those with your hands or if you eat the contaminated food or water then you can give the pathogen very easy access to your own gastrointestinal system. So once it's in your system, what is it going to do? So going back to our diagram over here, you have this wall that really kind of extends over the entire gastrointestinal tract, you know, your stomach and your small intestine and so on and so forth. So we call this wall or this lining the gastrointestinal wall. And this is where we're going to be focusing on. So let's actually zoom in on that a bit. So here I kind of have a zoomed in picture of that. And I want to mostly focus on this green structure over here. This green structure is just the epithelium. It contains all of the cells that will be specialized for digestion and absorption. So maybe you eat some food over here, right? That's been partially digested, but in the food that you ate, maybe there was some of the pathogen. The pathogen is then going to invade the epithelium. So it's going to invade those cells and those cells are going to die off. These epithelial cells are going to kind of slough off of the lining over here. So maybe you'll have some dead epithelial cells and partially digested food that you're trying to eat. So now you don't have those epithelial cells to digest and absorb food and water. So you're going to actually have a lot of water here. And instead of going into your system, it's just going to stay here, right so now you can't digest some of the foods that may lead to some vomit II. MEDICAL MANAGEMENT A. DIAGNOSTIC EXAMS TEST RATIONALE NURSING RESPONSIBILITIES The physical examination can help Physical Examination ● Prepare the identify the cause of gastroenteritis examination room and and evaluate whether or not there is equipment. any dehydration present. Body ● Assist the patient 99 weight, blood pressure, pulse, and ready for specific temperature physical examination can all show a problem's seriousness. There can ● Provide gown, drape, be a slight temperature increase and assist in (Lin, 2019). positioning the patient as needed. ● Assist the doctor during the examination/assessm ent. There is no other Rapid stool test other quick test for gastroenteritis ● -causing the procedure to the viruses, but a rapid stool test can immediately detect rotavirus and Discuss the test and patient. ● norovirus (Mayo Clinic 2022). Provide appropriate specimen containers and instruct on how to The Stool culture & sensitivity underlying cause of properly obtain the gastroenteritis can be determined using a stool culture & sensitivity. specimen. ● The test aims to check the stool for diaper in a leak proof bacteria, viruses, or parasites. It is an indication that the culture is bag. ● positive if infection-causing bacteria develop. Chemical microscope may tests be or used discover the best medication for treating the infection (Nall, 2022). containers with to test is occasionally performed to Use gloves in collecting the a determine the type of germ. This For infants, place the specimens. ● Make sure to label the container appropriately (e.g Patient’s name, Date/time, and name procedure). 100 A sigmoidoscopy is a diagnostic Sigmoidoscopy ● procedure used to examine the lower portion of the colon or large Explain the procedure to the client. ● Provide privacy with intestine. To check for symptoms of curtains and adequate inflammatory bowel disease, the draping. doctor will insert a thin, flexible tube ● Observe the client for with a tiny camera from the anus signs of perforation, into the lower large intestine.The such as bleeding, sigmoidoscopy takes 15 minutes liver, etc. and is typically performed without ● sedation (Cleveland Clinic 2023). Make sure to label the container correctly and send the specimen to the laboratory. B. MEDS 1. Antibiotics (Bacterial Gastroenteritis) - Bacterial gastroenteritis is sometimes treated with antibiotics. Antibiotics work to cure some forms of bacterial gastroenteritis within a few days. Generally, the modes of action of antibiotics for interference with cell walls. GENERIC NAME AMPICILLIN BRAND NAME Ampicin DRUG CLASSIFICATION PHARMACOTHERAPEUTIC: aminopenicillin THERAPEUTIC: antibiotic 101 SUGGESTED DOSE For Gastrointestinal Tract Infections: PO Adult dosage — Typical dosage is 500 mg — Four times per day. Child dosage (children who weigh more than 20 kg) — Typical dosage is 500 mg — Four times per day. (children who weigh 20 kg or less) — Typical dosage is 100 mg/kg per day — Four equally divided and spaced doses IV/IM Adult dosage <40 kg: 50 mg/kg/day — divided q6-8hr ≥40 kg: 500 mg; larger doses may be necessary in severe or chronic infection — q6hr Child dosage <40 kg: 50-100 mg/kg/day — divided q6hr ≥40 kg: 500 mg — q6hr ROUTE OF PO, IV/IM ADMINISTRATION MODE OF ACTION Exerts bactericidal activity via inhibition of bacterial cell wall synthesis by binding one or more of the penicillin binding proteins (PBPs). Exerts bacterial autolytic effect by inhibition of certain PBPs related to the activation of a bacterial autolytic process. INDICATION Infections of the Genitourinary Tract: including Gonorrhea, E. coli, P. mirabilis, enterococci, Shigella, S. typhosa and other 102 Salmonella, and non penicillinase-producing N. gonorrhoeae. Infections of the Respiratory Tract: Nonpenicillinase-producing H. influenzae and staphylococci, and streptococci including streptococcus pneumoniae. Infections of the Gastrointestinal Tract: Shigella, S. typhosa and other Salmonella, E. coli, P. mirabilis, and enterococci. Meningitis: O. Meningitidis. CONTRAINDICATION ● Hypersensitivity reaction to any of the penicillins ● Diarrhea from an infection with Clostridium difficile bacteria ● SIDE EFFECTS Infectious mononucleosis. FREQUENT ● Nausea ● Vomiting ● Diarrhea ● Rash RARE ● Hairy Tongue ● Serum Sickness Reaction ● Skin Disorder ● Allergic Reaction Causing Inflammation of Blood Vessels ADVERSE EFFECTS ● Damage To The Liver And Inflammation ● Decreased Blood Platelets ● Seizures ● The Appearance Of Crystals In The Urine ● Vocal Cord Swelling ● Cardiovascular: Lethargy & hallucinations 103 ● Digestive: Glossitis, stomatitis, enterocolitis, & pseudomembranous colitis ● Liver: Moderate elevation in serum glutamic oxaloacetic transaminase (SGOT) ● Hematologic: Bone marrow depression, hemolytic anemia; positive tests for antinuclear antibody, and positive Coombs test. ● DRUG INTERACTIONS Others: Laryngeal stride and high fever DRUG: ● Probenecid with ampicillin can cause more side effects. These can include severe nausea, vomiting, and diarrhea. ● Allopurinol increases the risk of skin rash when you take it with ampicillin. ● Chloramphenicol, macrolides, sulfonamides, and tetracyclines can make penicillin less effective because these antibiotics stop the growth of bacteria, and ampicillin needs bacteria to grow in order to kill them. LAB: ● Elevate AST, ALT FOOD: ● NURSING RESPONSIBILITIES Decreased effect with acidic or juice Baseline Assessment ● Obtain patient’s health and allergic history. ● Monitor vitals signs. Intervention/Evaluation 104 ● Requests for laboratory tests such as rapid stool tests as ordered by the physician. ● Check IV site carefully for signs of thrombosis or drug reaction. ● Do not give IM injections in the same site; atrophy can occur. Monitor injection sites. ● Administer oral drug on an empty stomach should be 1 hr before or 2 hr after meals with a full glass of water; do not give with fruit juice or soft drinks. Patient/Family Teaching ● The patient must take the drug at the appropriate time. ● The patient should also take the full course of therapy; do not stop taking the drug if you feel better. ● Explain to patient/s that they might experience these side effects: Nausea, vomiting, GI upset (eat frequent small meals), diarrhea. ● Discuss to the patient to immediately report pain or discomfort at sites, unusual bleeding or bruising, mouth sores, rash, hives, fever, itching, severe diarrhea, difficulty breathing. 2. Antidiarrheal agents (Viral Gastroenteritis) - Antidiarrheals work by reducing the flow of fluids and electrolytes into the bowel and slowing down the movement of the bowel to decrease the number of bowel movements. This allows more fluid to be absorbed into your body, which helps with less diarrhea and more formed and bulky stools. GENERIC NAME LOPERAMIDE 105 BRAND NAME Imodium DRUG CLASSIFICATION PHARMACOTHERAPEUTIC: Adsorbents CLINICAL: Antidiarrheal agents SUGGESTED DOSE For the treatment of Acute Diarrhea: Oral administration (Capsule) ● Adults and children 13 years of age and older - At first, 4 milligrams (mg) (2 capsules) after the first loose bowel movement, then 2 mg (1 capsule) after each loose bowel movement after the first dose has been taken. However, dose is usually not more than 16 mg (8 capsules). ● Children 8 to 12 years of age weighing more than 30 kilograms (kg) - 2 mg (1 capsule) 3 times a day. ● Children 6 to 8 years of age weighing 20 to 30 kg - 2 mg (1 capsule) 2 times a day. Oral administration (Oral solution) ● Children 8 to 12 years of age weighing more than 30 kilograms (kg) - 2 teaspoonfuls (2 mg) 3 times a day ● Children 6 to 8 years of age weighing 20 to 30 kg - 2 teaspoonfuls (2 mg) 3 times a day. ● Children 2 to 5 years of age weighing 13 to 20 kg - 1 teaspoonful (1 mg) 3 times a day. 106 For the treatment Chronic Diarrhea: Oral administration ● Adults - At first, 4 milligrams (mg) (2 capsules) after the first loose bowel movement, then 2 mg (1 capsule) after each loose bowel movement after the first dose has been taken. Doctor may adjust your dose as needed. ROUTE ● Children 2 years of age and older - Use and dose must be determined by the doctor. OF PO ADMINISTRATION MODE OF ACTION It acts by slowing intestinal motility and by affecting water and electrolyte movement through the bowel. Loperamide binds to the opiate receptor in the gut wall. INDICATION CONTRAINDICATION People with: ● Chronic diarrhea in Adults ● Infectious diarrhea in Adults ● Bacterial Gastroenteritis ● Irritable Bowel Syndrome ● known hypersensitivity to loperamide hydrochloride or to any of the excipients ● torsades de pointes, a type of abnormal heart rhythm. ● prolonged QT interval on EKG. ● abnormal EKG with QT changes from birth. ● paralysis of the intestines. ● liver problems. ● bloody diarrhea. 107 SIDE EFFECTS ADVERSE EFFECTS DRUG INTERACTIONS ● Dizziness ● Drowsiness ● Tiredness ● Constipation ● stomach pain ● skin rash ● itching ● severe constipation ● severe nausea ● severe vomiting ● stomach or abdominal pain ● uncomfortable fullness of the stomach or abdomen ● Pramlintide ● recent/current antibiotic use ● drugs that can cause constipation ○ Anticholinergics ■ ○ Antispasmodics ■ ○ RESPONSIBILITIES Diphenhydramine tricyclic antidepressants ■ NURSING Morphine certain antihistamines ■ ○ glycopyrrolate/oxybutynin potent opioid pain medicines ■ ○ belladonna/scopolamine Amitriptyline Baseline assessment ● Assess the type and severity of the Diarrhea ● Assess for presence of pain in the abdomen area ● Assess patient allergies 108 ● Review past medical history Intervention/evaluation ● Monitor pulse, B/P, VS ● Assist patient in a comfortable position ● Administer oxygen if prescribed by physician ● Assess for clinical improvement Patient/family teaching ● Inform patient about the likelihood of side effects like dizziness, drowsiness, tiredness, constipation, stomach pain, skin rash, or skin itching ● Acquire adequate rest ● Acquire adequate nutrition ● Avoid tasks requiring exertion. ● Report any presence of severe constipation, severe nausea, severe vomiting, stomach or abdominal pain, or uncomfortable fullness of the stomach or abdomen. 3. Antiemetics - Antiemetics are medications aimed at preventing or treating nausea and vomiting, which are common symptoms that may be linked to numerous causes. GENERIC NAME BRAND NAME ONDANSETRON Zofran 109 DRUG CLASSIFICATION SUGGESTED DOSE Selective 5-HT3 Antagonist ● Injectable Solution ○ ● ● Tablet ○ 4mg ○ 8mg ○ 24mg Oral Solution ○ ● ● ROUTE 2mg/mL 4mg/5mL Oral Soluble Film ○ 4mg ○ 8mg Orally Disintegrating Tablets ○ 4mg ○ 8mg OF PO, IV ADMINISTRATION MODE OF ACTION It works by blocking the action of serotonin, a natural substance that may cause nausea and vomiting. INDICATION Used to prevent nausea and vomiting caused by cancer chemotherapy, radiation therapy, and surgery. Recently, ondansetron has been used to control vomiting related to acute gastroenteritis. CONTRAINDICATION ● Contraindicated to those known to have hypersensitivity (e.g., anaphylaxis) to ondansetron or any of the components of the formulation SIDE EFFECTS More common ● Confusion 110 ● dizziness/drowsiness ● fast heartbeat ● fever ● headache ● trouble breathing ADVERSE EFFECTS ● General: rare cases of hypersensitivity reactions, sometimes severe (acute allergic reactions, rapid swelling, difficulty breathing, cardiopulmonary arrest, low blood pressure, laryngeal edema) ● Local reactions: pain, redness, and burning at the injection site ● Lower respiratory: hiccups ● Neurological: involuntary intermittent or sustained deviation of the eyes ● Cardiac: heart rate irregularities, palpitations, fainting ● Skin and subcutaneous tissue: hives, Stevens-Johnson syndrome, toxic epidermal necrolysis DRUG INTERACTIONS DRUG: ● Selective serotonin reuptake inhibitors (SSRIs): causes a possible interaction with SSRIs. Taking it with an SSRI can raise the risk of a condition called serotonin syndrome. ● Certain antibiotics (Fluoroquinolones, Macrolides): Taking them with ondansetron can cause a higher chance of an irregular heartbeat. ● Heart rhythm medications (Quinidine, Amiodarone, Sotalol): Combining these medications with ondansetron raises chances of having heart rhythm problems. NURSING RESPONSIBILITIES Baseline Assessment ● Obtain patient’s health and allergic history. 111 ● Monitor vitals signs. Intervention/Evaluation ● Monitor improvements in GI symptoms (decreased nausea and vomiting, increased appetite) to help document whether drug therapy is successful. ● Assess dizziness and drowsiness that might affect gait, balance, and other functional activities Patient/Family Teaching ● Instruct patient to report bothersome side effects such as severe or prolonged headache, weakness, fatigue, or GI problems. ● Explain to patient that the drug can be taken with or without food. ● Emphasize the importance of following the doctor's dosing instructions very carefully. C. TREATMENT THERAPY RATIONALE NURSING RESPONSIBILITIES A type of fluid replacement Oral rehydration therapy ● Assess the severity of utilized to prevent and treat the dehydration of the dehydration, primarily due to patient. diarrhea. It involves consuming ● Explain to the water with small salts, mainly patient/family the steps sodium, potassium, and sugar. in preparing ORS. A nasogastric tube can also be used to rehydration ● Monitor the patient administer oral regularly to check if treatment. Oral treatment is effective. rehydration therapy is equally effective as intravenous therapy 112 (Rehydreate.org 2019). IV therapy IV fluids are specially prepared ● Assess the IV site every liquids that are injected into a 1 to 2 hours or more vein frequently if required. to prevent or treat dehydration. They are used in ● people of all ages who are unwell, injured, or dehydrated. Calculate and ensure designated flow rate. ● Monitor for any signs of Intravenous rehydration is a unusualities simple, phlebitis or infiltration. safe and standard procedure with a low risk of ● complications (Cleveland Clinic as Document actions and observations. ● 2021). such Immediately report any significant unusualities. Maintain good personal hygiene One of the best defenses Health Teachings against gastrointestinal or ● infectious diseases is good personal hygiene since it ward Establish rapport to the patient and family. ● Explain the importance off bacteria to prevent infections of (HealthDirect 2021). personal hygiene. ● Maintain clean & safe Keeping the environment clean environment is crucial to being healthy. Many through good personal hygiene and keeping the environment clean (Taylor the to safe environment. Such as; disinfecting & proper ones that cause diarrhea and prevented Instruct maintain a clean and dirty environments, such as the that many diseases can be good patient/family disease-causing germs live in other infections. This implies maintaining waste management. ● Encourage patient/family the to only consume foods that do not worsen symptoms. Such as bland, easy-to- 2020). 113 Avoid specific foods or Avoid foods that can trigger and digest foods; crackers, substances worsen symptoms such as full- toast, gelatin, bananas, fat dairy products, such as and applesauce. whole milk and ice cream, and sugary foods, such as sodas and candy. Instead, consume foods or drinks with potassium, such as fruit juice and bananas (Mayo Clinic 2021). III. SURGICAL MANAGEMENT No surgical management is available for gastroenteritis. IV. NURSING MANAGEMENT NURSING DIAGNOSIS Acute Pain related GOAL to After 1 hour INTERVENTION of nursing 1. Perform a Inflammation of the lining in intervention, the patient will be comprehensive the stomach and intestines as able assessment to report decreased evidenced by cramps and abdominal pain of 1/10 and R: Identifying the location, abdominal discomfort improve comfort. intensity, frequency, characteristics pain is Rationale: critical Inflammation of the stomach, underlying small, and large intestines is abdominal referred to as gastroenteritis. effectiveness of the current Viral treatment regimen. gastroenteritis infection that can is an in of and determining the cause of pain and the induce vomiting or diarrhea and is 2. Review and assess brought on by a number of diagnostic studies. different viruses. Abdominal R: Ultrasounds, abdominal x- cramps, rays, and CT scans may be diarrhea, and 114 vomiting are symptoms. just The immune system inflammation by a few body's reacts performed to help diagnose the underlying condition. to releasing 3. Provide cytokines and prostaglandins, which increase vascular medications as ordered. R: Analgesics and sedatives permeability and create pain are provided in the patient's abdomen. management for pain and relief. Medications to relieve gas, nausea, constipation, and diarrhea may also relieve pain. 4. Assist to a position of comfort. R: Abdominal pain may be relieved with position a that specific promotes comfort. A knee-to-chest or side-lying position tends to decrease the intensity of abdominal pain. Raising the head of the bed may also relieve symptoms. 5. Provide nonpharmacologic pain management. R: Nonpharmacologic methods in pain management may include physical, cognitive-behavioral strategies. 115 6. Insert nasogastric (NG) tube. R: With specific diagnoses such as bowel obstruction, bowel rest, and the insertion of an NG tube is required to decompress the stomach. 7. Assist in surgical intervention. R: Depending underlying on cause, the surgery may be indicated in patients with abdominal pain. Assist and prepare the patient for surgery as ordered. Imbalanced Than Nutrition: Body Less After 2 days of nursing 1. Establish rapport Requirements intervention, the patient will be R: To gain cooperation and related to inadequate food able to consume adequate create intake as evidenced by nutrition, nausea and vomiting and a harmonious identify relationship with the patient. appropriate nutritional needs. 2. Measure client weight. Rationale: Vomiting symptoms disease R: This will accurately monitor is one of a of the response to therapy. common known gastroenteritis. the Usually, as 3. Monitor and record the a number of vomiting, bacterial or viral stomach virus amount, is the cause. Although it frequency. and affects people of all ages, 116 young children susceptible. Cumpian, most R: These data will help in According to initiating nursing actions and (2021), a subsequent treatment. T. are balanced diet is essential for a person's health and well- being. Imbalanced Nutrition 4. Monitor the client’s food intake. refers to food that is either too R: To determine the amount of much or too little for the body's food that is consumed. needs which any person can experience. 5. Encourage small, frequent feedings. R: Consistently offering the patient something to eat can improve their total caloric intake. This can also prevent dehydration, weight loss, and constipation. 6. Provide a diverse diet according to his needs. R: This will stimulate the appetite of the client. 7. Provide parenteral fluids, as ordered. R: To ensure adequate fluid and electrolyte levels. 8. Refer to a dietitian if indicated. 117 R: Collaboration with the dietician in order to guide the client about proper nutrition. Diarrhea related to bacterial After 8 hours of nursing 1. Inquire about the infection as evidenced by intervention, the patient will be patient's watery stool more than 3 times able to release soft, formed history: If the patient a day consumes stool not more than 3 times. recent untreated water. If the patient Rationale: consumes According to Cleveland Clinic undercooked (2020), diarrhea is the primary The last time when the sign of gastroenteritis. Multiple patient consumed raw viral activities cause diarrhea dairy products. food. when the GI tract becomes R: Consumption infected during gastroenteritis. contaminated foods or water Enterocytes, which are gut may expose the patient to cells, are destroyed when intestinal there is malabsorption. The intervention virus can also cause secretory doctor diarrhea, which causes loose, cause of intestinal infection. watery stools, and interfere Thus, he will be able to treat with the body's ability to the absorb water. appropriately. infection. will know patient's help the of This the possible condition 2. Examine the patient's feces pattern. R: If the doctor is knowledgeable of the patient's feces pattern, he will be able to prescribe appropriate treatment immediately. 118 3. Examine the patient for abdominal discomfort, cramps, hyperactive bowel movements, recurrence, urgency, and watery stool. R: These assessment findings are frequently associated with diarrhea. When gastroenteritis affects the large intestine, the colon cannot absorb water, resulting in excessively watery feces. 4. Submit the patient's stool of the patient for culture. R: A culture is a test that determines microorganisms which trigger an infection. 5. Teach the patient the necessity of cleaning their hands after every bowel movement and before cooking meals for others R: Contaminated hands can rapidly microorganisms to spread utensils 119 and surfaces used in food preparation. This hand washing after each bowel movement is the most effective strategy to avoid infection transmission to others. 6. After each movement, the bowel educate patient about perianal hygiene. R: The anal area should be thoroughly cleaned to avoid skin irritation and microorganism dissemination after a bowel movement. 7. Advise the patient to drink 1.5 to 2.5 liters of liquids per 24 hours, adding 200 ml every watery for stool, otherwise contraindicated. R: Fluid lost in liquid stools is replaced by increasing fluid intake. 8. Advise the patient to limit his or her consumption of coffee, 120 milk, and dairy products. R: These foods can upset the stomach lining and so aggravate diarrhea. 9. Encourage patients to consume potassium- rich meals. R: When a experiences patient persistent diarrhea, the potassium-rich stomach contents are flushed out of the gastrointestinal system into the feces and out of the body, leading to hypokalemia. 10. Advise the patient to take antidiarrheal drugs as directed by the health care provider. R: Adsorbent antidiarrheals are often used to manage gastroenteritis diarrhea. This class of antidiarrheal medications coats the gut membrane and absorbs bacterial toxins. V. LITERATURE Acute Infectious Gastroenteritis in Infancy and Childhood 121 Posovszky, C., Buderus, S., Claßen, M., Lawrenz, B., Keller, K. M., & Koletzko, S. (2020b). Acute Infectious Gastroenteritis in Infancy and Childhood. Deutsches Ärzteblatt International. https://doi.org/10.3238/arztebl.2020.0615 According to Posovszky et al. (2020), acute infectious gastroenteritis is the second most common non-traumatic cause of emergency hospitalization in children aged 1 to 5 years, accounting for about 9% of cases, despite the introduction of the rotavirus vaccine and the fact that it is frequently treated on an outpatient basis (39,410 cases in 2017% of adenovirus). Globally, acute infectious gastroenteritis causes the deaths of close to 500,000 children under the age of five every year. Infants and toddlers are sick one to two times a year on average in Europe. Five children died out of the over 40 000 children under five who were hospitalized in Germany in 2017 for acute infectious gastroenteritis, which represented about 9% of all hospitalizations for illnesses other than trauma in this age range. In hospitalized children under the age of 5, viral infections accounted for 93% of cases, with rotavirus accounting for 47%, norovirus for 29%, and adenovirus for 14%. Due to their high daily fluid requirements of 100 to 160 mL per kilogram of body weight, infants and toddlers are particularly vulnerable. The result of the study shows that weight loss and other clinical observations can be used to determine the degree of dehydration. Oral rehydration with oral rehydration solution was just as effective as intravenous rehydration with regard to weight gain, the length of diarrhea, and fluid administration, and was linked to shorter hospital stays in 17 randomized controlled trials on a total of 1811 kids with mild or moderate dehydration. Continuous nasogastric administration is the first line of treatment for children who are vomiting or who reject oral rehydration solutions given that it is equally as effective as intravenous rehydration. To conclude, despite the fact that ambulatory oral rehydration is strongly supported by the available research, children in Germany who are mildly or moderately dehydrated are frequently hospitalized for intravenous rehydration therapy. Reducing unnecessary hospitalizations and consequently lowering the risk of nosocomial infection requires overcoming barriers to intersectoral care, a staffing shortage, and inadequate access. Antiemetics in Children with Acute Gastroenteritis Niño-Serna, L. F., Acosta-Reyes, J., Veroniki, A. A., & Florez, I. D. (2020). Antiemetics in Children With Acute Gastroenteritis: A Meta-analysis. Pediatrics, 145(4). https://doi.org/10.1542/peds.2019-3260 122 Fedorowicz et al., who first compiled the data on antiemetics for acute DG. In this study, ondansetron showed a significant impact on the requirement for intravenous rehydration and the cessation of vomiting. Dimenhydrinate showed a favorable effect on the length of vomiting; however, metoclopramide was found to be effective in reducing vomiting bouts and hospital admissions. However, the authors only included seven trials and did not compare antiemetics between them. In a later network meta-analysis (NMA), Carter et al. included all antiemetics for which there was data at the time. The best strategy, according to the authors, was ondansetron, which also decreased hospitalizations, the requirement for intravenous rehydration, and vomiting. Ondansetron was linked to an increase in diarrhea; therefore, this prompted some questions. Numerous RCTs comparing various antiemetics to a placebo or to one another have been published in the past ten years but have not yet been synthesized. New data have been made public specifically from trials looking at ondansetron, metoclopramide, domperidone, and dexamethasone. There is presently no systematic review or NMA comparing all the antiemetics currently on the market for children with ADG. In order to compare antiemetics, directly and indirectly, using an NMA, we sought to evaluate their relative efficacy and safety in children with ADG. The result of the study shows that, in comparison to the placebo, ondansetron showed the most improvement in the prevention of vomiting. The only treatment that decreased the frequency of vomiting episodes and the requirement for intravenous rehydration was ondansetron. Dimenhydrinate was the only treatment worse than placebo in terms of side effects. CROHN’S DISEASE I. DEFINITION In 1932, Crohn, Ginzburg, and Oppenheimer presented a case series at the annual meeting of the American Medical Association that was the first to identify Crohn's Disease (CD), a chronic inflammatory bowel disease, as regional ileitis. (Petagna et al., 2020). It has a progressive and destructive course, is characterized by chronic inflammation of any part of the gastrointestinal tract, and is becoming more common worldwide. The deregulation of the immune system, changed bacteria, genetic vulnerability, and environmental variables are some factors of Crohn's disease. Still, the cause of the disease remains unknown. (Roda et al., 2020). Although less invasive biomarkers are in development, diagnosis still relies on endoscopy and histological assessment of biopsy specimens. II. ANATOMY/ PHYSIOLOGY Mouth 123 This oval-shaped opening in your skull starts at your lips and ends at your throat. The two main functions of the mouth are eating and speaking. Parts of the mouth include the lips, vestibule, mouth cavity, gums, teeth, hard and soft palate, tongue and salivary glands. Esophagus The primary function of the esophagus is to transport food entering the mouth through the throat and into the stomach. This function begins at the very beginning of the esophagus, following some taste buds located on the organ, at the upper esophageal sphincter (UES). Once you begin swallowing, the process becomes automatic. Your brain signals the muscles of the esophagus and peristalsis begins. Stomach After food enters your stomach, the stomach muscles mix the food and liquid with digestive juices. The stomach slowly empties its contents, called chyme, into your small intestine. The stomach serves as a temporary receptacle for storage and mechanical distribution of food before it is passed into the intestine. Large Intestine Any part of the digestive tract from the mouth to the anus can be involved in Crohn's disease, although it most commonly affects the end of the small intestine called the terminal ileum and the beginning of the large intestine called the cecum. The main function of cecum is to absorb fluids and salts that remain after completion of intestinal digestion and absorption and to mix its contents with a lubricating substance, mucus. The internal wall of the cecum is composed of a thick mucous membrane, through which water and salts are absorbed. According to expanding knowledge on the role of cecum, it is an essential organ for maintaining a diverse and physiologically beneficial microbiota in the colon. 124 Any undigested material moves to the large intestine. The large intestine or colon has four sections called the 1) cecum/ascending colon, 2) transverse colon, 3) descending colon/sigmoid, and 4) rectum. The main job of the large intestine is to remove water and salts (electrolytes) from the undigested material and to form solid waste (feces) that can be excreted. The remaining contents of the large intestine move to the rectum, where feces are stored until they leave the body through the anus as a bowel movement. III. SIGNS AND SYMPTOMS SIGNS & SYMPTOMS RATIONALE Bloating According to Chron's and Colitis Canada, 2019, As food is absorbed poorly by small intestines, more undigested food reaches the colon, in that the bacteria in the colon can digest it but, in turn, produces more gas, thus causing bloating. Constipation Crohn's disease can cause a section of the intestines to narrow due to severe inflammation. This section is called a stricture, which can block or slow the passage of stool or digested food through the bowels, leading to constipation. (Stuart, 2019) Fever A fever sometimes develops when the intestine becomes inflamed. There may also be an infection with Crohn's, or medications can cause agitation to help treat the disease. (Temple Health Org, 2023) Weight Loss The upset stomach and stress that come with an episode of Crohn's can make it difficult, or even unappealing, to eat, causing weight loss or loss of appetite. (Temple Health Org, 2023) Pain or bleeding with a bowel Crohn's can lead to tears (fissures) in the lining of the anus, movement which may cause pain and bleeding, especially during bowel movements, as well as infection. (Creaky Joints Org, 2020) 125 Mouth Sores The digestive system becomes damaged for people with Crohn's and can't properly absorb vitamins and minerals. Those deficiencies, paired with inflammation, can result in canker sores in the mouth. (Creaky Joints Org, 2020) IV. ETIOLOGY Predisposing factors Rationale Age While Crohn's disease can affect people of all ages, it’s primarily an illness of the young. Most people are diagnosed before age 30, but the disease can happen in people in their 50s, 60s, 70s, or even later in life (WebMD, 2022). Ethnicity Although Crohn's disease can affect any ethnic group, whites have the highest risk, especially people of Eastern European (Ashkenazi) Jewish descent. However, the incidence of Crohn's disease is increasing among Black people who live in North America and the United Kingdom. Crohn's disease is also being increasingly seen in the Middle Eastern population and among migrants to the United States (Mayo Clinic, 2020). Family history Although the condition is not hereditary, it appears to run in some families, as it is present in more than one family in roughly 15% of cases. You're at higher risk if you have a firstdegree relative, such as a parent, sibling or child, with the disease. As many as 1 in 5 people with Crohn's disease has a family member with the disease (Mayo Clinic, 2020). 126 Sex Women are more likely than men to have Crohn's disease, but men are more likely to develop ulcerative colitis. Crohn's disease is 1.1-1.8 times more common in women than in men (Ehrlich, 2021). Precipitating factors Rationale Cigarette Smoking Smoking can raise your risk of developing Crohn's disease and make the condition worse and more difficult to cure. Smokers experience more severe Crohn's symptoms as well as more relapses. Individuals with Crohn's who smoke may experience the following: Severer symptoms and consequences, such as strictures, which are narrowings in the intestine that can result in hazardous blockages (Watson, 2022). Nonsteroidal Anti- The American College of Gastroenterology recommends that Inflammatory Drug people with Crohn's avoid NSAIDs when possible because they could cause symptom flare-ups as well as stomach or intestinal ulcers. Using NSAIDs raises your risk of an emergency hospital admission for your Crohn's (Winsborough, 2022). High Fat Diet A high fat diet may lead to specific changes in gut bacteria that could fight harmful inflammation. Diets high in animal fats are associated with increased risks of inflammatory bowel disease, but the mechanism remains unclear (Li et al., 2019). Use of Oral Contraceptives Research has shown that combination birth control pills aren’t kind to your gut. They could raise your risk of Crohn’s disease by 24% to 50%, especially if you have certain genes. And people with Crohn’s who use the pill are more likely to have severe symptoms and need surgery for their disease (Rath, 2022). 127 V. PATHOPHYSIOLOGY 128 129 130 Narrative: Crohn’s disease is an inflammatory bowel disease that causes inflammation and ulcer formation in the GI tract. Although the disease can be found anywhere in the GI tract, from the mouth to the anus, it is most commonly found in the terminal ileum and the beginning of the colon in a skip lesion pattern or scattered patches. The mechanism behind the skipping pattern of lesions is still unclear however, this is a distinguishing characteristic of Crohn’s disease to Ulcerative colitis. The etiology of the disease is still unknown and the mechanism of IBD is not fully understood yet, all that is known is that it is caused by a faulty immune system. However, there are several factors that contribute to the progression of the disease, including age, ethnicity, family history and sex. On the other hand, there are also precipitating factors that affect the disease including cigarette smoking, NSAIDs, high fat diet, and the use of oral contraceptives. These factors have the potential to either impaired barrier function or activate m-cells, which is the main pathway for starting the production of mucosal immunoglobulin A (IgA), the one that protects mucosal tissues against microbial invasion and commensal enteric bacteria. As a result of the m-cells' function, antigens from the lumen are delivered to the mucosal tissues, where they trigger the activation of immune cells. Once activated, the creation of immunoglobulins by activated B cells allows them to pass through the bloodstream, penetrate other body fluids, and bind specifically to the foreign antigen that initially induced their formation. Once the antigen binds 131 to the receptor, it causes the release of inflammatory mediators. The antigen-presenting cell, which is the macrophage, will process these antigens and present them to the CD4 T cells. After that, the CD4 T-cell is activated, which may result in one of two outcomes. First, the adjacent macrophages are stimulated and further activated by the CD4 T cell, and second, both the CD4 and the macrophages start releasing a lot of cytokines, such as TNF alpha and interleukin 1 & 6. The ongoing release of these cytokines may result in chronic inflammation. It is the production of cytokines and chronic inflammation that produces the local and systemic problems associated with inflammatory bowel disease. After the chronic inflammation, the GI tract lining will experience transmural systemic inflammation, which means that the entire intestinal layer—from the mucosa to the serosa—has already suffered damage. This could occur across the entire GI tract from the mouth to the anus in random patches, but it only occurs frequently in the terminal region of the ileum up to the cecum, and that is what we now refer to as Crohn's disease. Furthermore, a person with Crohn's disease may experience periods of remission and flare-ups, which may also be brought on by certain food, lifestyle, and environmental variables. When the GI tract's blood vessels become more permeable throughout this time of remissions and flare-ups, more fluid may seep into the GI tract and result in severe intestinal damage. On the other hand, persistent inflammation prevents healing, which led to the deposition of an extracellular matrix to support preserving the body's equilibrium. However, an excessive extracellular matrix along with the fluids that had leaked within the GI tract can cause tissue scarring which will lead to a stricture – a narrowing of GI lumen that can cause bowel obstruction. Crohn’s disease damages mucosal epithelial cells thus leading to apoptosis and ulceration within the affected area. This event could cause prolonged bleeding which can lead to complications like anemia, disappearing transport proteins because of the programmed cell death and can lead to inability of the lumen to absorb sodium and water causing diarrheal problems, and microperforations through the intestinal wall because of the ulcerations. The initial problem that had occurred because of the stricture and these microperforations could predispose abscess formation – a swollen area containing pus that might actually leak. When abscesses are drained, a passage may remain between the anal gland and the skin, resulting in a fistula. Since Crohn’s disease affects the entirety of the GI tract, it can also cause damage within the small intestine and could lead to the scarring of the intestinal villi within the area which could actually lead to bloating or worse, weight loss. When left untreated, all of these conditions could result in organ sepsis, colon cancer, severe joint, skin, eye, mouth, and liver problems, as well as subsequent complications that could result in death and a poor prognosis. Crohn's disease doesn't have a cure however, when 132 managed with specific medications and surgical care, combined with some adjustments in lifestyle and diet it could lead to a good prognosis. VI. MEDICAL MANAGEMENT A. DIAGNOSTIC EXAMS TEST Blood Tests RATIONALE NURSING RESPONSIBILITIES The main characteristic of Crohn's Before the procedure: disease and ulcerative colitis is ● Explain the test procedure. inflammation in the gastrointestinal About what type of sample tract. White blood cells are attracted is needed, how it will be to sites of inflammation. These tests collected, check equipment to use. for signs of infection, inflammation, internal bleeding, and ● and what Explain that low levels of substances such as discomfort may iron, protein, or minerals. when the skin is punctured. ● slight be felt Apply manual pressure and dressings puncture over site the after the blood is drawn. After the procedure: ● Monitor the puncture site for oozing or hematoma formation. ● Instruct to resume normal activities and diet. Stool Culture Blood in your stool is a sign of Before the procedure: digestive problems, such as ● Assess the patient’s level of Crohn's disease. They may also comfort. Collecting stool order stool tests to check for specimens may produce a disease-causing organisms in your feeling of embarrassment digestive tract. This can help them and rule out other possible causes of patient. discomfort to 133 the your symptoms. ● Encourage the patient to urinate. Allow the patient to urinate before collecting to avoid contaminating the stool with urine. ● Avoid laxatives. Advise the patient that laxatives, enemas, or suppositories are avoided three days prior to collection. ● Inform the client how many stool specimens required and are a supply specimen container. After the procedure: ● Label the container ● Promptly send the specimen to the laboratory for analysis. ● Instruct the patient to do handwashing. Allow the patient to thoroughly clean his or her hands and perianal area. ● Resume activities. The patient may resume his or her normal diet and medication therapy unless otherwise specified. Magnetic resonance imaging (MRI) An MRI scanner uses a magnetic Before the procedure: field and radio waves to create ● Explain to the patient the 134 detailed images of organs and purpose of the test. Tell him tissues. MRI is particularly useful for who will perform the test evaluating a fistula around the anal and where it will take place. area (pelvic MRI) or the small ● Inform the patient that he’ll intestine (MR enterography). Sometimes an MR enterography can be performed to check for disease status or progression. This need to lie flat on a narrow bed, which slides into a large cylinder that houses the MRI magnets. test may be used instead of CT ● Advise the patient to avoid enterography to reduce the risk of alcohol, caffeine-containing radiation, especially in younger beverages, and smoking people. for at least 2 hours and food for at least 1 hour before the test. Explain to the patient that he can continue taking medications, except for iron, which interferes with the imaging. ● Advise the patient that he’ll have to remain still for the entire procedure. ● Instruct the patient to remove all metallic objects, including jewelry, hairpins, and watches. ● Make sure that the patient or a responsible family member has signed an informed consent form. ● Administer the prescribed sedative if ordered. After the procedure: 135 ● Tell the patient that he may resume his usual activities as ordered. ● Provide comfort measures and pain medication as needed and because of ordered prolonged positioning the scanner. ● Monitor the patient for the adverse reaction to the contrast medium (flushing, nausea, urticaria, and sneezing) CT Scan A special X-ray technique that Before the procedure: provides more detail than a ● Take off some or all of the standard X-ray does. This test looks clothing at the entire bowel as well as at hospital gown. ● tissues outside the bowel. and getting intravenous contrast images of the a Remove any metal objects, which might interfere with scan that involves drinking an oral material wear such as a belt or jewelry, CT enterography is a special CT contrast and image results. ● Stop eating for a few hours before the scan. If a patient intestines. This test provides better is going to have a contrast images of the small bowel and has injection, he or she should replaced barium X-rays in many not have anything to eat or medical centers. drink for a few hours before CT the scan because the injection may cause stomach upset. ● To receive the contrast injection, an IV is inserted 136 into the arm just prior to the scan. The contrast then enters the body through the IV. ● Prior to most CT scans of the abdomen and pelvis, it is important to drink an oral contrast agent that contains dilute barium. This contrast agent helps the radiologist identify gastrointestinal the tract (stomach, small and large bowel), detect abnormalities of these organs, and to separate these structures from other structures within the abdomen. ● If the patient has a history of allergy to contrast material (such as iodine), the requesting physician and radiology staff should be notified. ● The patient will be asked to drink slightly less than a quart spread out over 1.5 to 2 hours. After the procedure: ● After the exam, patients can return to their normal routine. 137 ● If a patient were given a contrast material, the patient may receive special instructions. In some cases, patients may be asked to wait for a short time before leaving to ensure that they feel well after the exam. After the scan, patients are likely to be told to drink lots of fluids to help remove their kidneys the contrast material from the body. Capsule Endoscopy For this test, you swallow a capsule Before the procedure: that has a camera in it. The camera takes pictures of your ● small the prescribed liquid diet at intestine and sends them to a recorder you wear on your belt. The Instruct the patient to start 12:00 Noon. ● images are then downloaded to a Administer the two packets of Klean-Prep starting at computer, displayed on a monitor 6:00 PM the evening prior and checked for signs of Crohn's to disease. The camera exits your the scheduled procedure. Dissolve each body painlessly in your stool. packet in one liter of water. ● Do not take any medication two hours before having the exam. ● Do not apply body lotion or powder to your abdomen. ● Wear loose-fitting, two- piece clothing. Your upper 138 clothing should be opaque. After the procedure: ● You may drink colorless liquids starting two hours after swallowing the capsule. ● You may have a light snack four hours after ingestion. After the examination is completed, you may return to your normal diet. ● Use the provided Capsule Endoscopy Event Form, to note the time of any event such as eating, drinking or a change in your activity. Return the Event Form completed to your physician at the time you return the equipment. ● Avoid strong electromagnetic fields such as MRI devices or ham radios after swallowing the capsule and until you pass it in a bowel movement. ● Do not disconnect the equipment or completely remove the recorder at any time during the procedure. ● Avoid sudden movements and banging of 139 the recorder. ● Avoid direct exposure to bright sunlight. Balloon-assisted For this test, a scope is used along enteroscopy with a device called an overtube. Before the procedure: This enables the doctor to look ● Secure the consent form further into the small bowel where ● Provide information about the procedure. standard endoscopes don't reach. This technique is useful when capsule endoscopy ● Instruct patient to wear loose comfortable clothing shows abnormalities but the diagnosis is and leave valuables still in question. including jewelry at home. Avoid using nail polish. ● Check the vital signs and review the medical history and medication list. An IV line will be started in a vein in the patient’s arm for IV fluids and sedation medication. After the procedure: ● Call for a family member to converse with the Doctor to discuss the procedure. ● Do not drive, operate heavy machinery, or drink alcohol for 24 hours after the procedure. Patient should go home and rest after the procedure. ● Instruct to eat something light since they have not 140 eaten for over 8 hours. Avoid fried foods, fatty foods and large quantities of food. Things such as: scrambled eggs, toast, and a sandwich are good choices. Colonoscopy This test allows your doctor to view Before the procedure: your entire colon and the very end ● Secure informed consent. of your ileum (terminal ileum) using ● Obtain a medical history of a thin, flexible, lighted tube with a the camera at the end. During the allergies, procedure, your doctor can also histories, medications, and take information relevant to the small samples of tissue (biopsy) for laboratory analysis, which may help to make a such as bleeding, current complaint. ● diagnosis. Clusters of inflammatory cells called granulomas may help patient Provide information about the procedure. ● suggest a diagnosis of Crohn's. Ensure that the patient has complied with the bowel preparation. He/she must have maintained a clear liquid diet for 24-48 hours before the test, NPO after midnight, and taken a laxative, as ordered. ● Inform the patient that an IV line will be started and a sedative will be administered before the procedure. Also, advise the patient to have someone drive him/her home after 141 the procedure since sedatives will be given. ● Instruct the patient to empty the bladder prior to the procedure. ● Instruct the patient to remove all metallic objects from the area to be patient to examined. After the procedure: ● Instruct the resume a normal diet, unless otherwise directed by the doctor. ● Inform the patient to refrain from driving or operating heavy machinery. ● Instruct patient to take any pain medications or stool softeners that have been prescribed by the doctor. ● Encourage the patient to drink plenty of liquids. ● Inform the patient to avoid consuming alcohol. ● Provide privacy while the patient rest after the procedure. ● Monitor unusualities such as rectal bleeding. B. MEDS 142 1. Aminosalicylates - These medicines contain 5-aminosalicylic acid (5-ASA), which helps control inflammation. Doctors use aminosalicylates to treat people newly diagnosed with Crohn’s disease who have mild symptoms. Aminosalicylates include GENERIC NAME Sulfasalazine BRAND NAME Azulfidine, , Azulfidine EN-tabs, Salazopyrin DRUG CLASSIFICATION PHARMACOTHERAPEUTIC:5-Ami-nosalicylic acid derivative. CLINICAL: Anti-inflammatory. SUGGESTED DOSE ROUTE 3-6 g/day PO in divided doses for up to 16 wks OF PO ADMINISTRATION MODE OF ACTION It is metabolized by intestinal bacteria, resulting in the release of sulfapyridine and 5-aminosalicylate. The drug is useful in the treatment of active ulcerative colitis as well as in preventing relapses of the disease in remission. INDICATION It's thought to stop your body producing chemicals that cause redness and swelling in the gut and in the joints. It has a similar effect to immunosuppressants. CONTRAINDICATION ● Hypersensitivity to sulfasalazine, sulfa, salicylates; porphyria; GI or GU obstruction. ● Urinary tract or intestinal obstruction; Porphyria Cautions: Severe allergies, bronchial asthma, impaired hepatic/renal function, G6PD deficiency, blood dyscrasias, history of recurring or chronic infections. SIDE EFFECTS Anorexia, nausea, vomiting, headache, rash, urticaria, pruritus, fever, anemia, hypoglycemia, diuresis, photosensitivity. 143 ADVERSE EFFECTS Anaphylaxis, Stevens-Johnson syndrome, hematologic toxicity, hepatotoxicity, nephrotoxicity occur rarely. DRUG INTERACTIONS ● May increase hypoglycemic action/risk agents, of toxicity phenytoin, from oral methotrexate, zidovudine, or warfarin. ● Increase the risk of drug-induced hepatitis with other hepatotoxic agents. ● Increase the risk of crystalluria with methenamine. May decrease metabolism and increase effects/toxicity of mercaptopurine or thioguanine. NURSING 1. Assess the patient for allergy to sulfonamides and RESPONSIBILITIES salicylates. R: Therapy should be discontinued if rash, difficulty breathing, swelling of face or lips, or fever occur. 2. Monitor CBC with differential and liver function tests before and every second week during the first 3 months of therapy, monthly during the second 3 months, and every 3 months thereafter as clinically indicated. Discontinue sulfasalazine if blood dyscrasias occur. R: Sulfasalazine may cause blood problems and induce liver injury that can result in minor ALT and alkaline phosphatase elevations, acute self-limited hepatitis, and even acute liver failure. 3. Assess for rash periodically during therapy. Discontinue therapy if severe or if accompanied by fever, general malaise, fatigue, muscle or joint aches, blisters, oral lesions, conjunctivitis, hepatitis, and/or eosinophilia. R: May cause Stevens-Johnson syndrome. 4. Assess abdominal pain and frequency, quantity, and consistency of stools at the beginning of and during therapy. R: A dosage increase may be needed if diarrhea continues or 144 recurs. 5. Administer after meals or with food; and with a full glass of water. Drink several glasses of water between meals. Do not crush or chew enteric-coated tablets. R: To minimize GI irritation and drink plenty of water to prevent possible kidney problems. 6. Varying dosing regimens of sulfasalazine may be used. R: To minimize GI side effects. 7. Instruct the patient on the correct method of administration. Advise patient to take medication as directed, even if feeling better. Take missed doses as soon as remembered unless almost time for the next dose. R: Taking medicine on time, as prescribed, is essential to making sure your body has an effective amount of the drug at all times. If not, this can cause the disease to develop a resistance to the medicine or simply prolong the amount of time it takes to feel better. 8. Advise patient to notify health care professional if skin rash, sore throat, fever, mouth sores, unusual bleeding or bruising, wheezing, fever, or hives occur. R: To facilitate prompt management . 9. Caution patient to use sunscreen and protective clothing. R: To prevent photosensitivity reactions. 10. Inform the patient that this medication may cause orange-yellow discoloration of urine and skin, which is not significant. May permanently stain contact lenses yellow. R: To avoid the patient from worrying since this is a normal side effect of the drug. 145 2. Corticosteroids - This lowers the activity of your immune system and limits the inflammation in the digestive tract. They are used as short-term treatments for Crohn's disease and ulcerative colitis flares because they reduce inflammation quickly, sometimes within a few days to a few months. Generic Name HYDROCORTISONE Brand Name Hydrocort, Alphosyl, Aquacort, Cortef, Cortenema, and SoluCortef. Classification Mode of Action Corticosteroids Decreases inflammation polymorphonuclear by suppressing migration of leukocytes and lysosomal stabilization (systemic); antipruritic, anti-inflammatory (topical) Suggested Dose Inflammation: ● Adult: 15-240 mg (PO/IM/IV) every 12 hours ● Children under 12 years: 2.5-10 mg/kg/day orally divided every 6-8 hours; if 12 years and older: 15-240 mg (PO/IM/IV/SC) every 12 hours Route of Administration PO/IM/IV Indications It works by calming down your body's immune response to reduce pain, itching and swelling. It can also be used as hormone replacement for people who do not have enough of the natural stress hormone, cortisol. 146 Contraindications Hypersensitivity, fungal infections Precautions: Pregnancy C, breastfeeding, diabetes mellitus, glaucoma, osteoporosis, seizure disorders, ulcerative colitis, myasthenia gravis, renal disease, esophagitis, peptic ulcer, metastatic carcinoma, septic shock, Cushing syndrome, hepatic disease, hypothyroidism, coagulopathy, acute glomerulonephritis, amebiasis, AIDS, TB Side Effects Aggression, anxiety, blurred vision, itching eyes, decrease in the amount of urine, dizziness, dry mouth, ear congestion, fever, headache, irregular heartbeats, irritability, numbness or tingling in the arms or legs, swelling of eye, eyelid, or inner lining of the eyelid, stuffy nose, sneezing, sore throat, unusual tiredness or weakness and weight gain. Adverse Effects CNS: Depression, flushing, sweating, headache, mood changes, pseudotumor cerebri, euphoria, insomnia, seizures CV: Hypertension, circulatory collapse, thrombophlebitis, embolism, tachycardia, edema, heart failure EENT: Fungal infections, increased intraocular pressure, blurred vision, cataracts, glaucoma GI: Diarrhea, nausea, abdominal distention, increased appetite, pancreatitis, vomiting HEMA: Thrombocytopenia INTEG: Acne, poor wound healing, ecchymosis, petechiae MISC: Adrenal insufficiency (after stress/ withdrawal) MS: Fractures, Drug Interaction osteoporosis, weakness Amphotericin B, cyclosporine, digoxin: increased side effects Bosentan, carbamazepine, cholestyramine, colestipol, ephedrine, phenytoin, rifampin, theophylline: decreased action of hydrocortisone Classifications: Acetaminophen, NSAIDs, salicylates: increased risk of GI bleeding 147 Anticoagulants, calcium supplements, toxoids, vaccines: decreased action of each specific drug Anticonvulsants: decreased effects of anticonvulsant Antidiabetics: decreased effects of antidiabetics Barbiturates: decreased action of hydrocortisone Diuretics: increased side effects Herb: Ephedra: decreased hydrocortisone levels Nursing Responsibilities 1. Make sure the medicine is appropriate for the patient's condition before administering it. R: To ensure the patient is receiving the correct medication, for the correct reason, and at the correct time. 2. Monitor potassium, blood glucose, urine glucose while the patient is on long-term therapy; hypokalemia and hyperglycemia may occur. R: Corticosteroids are shown to cause a decrease in serum potassium levels in patients known to administer them. Regular monitoring of serum potassium levels can prevent hypokalemia symptoms and complications 3. Monitor I&O ratio; be alert for decreasing urinary output and increasing edema. R: Cortisol urine tests can help with the diagnosis of various medical conditions. 4. Assess for infection. R: Hydrocortisone can weaken your body's response to infection because the drug weakens your immune system. 5. Assess mental status: affect, mood, behavioral changes, aggression. R: Chronic stress and elevated cortisol levels also increase one's risk for depression, mental illness, and lower life expectancy. 148 6. Assess GI effects such as gastritis and pancreatitis. R: It is assumed to occur when ulcers erode into underlying vessels. The mechanism by which corticosteroids might induce GI bleeding or perforation has not been fully established, but corticosteroids may impair tissue repair, thus leading to delayed wound healing. 7. Check for potassium depletion: fatigue, nausea, vomiting, depression, polyuria, dysrhythmias, weakness. R: A low potassium level can make muscles feel weak, cramp, twitch, or even become paralyzed, and abnormal heart rhythms may develop. 8. Avoid alcohol and caffeine. R: It can cause damage to the liver and kidneys and may contribute to steroid-ulcer development in long-term therapy. 9. Teach patient to avoid live-virus vaccines if using steroids long term. R: Corticosteroids used in greater than physiologic doses also may reduce the immune response to vaccines. Physicians should wait at least 3 months after discontinuation of therapy before administering a live-virus vaccine to patients who have received high-dose, systemic steroids for greater than or equal to 2 weeks. 10. Teach patient to immediately report abdominal pain, black tarry stools, as GI bleeding/perforation can occur. R: Black stools are a worrisome symptom because it may be due to a large amount of bleeding into the digestive system. 3. Immunomodulators - These medicines reduce immune system activity, resulting in less inflammation in your digestive tract. It works by reducing IBD inflammation. They impact the 149 number or function of immune cells (cells of the immune system) and by doing so, they suppress the immune system in order to reduce inflammation caused by these type of cells in your body. GENERIC NAME Methotrexate BRAND NAME Otrexup, Rasuvo, Rheumatrex, Trexall DRUG CLASSIFICATION Pharmacologic: Folic acid antagonist Therapeutic: Antineoplastics, Antimetabolite MODE OF ACTION Inhibit several enzymes in the metabolic pathway of folic acid. While the cytotoxic and antiproliferative effects of high dose methotrexate are ascribed to inhibition of dihydrofolate reductase, with consequent inhibition of DNA, RNA, and protein synthesis, the anti-inflammatory and immunomodulatory actions of low doses are probably due to inhibition of other folate dependent enzymes. SUGGESTED DOSE Adult: Start with 25mg IM once a week up to 16 weeks then reduced to 15mg IM once a week or consider changing to oral therapy at this point (15mg once per week) ROUTE ADMINISTRATION INDICATION OF IM It works by interrupting the activity of the immune system to reduce inflammation in the bowel. reduces the chance of complications caused by uncontrolled inflammation. 150 CONTRAINDICATION Hypersensitivity, leukopenia, thrombocytopenia, anemia, psoriatic patients with severe renal disease, alcoholism, HIV infection SIDE EFFECTS Nausea, vomiting, stomatitis, burning/erythema at psoriatic site, Diarrhea, rash, dermatitis, pruritus, alopecia, dizziness, anorexia, malaise, headache, drowsiness, blurred vision. ADVERSE EFFECT CNS: Dizziness, seizures, headache, confusion, encephalopathy, hemiparesis, malaise, fatigue, chills, fever, leukoencephalopathy; arachnoiditis (intrathecal) EENT: Blurred vision, optic neuropathy GI: Nausea, vomiting, anorexia, diarrhea, ulcerative stomatitis, hepatotoxicity, cramps, ulcer, gastritis, GI hemorrhage, abdominal pain, hematemesis, hepatic fibrosis, acute toxicity GU: Urinary retention, renal failure, menstrual irregularities, defective spermatogenesis, hematuria, azotemia, uric acid nephropathy HEMA: Leukopenia, thrombocytopenia, myelosuppression, anemia INTEG: Rash, alopecia, dry skin, urticaria, photosensitivity, folliculitis, vasculitis, petechiae, ecchymosis, acne, alopecia, severe fatal skin reactions RESP: Methotrexate-induced lung disease SYST: Sudden death, Pneumocystis jiroveci pneumonia, tumor lysis syndrome 151 DRUG INTERACTION Drug: ● Acitretin: increased hepatitis; avoid concurrent use ● Alcohol, phenylbutazone, probenecid, radiation, theophylline: increased toxicity ● Digoxin (PO), fosphenytoin, phenytoin: decreased effect of each specific product ● Folic acid: decreased effect of methotrexate ● Radiation: increased bone marrow suppression Drug classifications: ● Anticoagulants (oral): increased hypoprothrombinemia ● Antineoplastics, NSAIDs, penicillins, salicylates, sulfa products: increased toxicity ● NURSING RESPONSIBILITIES Live virus vaccines: decreased antibodies 1. Assess symptoms indicating severe allergic reaction: rash, pruritus, urticaria, purpuric skin lesions, itching, flushing R: Information from allergy tests may help your doctor develop an allergy treatment plan that includes allergen avoidance, medications or allergy shots. 2. Assess tachypnea, ECG changes, dyspnea, edema, fatigue; identify dyspnea, crackles, unproductive cough, chest pain. R: It helps to determine the adequacy of respiration and enables the identification of changes to respiratory function. 3. Assess for bleeding: hematuria, stool guaiac, bruising or petechiae, mucosa or orifices; check for inflammation of mucosa, breaks in skin R: A person who is bleeding can die from blood loss within five minutes; therefore it is important to quickly stop the blood loss. 152 4. Teach patient that hair may be lost during treatment; a wig or hairpiece may make patient feel better; new hair may be different in color, texture. R: It is important to inform the patient ahead of time so she can already anticipate what to do. 5. Identify edema in feet, joint and stomach pain, shaking; prescriber should be notified. R: It's very important to see your healthcare provider if you experience edema or swelling in your body. Edema can stretch your skin and if not treated, swelling could increase and cause serious health problems. 6. Monitor methotrexate levels, adjust leucovorin dose based on the level. R: Methotrexate may increase the risk of problems with your liver or lungs, especially if you take a high dose. 7. Advise patient to report stomatitis: any bleeding, white spots, ulcerations in mouth to prescriber. R: Stomatitis is a complex oral complication of cancer treatment resulting from toxicities, tissue damage, and inflammation 8. Caution patient not to have any vaccinations without the advice of the prescriber R: Serious reactions can occur. 9. Advise patient to use sunblock or protective clothing to prevent burns R: A sunscreen protects from sunburn and minimizes suntan by absorbing or reflecting UV rays. Selecting a good sunscreen is important in protecting the skin. 153 10. Teach the patient to use good dental care. R: To prevent overgrowth of infection in the mouth. 4. Biologic therapies - It can help achieve remission by reducing symptoms, as well as provide healing for damage to intestines caused by inflammation. Biologic therapies are usually prescribed in people with more severe Crohn's symptoms who haven't found relief with other methods. GENERIC NAME Adalimumab BRAND NAME Humira, Amgevita, Hyrimoz, Idacio, Imraldi, Yuflyma, Cyltezo DRUG CLASSIFICATION PHARMACOTHERAPEUTIC: Monoclonal antibody. CLINICAL: Antirheumatic, disease modifying; GI agent; TNF blocking agent. 154 SUGGESTED DOSE Crohn’s Disease Induction: 160 mg SC either as 4 injections of 40 mg on day 1 or as 2 injections of 40 mg daily on 2 consecutive days, then 80 mg SC 2 weeks later (day 15) Maintenance (beginning Week 4 [Day 29]): 40 mg SC q2wk ROUTE OF SQ Injection ADMINISTRATION MODE OF ACTION Binds specifically to tumor necrosis factor (TNF) alpha cell, blocking its interac-tion with cell surface TNF receptors and cytokine-driven inflammatory processes. Therapeutic Effect: Decreases signs/symptoms of RA, psoriatic arthritis, ankylos-ing spondylitis, Crohn’s disease, ulcerative colitis. Inhibits progression of rheumatoid and psoriatic arthritis. Reduces epidermal thickness, inflammation of plaque psoriasis. INDICATION It is used to treat inflammation of the: joints (rheumatoid arthritis, polyarticular juvenile idiopathic arthritis and active enthesitisrelated arthritis) skin (plaque psoriasis and hidradenitis suppurativa) joints and skin (psoriatic arthritis) CONTRAINDICATION Contraindications: Hypersensitivity to adalimumab. Severe infections (e.g., sep-sis, TB). SIDE EFFECTS Injection site erythema, pruritus, pain, swelling, Headache, rash, sinusitis, nausea, Abdominal or back pain, hypertension. ADVERSE EFFECTS ● Hypersensitivity reactions (rash, urticaria, hypotension, dyspnea), infections (pri-marily upper respiratory tract, bronchitis, urinary tract) occur rarely. ● May increase risk of serious infections (pneumonia, tu- 155 berculosis, cellulitis, pyelonephritis, septic arthritis). ● May increase risk of reactivation of hepatitis B virus in pts who are chronic carriers. ● May cause new-onset or exacer-bation of central nervous demyelinating disease; worsening and newonset HF. ● May increase risk of malignancies. Immunoge-nicity (anti-adalimumab autoantibodies) occured in 12% of pts. DRUG INTERACTIONS ● May increase the adverse effects of abatacept, anakinra, belimumab, canakinumab, natalizumab, tofaci-tinib, vaccines (live), vedolizumab. ● May decrease the therapeutic effect of BCG (intravesical), vaccines (live). ● May increase the immunosuppressive effects of certolizumab, infliximab. ● Tocilizumab may increase the immunosuppressive effect. NURSING RESPONSIBILITIES 1. Ask if the patient have or have ever had HIV, hepatitis B or C (a viral liver infection) R: You will usually have a blood test to check for these diseases before starting adalimumab.If you have hepatitis B or have had it in the past, using Humira may cause reactivation of the virus. 2. Review immunization status/screening for TB. If pt is to self-administer, instruct on SQ injection technique, including areas of the body acceptable for injection sites. R: If you have any history of tuberculosis (TB) or any recent exposure to people with TB. You should not be given adalimumab if you have active TB, and if you have underlying inactive TB, this will need to be treated before starting 156 adalimumab. 3. Monitor lab values, particularly CBC. R: You will need regular checks and may need additional blood tests. Monitoring your treatment in this way helps your doctors fit your treatment to your needs. It can also make sure that any complications or problems with your treatment are avoided or caught at an early stage. 4. Assess history of infections, cancer, liver and heart problems. R: If you have a history of infections, currently have an infection or have symptoms such as feeling feverish or generally unwell your adalimumab treatment may need to be postponed. 5. Monitor neurological status closely. Report any change in status such as blurred vision or paresthesia. R: Humira can cause nervous system problems. Symptoms of some nervous system problems may include changes in your vision. 6. Try to avoid close contact with people who have infections. Do not receive live vaccines during treatment. R: Adalimumab affects the way your immune system works, so you may be more prone to infections. Also, even a mild infection such as a cold or sore throat could develop into a more serious illness if you are taking adalimumab. 7. Take care with food hygiene and avoid eating raw eggs or undercooked pate, meat and poultry, as well as unpasteurised dairy products and soft or blue cheeses. R: You may be more open to the type of infections caused by 157 bacteria such as listeria when being treated with adalimumab. 8. Report swelling, redness, bruising and itching on the injection site. R: Others may experience reactions to the injection such as pain or swelling, redness, bruising and itching. This can be very common, affecting at least one in 10 people. 9. Take extra precautions when in the sunlight, for example wearing a hat and high factor sun cream. R: Adalimumab can increase the risk of skin reactions, and in rare cases skin cancer. 10. Do not breastfeed when taking this medication, consult your doctor first. R: Breastfeeding during treatment with Humira may not be safe. This is because Humira passes into breast milk. C. TREATMENT THERAPY Medications RATIONALE NURSING RESPONSIBILITIES Treating Crohn’s disease is Before the procedure: designed to suppress your ● Instruct patient to take the immune system’s abnormal proper dosage, and process inflammatory response that is of causing prescribed by their doctor or your symptoms. Suppressing inflammation not only offers relief from common the medications physician. ● Educate to not take drugs all symptoms like fever, diarrhea, at once or together with and pain, it also allows your other drugs as this may intestinal tissues to heal. lessen the effect of the prescribed drug or it may 158 In addition to controlling and cause suppressing effects symptoms (inducing severe adverse remission), medication can also be used to After the procedure: decrease the frequency of symptom flare ups. ● With Advice on proper bed rest after intake of proper treatment over time, medications periods of remission can be proper absorption of the extended drug. and periods of to the facilitate symptom flare ups can be reduced. Several types of medication are being used to treat Crohn's disease today. Surgery This becomes necessary Before the procedure: when medications can no ● Secure an informed consent longer control symptoms, or if ● Obtain a medical history of you develop a fistula, fissure, or intestinal Surgery removal obstruction. often of the the patient. ● involves diseased Provide information about the procedure. ● Ensure that the patient has segment of bowel (resection), complied with the bowel the two ends of healthy bowel preparation. together ● Establish an IV line. (anastomosis). While these ● Instruct the patient to empty are then joined procedures may cause your the bladder prior to the symptoms to disappear for procedure. many years, Crohn’s frequently recurs later in life. ● Instruct the patient to remove all metallic objects from the area. After the procedure: ● Obtain and record the patient’s vital signs. Monitor 159 vital signs and neurological status every 15 minutes for 1 hour, then every 2 hours for 4 hours, or as ordered. Assess temperature every 4 hours for 24 hours. ● Instruct patient to resume a normal diet, fluids, and activity as advised by the health care provider. ● Provide privacy while the patient rest after the procedure. ● Monitor patient for any unusualities. ● Encourage patient to increase oral fluid intake. Diet and Nutrition It is essential to maintain good nutrition because ● Crohn’s Inform the client as well as family members regarding often reduces your appetite the while increasing your body’s healthy and nutritious diet. energy needs. Additionally, ● importance of the Educate patient about best common Crohn’s symptoms and easy ways to achieve a like diarrhea can reduce your good nutritious diet. body’s ability to absorb ● protein, fat, carbohydrates, as well as water, vitamins, and Maintenance of adequate hydration. ● minerals. Maintaining parental nutrition for the client. ● Helps in monitoring the Many people who experience conditions of the client like Crohn's disease flare ups find vomiting, that soft, bland foods cause electrolyte input-output, monitoring, in 160 less discomfort than spicy or order to add different high-fiber foods. While your components in the diet. diet can remain flexible and should include a variety of foods from all food groups, your doctor will likely recommend restricting your intake of dairy if you are found to be lactose-intolerant. VII. SURGICAL MANAGEMENT PROCEDURE Strictureplasty RATIONALE NURSING RESPONSIBILITIES It is repairing a stricture by Before the procedure: widening the narrowed area ● Provide answers to patient without removing any portion queries and address their of your intestine. It is important concerns to repair structures because process. regarding the the narrowing of your intestine ● Secure the consent could lead to a blockage that ● Remove all jewelry and nail prevents stool from passing polish before the surgery. through strictures the are body. When caused by disease inflammation, initial treatment may typically include medication to help improve the narrowing of the intestines. Small and Large Bowel It is a surgical procedure to Resection remove a portion of your small ● Inspect the patient's mouth and remove dentures or plates. ● Change the gown of the patient ● Prepare the equipment, instruments, and supplies needed for the procedure. or large intestine that has been damaged by Crohn’s disease. 161 ● Take the vital signs, start an During diseased the surgery, section of the your IV, and give the patient any medication required intestine is removed and the two healthy ends are joined together. 162 ● Transfer Proctocolectomy and Ileostomy It is to remove your entire colon and ileostomy is rectum. a Operating An stoma, patient to Room the and Administer Sedative. or opening in your abdomen, that a surgeon creates from a part of your ileum. The surgeon After the Procedure: ● the procedure thoroughly. brings the end of your ileum through an opening in your ● ● ● ● Advise patients that they are allowed to drink water 6 located in the lower part of hours after surgery. your abdomen, just below the ● beltline. Ensure that the patient is comfortable. inch to a little less than 2 inches wide and is most often Check for any unusualities such as rectal bleeding outside your body. The stoma is about three-quarters of an Re-evaluate the patient's vital signs. abdomen and attaches it to your skin, creating an opening After the surgery, document Provide a relaxing and noise-free environment to A removable external aid in uninterrupted rest. collection pouch, called an ostomy pouch or ostomy appliance, connects to the stoma outside and your collects stool body. Stool passes through the stoma instead of passing through your anus. The stoma has no muscle, so it cannot control the flow of stool, and the flow occurs whenever it occurs. VIII. NURSING MANAGEMENT 163 NURSING DIAGNOSIS Imbalanced than nutrition: body related to GOAL less After 8 hours of nursing INTERVENTION Independent requirements intervention, the patient will increased be able to: metabolism as evidenced by weight loss. R: Provides information about a. maintain weight within the normal BMI range, Rationale: 1. Weigh daily. dietary needs and effectiveness of therapy. b. recognize factors that If your metabolism is "high" (or are contributing to fast), you will burn more being underweight, and calories at rest and during and during the acute phase activity. A high metabolism means you'll need to take in 2. Encourage c. consume adequate nutrition. bedrest limited activity of illness. R: Decreasing aids metabolic more calories to maintain your needs in preventing weight. That's one reason why caloric some people can eat more conserves energy. depletion and than others without gaining weight. 3. Recommend rest before meals. Reference: R: Quiets peristalsis and Harvard Health. (2021, increases available energy for October 6). Does metabolism eating. matter in weight loss? Retrieved February 25, 2023, 4. Provide oral hygiene. from R: A clean mouth https://www.health.harvard.ed enhance the taste of food. can u/diet-and-weight-loss/doesmetabolism-matter-in-weightloss 5. Serve foods in wellventilated, pleasant surroundings, with an unhurried atmosphere, 164 congenial company. R: Pleasant environment aids in reducing stress and is more conducive to eating. 6. Promote patient participation in dietary planning as possible. R: Provides a sense of control for patients and opportunity to select foods desired, which may increase intake. 7. Assess the patient's overall safety. R: Imbalanced nutrition can decrease the patient’s strength and overall safety. 8. Remind foods to avoid during flares. R: When the patient experiences a flare-up, highfiber fruits and vegetables, whole grains, nuts and seeds, fatty and spicy foods, caffeine, and alcohol can worsen symptoms. Dependent 9. Administer supplements as 165 prescribed. R: Supplements can help replenish the body’s essential vitamins and nutrients since the patient is at risk for malnutrition and malabsorption. Collaborative 10. Consult with a nutritionist or dietitian. R: A dietician can assist the patient in creating a customized diet by providing information on the foods that are recommended or should be avoided. Knowledge deficit related to After 2 hours of nursing unfamiliarity of the treatment intervention, the patient will plan as evidenced by be able to: nonadherence with prevention and 1. Assess the patient’s knowledge of Crohn’s disease. management a. Verbalize knowledge about recommendations. Independent R: This will help the nurse to Crohn's disease and its signs determine what should be and symptoms, focused on during teaching. Rationale: Patients may not heed the b. Identify trigger factors that 2. Stress importance of guidance provided by their can exacerbate Crohn's good skin care (proper physicians for many reasons. disease, and handwashing Changes may be difficult for techniques the patient, either because of c. Verbalize understanding of perineal skin care). other obligations, lack of therapeutic regimen. and R: Reduces spread of bacteria 166 commitment, interest, understanding. economic mean or Socio- conditions or breakdown, infection. may treatments unaffordable and risk of skin irritation or are 3. Involve the patient in living the development of the conditions are difficult. Issues of language, culture, or care plan. R: Patient engagement in the literacy may also come into care play. independence, Non-adherence plan will promote commitment, generally may be as high as and 40%. prevention of exacerbations and Reference: adherence to management the of symptoms of Crohn’s disease. What to do when patients do 4. Welcome clarifications not follow the doctor’s advice: and questions. Dealing with non-adherence. R: Patients with Crohn’s (2021, November). CMPA. disease experience anxiety, Retrieved from embarrassment, https://www.cmpa- powerlessness. acpm.ca/en/advice- and questions from patients publications/browse- should be encouraged and articles/2013/what-to-do- welcomed. An approachable when-patients-do-not-follow- manner will create a trusting the-doctor-s-advice-dealing- environment with-non-adherence nurse and patients. fear, and Clarification between 5. Appreciate the the patient’s efforts. R: Express appreciation for the patient’s efforts and commitment to their care plan. Adhering to the management 167 of Crohn’s disease requires a lifetime commitment. 6. Ask the patient to list the preventive measures for Crohn’s disease. R: Avoiding triggering factors is the best way to manage symptoms and prevent flareups. Evaluate the patient’s understanding by having them list factors that trigger their symptoms. 7. Assess the motivation and willingness of the patient to learn. R: Learning requires energy. Patients must see a need or purpose for learning. 8. Observe and note existing misconceptions regarding material to be taught. R: Assessment provides an important starting point in education. Knowledge serves to correct faulty ideas. 9. Assess barriers to 168 learning (e.g., perceived change in lifestyle, financial concerns, cultural patterns, lack of acceptance by peers or coworkers). R: The patient brings to the learning situation a unique personality, established social interaction patterns, cultural norms and values, and environmental influences. Collaborative 10. Refer to an IBD specialist. R: Inflammatory disease deliver and (IBD) bowel specialists professional expertise. advice They can answer inquiries and guide the patient about Crohn’s disease care. Risk for fluid volume deficit as After 4 hours of nursing evidenced by vomiting and intervention, the patient will Independent 1. Monitor I&O. Note diarrhea due to narrowing in be able to maintain adequate number, the small intestine. and amount of stools; fluid volume as evidenced by: estimate Rationale: character, insensible a. Good skin turgor (<2 fluid seconds), (diaphoresis). losses 169 Crohn’s disease can lead to Measure urine specific long-term inflammation that b. Capillary refill (<3 gravity; can cause a stricture, which is seconds), and oliguria. observe for a narrowing in the small R: Provides information about intestine that can lead to a c. Balanced intake and overall fluid balance, renal blockage over time. A stricture output. function, and bowel disease can control, as well as guidelines prevent food from traveling normally through the digestive tract, for fluid replacement. causing nausea and vomiting. 2. Observe excessively dry skin and mucous Reference: membranes, Holmer, A. (2022, October 7). decreased skin turgor, Five inflammatory bowel slowed capillary refill. disease symptoms you R: Indicates excessive fluid should never ignore. NYU loss or resultant dehydration. Langone Health. Retrieved February 25, 2023, from 3. Assess vital signs (BP, https://nyulangone.org/news/fi pulse, temperature). ve-inflammatory-bowel- R: Hypotension (including disease-symptoms-you- postural), tachycardia, fever should-never-ignore can indicate response to fluid loss. 4. Weigh daily. R: Indicator of overall fluid and nutritional status. 5. Maintain oral restrictions, bedrest; avoid exertion. R: Colon is placed at rest for healing and to decrease 170 intestinal fluid losses. 6. Note generalized muscle weakness or cardiac dysrhythmias. R: Excessive intestinal loss may lead to electrolyte imbalance, e.g., potassium, which is necessary for proper skeletal and cardiac muscle function. Minor alterations in serum levels can result in profound or life-threatening symptoms. Dependent 7. Administer parenteral fluids, blood transfusions as indicated. R: Maintenance of bowel rest requires alternative fluid replacement to correct losses and anemia. 8. Monitor studies laboratory such as electrolytes (especially potassium, magnesium) ABGs and (acid-base balance). R: Determines replacement 171 needs and effectiveness of therapy. 9. Observe for overt bleeding and test stool daily for occult blood. R: Inadequate decreased diet and absorption may lead to vitamin K deficiency and defects in coagulation, potentiating risk of hemorrhage. Collaborative 10. Collaborate with dietician as indicated. R: Nutritional may be consultation beneficial determining in individual needs/dietary plans. IX. LITERATURE Prevention and Treatment of Stricturing Crohn’s Disease – Perspectives and Challenges (Seliman et al., 2020) Sleiman, J., El Ouali, S., Qazi, T., Cohen, B., Steele, S. R., Baker, M. E., & Rieder, F. (2020). Prevention and Treatment of Stricturing Crohn’s Disease – Perspectives and Challenges. Expert Review of Gastroenterology &Amp; Hepatology, 15(4), 401–411. https://doi.org/10.1080/17474124.2021.1854732 Although the pathophysiology of stricturing CD is still not fully known, it involves a complex interplay of inflammatory and non-inflammatory processes in the growth of fibrostenosis. The 172 amount of stricture reversibility and the existence of fibrotic pathways distinct from inflammatory pathways have undergone paradigm shifts over the past 15 years. Although obstruction symptoms such nausea, vomiting, postprandial abdominal pain, distention, and food limitations may point to the presence of a stricture, they are not closely associated with strictures on imaging or endoscopy. Moreover, there is no connection between the severity of small bowel strictures and the occurrence of obstructive symptoms. This indicates that additional testing is necessary to diagnose strictures as symptoms alone are insufficient. Patient risk stratification close to diagnosis in naïve, non-complicated CD would be ideal to determine which patients may or may not progress to stricturing CD. This would direct clinical judgment (e.g. combination therapy, how often to monitor, and additionally the design of future clinical trials). Reversing fibrosis in already-existing strictures would therefore be a key objective in CD care given the current incapability to identify strictures. In fact, reversibility of fibrosis has been demonstrated in various organs, including the lung, heart, skin, and kidney. Complications involving restriction are prominent in CD patients. Despite advances in medical and endoscopic therapies, most CD patients eventually undergo surgery for complicated CD. Postoperative recurrence is, unfortunately, frequent. So, the ultimate objective would be to stop intestinal fibrosis, which results from abnormal tissue repair, from developing. Although there are more biologic medicines available now than ever before, the path to stricturing problems has, for the most part, stayed constant. Hence, trying to reverse alreadypresent fibrosis would be a crucial current goal. Nutritional Treatment in Crohn’s Disease (Caio et al., 2021) Caio, G., Lungaro, L., Caputo, F., Zoli, E., Giancola, F., Chiarioni, G., De Giorgio, R., & Zoli, G. (2021). Nutritional Treatment in Crohn’s Disease. Nutrients, 13(5), 1628. https://doi.org/10.3390/nu13051628 Skip lesions and transmural inflammation from the mouth to the anus are symptoms of the chronic inflammatory bowel disease Crohn's Disease. In both adults and children, CD prevalence is rising globally, and its commencement is frequently marked by typical presenting symptoms such diarrhea, abdominal pain, rectal bleeding, fever, weight loss, and exhaustion. The best methods for determining a diagnosis and the degree of CD are endoscopy and cross-sectional imaging. Moreover, laboratory results including thrombocytosis, C-reactive protein (CRP), and some stool markers like fecal calprotectin are helpful screening tests to evaluate the disease. In approximately 65-75% of people with CD and 18-62% of patients with ulcerative colitis, malnutrition is a common, natural result of IBD (UC). Around 70% of CD patients experience 173 stricturing or penetrating problems, which frequently necessitate elective surgery within the first 20 years of diagnosis, despite major advancements in medical therapy. The worst post-operative results were typically linked to poor nutritional status and a loss of more than 10% of body weight in the six months before surgery. Nutritional supplementation may lessen the gut's inflammatory process, promoting intestinal relaxation, and improving the prognosis for recovery after surgery. The European Crohn's and Colitis Organization (ECCO) and the European Society of Clinical Nutrition and Metabolism (ESPEN) guidelines for malnourished patients undergoing major gastrointestinal surgery and/or as a minor supportive therapy in addition to an oral diet are both in favor of enteral nutrition (EN) and parenteral nutrition (PN) in CD patients. Enteral nutrition (EN) is a liquid diet plan that provides all the required calories while excluding solid meals. This kind of diet is especially advised during a disease relapse, when it should be followed for 6–8 weeks to bring about remission. A central venous catheter is used to administer nutrients (macronutrients, micronutrients, and electrolytes) through parenteral nutrition (PN) and its unique version, total parenteral nutrition (TPN). Consistent findings suggest that CD is a disorder resulting from the intricate interplay of various causes, such as gene abnormalities, altered immune response, environmental alterations, and gut microbiota changes. In this case, nutrition, including dietary modification and EN/PN, is crucial to the management of IBD, and in particular CD. Food ingredients can affect gene expression, activate metabolic pathways, and change the makeup of the microbiota, as is becoming increasingly obvious. Since they lessen inflammation, encourage mucosal healing, and lessen post-operative problems, liquid diets serve as the main therapy for CD treatment. Surgical management of Crohn’s disease: a state of the art review (Meima - Van Praag et al., 2021) Meima - Van Praag, E. M., Buskens, C. J., Hompes, R., & Bemelman, W. A. (2021). Surgical management of Crohn’s disease: a state of the art review. International Journal of Colorectal Disease, 36(6), 1133–1145. https://doi.org/10.1007/s00384-021-03857-2 An inflammatory bowel illness with granulomatous symptoms that can affect both extraintestinal organs and the entire gastrointestinal tract is called Crohn's disease. Patients often have terminal ileal or colonic penetrating illness when they first present. With a peak occurrence in adolescence and early adulthood, Crohn's disease has the highest incidence and prevalence rates in western nations. Many medicines have been investigated due to the fact that Crohn's disease is well known for its intermittent and relapsing course and the significant impact it has on 174 a patient's quality of life. Surgery was traditionally used as a last resort after medical treatments failed and is typically started as the first line of treatment. With surgical treatments becoming less invasive, it has become clear over the past few decades that earlier surgery can be used for some disease variations and in individuals with severe disease. Because it has been found to be associated with quicker recovery, less problems, fewer adhesions and incisional hernias, and preserved body image and fertility, the surgical approach in IBD must generally be minimally invasive. The function of surgery in Crohn's disease is growing in significance. For example, it is still unclear how to treat the mesentery after ileocolonic resection and proctectomy, though current research appears to support mesenterectomy in the latter. According to the study, laparoscopic ileocaecal resection is a more cost-effective treatment option for Crohn's terminal ileitis and can provide the gastroenterologist a new lease on life. The waiting period for surgery becomes an issue once it has been determined that surgery is the best course of action. There is currently a longer waiting period for both active and inactive Crohn's disease surgeries (such as pouch surgery following subtotal colectomy), as oncological surgery is prioritized above benign surgery. According to a recent cohort research, 15% of patients with inactive illness and 19% of patients with active disease experienced difficulties while waiting for surgery, and 13% of inflammatory bowel disease patients had to undergo acute- or semi-acute surgery while waiting. Consequently, cutting the waiting time to a tolerable amount could not only aid patients during the waiting period but also help prevent more complicated diseases. Eventually, surgery has been shown to be a good alternative in terms of effectiveness, quality of life, and cost as a first-line therapy or as part of combination therapy with biologicals for some conditions, and should no longer be viewed as a last resort therapy for medically refractory or complex Crohn's disease. ULCERATIVE COLITIS I. DEFINITION Ulcerative colitis is an Idiopathic inflammatory bowel disease that causes chronic inflammation and ulceration in the innermost linings of the large colon and rectum. It is an autoimmune disease when the T-cells Lymphocytes mistakenly attack the gut bacteria in the colon resulting in symptoms like abdominal pain, diarrhea, fever, fatigue, weight loss, and presence of blood in the stool. Nonetheless, This condition is one of the most common inflammatory bowel diseases along with Crohn’s disease with an estimated 156 to 291 cases per 100,000 persons per year. (Lynch, 2022) There are five types of ulcerative colitis which are ulcerative proctitis, Proctosigmoiditis, Left-sided colitis, Pancolitis, and acute severe ulcerative colitis. Ulcerative proctitis is the mildest 175 form of UC which only affects the rectum. Proctosigmoiditis affects the rectum to the lower end of the colon called sigmoid. Left-sided colitis includes the left side of the colon called descending colon down to rectum. Pancolitis and acute severe ulcerative colitis both include the entire colon. However, acute severe ulcerative colitis causes severe abdominal pain. People with UC will experience flare-ups, where the symptoms of the condition become worse, and periods of remission, which are times when the symptoms go away. (Smith, 2021) II. ANATOMY/ PHYSIOLOGY The digestive system performs mechanical processing, digestion, absorption of food, secretion of water, acids, enzymes, buffer, and salt, as well as excretion of waste materials. The digestive tract and accessory organs comprise the digestive system. The oral cavity, pharynx, esophagus, stomach, small intestine, and large intestine make up the gastrointestinal system. The teeth, tongue, and glandular organs such the pancreas, liver, gallbladder, and salivary glands are examples of accessory organs. These organs work together to provide mechanical processing, the production of bile and enzymes to aid in compound breakdown, and the excretion of waste. Mouth Even before food reaches the mouth, the digestion starts. The salivary glands start secreting saliva when a person smells or thinks about food or eating. When food enters the mouth, saliva moistens it, the teeth and tongue mechanically break it down, and salivary amylase, an enzyme, turns the food into starch. A tiny, round blob, or bolus, is formed from the food after chewing and amylase digestion. This makes it simple for an individual to swallow. Esophagus After being ingested, the bolus travels through the esophagus, where it is helped descend to the stomach by peristalsis, a process involving muscular contractions and gravity. Smooth muscles slowly contracting in and around the digestive system is known as peristalsis.These contractions push the bolus towards the direction of the stomach as it travels through the esophagus. 176 Stomach A muscle known as the lower esophageal sphincter, which resembles a ring, allows the bolus to enter the stomach. The bolus can enter the stomach when this sphincter relaxes. Temporary food storage occurs in the stomach. Gastric fluids are produced by cells in the stomach. Hydrochloric acid is one of them, and it keeps the stomach's pH between 1.5 and 2.0.Three muscular layers in the stomach mix and churn the contents. Through these procedures, the food is transformed into chyme, a thick paste. Pepsin, a protein-digesting enzyme, is activated by the breakdown of proteins and plant fibers. However, because the stomach lining is vulnerable to injury from the acid, some cells create mucus to shield it. The chyme reaches the small intestine through the pyloric sphincter because the stomach does not absorb many nutrients from the chyme into the bloodstream. Small Intestine 90% of the nutrients from food are absorbed into the bloodstream through the small intestine, which is around 20 feet (6 meters) long. First is the duodenum, which takes chyme from the stomach and digestive enzymes from the liver and pancreas. The majority of chemical digestion and absorption takes place in the jejunum, which comes in second. Third is the ileum, which houses the ileocecal valve, a sphincter via which food enters the large intestine. The villi absorb the nutrients after the meal has been completely digested, allowing them to reach the bloodstream. The small intestine is lined with vili, which resemble tiny fingerlike projections. Lacteals, which are very small capillaries, are found inside villi. The villi maximize their absorption of nutrients by expanding their surface area. Large intestine The large intestine is about five feet (or 1.5 meters) long. The large intestine is much broader than the small intestine and takes a much straighter path through the abdomen. The purpose of the large intestine is to absorb water and nutrients from the material that has not been digested as food, and get rid of any waste products left over. 177 Appendix The safe house theory of appendix states that the appendix contains a particular type of tissue associated with the lymphatic system, which carries the white blood cells needed to fight infections. In recent years, scientists have found that lymphatic tissue encourages the growth of some beneficial gut bacteria, which play an important role in human digestion and immunity. Cecum This first section of the large intestine looks like a pouch, about two inches long. It takes in digested liquid from the ileum and passes it on to the colon. Colon This is the major section of the large intestine. The colon is also the principal place for water reabsorption, and absorbs salts when needed. The colon consists of four parts: ● Ascending colon: Using muscle contractions, this part of the colon pushes any undigested debris up from the cecum to a location just under the right lower end of the liver. ● Transverse colon: Food moves through this second portion of the colon, across the front (or anterior) abdominal wall, traveling from left to right just under the stomach. ● Descending colon: The third portion of colon pushes its contents from just near the spleen, down to the lower left side of the abdomen. ● Sigmoid colon: The final S-shaped length of the colon, curves inward among the coils of the small intestine, then empties into the rectum. Rectum: The final section of digestive tract measures from 1 to 1.6 inches (or 2.5 to 4 cm). Leftover waste collects there, expanding the rectum, until defection occurs. At that time, it is ready to be emptied through the anus. Anus: The anus is the last part of the digestive tract. It's at the end of the rectum. It's where stool comes out of the body. It consists of a muscular ring (called a sphincter), that opens during a bowel movement to allow stool (feces) to pass through, as well as flat cells that line the inside of the anus. III. SIGNS AND SYMPTOMS Signs and Symptoms Rationale 178 Bloody stool Rectal bleeding is more common in ulcerative colitis. It is a result of small ulcerations in the lining of the large intestine, this leads to blood in stools. (Smith, 2021) Diarrhea During an UC flare, the lining of the intestine becomes inflamed and cannot absorb all fluid. This results in stools being loose and watery, or even entirely liquid. The looser stool can also move more rapidly through the colon, causing more frequent bowel movements. Other causes of diarrhea can include side effects of medications, changes in diet, and infections. (Basson, 2021) Abdominal pain Abdominal pain is caused by inflammatory process of the body that is further exacerbate By eating gas forming foods and food high in fiber that irritates the stomach. (Smith, 2021) Tenesmus Tenesmus is most often caused by the inflammation in the colon (large intestine). It may be a continuous or recurring sensation, and it can occur just after finishing a bowel movement. Ulceration, narrowing, blocking, or scarring of the intestinal wall can also contribute to tenesmus. (Wint, 2021) Weight Loss Symptoms like diarrhea, nausea, and abdominal pain can make the person less interested in eating. Also, inflammation can increase energy expenditure making the calorie burn quickly. (Watson, 2021) 179 Fatigue Medication side effects, sleep difficulties, associated illnesses such as anemia, and flare-ups are all possible causes of fatigue in patients with IBD. (Basson, 2022) Fever Fever is an increase in your body’s temperature in response to disease or infection. It can be developed as an inflammatory process or side effects that treat several medications of UC. (Basson, 2022) Nausea People may experience nausea during a flareup of ulcerative colitis. They may find that certain factors trigger nausea or other symptoms of ulcerative colitis, such as diarrhea or stomach pain. (Padua, 2022) Anemia People with ulcerative colitis may be anemic either due to frank blood loss from the intestine or to an iron deficiency. Malabsorption of vitamins and minerals is common in patients with IBD, and without enough iron, folic acid, and vitamin B12, the body can't make more red blood cells. (Tresca, 2020) IV. ETIOLOGY Predisposing factors Rationale Age Ulcerative colitis usually begins before the age of 30, but it can occur at any age. Some people may not develop the disease until after age 60. Since this is an autoimmune disease, cells in our body tend to change as we age thus can produce defective or bad cells. 180 (Martin, 2021) Gender Women are more likely to develop Crohn's disease than men, but more men develop ulcerative colitis than women. Even though the average age of developing IBD is between 15 and 35, more men are diagnosed with ulcerative colitis in their 50s and 60s than women of the same age. (Ehrlich, 2021) Race/Ethnicity Ulcerative colitis is more common in white people than in any other race. The incidence currently appears to have stabilized in western countries but continues to rise in Asia and South America. Consequently, for ethnicity, a genetic variation may predispose the Ashkenazi community to a greater risk of Ulcerative colitis than non-Jewish persons. (Wiginton, 2022) Family history People who have a relative who has ulcerative colitis are at risk of acquiring the same disease. A firstdegree relative of a patient with ulcerative colitis has a four times higher risk of developing the disease. (Sethi, 2022) Immune Reaction In ulcerative colitis, a theory is that the immune system mistakes "friendly bacteria" in the colon, which aid digestion, as a harmful infection, leading to the colon and rectum becoming inflamed.The imbalance of the T helper cells can also be the primary precursor of the disease process of ulcerative colitis, causing an immune response in the body can be a factor in acquiring ulcerative colitis in patients. (NHS, 2022) Decreased Bacterial Diversity Decreased diversity, considered an indicator of an 181 unhealthy microbiome, has been linked to different chronic conditions such as obesity and type 2 diabetes. The intestinal microbial population and the available variety and stability of intestinal bAnacteria are compromised in ulcerative colitis patients, with decreases in particular Firmicutes bacteria and increases in Bacteroidetes bacteria and facultative anaerobes. (NHS, 2020) Precipitating factors Rationale Diet There's no firm evidence that diet causes ulcerative colitis but certain foods and beverages can aggravate your signs and symptoms, especially during a flareup. It should also be pointed out that diet has the potential to impact the mucous layer, which protects the epithelium from the contents of the gut. (Mayo Clinic, 2023) Antibiotics Using antibiotics can cause the bacterium Clostridium difficile (C. diff) to grow and infect the lining of the intestine, which produces the inflammation. Particularly drugs with a larger microbiological scope, may be linked to an increased risk of new-onset ulcerative colitis. (Cleveland Clinic, 2023) NSAIDs Local and/or systemic effects of NSAIDs on mucosal cells might lead to an increased intestinal permeability, which is a prerequisite for colitis. The use of non-steroidal anti-inflammatory drugs can harm the colon by developing non-specific colitis or aggravating an existing colonic condition. (Mayo Clinic, 2023) 182 Stress Your body goes into fight-or-flight mode when stressed. That triggers the release of lots of chemicals, including cytokines. Those are molecules that turn on your immune system and lead to inflammation. Chronic stress promotes colitis by disturbing the gut microbiota and triggering immune system response. (Pathak, 2021) 183 V. PATHOPHYSIOLOGY A. SCHEMATIC DIAGRAM 184 185 186 Narrative: Ulcerative colitis is a long-term inflammatory condition that starts in your rectum and may spread to your colon. The colon is the large intestine (bowel) and the rectum is the end of the bowel where excrement is stored. Small ulcers can develop on the colon's lining, and can bleed and produce pus. Ulcerative colitis is thought to be an autoimmune or idiopathic condition. This means the immune system, the body's defense against infection, goes wrong and attacks healthy tissue, but there are some factors that may aggravate the condition. The predisposing factors include the age, gender specifically males are more prone, race/ethnicity, a family history of inflammatory bowel conditions, Immune reactions wherein your own cells attack healthy ones, and lastly Decreased Bacterial Diversity in the intestines. The precipitating factors then include, Diet, Antibiotics with a larger microbiological scope, NSAIDs which are said to lead to an increased intestinal permeability, and lastly, stress which triggers the release of cytokines. The epithelial barrier, covered by a mucinous layer, is the first-line of defense of the mucosal immune system, because it provides physical separation between host immune cells and luminal microbes, and synthesized antimicrobial peptides. The mentioned predisposing and precipitating factors of ulcerative colitis, associated with its uncertain cause, weaken the intestinal mucin barrier's ability to function and thus increases the permeability of the intestinal epithelial cells. As a result, a movement of microbial products into the intestinal wall takes place, activating immune cells like the T-cells and antigen-presenting cells. Then, these T-cells, when accumulated with the antigen presenting cells, stimulate the release of inflammatory cytokines. These inflammatory cytokines include the IL - 4 which is known to increase the immune response of the body, thus contributing to the development of chronic inflammation; and the IL - 12 which increases the release of cytotoxic T-cells which contributes to the destruction of intestinal tissues. Moreover, the other inflammatory cytokines such as the IL - 1, IL - 6, and TNF stimulate both the plasma cells and the endothelial cells of the blood vessels. To specify, the stimulation of the plasma cells by the three inflammatory cytokines, causes the plasma cells to differentiate into a specific antibody called the P-ANCA (perinuclear antineutrophil cytoplasmic antibody) that destroy neutrophils instead of pathogens, thus aggravating the inflammation caused by other cytokines such as IL - 4 which then lead to chronic inflammation. Furthermore, the three inflammatory cytokines also stimulate the endothelial cells of the blood vessels which leads to an increased expression of the cell adhesion molecule that interacts with WBCs; this makes the WBCs, specifically Neutrophils, travel into the intestinal wall, thus increasing its number in the intestinal wall causing more tissue destruction. Then, this chronic inflammation and tissue destruction lead to the manifestations of which include tenesmus, 187 abdominal pain, fever, fatigue, gastrointestinal bleeding, bloody diarrhea, weight loss and dehydration. Along with chronic inflammation is tissue destruction which can lead to lesions hitting the blood vessels, which causes gastrointestinal bleeding and bloody diarrhea. These symptoms are assessed as blood in stool. Diagnostic tests that are relevant to the symptoms are stool exams, blood tests and endoscopy. Simultaneously, chronic inflammation and tissue destruction lead to the inflammation and ulceration of the colon resulting in Ulcerative Colitis. Unfortunately, ulcerative colitis has no known cure, however, as mentioned, it can be managed with proper medication and diet. The prognosis of this disease lies in whether or not the patient gets treated. With proper interventions, the symptoms may be relieved. The longer periods of remission, the better outlook for the patient which leads to a fair prognosis. However, as ulcerative colitis is a chronic condition, the patient will experience periods of flare-ups and remissions throughout their life. If ulcerative colitis is left untreated, the symptoms will escalate and will further lead to complications and get worse over time. If the inflammation has reached the deeper layers of the large intestine, it can spread throughout the colon and result in complications like malnutrition, chronic fatigue, kidney failure, osteoporosis, and toxic megacolon, which causes the gut to enlarge and stop functioning. The likelihood of the colon's lining suffering extra harm rises with each flare-up. Also, people who have had ulcerative colitis for more than ten years and those who have not gotten therapy have a higher risk of getting colorectal cancer because uncontrolled inflammation can change the colon's cell structure and may result in a poor prognosis resulting in death. VI. MEDICAL MANAGEMENT A. DIAGNOSTIC EXAMS TEST RATIONALE NURSING RESPONSIBILITIES Complete blood count Blood tests can look for signs of Before the procedure: infection as well as anemia, which ● Explain the test could indicate bleeding in your procedure. About what colon or rectum. CBC can also type detect thrombocytosis needed, how it will be that most of sample patients with ulcerative colitis collected, have (Ulcerative Colitis Diagnosis equipment to use. is and what 188 ● and Testing, n.d.-b). Explain that slight discomfort may be felt when the skin is punctured. ● Encourage patients to avoid stress if possible because altered physiologic status influences and changes normal hematologic values. ● Explain that fasting is not necessary. However, fatty meals may alter some test results due to lipidemia. ● Apply manual pressure and dressings over the puncture site after the blood is drawn. After the procedure: ● Monitor the puncture site for oozing or hematoma formation. ● Instruct to resume normal activities and diet. Stool Culture Your stool specimen will be Before the procedure: analyzed to eliminate the possibility ● Assess the patient’s 189 that your symptoms are caused by level of comfort. bacteria, a virus, or a parasite Collecting stool (Ulcerative Colitis Diagnosis and specimen may Testing, n.d.-b). produce a feeling of embarrassment and discomfort the to patient. ● Encourage the patient to urinate. Allow the patient to urinate before collecting to avoid contaminating the stool with urine. ● Avoid laxatives. Advise the patient that laxatives, enemas, or suppositories avoided are three days prior to collection. ● If any special dietary restrictions are applicable, instruct the client as indicated ● Inform the client how many stool specimens are required and a supply specimen container. After the procedure: ● Label the container ● Promptly send the specimen to the 190 laboratory for analysis. ● Instruct the patient to do handwashing. Allow the patient to thoroughly clean his or her hands and perianal area. ● Resume activities. The patient may resume his or her normal diet and medication therapy unless otherwise specified. X-ray In ulcerative colitis, bowelwall Before the procedure: inflammation extends proximally ● Remove all metallic from the rectum. Therefore, x-ray objects. Items such as suggests that inflammation affects jewelry, pins, buttons the whole colon. Radiological etc can hinder the features of UC may also include visualization rectal narrowing, chest. widening of presacral space and stranding of ● perirectal fat (Jones, 2019). No of preparation the is required. Fasting or medication restriction is not needed unless directed by the health care provider. ● Ensure the patient is not pregnant suspected to or be pregnant. X-rays are usually not recommended for 191 pregnant unless women the benefit outweighs the risk of damage to the mother and fetus. ● Provide appropriate clothing. Patients are instructed to remove clothing from the waist up and put on an X-ray gown to wear during the procedure. ● Instruct patient to cooperate during the procedure. The patient is asked to remain still because any movement will affect the clarity of the image. After the procedure: ● No special care. Note that no special care is required following the procedure ● Provide comfort. If the test is facilitated at the bedside, reposition the patient properly. CT Scan CT scans use digital X-ray Before the procedure: detectors instead of traditional film ● Take off some or all of 192 detectors to create a clearer image the clothing and wear of a person’s internal structure and a hospital gown. ● how much of a person’s colon any metal inflamed objects, such as a belt (Osborne, 2022). It is performed if a or jewelry, which might complication from ulcerative colitis interfere with image is suspected. CT scan typically results. demonstrates is Remove circumferential, ● Stop eating for a few symmetrical wall thickening with hours before the scan. fold enlargement (Frcr, n.d.). If a patient is going to have a contrast injection, he or she should not anything to have eat or drink for a few hours before the CT scan because the injection may cause stomach upset. ● To receive the contrast injection, an IV is inserted into the arm just prior to the scan. The enters contrast the then body through the IV. ● Prior to most CT scans of the abdomen and pelvis, it is important to drink an oral contrast agent dilute that contains barium. This contrast agent helps 193 the radiologist identify the gastrointestinal tract (stomach, small and large bowel), detect abnormalities of these organs, and to separate these structures from other structures within the abdomen. ● If the patient has a history of allergy to contrast material (such as iodine), the requesting and physician radiology staff should be notified. ● The patient will be asked to drink slightly less than a quart spread out over 1.5 to 2 hours. After the procedure: ● After the exam, patients can return to their normal routine. ● If a patient were given a contrast material, the patient may receive special instructions. In some cases, patients may be asked to wait 194 for a short time before leaving to ensure that they feel well after the exam. After the scan, patients are likely to be told to drink lots of fluids to help their kidneys remove the contrast material from the body. Biopsy sample During the biopsy, a small piece of Before the procedure: tissue is removed from the inside of ● the intestine for further testing and analysis. Your biopsied tissue will be analyzed in a laboratory and disease (Ulcerative sterile dressing. ● pathology screened Cover the site with a Help the patient to a comfortable position. for Colitis After the procedure: Diagnosis and Testing, n.d.-b). ● Monitor his vital signs and assess puncture site the for bleeding. ● Properly label and promptly transport all specimens to the lab. sigmoidoscopy A sigmoidoscopy allows your doctor Pretest Nursing to examine the extent of the Responsibilities: inflammation in your lower colon and rectum (Ulcerative ● Colitis Instruct the patient to eat a low-residue diet Diagnosis and Testing, n.d.-b). for 3 days prior to the procedure. This procedure is the "gold standard" for diagnosing ulcerative ● Instruct the patient to only take clear liquids 195 colitis. Sigmoidoscopy allows that should be doctors to look at the inside of the consumed the evening patient’s colon as well as to take a before. biopsy that will examine via a ● Inform the client to be microscope to look for any changes NPO 8 hours prior to of UC, together with the signs of the procedure. other health conditions (Phillips, ● 2021). Note the intake of oral iron preparations within one week before the procedure because cause they black, may sticky stools that are hard to remove with bowel preparation. Post-test Nursing Responsibilities ● Patient may have mild abdominal discomfort and may feel bloated or pass gas for a few hours as he/she clears the air from his/her colon. By this, walking may help relieve any discomfort. ● Patient should be able to return to their usual diet and activities right away. Patient may also notice a small amount of blood with 196 their first bowel movement after the exam, which usually does not cause alarm. Consult a doctor if a patient continues to pass blood or blood clots or if he/she has persistent abdominal pain or a fever of 100 F (37.8 C) or higher. Colonoscopy A total colonoscopy is similar to a Pretest Nursing sigmoidoscopy, but this procedure Responsibility allows your doctor to examine your entire colon (Ulcerative ● Colitis Diagnosis and Testing, n.d.-b). Secure informed consent. ● Obtain a medical history of the patient It is also the "gold standard" for such diagnosing ulcerative colitis. This bleeding, procedure looks for UC damage medications, such as swelling, redness, and information relevant to sores in the intestine. This shows the current complaint. how severe the disease is and how ● the colon is greatly affected. as allergies, histories, Provide and information about the procedure. ● Ensure that the patient has complied with the bowel preparation. He/she must maintained a have clear liquid diet for 24-48 hours before the test, NPO after midnight, 197 and taken a laxative, as ordered. ● Inform the patient that an IV line will be started and a sedative will be administered before the procedure. Also, advise patient to the have someone drive him/her home after the procedure since sedatives will be given. ● Instruct the patient to empty the bladder prior to the procedure. ● Instruct the patient to remove all metallic objects from the area to be examined. Posttest Nursing Responsibilities: ● Observe the patient closely for signs of bowel perforation. ● Obtain and record the patient’s vital signs. Signs of bowel perforations such as severe pain, abdominal nausea, 198 vomiting, fever, and chills must be reported immediately. ● Instruct the patient to resume a normal diet, fluids, and activity advised by the health care provider. ● Provide privacy while the patient rest after the procedure. ● Monitor for any rectal bleeding. ● Encourage increased fluid intake to replace the fluid lost during the procedure. Chromoendoscopy Chromoendoscopy involves the Before the procedure: topical application of stains or pigments to localization, diagnosis improve tissue characterization, during ● consent is signed prior or endoscopy. Ensure the informed to premedication. ● Encourage questions, During a chromoendoscopy, a blue and provide answers liquid dye is sprayed into the colon and support. to highlight and detect slight ● Withhold food and changes in the lining of your fluids for 6 to 8 hours intestine(Ulcerative before the procedure. Colitis Diagnosis and Testing, n.d.-b). ● Remove dentures and eyewear. Provide mouth care. After the procedure: 199 ● After the procedure, you will be allowed to eat and drink as soon as your gag reflex returns and you are able to swallow. ● You may experience mild bloating, belching, or flatulence following the procedure. ● Contact your physician immediately if you develop any of the following: difficulty swallowing;epigastric, substernal or shoulder pain; vomiting blood or black tarry stools; or fever. B. MEDS 1. Aminosalicylates (5-ASA) Aminosalicylates are medications that contain 5-aminosalicylic acid (5-ASA) and work in the lining of the gastrointestinal tract to decrease inflammation. Aminosalicylates work best in the colon and are often given orally in the form of delayed release tablets, or rectally as enemas or suppositories. Aminosalicylates are thought to be effective in treating mild-to-moderate ulcerative colitis flares and can be useful as a maintenance treatment in preventing relapses of the disease (Medication Options for Ulcerative Colitis, 2022.). Examples: Sulfasalazine, Mesalamine, Olsalazine, Balsalazide GENERIC NAME Sulfasalazine 200 BRAND NAME Azulfidine, , Azulfidine EN-tabs, Salazopyrin DRUG CLASSIFICATION PHARMACOTHERAPEUTIC:5-Ami-nosalicylic acid derivative. CLINICAL: Anti-inflammatory. SUGGESTED DOSE PO: ADULTS, ELDERLY: Initially, 3-4 g/day in divided doses q8h. May initiate at 1-2 g/day to reduce GI intolerance. Maximum: 6 g/day. Maintenance: 2 g/day in divided doses at intervals less than or equal to q8h. CHILDREN 6 YRS AND OLDER: Initially, 40–70 mg/kg/day in 3–6 divided doses. Maximum initial dose: 4 g/day. Maintenance: 30–70 mg/kg/day in 3–6 divided doses. Maximum daily dose: 4 g/day ROUTE OF PO ADMINISTRATION MODE OF ACTION Modulates local mediators of inflam-matory response. Inhibits tumor necrosis factor (TNF). Therapeutic Effect: Decreases inflammatory response, interferes with GI secretion. Effect appears topical rather than sys-temic. INDICATION Treatment of mild to moderate ulcerative colitis, adjunctive 201 therapy in severe ulcerative colitis, rheumatoid arthritis (RA), juvenile rheumatoid arthritis. CONTRAINDICATION -Hypersensitivity to sulfasalazine, sulfa, salicylates; porphyria; GI or GU obstruction. -Urinary tract or intestinal obstruction; Porphyria Cautions: Severe allergies, bronchial asthma, impaired hepatic/renal function, G6PD deficiency, blood dyscrasias, history of recurring or chronic infections. SIDE EFFECTS Frequent (33%): Anorexia, nausea, vomiting, headache, oligospermia (generally reversed by withdrawal of drug). Occasional (3%): Hypersensitivity reaction (rash, urticaria, pruritus, fever, anemia). Rare (less than 1%): Tinnitus, hypoglycemia, diuresis, photosensitivity. ADVERSE EFFECTS Anaphylaxis, Stevens-Johnson syndrome, hematologic toxicity (leukopenia, agranulocytosis), hepatotoxicity, nephrotoxicity occur rarely. DRUG INTERACTIONS ● May increase hypoglycemic action/risk agents, of toxicity phenytoin, from oral methotrexate, zidovudine, or warfarin. ● Increase the risk of drug-induced hepatitis with other hepatotoxic agents. ● Increase the risk of crystalluria with methenamine. May decrease metabolism and increase effects/toxicity of mercaptopurine or thioguanine. NURSING RESPONSIBILITIES 1. Assess the patient for allergy to sulfonamides and salicylates. R: Therapy should be discontinued if rash, difficulty breathing, swelling of face or lips, or fever occur. 202 2. Monitor CBC with differential and liver function tests before and every second week during the first 3 months of therapy, monthly during the second 3 months, and every 3 months thereafter as clinically indicated. Discontinue sulfasalazine if blood dyscrasias occur. R: Sulfasalazine may cause blood problems and induce liver injury that can result in minor ALT and alkaline phosphatase elevations (sometimes with other signs of hypersensitivity and with hepatic granulomas), acute self-limited hepatitis, and even acute liver failure. 3. Assess for rash periodically during therapy. Discontinue therapy if severe or if accompanied by fever, general malaise, fatigue, muscle or joint aches, blisters, oral lesions, conjunctivitis, hepatitis, and/or eosinophilia. R: May cause Stevens-Johnson syndrome. 4. Assess abdominal pain and frequency, quantity, and consistency of stools at the beginning of and during therapy. R: A dosage increase may be needed if diarrhea continues or recurs. 5. Administer after meals or with food; and with a full glass of water. Drink several glasses of water between meals. Do not crush or chew enteric-coated tablets. R: To minimize GI irritation and drink plenty of water to prevent possible kidney problems. 6. Varying dosing regimens of sulfasalazine may be used. R: To minimize GI side effects. 7. Instruct the patient on the correct method of 203 administration. Advise patient to take medication as directed, even if feeling better. Take missed doses as soon as remembered unless almost time for the next dose. R: Taking medicine on time, as prescribed, is essential to making sure your body has an effective amount of the drug at all times. If not, this can cause the disease to develop a resistance to the medicine or simply prolong the amount of time it takes to feel better. 8. Advise patient to notify health care professional if skin rash, sore throat, fever, mouth sores, unusual bleeding or bruising, wheezing, fever, or hives occur. R: To facilitate prompt management . 9. Caution patient to use sunscreen and protective clothing. R: To prevent photosensitivity reactions. 10. Inform the patient that this medication may cause orange-yellow discoloration of urine and skin, which is not significant. May permanently stain contact lenses yellow. R: To avoid the patient from worrying since this is a normal side effect of the drug. 11. Instruct the patient to notify the health care professional if symptoms worsen or do not improve. If symptoms of acute intolerance (cramping, acute abdominal pain, bloody diarrhea, discontinue fever, therapy and headache, notify the rash) occur, health care professional immediately. R: Relapses occur in about 40% of patients after an initial 204 satisfactory response. Response to therapy and duration of treatment are governed by endoscopic examinations. 2. CORTICOSTEROIDS Corticosteroids suppress the immune system and are used to treat moderate to severely active ulcerative colitis. These drugs work non-specifically, meaning that they suppress the entire immune response, rather than targeting specific parts of the immune system that cause inflammation. These medications are available orally and rectally. Corticosteroids have significant short and long-term side effects and should not be used as a maintenance medication. Because they cause the adrenal glands to slow or even stop producing the body’s natural cortisol, these medications cannot be stopped abruptly. If you cannot come off steroids without suffering a relapse of your symptoms, your doctor may need to prescribe other medications to help manage your disease (Medication Options for Ulcerative Colitis, n.d.). Examples: Prednisone, Prednisolone, Methylprednisolone, Budesonide GENERIC NAME Prednisone BRAND NAME Intensol, Rayos, Winpred DRUG CLASSIFICATION PHARMACOTHERAPEUTIC: Adrenal corticosteroid. CLINICAL: Anti-inflammatory, immunosuppressant. SUGGESTED DOSE PO: ADULTS, ELDERLY: 10–60 mg/day in divided doses. Range: 2.5–100 mg/day. CHILDREN: 0.05–2 mg/kg/day in 1–4 divided doses 205 ROUTE OF PO ADMINISTRATION MODE OF ACTION Inhibits accumulation of inflammatory cells at inflammation sites, phagocytosis, lysosomal enzyme release/synthesis, release of mediators of inflammation. Therapeutic Effect: Prevents/suppresses cell mediated immune reactions. Decreases/prevents tissue response to inflammatory process. INDICATION ● Replacement therapy in adrenal cortical insufficiency. ● Hypercalcemia associated with cancer. ● Short-term management of various inflammatory and allergic disorders, such as rheumatoid arthritis, collagen diseases (eg, SLE), dermatologic diseases (eg, pemphigus), status asthmaticus, and autoimmune disorders. ● Hematologic disorders: Thrombocytopenia purpura, erythroblastopenia. ● Ulcerative colitis, acute exacerbations of MS and palliation in some leukemias and lymphomas. ● CONTRAINDICATION Trichinosis with neurologic or myocardial involvement. Hypersensitivity to predniSONE. Acute superficial herpes simplex keratitis, systemic fungal infec-tions, varicella, administration of live or attenuated virus vaccines. SIDE EFFECTS Frequent: Insomnia, heartburn, nervous-ness, abdominal distention, increased diaphoresis, acne, mood swings, appetite, facial flushing, delayed wound healing, increased susceptibility to infection, di-arrhea, constipation. Occasional: Head-ache, edema, change in skin color, frequent urination. Rare: Tachycardia, allergic reaction (rash, urticaria), psychological changes, hallucinations, de-pression. 206 ADVERSE EFFECTS Long-term therapy: Muscle wasting (esp. in arms, legs), osteoporosis, spon-taneous fractures, amenorrhea, cataracts, glaucoma, peptic ulcer, HF. Abrupt with-drawal following long-term therapy: Anorexia, nausea, fever, headache, re-bound weakness, inflammation, fatigue, lethargy, dizziness, orthostatic hypoten-sion. Sudden discontinuance may be fatal. DRUG INTERACTIONS ● CYP3A4 inducers (e.g., carBA-Mazepine, phenytoin, rifAMPin) may decrease effects. ● Live virus vaccines may increase vaccine side effects, po-tentiate virus replication, decrease pt’s antibody response to vaccine. ● May in-crease effect of warfarin. May decrease therapeutic effect of aldesleukin. May increase hyponatremic effect of des-mopressin. NURSING RESPONSIBILITIES 1. Obtain baselines for height, weight, B/P, serum glucose, electrolytes. R: Serves as a baseline in comparison with the effects of the medication. 2. Check results of initial tests (tuberculosis [TB] skin test, X-rays, ECG). R: Prednisone may cause what is known as tachycardia, or a rapid heart rate over 100 beats per minute. In clinical studies, other possible adverse cardiovascular effects reported were: Cardiac arrhythmias. Bradycardia (slowed heart rate). In patients with latent tuberculosis or tuberculin reactivity, the use of pharmacologic dosages of corticosteroids may cause a reactivation of the disease. During prolonged corticosteroid therapy, tuberculosis chemoprophylaxis may be considered. 207 3. Monitor B/P, serum electrolytes, glucose, results of bone mineral density test, height, weight in children. R: Corticosteroids can raise blood glucose level by antagonizing the action and suppressing the secretion of insulin, which results in inhibition of peripheral glucose uptake and increased gluconeogenesis. Corticosteroids can cause hypernatremia, hypokalemia, and fluid retention. All corticosteroids also increase excretion of calcium and can cause hypocalcemia. Prolonged steroid use is significantly associated with short stature and heavier weight. 4. Be alert to infection (sore throat, fever, vague symptoms); assess oral cavity daily for signs of Candida infection. R: Additional predisposing factors for Candida infection include the use of antibiotics, oral contraceptives, or adrenal corticosteroids (such as prednisone). 5. Monitor for symptoms of adrenal insufficiency,immunosuppression. R: Long-term steroid therapy can result in secondary adrenal insufficiency due to suppression of the hypothalamic-pituitaryadrenal axis. Systemic intercurrent illness can often precipitate adrenal crisis in such patients if steroid therapy is not increased temporarily to tide over the period of metabolic stress. 6. Report fever, sore throat, muscle aches, sudden weight gain, swelling, loss of appetite, or fatigue. R: General aches and pains, headache, an increased appetite that may result in weight gain, increased sweating, indigestion, and insomnia are the most common side effects reported. 7. Avoid alcohol, minimize use of caffeine. 208 R: Limit or avoid alcohol use while taking prednisone to help prevent stomach ulcers. 8. Report symptoms of elevated blood sugar levels (blurred vision, headache, increased thirst, frequent urination). R: All corticosteroids, including prednisolone, can cause salt and fluid retention, which may lead to blood pressure elevation and increased potassium excretion. Calcium excretion is also increased. Cataracts, glaucoma, eye infections, an increase in new episodes of optic neuritis, and corneal perforation associated with herpes simplex of the eye, have all been reported with prednisone use. 9. Do not abruptly discontinue without physician’s approval. R: May cause withdrawal symptoms if stopped suddenly after long-term or high-dose therapy. Symptoms include fever, vomiting, loss of appetite, diarrhea, weight loss, general aches, and pains. 10. Avoid exposure to chickenpox, measles. R: Prednisone may decrease your ability to fight infection and can prevent you from developing symptoms if you get an infection. Stay away from people who are sick and wash your hands often while you are taking this medication. 11. Gradually reduce dosage after long-term therapy. R: Long-term use may significantly increase risk of serious infections. 3. IMMUNOMODULATORS This class of medication controls or suppresses the body’s immune system response so it cannot cause ongoing inflammation. Immunomodulators, which may take several months to begin 209 working, are generally used when aminosalicylates and corticosteroids haven’t been effective, or have been only partially effective. These medications may be useful in reducing or eliminating the need for corticosteroids, and in maintaining remission in people who haven’t responded to other medications given for this purpose. Some immunomodulators are used to make other medications, such as biologics, work better (Medication Options for Ulcerative Colitis, 2022). Examples: Azathioprine, 6-mercaptopurine, Cyclosporine, Tacrolimus GENERIC NAME Azathioprine BRAND NAME Azasan, Imuran DRUG CLASSIFICATION PHARMACOTHERAPEUTIC: Immunologic agent. CLINICAL: Immunosuppressant. SUGGESTED DOSE Ulcerative Colitis (Off-label): Maintenance, remission, or reduction of steroid 1.5-2.5 mg/kg PO once daily ROUTE OF PO/IV ADMINISTRATION MODE OF ACTION Metabolites are incorporated into replicating DNA and halt replication. Blocks purine synthesis pathway. Therapeutic Effect: Suppresses cell-mediated hypersensitivities; alters antibody production, immune response in transplant recipients. Reduces symptoms of arthritis severity. 210 INDICATION ● Renal homotransplantation: Adjunct for prevention of rejection ● Rheumatoid arthritis: Use only with adults meeting criteria for classic rheumatoid arthritis and not responding to conventional management ● Unlabeled use: Treatment of chronic ulcerative colitis, myasthenia gravis, Behçet’s syndrome, Crohn’s disease CONTRAINDICATION Contraindications: Hypersensitivity to azaTHIOprine. Pregnant women with RA, and pts previously treated for RA with alkylating agents (cyclophosphamide, chloram-bucil, melphalan) may have a prohibitive risk of malignancy with azathioprine. Cautions: Immunosuppressed pts, pts with hepatic/renal impairment, active infection. Testing for genetic deficiency of thiopurine methyltransferase should be obtained. (Absence or reduced levels increase risk of myelosuppression.) SIDE EFFECTS Frequent: Nausea, vomiting, anorexia (particularly during early treatment and with large doses). Occasional: Rash. Rare: Severe nausea/vomiting with diarrhea, abdominal pain, hypersensitivity reaction. ADVERSE EFFECTS Increases risk of neoplasia (new abnormal-growth tumors). Significant leukopenia and thrombocytopenia may occur, particularly in pts undergoing renal transplant rejection. Hepatotoxicity occurs rarely. DRUG INTERACTIONS Allopurinol may increase activity and toxicity. May increase the immunosuppressive effect of baricitinib, fingolimod, and mercaptopurine. May decrease the therapeutic effect of BCG (intra-vesical), and vaccines (live). May increase adverse effects of natalizumab, and vaccines (live). NURSING 1. History: Allergy to azathioprine; rheumatoid arthritis 211 RESPONSIBILITIES patients previously treated with alkylating agents; pregnancy or male partners of women trying to become pregnant; lactation R:IMURAN should not be given to patients who have shown hypersensitivity to the drug. Patients with rheumatoid arthritis previously treated with alkylating agents (cyclophosphamide, chlorambucil, melphalan, or others) may have a prohibitive risk of malignancy if treated with IMURAN. IMURAN should not be used for treating rheumatoid arthritis in pregnant women.IMURAN can cause fetal harm when administered to a pregnant woman. IMURAN should not be given during pregnancy without careful weighing of risk versus benefit. 2. Physical: T; skin color, lesions; liver evaluation, bowel sounds; LFTs, renal function tests, CBC R: Taking azathioprine can sometimes affect your liver, kidneys or bone marrow. You will have blood tests to check your liver function, kidney function and blood count before you start taking this medicine. 3. Give drug IV if oral administration is not possible; switch to oral route as soon as possible. R: Intravenous azathioprine should only be used when the oral route is impractical.It should be switched to the oral route as soon as possible as this is a very irritant solution due to alkaline nature of injection. Use only if oral route not feasible, and avoid extravasation 4. Administer in divided daily doses or with food if GI upset occurs. R: These should be taken with a meal to reduce upset stomach. 5. BLACK BOX WARNING: Monitor blood counts regularly; 212 severe hematologic effects may require the discontinuation of therapy; increases risk of neoplasia. R: Azathioprine can cause a decrease in the number of blood cells in your bone marrow, which may cause serious or lifethreatening infections. You will need to have regular blood tests to monitor for side effects and to check whether the treatment is effective. 6. Monitor I&O ratio; note color, character, and specific gravity of urine. Report an abrupt decrease in urinary output or any change in I&O ratio. R: Decreased urine output may lead to toxicity with this medication. 7. Avoid infections; avoid crowds or people who have infections. Instruct patient to not receive/take vaccinations or other immunity-conferring agents during therapy R: Azathioprine may lower your body's resistance and the vaccine may not work as well or you might get the infection the vaccine is meant to prevent. In addition, you should not be around other persons living in your household who receive live virus vaccines because there is a chance they could pass the virus on to you. 8. Avoid prolonged or unnecessary exposure to sunlight and wear protective clothing, sunglasses, and sunscreen. R: To decrease the risk that you will develop skin cancer, Azathioprine may increase your risk of developing certain types of cancer, especially skin cancer and lymphoma (cancer that begins in the cells that fight infection). 213 9. Notify your health care provider if you think you are pregnant or wish to become pregnant, or if you are a man whose sexual partner wishes to become pregnant. R: Using this medicine while you are pregnant can harm your unborn baby. Use an effective form of birth control to keep from getting pregnant. If you think you have become pregnant while using this medicine, tell your doctor right away. 10. Report unusual bleeding or bruising, fever, sore throat, mouth sores, signs of infection, abdominal pain, severe diarrhea, darkened urine or pale stools, severe nausea and vomiting. R: These could be symptoms of a serious reaction to the medicine in your bowel. Azathioprine can temporarily lower the number of white blood cells in your blood, increasing the chance of getting an infection. It can also lower the number of platelets, which are necessary for proper blood clotting. 4. BIOLOGICS Biologics are used to treat people with moderate-to-severe ulcerative colitis. Unlike other medications, biologics are protein-based therapies that are created out of material naturally found in life. These medications are antibodies that stop certain proteins in the body from causing inflammation (Medication Options for Ulcerative Colitis, 2022). Examples: Adalimumab, Golimumab, Infliximab, Ustekinumab, Vedolizumab GENERIC NAME Adalimumab 214 BRAND NAME Humira, Amgevita, Hyrimoz, Idacio, Imraldi, Yuflyma, Cyltezo DRUG CLASSIFICATION PHARMACOTHERAPEUTIC: Monoclonal antibody. CLINICAL: Antirheumatic, disease modifying; GI agent; TNF blocking agent. SUGGESTED DOSE Ulcerative Colitis SQ: ADULTS, ELDERLY: Initially, 160 mg (4 injections in 1 day or 2 injections over 2 consecutive days) then 80 mg 2 wks later (day 15), then 40 mg every other wk beginning on day 29. ROUTE OF Subcutaneous Injection ADMINISTRATION MODE OF ACTION Binds specifically to tumor necrosis fac-tor (TNF) alpha cell, blocking its interac-tion with cell surface TNF receptors and cytokine-driven inflammatory processes. Therapeutic Effect: Decreases signs/symptoms of RA, psoriatic arthritis, ankylos-ing spondylitis, Crohn’s disease, ulcerative colitis. Inhibits progression of rheumatoid and psoriatic arthritis. Reduces epidermal thickness, inflammation of plaque psoriasis. INDICATION ● Reduces signs/symptoms, progression of structural damage and improves physi-cal function in adults 215 with moderate to severe RA. May be used alone or in com-bination with other disease-modifying antirheumatic drugs. ● First-line treatment of moderate to severe RA, treatment of psoriatic arthritis, treatment of anky-losing spondylitis, to induce/maintain remission of moderate to severe active Crohn’s disease, moderate to severe plaque psoriasis in pts 6 yrs of age and older. ● Reduces signs and symptoms of moderate to severe active polyarticular juvenile rheumatoid arthritis in pts 2 yrs and older. ● Treatment of active ulcerative colitis in pts unresponsive to immunosuppressants. ● Treatment of moderate to severe hidradenitis suppurativa. ● Treatment of uveitis (noninfectious intermediate, posterior and panuveitis) in adults. CONTRAINDICATION Contraindications: Hypersensitivity to adalimumab. Severe infections (e.g., sep-sis, TB). SIDE EFFECTS Frequent (20%): Injection site erythema, pruritus, pain, swelling. Occasional (12%–9%): Headache, rash, sinusitis, nausea. Rare (7%–5%): Abdominal or back pain, hypertension. ADVERSE EFFECTS ● Hypersensitivity reactions (rash, urticaria, hypotension, dyspnea), infections (pri-marily upper respiratory tract, bronchitis, urinary tract) occur rarely. ● May increase risk of serious infections (pneumonia, tuberculosis, cellulitis, pyelonephritis, septic arthritis). ● May increase risk of reactivation of hepatitis B virus in pts who are chronic carriers. 216 ● May cause new-onset or exacer-bation of central nervous demyelinating disease; worsening and newonset HF. ● May increase risk of malignancies. Immunoge-nicity (anti-adalimumab autoantibodies) occured in 12% of pts. DRUG INTERACTIONS ● May increase the adverse effects of abatacept, anakinra, belimumab, canakinumab, natalizumab, tofaci-tinib, vaccines (live), vedolizumab. ● May decrease the therapeutic effect of BCG (intravesical), vaccines (live). ● May increase the immunosuppressive effects of certolizumab, infliximab. ● Tocilizumab may increase the immunosuppressive effect. NURSING RESPONSIBILITIES 1. Assess history of infections, cancer, liver and heart problems. R: If you have a history of infections, currently have an infection or have symptoms such as feeling feverish or generally unwell your adalimumab treatment may need to be postponed. If you have heart problems, as adalimumab may make your symptoms worse, and your heart will need to be monitored closely before, during, and after treatment. If you have a history of cancer. Adalimumab affects the way in which your immune system works and you may have an increased risk of developing some types of cancer. Humira may cause you to develop liver problems. If you have liver problems or have had them in the past, tell your doctor before using Humira. 2. Ask if the patient have or have ever had HIV, hepatitis B or C (a viral liver infection) R: You will usually have a blood test to check for these diseases 217 before starting adalimumab.If you have hepatitis B or have had it in the past, using Humira may cause reactivation of the virus. They’ll likely monitor you more closely throughout your Humira treatment to make sure your hepatitis B symptoms don’t return. 3. Review immunization status/screening for TB. If pt is to self-administer, instruct on SQ injection technique, including areas of the body acceptable for injection sites. R: If you have any history of tuberculosis (TB) or any recent exposure to people with TB. You should not be given adalimumab if you have active TB, and if you have underlying inactive TB, this will need to be treated before starting adalimumab. Most doctors now use a blood test to check for underlying or inactive TB, but you may be given a chest x-ray as well. 4. Monitor lab values, particularly CBC. R: you will need regular checks and may need additional blood tests. Monitoring your treatment in this way helps your doctors fit your treatment to your needs. It can also make sure that any complications or problems with your treatment are avoided or caught at an early stage. You may also be given a special blood test to check the levels of adalimumab in your blood. This can help your doctor see how well the adalimumab is working, and whether you have developed antibodies to it. 5. Monitor neurological status closely. Report any change in status such as blurred vision or paresthesia. R: Humira can cause nervous system problems. Symptoms of some nervous system problems may include changes in your vision. 218 6. Try to avoid close contact with people who have infections. Do not receive live vaccines during treatment. R: Adalimumab affects the way your immune system works, so you may be more prone to infections. Also, even a mild infection such as a cold or sore throat could develop into a more serious illness if you are taking adalimumab. You may also be at greater risk of becoming more seriously ill from viruses and bacteria such as those that cause chickenpox and shingles, measles, and pneumococcal disease. 7. Take care with food hygiene and avoid eating raw eggs or undercooked pate, meat and poultry, as well as unpasteurised dairy products and soft or blue cheeses. R: You may be more open to the type of infections caused by bacteria such as listeria when being treated with adalimumab. 8. Report swelling, redness, bruising and itching on the injection site. R: Others may experience reactions to the injection such as pain or swelling, redness, bruising and itching. This can be very common, affecting at least one in 10 people. 9. Take extra precautions when in the sunlight, for example wearing a hat and high factor suncream R: Adalimumab can increase the risk of skin reactions, and in rare cases skin cancer. 10. Tell your doctor immediately if you develop any of the following symptoms: A severe rash, hives (swollen red patches of skin) or other signs of allergic reaction Swollen face, hands and feet Trouble breathing or swallowing, Shortness of breath, Persistent fever, 219 bruising, bleeding or paleness, Fatigue, cough, or flu-like symptoms. R: Symptoms that mean you are having an allergic reaction to adalimumab. For example, rashes, hives (a raised itchy rash that appears on the skin), a swollen face, hands and feet, or trouble breathing and shortness of breath. Some of the more common side effects of adalimumab include abdominal pain, nausea, headaches, fatigue and joint pain. 11. Do not breastfeed when taking this medication, consult your doctor first. R: Breastfeeding during treatment with Humira may not be safe. This is because Humira passes into breast milk. 5. Janus kinase inhibitors (JAK inhibitors) These are oral medicines that can work quickly to get and maintain a remission in ulcerative colitis. Tofacitinib (Xeljanz) is the first JAK inhibitor that is FDA-approved for the treatment of ulcerative colitis (Pathak, 2021). GENERIC NAME Tofacitinib BRAND NAME Xeljanz, Xeljanz XR DRUG CLASSIFICATION PHARMACOTHERAPEUTIC: Janus-associated kinase (JAK) inhibitor. CLINICAL: Antirheumatic, disease-modifying. 220 SUGGESTED DOSE PO: ADULTS/ELDERLY: (Xeljanz): Induc-tion: 10 mg twice daily for 8 wks. May transition to maintenance dose or con-tinue 10 mg twice daily for additional 8 wks. Discontinue if 10 mg twice daily is in-effective after 4 mos. Maintenance: 5 mg twice daily. May increase to 10 mg twice daily for shortest duration. Use lowest ef-fective dose to maintain response. ROUTE OF PO ADMINISTRATION MODE OF ACTION Inhibits JAK enzymes, which are intracel-lular enzymes involved in stimulating he-matopoiesis and immune cell functioning through a signaling pathway. Therapeutic Effect: Reduces inflammation, tenderness, swelling of joints; slows or prevents progres-sive joint destruction in rheumatoid arthritis (RA). Prevents cytokine or growth factor gene expression, reducing circulating natu-ral killer cells and increasing B cells. INDICATION ● Treatment of adult pts with moderate to se-vere active rheumatoid arthritis with previous inadequate response or intolerance to meth-otrexate. ● May be used as monotherapy or in combination with methotrexate or other nonbiologic disease-modifying antirheu-matic drugs (DMARDs). ● Treatment of active psoriatic arthritis (PsA) in pts who have had inadequate response to methotrexate, other DMARDs. ● Treatment of moderate to severe active ulcerative colitis (UC) in adults. Do not use in combination with other biologic DMARDs immunosuppressants (e.g., or with potent azaTHIOprine, cycloSPORINE). CONTRAINDICATION Contraindications: Hypersensitivity to to-facitinib. 221 Cautions: Pts exposed to TB, his-tory of serious opportunistic infections, con-ditions that predispose to infections (e.g., diabetes), pts at risk for GI perforation (e.g., diverticulitis), pts who resided or traveled in areas where TB is endemic, moderate to severe renal impairment, elderly pts, he-patic impairment, history of anemia, hyper-lipidemia, hepatitis, Asian ancestry, pts with history of interstitial lung disease, heart rate less than 60 bpm, conduction abnormali-ties, ischemic heart disease, HF. SIDE EFFECTS Rare (4%–2%): Upper respiratory tract infection, diarrhea, nasopharyngitis, headache, hypertension. ADVERSE EFFECTS Neutropenia, lymphopenia may increase risk Serious infections may for infection. include aspergillosis, BK virus, cellulitis, coccidioidomycosis, cryptococcus, cy-tomegalovirus, esophageal candidiasis, histoplasmosis, infections, listeriosis, tuberculosis, UTI, invasive pneumocystosis, sepsis. Increased risk fungal pneumonia, for various malignancies. May induce viral re-activation of hepatitis B or C virus infection, herpes zoster, HIV. Epstein-Barr virus–associated post-transplant lymphoproliferative disorder reported in 2% of pts with renal transplant. Increased risk for GI perforation. DRUG INTERACTIONS Immunosuppressants (e.g., azaTHIOprine, cycloSPORINE) may increase risk for added immunosuppression, infection. CYP3A4 inhibitors concentration/effect. (e.g., ketoconazole) CYP3A4 inducers may (e.g., increase phenytoin, rifAMPin) may decrease concentration/effect. May increase adverse effects; decrease therapeutic effect of vaccines (live). NURSING RESPONSIBILITIES 1. Obtain vital signs, CBC, BMP, LFT, lipid panel, urine pregnancy test results. 222 R: A baseline complete blood count (CBC) should be done before starting tofacitinib and 1 to 2 months following initiation, and every 12 weeks after that. Subjects with hemoglobin (Hb) levels below 9 g/dL, absolute lymphocyte count below 500 cells/mm^3, and absolute neutrophil count below 1000 cells/mm^3 should not be started on therapy. Baseline lipid levels should be obtained and monitored 4 to 8 weeks after initiation of treatment. Dose-dependent increases in total cholesterol, low-density lipoprotein (LDL) cholesterol, and highdensity lipoprotein (HDL) cholesterol may occur. 2. Evaluate for active tuberculosis (TB) and test for latent infection prior to and during treatment. Induration of 5 mm or greater with purified protein derivative (PPD) is considered positive result when assessing for latent TB. R: Before initiating treatment with tofacitinib, the patient should be tested for active or latent TB. In the case of a positive active or latent TB test, patients should be treated accordingly prior to receiving treatment with tofacitinib. 3. Question possibility of pregnancy or breastfeeding. R: Using this medicine while you are pregnant can harm your unborn baby. Use an effective form of birth control to keep from getting pregnant.If you think you have become pregnant while using this medicine, tell your doctor right away. 4. Obtain a full medication history including vitamins, herbal products. R: Do not take other medicines unless they have been discussed with your doctor. This includes prescription or nonprescription (over-the-counter [OTC]) medicines and herbal or vitamin supplements. 223 5. Obtain CBC every 4–8 wks, then every 3 mos, lipid panel 4–8 wks after initiation; hepatic function panel if hepatic impairment suspected. R: May increase ALT, AST, bilirubin, lipids, creatinine. May decrease Hgb, neutrophils, lymphocytes. Liver function tests should also be monitored routinely as tofacitinib may cause hepatotoxicity. If hepatic injury from tofacitinib is suspected, treatment should be interrupted. Use in severe hepatic impairment is not recommended. 6. Monitor for TB regardless of baseline PPD. R: Studies have suggested that its administration leads to increased TB reactivation. Thus, as with TNF inhibitor, LTBI screening and treatment are recommended prior to starting tofacitinib. 7. Routinely monitor blood levels. R: You should not receive XELJANZ/XELJANZ XR if your lymphocyte count, neutrophil count, or red blood cell count is too low or your liver tests are too high.This will allow your doctor to see if this medicine is working properly and to decide whether you should continue to use it. Blood tests are needed to check for unwanted effects. 8. Consider infection, discontinuation opportunistic if pt infection, develops acute sepsis; initiate appropriate antimicrobial therapy. R: Patients receiving treatment should be routinely monitored for the development of any severe infections. If you have any kind of infection. You may be at a higher risk of developing shingles (herpes zoster). 224 9. Immediately abdominal report pain, any hemorrhaging, melena, hemoptysis (may indicate GI perforation). R: People who take anti-inflammatory medications such as NSAIDs or corticosteroids while they are also taking tofacitinib may be more likely to experience a tear in the lining of the stomach, which can cause serious bleeding. 10. Do not receive live virus vaccines. R: While you are being treated with tofacitinib, and after you stop treatment with it, do not have any immunizations (vaccines) without your doctor's approval. Tofacitinib may lower your body's resistance and there is a chance you might get the infection the vaccine is meant to prevent. Some examples of live vaccines include measles, mumps, influenza (nasal flu vaccine), poliovirus (oral form), rotavirus, and rubella. 11. Educate patients about the risk of infection and tell them to immediately report any signs and symptoms of infection to their healthcare provider. R: Your body's ability to fight infections may be reduced while you are using tofacitinib. It is very important that you call your doctor at the first sign of an infection. Check with your doctor right away if you have a fever, chills, cough, flu-like symptoms, or unusual tiredness or weakness. 12. Re-port history of HIV, recent infections, hepa-titis B or C, TB or close relatives who have active TB. R: XELJANZ/XELJANZ XR may cause serious side effects, including Hepatitis B or C activation infection in people who carry the virus in their blood. If you are a carrier of the Hepatitis B or C virus (viruses that affect the liver), the virus may become active while you use XELJANZ/XELJANZ XR.you should not be 225 around other persons living in your household who have active TB because there is a chance they could pass the virus on to you. 13. Report any travel plans to possible endemic areas. R: Tofacitinib can temporarily lower the number of white blood cells in your blood, increasing the chance of getting an infection. If this occurs, there are certain precautions you can take, especially when your blood count is low, to reduce the risk of infection. 14. Notify physician if pregnant or planning pregnancy. R: If you plan to have children, talk with your doctor before using this medicine. Some women using this medicine have become infertile (unable to have children). 15. Tell your doctor right away if you have black, tarry stools, general feeling of illness, swollen glands, weight loss, yellow skin and eyes, persistent non-healing sore, reddish patch or irritated area, shiny bump, pink growth, or white, yellow or waxy scar-like area on the skin. R: This medicine may increase your risk of cancer (eg, lymphoma, lung cancer, non-melanoma skin cancer). 16. Tell your doctor right away if you start to have swelling of your face, lips, tongue, throat, arms, or legs, or if you are having trouble swallowing or breathing. R: This medicine can cause serious allergic reactions, including angioedema or urticaria. 17. Check with your doctor right away if you have anxiety, chest pain, cough, dizziness, lightheadedness, or fainting, fast heartbeat, pain, redness, or swelling in the 226 arm or leg, pains in the chest, groin, or legs, especially calves of the legs, severe headaches, sudden loss of coordination, sudden onset of slurred speech, sudden vision changes, or trouble breathing. R: This medicine may increase your risk of developing blood clots (eg, arterial thrombosis, deep vein thrombosis, pulmonary embolism), especially in patients with rheumatoid arthritis who are 50 years of age and older and with a heart or blood vessel disease. 18. Avoid grapefruit products. R: It is best to avoid taking Tofacitinib with grapefruit juice and to avoid grapefruit juice completely during your Tofacitinib treatment. Grapefruit juice may increase the levels of Tofacitinib and the risk for side effects from your treatment. C. TREATMENT THERAPY RATIONALE Medications Medication for ulcerative colitis NURSING RESPONSIBILITIES ● Educate client about can suppress the inflammation medications such as The of the colon and allow for purpose of the medication, tissues to heal. Symptoms the dosage, the side effects, including diarrhea, bleeding, and the possible adverse and abdominal pain can also effects of the medication be reduced and controlled with ● effective medication. Educate client medication on self- administration procedures In addition to controlling and suppressing (inducing symptoms remission), ● Prepare and administer medications, using rights of medication administration 227 medication can also be used to ● Review pertinent data prior decrease the frequency of to medication administration symptom ups (e.g., contraindications, lab (maintaining remission). With results, allergies, potential proper treatment over time, interactions) flare periods of remission can be extended and periods ● of vials when necessary (e.g., symptom flare ups can be reduced. Several types of Mix medications from two insulin) ● Administer and document medication are being used to medications treat ulcerative colitis today common routes (e.g., oral, (crohn’scolitisfoundation.org, topical) ● 2022). given Administer and document medications Combination Therapy In some circumstances, a health care provider may adding an recommend additional therapy that will parenteral effectiveness. combination ● the addition of a biologic to an ● glucose toxicity. Your healthcare dosage of based on (e.g., giving levels, titrating medication to maintain a specific blood pressure) ● Dispose of unused medications according to of IBD treatment, but there of additional side effects and medication insulin according to blood can increase the effectiveness may also be an increased risk Titrate parameters combination therapy. Combining therapies in assessment and ordered therapy, there are risks and of Participate medication immunomodulator. As with all benefits (e.g., reconciliation process could include routes by subcutaneous) For example, therapy given intravenous, intramuscular, work in combination with the initial therapy to increase its by facility/agency policy ● Evaluate appropriateness and accuracy of medication order for client 228 provider will identify the ● treatment option that is most effective for your individual Educate the patient abouot the following: ● How and where the health care needs (crohn's medication should be safely colitis foundation.org, 2022). stored, such as in the refrigerator or in a dark place. ● The importance of and the method for checking the medication's label for the name, dose, and expiration date. ● Special instructions such as shaking the medication, taking the medication with meals or between meals and on an empty stomach. ● When to call the doctor about any side effects ● The importance of taking the medication as instructed ● The need to continue the medication unless the doctor discontinues it ● Information supplements about foods, and other medications, including over the counter medications and preparations, that can interact with the ordered medication ● The safe disposal of unused and expired medications 229 ● The importance of keeping medications in a secure place that would not place a curious child or a cognitively impaired adult at risk for taking medications not intended for them ● The proper disposal and safe of biohazardous any equipment such as used needles that the client uses for insulin and other medications. Surgery Surgery is an option if PREOPERATIVE NURSING medications aren’t working or CARE: you have complications, such as bleeding or ● abnormal lesions, or routine preoperative care for the growths. You might develop precancerous Provide surgical client. ● Arrange for consultation growths that can turn into with enterostomal therapy colorectal cancer. A (ET) healthcare provider can appropriate. The ET nurse remove these lesions with is trained to identify and surgery mark an appropriate stoma (a colectomy) or during a colonoscopy. specialist location, taking if into consideration the level of There are two kinds of surgery ostomy, skinfolds, and the for ulcerative colitis: client’s 1. Proctocolectomy and clothing preferences. Initial ostomy ileoanal pouch- The care teaching also is proctocolectomy and provided by the ET nurse ileoanal pouch (also during the preoperative visit. 230 called J-pouch ● Insert a nasogastric tube if surgery) is the most ordered.Although it is often common procedure for inserted in the surgical suite ulcerative colitis. just prior to surgery, the 2. Proctocolectomy ileostomy- If and nasogastric tube may be placed preoperatively ileoanal pouch won’t remove secretions work empty stomach contents. for you, an your healthcare team might recommend permanent (without an ● a and Perform bowel preparation procedures as ordered. Oral ileostomy ileoanal to and ● parenteral antibiotics as well pouch)(Cleveland as cathartics and enemas Clinic, 2020). may be ● prescribed preoperatively to clean the bowel and reduce the risk of contamination peritoneal by bowel contents during surgery. POSTOPERATIVE NURSING CARE: ● Provide routine care for the surgical client. ● Monitor bowel sounds and degree of abdominal distention. Surgical manipulation of the bowel disrupts peristalsis, resulting in an initial ileus. Bowel sounds and the passage of flatus indicate a return of peristalsis. ● Assess the position and 231 patency of the nasogastric tube, connecting it to low suction. If the tube becomes clogged, gently irrigate with sterile normal saline. A nasogastric or gastrostomy tube is used postoperatively to provide gastrointestinal decompression facilitate and healing of the anastomosis. Ensuring its patency is important for comfort and healing. ● Assess color, amount, and odor of surgical drainage drains colostomy (if from and the present), noting any changes or the presence of clots or bright bleeding. Initial, drainage may be bright red and then become dark and finally clear or greenish yellow over the first 2 to 3 days. A change in the color, amount or odor of the drainage may indicate a complication such as hemorrhage, intestinal obstruction, or infection. ● Alert all personnel caring for the client with an abdominoperineal resection to avoid rectal 232 temperatures, suppositories, or ● other These rectal procedures. procedures could disrupt the anal ● suture line, bleeding, causing infection, or impaired healing. ● Maintain intravenous fluids while nasogastric suction is in place. The client on nasogastric suction is unable to take oral food and fluids and, moreover, is losing electrolyte-rich fluid through the nasogastric tube. If replacement fluid and electrolytes are not maintained, the client is at risk for dehydration; sodium, potassium, and chloride imbalance; and metabolic alkalosis. ● Provide antacids, histamine2-receptor antagonists, and antibiotic therapy as ordered. The above medications may be ordered for postoperative the client, depending on the procedure performed. therapy is Antibiotic a common 233 measure to infection prevent resulting contamination abdominal from of the cavity with gastric contents. ● Resume oral food and fluids as ordered. Initial feedings may ● be clear liquids, progressing to full liquids, and then frequent small feedings of regular foods. Monitor bowel sounds and monitor for abdominal frequently distention during this period. Oral feedings are reintroduced slowly minimize to abdominal distention and trauma to the suture lines. ● Begin discharge planning and teaching. Consult with a dietitian for instructions and menu planning; reinforce teaching. Teach potential postoperative complications, abdominal bowel about such as abscess, or obstruction, their signs and symptoms, and preventive measures. Diet and Nutrition While ulcerative colitis is not ● Educated about best and 234 caused by the foods you eat, easy ways to achieve a you may find that once you good nutritious diet. have the disease, particular foods can aggravate ● the Educates the client as well as family members symptoms. It’s important to regarding the importance of maintain the healthy and nutritious a healthy and soothing diet that helps reduce your symptoms, replace lost nutrients, and diet. ● promote Nurse maintains the adequate diet plans for the healing. client. ● Helps in monitoring the For people diagnosed with conditions of the client like ulcerative colitis, it is essential vomiting, to electrolyte monitoring, because the disease often order add reduces your appetite while components in the diet. maintain good nutrition increases your body’s energy ● needs. Additionally, common symptoms like diarrhea can reduce your body’s ability to absorb protein, carbohydrates, as well to Maintaining input-output, in different parental nutrition for the client. ● Maintenance of adequate hydration. fat, as water, vitamins, and minerals. Many people with ulcerative colitis find that soft, bland foods cause less discomfort than spicy or high-fiber foods. While your diet can remain flexible and should include a variety of foods from all food groups, your doctor will likely recommend restricting your 235 intake of dairy foods if you are found to be lactose-intolerant (crohn’scolitisfoundation.org, 2022). VII. SURGICAL MANAGEMENT PROCEDURE Proctocolectomy with Ileal Pouch-Anal Anastomosis (IPAA) RATIONALE NURSING RESPONSIBILITIES This procedure doesn't require PREOPERATIVE CARE a permanent surgery is stoma. also restorative This called a stool routine care and teaching ● Refer to an enterostomal the therapist for marking and anus. The colon and rectum are teaching about the stoma removed, location, ostomy care, and and through Provide preoperative proctocolectomy. The patient is still able to eliminate ● the small intestine is used to form an options internal pouch or reservoir -- appliances. It is important called a J-pouch -- that will to begin teaching prior to serve as a new rectum. This surgery pouch is connected to the anus. learning and acceptance of This procedure is frequently the done in two operations. In postoperatively. between the operations, you’d ● for to bowel (Khatri, 2022). ordered. facilitate ostomy Provide need a temporary ileostomy ostomy preoperative preparation as Cathartics, enemas, and preoperative Total Proctocolectomy This proctocolectomy surgical with End Ileostomy procedure removes the colon, rectum, and anus, and creates antibiotics are often ordered to reduce the risk of abdominal an end ileostomy so that waste can exit your body into an 236 ostomy bag. This procedure is contamination similar infection after surgery. to the temporary and ileostomy in the IPAA surgery, except the ileostomy will be POSTOPERATIVE CARE permanent (Surgery for ● Ulcerative Colitis, n.d.). Provide routine postoperative care and teaching continent ileostomy or Kock pouch is an option for people who would like their ● ileostomy over the stoma. Stool from converted to an internal pouch. an ileostomy is expressed It's also an option for people continuously or irregularly, who aren’t able to have IPAA. In and it is liquid in nature: this procedure, you’ll have a continuous use of a pouch stoma but no bag. The colon to collect the drainage is and rectum are removed, and an internal reservoir is created therefore necessary. ● from the small intestine. An opening abdominal is made wall, in the and the amounts of blood in the pouch are expected. A healthy inserts a catheter through the It preferred surgical treatment for (Khatri, 2022). appears result of mucus production. This procedure isn’t not the should protrude approximately 2 cm from has in the need for more surgery stoma pink or red and moist as a valve into the internal reservoir. uncertain results and may result for postoperative period, small drain the pouch, the patient It frequently and function. In the early skin with a nipple valve. To patients. Assess bleeding, stoma viability, reservoir is then joined to the ulcerative Apply an ostomy pouch the abdominal wall. ● Frequent assessment is particularly important in the initial postoperative period to ensure stoma Health and monitor for possible complications. A dusky 237 brown, black, or white stoma indicates circulatory compromise Other possible stoma complications include retraction (indentation or loss of the external portion of the stoma) or prolapse (outward telescoping of the stoma, that is, an abnormally long stoma). ● As the stoma starts to function, empty the pouch, explaining the procedure to the client. Initial drainage is dark green, viscid, and usually odorless. Drainage gradually thickens and becomes yellow brown. ● Empty the pouch when it is one-third full. Emptying the pouch when it is no more than one-third full helps prevent the skin seal from breaking as a result of the weight of the pouch. ● Measure drainage, and Include it as output on intake and output records. Rinse reapply the pouch the and clamp. Because of the potential for excess fluid loss through 238 ileostomy drainage, it is important to include it as fluid output. ● Assess the peristomal skin. Skin around the stoma should remain clean and pink and free of irritation,rashes inflammation, or excoriation. Skin complications may arise from appliance irritation or hypersensitivity, excoriation from a leaking appliance.or Candida albicans, a yeast infection. ● Protect peristomal skin from enzymes and bile salts in effluent. the Using ileostomy a skin barrier on the pouch is essential. Change the pouch if leakage occurs or if the client complains of burning or itching skin. Enzymes and bile salts normally reabsorbed in the large intestine are irritating to the skin. Excoriation of skin surrounding the stoma impairs the first line of defense against microorganisms and can 239 interfere with the ability to achieve a tight skin seal and prevent pouch leakage. ● Report the abnormal following assessment findings to the physician: a. Allergic or contact dermatitis. A rash may result from contact with fecal drainage or sensitivity to pouch, paste, tape, or sealant. b. Indicate Purulent ulcerated areas surrounding the stoma Disruption of the protective barrier of the skin allows bacterial entry. c. A red, bumpy, itchy rash or white-coated area.This is a manifestation of Candida albicans, a yeast infection. d. Buiging around the stoma. This finding may indicate herniation, caused by loops of intestine through the protruding abdominal wall. ● Apply protective ointments to the perirectal area of clients functioning with newly ileoanal 240 reservoirs and anastomoses. This helps protect the skin from the initial stools. As stools thicken and become fewer per day, the client experiences less perirectal irritation. VIII. NURSING MANAGEMENT Nursing Diagnosis Diarrhea related Goal Interventions to Within the 24 hours of nursing Independent: inflammation of the bowel as intervention, the patient will be evidenced urgency by to increased able defecate abdominal cramping. to and urgency exhibit to decreased defecate Rationale: Report decrease the patient the reason and specifically will be able to: a. 1. Explain thoroughly to behind the diarrhea Rationale: Promotes of cooperation from the client cramping b. Exhibit improved and understanding of the Inflammation causes the colon stool consistency from type 7 current situation to constrict and empty more to type 6 from bristol stool regularly, which is why scale 2. Provide a quiet patients may have diarrhea c. Consumes 1500 ml to 2000 environment for the and patient need to go bathroom frequently. to the ml of water d. Reports 2 ways on how to Rationale: To promote the lessen diarrhea health and patients well-being of improve the and patient’s perception of the healing environment 3. Examine for signs of diarrhea, such as 241 stomach cramps, discomfort, watery stools, frequency and urgency of stools Rationale: To monitor the bowel frequency 4. Encourage patients to drink more water Rationale: To avoid dehydration 5. Inform the patient to limit milk products, caffeinated beverages, alcohol and food heavy in fiber and fat Rationale: To ease intestinal cramps, diarrhea and encourage healthy eating habits 6. Monitor input and output of the patient Rationale: To assess and avoid dehydration 7. Monitor patient’s for the stool and characteristics Rationale: To detect for changes in 242 characteristic of the stool of the patient 8. Educate the patient on the need of disinfecting hands after bowel each movement Rationale: To decrease the spread of germs and pathogen transmission 9. Encourage the patient to enhance his or her potassium intake by eating more potassium rich food Rationale: To hypokalemia due potassium avoid to deficiency a 10. Weigh the patient daily and note for decreasing weight Rationale: To note and avoid severe water loss from the body Imbalanced than Body Nutrition: Less Within 3 days of nursing Requirement intervention the patient will be 1. Establish rapport. R: To easily gain cooperation related to altered absorption of able to present normal BMI to client. nutrients as evidenced by BMI and healthy physical status 2. Monitor Rationale: assess Ulcerative colitis can impact status I&O and hydration your body’s ability to properly 243 digest food and absorb R: to monitor the imbalances nutrients, which may lead to in fluids and serious vitamin deficiencies deficiencies based on the and malnutrition symptoms the identify client will present. Malnutrition and IBD. Crohn's & Colitis Foundation. (n.d.). 3. Weigh the patient daily Retrieved April 26, 2022, from R: serve as an initial https://www.cr o h n s c olitis assessment particularly in the fo u n d a tio n.o r g / di et-and- nutrition status of the patient. nutritio n/malnutrition -andibd#:~:txt=Crohn's%2 4. Administer IV therapy 0disease%20 and%20ulcer ative%20coliti s,serious%20 R: IV nutrition therapy is also vitamin%20d eficiencies%2 important if you have trouble 0and%20mal nutrition. as ordered with malabsorption 5. Increase OFI R: replacing fluid losses and correcting dehydration 6. Encourage ORS R: can replenish lost fluid, sugar and salt 7. Encourage and bedrest limited activity during acute phase of illness. R: Decreasing needs caloric aids in metabolic preventing depletion and conserves energy. 244 8. Recommend rest before meals. R: Quiets peristalsis and increases available energy for eating. 9. Provide oral hygiene. R: a clean mouth can enhance the taste of food. 10. Serve foods in wellventilated, pleasant surroundings, with unhurried atmosphere, congenial company. R: Pleasant environment aids in reducing stress and is more conducive to eating. 11. Avoid foods such as mil products, food high in fiber or fat, alcohol, caffeinated beverage chocolate, peppermint, tomatoes and orange juice. R: It abdominal can exacerbate cramping flatulence. and Individual tolerance varies, depending on stage of disease and area of bowel affected. 245 12. Encourage client to participate in dietary planning R: allows the patient to have a sense of control to food intake. 13. Encourage to eat low residue with high protein and high caloric diet. Food must be caffeine free, nonspicy and low fiber as indicated R: Protein is needed for wound healing. The diet of the patient is dependent on the severity of the disease. In most cases of mild Ulcerative colitis, patient is suggested to eat a low residue diet to improve the symptoms such as diarrhea. Impaired Skin Integrity Within 24 hours of nursing 1. Instruct in and (perianal) related to frequent interventions, the patient will encourage passage of loose stools as verbalize relaxation techniques, relief from evidenced by redness over discomfort and will have a such as and burning sensation over healthy intact skin. breathing, perianal area. CDs/tapes. use of focused imaging, R: To distract attention and Rationale: reduce tension/pain. One major manifestation of Ulcerative Colitis is the frequent passage of loose 246 stools or diarrhea. Due to 2. Administer analgesics diarrhea, the anal skin is as prescribed if pain is overhydrated making it more not tolerable. at risk for friction and shearing R: To provide comfort and forces. relief from pain. Moreover, makes the it skin also more permeable to chemicals and pathogens. Furthermore, diarrhea also can cause tenesmus which contributes to 3. Administer a warm sitz bath as ordered. R: To prevent excoriation and provide comfort. the tearing of the anal area. With this, the skin may be 4. Provide perianal care inflamed and thus causes a every after each loose burning sensation. With this, stool motion, keeping it the skin may be inflamed and clean and dry. thus causes a burning sensation. R: To cleanse the skin and protect it from injury. 5. Apply moisture barrier Rudd, A. (2019). Can diarrhea such as petroleum jelly cause impaired skin integrity. or medicated ointment Retrieved April 25, 2022 from as https://www.nbcco perianal medyplayground. diarrheakin-integ com/can- cause-impaired-s ordered to area the after cleaning R: To protect perianal skin from contact with liquid stools. 6. Adjust the temperature of the room to avoid humidity R: To prevent further irritation as humidity aggravates the irritation. 247 7. Adjust the patient’s position when sitting within 2-3 hour intervals. R: To prevent further discomfort. 8. Encourage the patient to increase oral fluid intake of at least 1500 ml to 2000 ml of fluid. R: To replenish fluid losses from diarrhea and prevent dehydration and further skin breakdown. 9. Perform regular hydration rounds. R: To monitor the hydration status and look out for signs of dehydration which may contribute to the impairment of skin integrity. IX. LITERATURE Ulcerative Colitis Narrative Global Survey Findings: The Impact of Living With Ulcerative Colitis—Patients’ and Physicians’ View U.S. National Library of Medicine. (n.d.). Ulcerative colitis narrative global survey findings: The impact of living with ulcerative colitis-patients' and physicians' view. Inflammatory bowel diseases. Retrieved February 15, 2023, from https://pubmed.ncbi.nlm.nih.gov/33529314/ 248 More than half of ulcerative colitis (UC) patients claim that it took longer than a year between their initial symptoms and diagnosis. The patient may become frustrated and anxious if the diagnosis of UC is delayed, which could also have a negative impact on the patient-physician relationship. Delayed diagnosis can result in difficulties, such as an increased risk of intestinal surgery due to UC, and delayed commencement of UC therapy. Only 37% of people report that their overall health is excellent or good, which may indicate that patients have low expectations for their condition's treatment. The findings imply that UC management conversations require more time. Many people with ulcerative colitis (UC) worry about infertility and are worried about passing the condition on to their offspring. The impact of UC on patients' professional lives is significant, and many report absenteeism from work as well as a decline in confidence at work as a result. It is important to note that rather than experiencing actual UC symptoms, patients in Europe and Japan reported missing work due to concern over the symptoms. The results of this global survey show that people with UC have poor illness control, delayed diagnosis, and unfavorable effects on their quality of life. Patients claim that having UC is mentally taxing, although emotional and mental health problems are rarely discussed during periodic checkups. Demographic profile and clinical presentation of IBD among inpatients: a UERMMMC experience Gomes TNF;de Azevedo FS;Argollo M;Miszputen SJ;Ambrogini O; (n.d.). Clinical and demographic profile of inflammatory bowel disease patients in a reference center of São Paulo, Brazil. Clinical and experimental gastroenterology. Retrieved February 15, 2023, from https://pubmed.ncbi.nlm.nih.gov/33762838/ In the past, the Philippines had only a small amount of clinical and demographic data on inflammatory bowel disease. At the University of the Eastern Ramon Magsaysay Memorial Medical Center in the Philippines, IBD diagnoses have increased during the previous six years. This article's goal is to present clinical and demographic information about IBD among patients seen at our hospital. There were 24 patients in total with an IBD diagnosis. 15 patients (62.5%) have Crohn's disease, and 9 (37.5%) have ulcerative colitis. Over the past two years, 5–6 new cases have been diagnosed, with an average of 2-3 people being diagnosed each year. Three new instances were 249 reported on average each year, with more men than girls (19 vs. 5). The age at presentation had a bimodal peak between individuals between the ages of 21 and 40, with the mean age being 40. Diarrhea (58.3%), abdominal pain (20.8%), lower GI hemorrhage (12.5%), and recurrent perianal fistula (8.3%) were common symptoms. Two cases were initially negative. One instance had HIV and MTB co-infections, while the other two just had a biopsy that suggested Crohn's disease. Esophageal fistula was present in one patient. Ninety percent of UC cases had rectosigmoid colitis, and ten percent had pancolitis. 60 percent of CD patients had pure colitis, 35 percent had ileo-colitis, and 5 percent had terminal ileitis. Inflammatory Bowel Disease: An emerging problem in the Philippines Garcia, L., & Ypil, G. (2021, August 31). Inflammatory bowel disease: An emerging problem in the Philippines. Philippine Journal of Internal Medicine. Retrieved February 15, 2023, from https://www.herdin.ph/index.php?view=research&cid=18595 Filipinos from the Visayas and Mindanao regions were found to have six documented cases of inflammatory bowel disease, including two cases of Crohn's disease and four cases of ulcerative colitis. There were 5 women and 1 man, with a mean age of 42. The most common clinical symptoms included abdominal discomfort, rectal bleeding, diarrhea, fever, and cramps. One Crohn's disease patient experienced arthritis, a subcutaneous nodule, erythema nodosum, and erythema multiforme, whereas three ulcerative colitis patients experienced arthralgia and petechial skin abnormalities. In the course of the disease's active stage, the ESR of every patient was high. All responded well to steroids, but only patients with ulcerative colitis responded well to sulfasalazine. Repeated treatment with anti-amoebic drugs for the mistaken diagnosis of amoebic colitis delayed the correct diagnosis in all four patients with ulcerative colitis. Both patients with Crohn's disease received prolonged treatment for intestinal tuberculosis before the correct diagnosis was made. Inflammatory bowel disease should now be included in the differential diagnosis of Filipino patients with amoebic colitis and intestinal tuberculosis who do not respond readily to conservative treatment. HEMORRHOIDS I. DEFINITION 250 Hemorrhoids are swollen blood vessels in the lower rectum. They are among the most common causes of anal pathology, and subsequently are blamed for virtually any anorectal complaint by patients and medical professionals alike, Confusion often arises because the term "hemorrhoid" has pathologic structures. the context of this article. "hemorrhoids" refers to pathology. been presentation used to refer to hemorrhoidal both normal venous anatomic cushions; structures and Hemorrhoidal venous cushions are normal structures of the anorectum and are anatomically present unless a previous intervention has taken place Because of their rich vascular supply., highly sensitive location, and tendency to engorge and prolapse, hemorrhoidal venous cushions are common causes of anal pathology. Symptoms can range from mildly bothersome, such as pruritus, to quite concerning. such as rectal bleeding. Although hemorrhoids are a common condition diagnosed in clinical practice, many patients are too embarrassed to seek treatment. Consequently, the true prevalence of pathologic hemorrhoids is not known. In addition, although hemorrhoids are responsible for a large portion of anorectal complaints, it is important to rule out more serious conditions, such as other causes of gastrointestinal (GI) bleeding, before reflexively attributing symptoms to hemorrhoids. II. ANATOMY/ PHYSIOLOGY Hemorrhoids are highly vascular submucosal cushions that typically occur in three columns in the anal canal: left lateral, right anterior, and right posterior. These vascular cushions are formed of elastic connective tissue and smooth muscle, but because some lack muscular walls, they may be classified as sinusoids rather than arteries or veins. Clinically visible bleeding is caused by perisinusoidal arterioles and is thus arterial in character. Hemorrhoids protect the anal sphincter muscles and augment closure of the anal canal during moments of elevated abdominal pressure (e.g., coughing, sneezing) to prevent incontinence, contributing 15 to 20% of the resting anal canal pressure. Abdominal pressure increases the pressure in the inferior vena 251 cava, causing these vascular cushions to engorge and prevent leaking. This tissue is also suggested to aid in the separation of stool, liquid, and gas in the anal canal. The dentate line distinguishes between exterior and internal hemorrhoids. External hemorrhoids are positioned below the dentate line and drain into the pudendal vessels, which then drain into the internal iliac vein via the inferior rectal veins. These vessels are protected by anoderm, which is made out of modified squamous epithelium. As a result, pain fibers are present in various tissues, influencing how patients present and are treated. Internal hemorrhoids are located above the dentate line and are surrounded by columnar cells with visceral innervation. They drain into the internal iliac arteries via the middle rectal veins. Internal hemorrhoids are further characterized based on the degree of prolapse. Hemorrhoids of the first degree extend into the anal canal but do not prolapse out of it. Second-degree hemorrhoids prolapse outside of the canal, but reduce spontaneously. Third-degree hemorrhoids prolapse out of the canal and require manual reduction; fourth-degree hemorrhoids are irreducible. III. SIGNS AND SYMPTOMS Signs and Symptoms Rationale Rectal Bleeding Straining or passing a particularly hard stool can damage the surface of a hemorrhoid, causing it to bleed. Blood from a hemorrhoid will look bright red on a piece of toilet paper. Internal, external, and thrombosed hemorrhoids can all bleed. Painful Swelling The veins around your anus tend to stretch under pressure and may bulge or swell. Hemorrhoids can develop from increased pressure in the lower rectum due to: Straining during bowel movements. Pruritus The most common cause of occasional anal itching (pruritus ani) is a fungus/yeast infection. Enlarged hemorrhoids cause the leakage of moisture, stool, 252 and fungus. Repeated wiping, cleaning, scratching, and the use of harsh cleaners make the itching worse. Painless rectal bleeding Internal hemorrhoids lie inside the rectum. You usually can't see or feel them, and they rarely cause discomfort. But straining or irritation when passing stool can cause: Painless bleeding during bowel movements. IV. ETIOLOGY Predisposing factors Rationale Family History Genetics can influence the condition of the muscles and cartilage. In some families, these structures have a higher chance of weakening over time. The genes for weakened colorectal muscles and connective tissue may run in your family if you have a history of hemorrhoids (Chandler, 2021). Age Hemorrhoids are most common between ages 45 and 65, however it’s not unusual to see them in younger adults as well. According to the NIDDK, as people age, the connective tissue between the anus and rectum weakens, making them more susceptible to hemorrhoids (Theobald, 2023). Precipitating factors Rationale Constipation Spending much time in the toilet puts extreme pressure on your anus and rectum. While in the washroom, your rectum gets lower than the rest of your buttocks; hence gravity pulls down the blood 253 pools in the veins. If you are already suffering from constipation, you increase this pressure further (Mayo Clinic 2021). Diarrhea When someone has diarrhea, they are frequently forced to sit on the toilet for a long time or they could strain more than normal. Hemorrhoids may be brought on by prolonged sitting down as well as the strain from diarrhea (Saks, 2022). Obesity Hemorrhoids are more prevalent in the overweight population for various reasons, including insufficient fiber consumption, a decline in physical activity, and prolonged sitting (Obesity Action Coalition 2023). Pregnancy Although hemorrhoids can arise anytime, most pregnant women get them in the third trimester, starting around week 28. The veins in the anus may bulge due to increased blood supply to the pelvic region, pressure from the expanding uterus, and the growing fetus (HonorHealth 2023). Sitting or Standing for a Prolonged Hemorrhoids develop while sitting because the Time pressure causes the gluteal muscles to spread out. The small rectum and anal veins stretch out and lose flexibility. As the veins which have become brittle swell up with blood, hemorrhoids occur (FLEXISPOT 2022). Frequent Heavy Lifting When lifting heavy weights, people commonly strain and hold their breath. Thus, the internal organs will be put under more pressure while holding breath and grunting, which will cause the veins surrounding your rectum to grow into hemorrhoids (Perryman, 2023). V. PATHOPHYSIOLOGY 254 Narrative: 255 Several factors may affect the formation of hemorrhoids. Hereditary bowel/rectal problems, advanced age, and other factors may also cause the development of hemorrhoids, such as increased intra-abdominal pressure (e.g., pregnancy, constipation, diarhhea, chronic straining, lifting). This may cause the weakening of the anal cushion and the supporting tissue and spasms of the internal sphincter. It might also prevent venous return, which would enlarge the hemorrhoidal plexus and the arteriovenous anastomoses of the anorectal junction, resulting in hemorrhoids (Kibret et al., 2021). External hemorrhoids occur since hemorrhoidal venous cushions have a rich vascular supply, highly sensitive location, and can engorge and prolapse along the anal canal. This leads to inflammation of the vascular wall and connective tissues. Thrombosed hemorrhoids will then develop since the inflammation will lead to a blood clot forming inside a hemorrhoidal vein, obstructing blood flow and causing painful swelling of the perianal tissues. Thrombosed hemorrhoids can also cause rectal bleeding if they become ulcerated (Castillo, 2022). Moreover, enlarged internal hemorrhoids cause the majority of symptoms. Abnormal swelling of the anal cushions provokes dilatation and engorgement of the arteriovenous plexuses. This will then lead to stretching the suspensory muscles and eventual prolapse of rectal tissue through the anal canal, and the engorged anal mucosa is easily traumatized, leading to rectal bleeding that is typically bright red due to high blood oxygen content within the arteriovenous anastomoses. Prolapse leads to soiling and mucus discharge (triggering pruritus) and predisposes to incarceration and strangulation. There are different degrees of internal hemorrhoids. First-degree internal hemorrhoids bulge into the anal canal during bowel movements. A second-degree internal hemorrhoid bulges from the anus during bowel movements before returning inside on its own. In comparison, a thirddegree hemorrhoid protrudes from the anus and needs to be pulled back with a finger during bowel movements. A constant protrusion from the anus is a fourth-degree hemorrhoid. Moreover, hemorrhoids can be treated depending on their type and severity. If provided with appropriate treatments and there will be elimination or removal of hemorrhoids, it will result in a good prognosis. But if left ignored and untreated long enough, the prolapsing will continue, leading to blood loss, severe pain, & infection related to the disease resulting in poor prognosis (Itriago, 2022). VI. MEDICAL MANAGEMENT A. DIAGNOSTIC EXAMS 256 TEST RATIONALE NURSING RESPONSIBILITIES Digital Rectal Exam A digital rectal exam, or DRE, is a medical test that checks 1. Explain the patient on for the procedure. abnormalities in the rectum, anus R: to promote cooperation and and prostate gland. a healthcare inform the procedure for provider will put on gloves and proper understanding. apply lubricant before gently sliding their index finger into the rectum. (Cleveland Clinic, n.d) 2. Ask you to lie down on your left side, with your knees Anoscopy Anoscopy is an examination of the anal canal and rectum with an anoscope to help diagnose anal lifted up towards your chest. R: This is the easiest position to examine your rectum. and rectal conditions. An anoscope is a small-diameter plastic or metal hollow tube (slightly wider than a finger) with an insert called an obturator. The device is about 5 3. Wear gloves during the procedure. R: to avoid acquiring bacterias from the rectum. inches long. After inserting the anoscope into the anal canal, the doctor removes the obturator insert and is able to see inside the rectum. By shining a light through the tube, the doctor can get a look at the lining of the anal canal and lower 4. Put some lubricating gel on 1 finger and gently slide it into your rectum. R: this is to avoid irritating the rectal tissue. rectum. (John Hopkins Medicine, 2023) Sigmoidoscopy A flexible sigmoidoscopy 5. Inform the patient to is an the result of the test. exam used to evaluate the lower part of the large intestine (colon). During a flexible sigmoidoscopy 257 exam, a thin, flexible tube (sigmoidoscope) is inserted into the rectum. (John Hopkins Medicine, 2023) B. MEDS 1. Analgesic - Analgesics, commonly known as painkillers, are drugs that treat a variety of pain, such as headaches, injuries, and arthritis. Both opioid analgesics and antiinflammatory analgesics alter how the brain interprets pain. While certain analgesics can be purchased without a prescription, others need one. 2. Antipyretic - Antipyretics do not affect body temperature in the afebrile state, but they can prevent or reverse the cytokine-mediated rise in core temperature that occurs with fever. These should be separated from hypothermia agents, or cryogens, which can lower core temperatures even when a person is not febrile. GENERIC NAME Acetaminophen BRAND NAME Tylenol DRUG CLASSIFICATION Pharmacotherapeutic: Central Analgesic Clinical: Non Narcotic analgesic, Antipyretic SUGGESTED DOSE Dosage Considerations Analgesia and Fever Maximum dose ● Acetaminophen containing products: Not to exceed a cumulative dose of 3.25 g/day of acetaminophen; under 258 supervision of healthcare professional, daily doses of up to 4 g/day may be used ● Tylenol Extra-Strength (i.e., 500 mg/tab or cap): Not to exceed 3 g/day (6 tabs or caps); under supervision of a healthcare professional, daily doses of up to 4 g/day may be used Renal Impairment ● Longer dosing intervals and the reduced total dose may be warranted in patients with severe renal impairment (CrCl less than or equal to 30 mL/min)= Hepatic Impairment ● Use caution with any type of liver disease. Pediatric Pain & Fever Relief Weight-based dosing ● Children under 12 years: 10-15 mg/kg/dose taken orally once every 4-6 hours; not to exceed 5 doses in 24 hours Fixed dosing ● Children under 6 years: Ask a healthcare provider ● Children 6-12 years: 325 mg orally once every 4-6 hours; not to exceed 1.625 g/day for not more than 5 days unless directed by a healthcare provider ● Children under 12 years and older: ○ Regular strength: 650 mg once every 4-6 hours; not to exceed 3.25 g in 24 hours; under supervision of healthcare professional, doses of up to 4 g/day may be used ○ Extra strength: 1000 mg once every 6 hours; not to exceed 3 g in 24 hours; under supervision of healthcare professional, doses of up to 4 g/day may be used ○ Extended-release: 1.3 g once every 8 hours; not to exceed 3.9 g in 24 hours 259 ROUTE OF PO, IV, Rectal ADMINISTRATION MODE OF ACTION Analgesic: Activates descending serotonergic inhibitory pathways in CNS. Antipyretic: Inhibits hypothalamic heat-regulating centre. Therapeutic Effect: Results in antipyresis. Produces analgesic effect. INDICATION Acetaminophen (APAP) is a non-opioid analgesic and antipyretic agent used to treat pain and fever. Clinicians can use it for their patients as a single agent for mild to moderate pain and in combination with an opioid analgesic for severe pain. CONTRAINDICATION Contraindications to using acetaminophen include hypersensitivity to acetaminophen, severe hepatic impairment, or severe active hepatic disease. However, there is a general debate among experts as to whether hepatic impairment is truly a limiting factor, as it would likely be associated with decreased production of the toxic metabolite, N-acetyl-p- benzoquinoneimine (NAPQI). SIDE EFFECTS Rare: Hypersensitivity reaction ADVERSE EFFECTS Early Signs of Acetaminophen Toxicity: ● Anorexia, nausea, diaphoresis, fatigue within the first 12–24 hrs. Later Signs of Toxicity: ● Vomiting, right upper quadrant tenderness, elevated LFTs within 48–72 hrs after ingestion. Antidote: Acetylcysteine. DRUG INTERACTIONS DRUG: Alcohol (chronic use), hepatotoxic medications (e.g., phenytoin), hepatic enzyme inducers (e.g., phenytoin, rifAMPin) may increase risk of hepatotoxicity with prolonged high dose or single toxic dose. Dasatinib, probenecid may increase 260 concentration/effect. HERBAL: None significant. FOOD: Food may decrease the rate of absorption. LAB VALUES: May increase serum ALT, AST, bilirubin; prothrombin levels (may indicate hepatotoxicity). NURSING RESPONSIBILITIES 1. Instruct patients to never take more than 4,000 mg of acetaminophen per 24 hours. This includes all forms of acetaminophen and acetaminophen-containing products. R: Taking too much acetaminophen can damage the liver, sometimes leading to a liver transplant or death. 2. Do not take acetaminophen with alcohol due to the risk of liver toxicity. R: Mixing too much alcohol with any acetaminophen (or too much acetaminophen with any alcohol) can make removal of this substance even more difficult. The excess substance attacks your liver. This can cause severe liver damage. 3. Educate that acetaminophen can increase anticoagulant effects. Teach the patient to monitor for bruising and signs of bleeding, and to prevent the risk of injury. R: If the patient is taking warfarin, acetaminophen can increase the risk of bleeding. 4. Acetaminophen may not be safe for children under the age of 2. Always discuss with a healthcare provider first. Acetaminophen comes in preparations and doses for children such as Children’s Tylenol liquid. Always use the appropriate dropper or measuring cup provided when administering to children. 261 R: It may cause long-term neurodevelopmental problems. 5. Store at room temperature. Suppositories should be stored in the refrigerator. R: Some medications in suppository form need to be stored in the refrigerator so that they do not melt before use. 6. Assess overall health status and alcohol usage before administering acetaminophen. R: Patients who are malnourished or chronically abuse alcohol are at higher risk of developing hepatotoxicity with chronic use of usual doses of this drug. 7. Monitor the patient’s response to the medication. R: To ensure that the medication is effectively managing the patient’s pain and to make any necessary adjustments to the dosage or treatment plan. 8. Assess the patient’s allergies and previous reactions to medications before administering acetaminophen. R: The patient’s allergies and previous reactions to medications are important things to consider to avoid potential allergic reactions. Acetaminophen may cause Stevens-Johnson syndrome. 9. Assess fever; note the presence of associated signs (diaphoresis, tachycardia, and malaise). R: Assessing a patient’s fever is an important nursing consideration when administering acetaminophen. Fever is a common symptom of many illnesses and can be an indicator of an underlying infection or condition. 10. Monitor patients with liver or kidney dysfunction for potential adverse effects and adjust the dosage 262 accordingly. R: Individuals with liver or kidney disease should be extra careful when taking acetaminophen, as it is metabolized by the liver and excreted by the kidneys. 3. Non-steroidal anti-inflammatory drug NSAIDs block the body from producing specific molecules that lead to inflammation. NSAIDs are effective at treating pain brought on by gradual tissue deterioration, including arthritis pain. NSAIDs are effective in treating headaches, menstrual cramps, and back discomfort. GENERIC NAME Acetylsalicylic acid BRAND NAME Aspirin DRUG CLASSIFICATION Pharmacotherapeutic: Non-steroidal anti-inflammatory drug (NSAID) Clinical: Anti-inflammatory, antipyretic, analgesic, anti-platelet SUGGESTED DOSE Analgesia, Fever PO: ADULTS, ELDERLY, CHILDREN 12 YRS AND OLDER AND WEIGHING 50 KG OR MORE: 325–650 mg q4–6h or 975 mg q6h prn or 500–1,000 mg q4–6h prn. Maximum: 4 g/day. RECTAL: 300– 600 mg q4h prn. INFANTS, CHILDREN WEIGHING LESS THAN 50 KG: 10–15 mg/kg/dose q4–6h. Maximum: 4 g/day or 90 mg/kg/day. Revascularization PO: ADULTS, ELDERLY: 80–325 mg/day. Kawasaki’s Disease PO: CHILDREN: 80–100 mg/kg/day in divided doses q6h up to 14 days (until fever resolves for at least 48 hrs). After fever resolves, 1–5 mg/kg once daily for at least 6–8 wks. 263 MI, Stroke (Risk Reduction) PO: ADULTS, ELDERLY:(Durlaza): 162.5 mg once daily. Dosage in Renal/Hepatic Impairment Avoid use in severe impairment. ROUTE OF PO, Rectal ADMINISTRATION MODE OF ACTION Irreversibly inhibits cyclo-oxygenase enzymes, resulting in a decreased formation of prostaglandin precursors. Irreversibly inhibits formation of thromboxane, resulting in inhibiting platelet aggregation. Therapeutic Effect: Reduces inflammatory response, intensity of pain; decreases fever; inhibits platelet aggregation. INDICATION Aspirin is indicated for temporary relief of headache, pain and fever of colds, minor pain of arthritis, muscle pain, menstrual pain, and toothache. CONTRAINDICATION Aspirin is contraindicated in patients with known allergy to NSAIDs and in patients with asthma, rhinitis, and nasal polyps. It may cause anaphylaxis, laryngeal edema, severe urticaria, angioedema, or bronchospasm (asthma). SIDE EFFECTS Occasional: GI distress (including abdominal distention, cramping, heartburn, mild nausea); allergic reaction (including bronchospasm, pruritus, urticaria). ADVERSE EFFECTS High doses of aspirin may produce GI bleeding and/or gastric mucosal lesions. Dehydrated, febrile children may experience aspirin toxicity quickly. Reye’s syndrome, characterized by persistent vomiting, signs of brain dysfunction, may occur in children taking aspirin with recent viral infection (chickenpox, 264 common cold, or flu). Low-grade aspirin toxicity characterized by tinnitus, generalized pruritus (may be severe), headache, dizziness, flushing, tachycardia, hyperventilation, diaphoresis, thirst. Marked toxicity characterized by hyperthermia, restlessness, seizures, abnormal breathing patterns, respiratory failure, coma. DRUG INTERACTIONS Aspirin may decrease the effect of angiotensin-converting enzyme (ACE) inhibitors, diuretics, beta-blockers, and uricosurics (probenecid and sulfinpyrazone); increase the toxicity of acetazolamide and methotrexate; prolong prothrombin time and bleeding time in patients taking warfarin; increase the anticoagulant activity of heparin; lower phenytoin blood levels; raise valproic acid serum levels; and increase the efficacy of oral hypo-glycemics to the point that the patient may experience hypoglycemia. If given concurrently with other nonsteroidal anti-inflammatory drugs (NSAIDs), aspirin can increase bleeding or reduce renal function. NURSING RESPONSIBILITIES 1. Instruct patient to be aware that aspirin can prolong bleeding time. R: Note that aspirin prolongs the bleeding time for 4 – 7 days and, in large doses, may cause prolonged prothrombin time. A prolonged PT means that the blood is taking too long to form a clot. Aspirin alters platelet function through interference with prostaglandin biosynthesis. 2. Evaluate the patient's lifestyle. R: Determine patient’s alcohol use, tobacco use, and diet, which may impact the effectiveness and safety of aspirin therapy. 3. Review patient’s history for GI bleeding and ulceration. R: Review the patient’s health history, including any previous gastrointestinal bleeding or ulceration, liver or kidney disease, 265 or bleeding disorders. 4. Assess patient’s allergy to aspirin. R: Ask about any allergies or intolerances the patient may have to aspirin. Patients who have asthma, allergies, and nasal polyps or who are allergic to tartrazine are at an increased risk for developing hypersensitivity reactions. 5. Determine current aspirin regimen. R: Assess the patient’s current aspirin regimen, including the dose, frequency, and route of administration. 6. Assess pain and limitation of movement. R: Determine type, location, and intensity before and at the peak after administration. 7. Assess fever and note associated signs. R: Manifestations such as diaphoresis, tachycardia, malaise, and chills should be documented for baseline data and to determine effectiveness of therapy. 8. Monitor hepatic function. R: May cause increased serum AST, ALT, and alkaline phosphatase, especially when plasma concentrations exceed 25 mg/100 mL. May return to normal despite continued use or dose reduction. If severe abnormalities or active liver disease occurs, discontinue and use with caution in the future. 9. Monitor serum salicylate levels periodically. R: Especially with prolonged high-dose aspirin therapy to determine dose, safety, and efficacy, especially in children with Kawasaki disease. 10. Instruct patient to be aware that aspirin can alter results 266 of some lab tests. R: Note that aspirin may alter the results of serum uric acid, urine vanillylmandelic acid (VMA), protirelin-induced thyroidstimulating hormone (TSH), urine hydroxy indole acetic acid (5HIAA) determinations, and radionuclide thyroid imaging. 11. Monitor for signs of toxicity and overdose. R: Monitor for the onset of fever, tinnitus, headache, drowsiness, hyperventilation, agitation, mental confusion, lethargy, diarrhea, and sweating. If these symptoms appear, withhold medication and notify a healthcare professional immediately. 4. Corticosteroid Steroids function by suppressing immune system activity and reducing inflammation. White blood cells and other molecules in the body can fight infection and foreign agents like bacteria and viruses during the process of inflammation. The immune system, the body's defense mechanism, however, malfunctions in several diseases. Inflammation could then start to damage the body's tissues as a result. GENERIC NAME Hydrocortisone BRAND NAME Anusol HC DRUG CLASSIFICATION Pharmacotherapeutic: Corticosteroid 267 Clinical: Glucocorticoid SUGGESTED DOSE Acute Adrenal Insufficiency IV: ADULTS, ELDERLY: 100 mg IV bolus, then 25–75 mg q6h for 24 hrs (or 200 mg/24h as continuous infusion), then taper slowly. INFANTS, CHILDREN, ADOLESCENTS: 50–100 mg/m2 once, then 50–100 mg/m2/day in 4 divided doses. Anti-inflammation, Immunosuppression IV, IM: ADULTS, ELDERLY: 100–500 mg/dose at intervals of 2 hrs, 4 hrs, or 6 hrs. CHILDREN: 1–5 mg/kg/day in divided doses q12h. PO: ADULTS, ELDERLY: 20–240 mg q12h. CHILDREN: 2.5–10 mg/kg/day in divided doses q6–8h. Adjunctive Treatment of Ulcerative Colitis Rectal: (Enema): ADULTS, ELDERLY: 100mg at bedtime for 21 nights or until clinical and proctologic remission occurs (may require 2–3 mos of therapy). (Rectal Foam): ADULTS, ELDERLY: 1 applicator 1–2 times/day for 2–3 wks, then every second day until therapy ends. Usual Topical Dose ADULTS, ELDERLY: Apply sparingly 2–4 times/day. Dosage in Renal/Hepatic Impairment No dose adjustment. ROUTE OF IV, IM, Rectal, PO ADMINISTRATION MODE OF ACTION Inhibits accumulation of inflammatory cells at inflammation 268 sites, phagocytosis, lysosomal enzyme release, synthesis and/ or release of mediators of inflammation. Reverses increased capillary permeability. Therapeutic Effect: Prevents/suppresses cell-mediated immune reactions. Decreases/prevents tissue response to inflammatory processes. INDICATION Topical corticosteroids are indicated for the relief of the inflammatory and pruritic manifestations of corticosteroidresponsive dermatoses. CONTRAINDICATION Topical corticosteroids are contraindicated in those patients with a history of hypersensitivity to any of the components of the preparation. SIDE EFFECTS Frequent: Insomnia, heartburn, anxiety, abdominal distention, diaphoresis, acne, mood swings, increased appetite, facial flushing, delayed wound healing, increased susceptibility to infection, diarrhea or constipation. Occasional: Headache, edema, change in skin color, frequent urination. Topical: Pruritus, redness, irritation. Rare: Tachycardia, allergic reaction (rash, hives), psychological changes, hallucinations, depression. Topical: Allergic contact dermatitis, purpura. Systemic: Absorption more likely with use of occlusive dressings or extensive application in young children. ADVERSE EFFECTS Long-term therapy: Hypocalcemia, hypokalemia, muscle wasting (esp. arms, legs), osteoporosis, spontaneous fractures, amenorrhea, cataracts, glaucoma, peptic ulcer, HF. Abrupt withdrawal after long-term therapy: Nausea, fever, headache, sudden severe joint pain, rebound inflammation, fatigue, weakness, lethargy, dizziness, orthostatic hypotension. 269 DRUG INTERACTIONS DRUG: May increase hypokalemic effects of diuretics (e.g., furosemide). CYP3A4 inducers (e.g., carBAMazepine, phenytoin, rifAMPin) may decrease effects. Live virus vaccines may decrease pt’s antibody response to vaccine, increase vaccine side effects, potentiate virus replication. May decrease therapeutic effect of aldesleukin, BCG (intravesical). May increase the hyponatremic effect of desmopressin. HERBAL: St. John’s wort may decrease concentration. Echinacea may decrease therapeutic effect. FOOD: None known. LAB VALUES: May increase serum glucose, lipids, sodium. May decrease serum calcium, potassium, thyroxine; WBC count. NURSING RESPONSIBILITIES 1. Instruct patient to avoid contact with people who have infections that may spread to others (such as chickenpox, measles, flu). R: Rarely, this drug can make you more likely to get infections or may worsen any current infections. 2. Do not abruptly discontinue taking the drug. R: Doses are gradually reduced to prevent withdrawal symptoms. 3. Do not give IM injections if the patient has thrombocytopenic purpura. R: Intramuscular injection is avoided due to the possibility of causing bleeding into the skin. 4. Instruct to avoid alcohol and caffeine. 270 R: To decrease the risk of stomach/intestinal bleeding. 5. Before having surgery or emergency treatment, or the patient gets injured, instruct the patient to tell the doctor that they are using the medication. R: Rarely, using corticosteroid medications for a long time can make it more difficult for your body to respond to physical stress. 6. If the patient is still growing, advise the guardian to see a doctor regularly to check the child's height. R: Though it is unlikely, this medication may temporarily slow down a child's growth if used for a long time. 7. During pregnancy, this medication should be used only when clearly needed and not for prolonged periods. R: Other forms of hydrocortisone (given by mouth or by injection) may harm an unborn baby. Discuss the risks and benefits with your doctor. 8. Use minimal doses for minimal duration. R: To minimize adverse effects. 9. Instruct patient to get medical help right away if you notice any symptoms of a serious allergic reaction, including: rash, itching/swelling (especially of the face/tongue/throat), severe dizziness, trouble breathing. R: A very serious allergic reaction to this drug is rare. 10. Before using hydrocortisone, tell your doctor or pharmacist if you are allergic to it; or to other corticosteroids (such as prednisone); or if you have any other allergies. R: This product may contain inactive ingredients, which can 271 cause allergic reactions or other problems. Talk to your pharmacist for more details. C. TREATMENT THERAPY RATIONALE NURSING RESPONSIBILITIES Medications Your doctor might advise over- ● Administration includes the-counter creams, ointments, ensuring suppositories, or pads if your medication hemorrhoids only cause mild drawn up in the correct discomfort. These lotions have dose, and administered at chemicals including witch hazel, the right time through the hydrocortisone, and lidocaine that right route to the right help reduce itching and pain patient. momentarily. If not prescribed by ● that the is right properly To limit or reduce the risk a doctor, avoid using an over-the- of administration errors, counter steroid cream for longer many hospitals employ a than a week because it can thin single-dose system. your skin. (Hemorrhoids - ● The client should be Diagnosis and Treatment - Mayo educated about the safe Clinic, 2021). and correct method of self administration of medications. In addition to the education discussed immediately above, some clients may also have to be instructed about special procedures like the proper use of an inhaler, taking insulin, giving mixing insulins, oneself an intramuscular injection or 272 self-administering tube feedings. ● Educate client about medications ● Dispose of unused medications according to facility/agency policy Home Remedies You can often relieve the mild ● Advise patient that some pain, swelling and inflammation of home remedies may help hemorrhoids alleviate with home treatments. short-term symptoms, but they won't treat an underlying illness. ● Consume fiber-rich meals. It's Consume address your symptoms more whole grains, fruits, and veggies. By doing this, the stool will important that you and pain with your doctor. ● Inform patient that there is become softer and more no guarantee of safety for bulk, preventing you from doing home remedies. straining, which can make the symptoms existing of pre- hemorrhoids worse. To avoid issues with gas, progressively incorporate more fiber into your diet. ● Apply topical remedies. Use pads with witch hazel or a numbing ingredient, or apply an over-the- counter hemorrhoid cream or suppository with hydrocortisone. 273 ● Regularly take sitz baths or warm baths. Take a 10to 15-minute bath in plain, warm water twice or three times daily to treat your anal area. The toilet may fit over a sitz bath. ● Take oral pain relievers. To temporarily ease your discomfort, you can take acetaminophen (Tylenol, among others), aspirin, or ibuprofen (Advil, Motrin IB, among others). (Hemorrhoids - Diagnosis and Treatment - Mayo Clinic, 2021). Surgical Therapy Only a small percentage of people Before the with hemorrhoids require surgery. Procedure/Examination: However, if other procedures haven't been successful or you ● Assess patient for the have large hemorrhoids, your presence of hemorrhoids, doctor might recommend one of discomfort the following: associated or hemorrhoids, ● Hemorrhoidectomy - thorough and with diet, fluid intake, and presence of Hemorrhoidectomy is the most pain constipation. ● Instruct patient and/or effective method of family regarding causes of treating severe or hemorrhoids, methods of recurrent hemorrhoids. avoiding hemorrhoids, and Urinary tract infections 274 can occur as a result of treatments that can be temporary performed. problems emptying your ● ● Instruct patient This side effect generally family regarding follows spinal anesthesia. procedures required. Hemorrhoid bladder. stapling - ● Instruct patient and/or all and/or Stapled hemorrhoidopexy, family in comfort measures also known as hemorrhoid to use with the presence of stapling, prevents blood hemorrhoids. from reaching hemorrhoidal tissue. During the Usually, it is exclusively Procedure/Examination: applied to internal ● Note for the time the hemorrhoids. surgery and the general Hemorrhoidectomy anesthesia started. typically causes more ● discomfort than stapling, Ensure the IV fluids given to the patient. which enables a sooner return to normal activities. After the Nevertheless, stapling has Procedure/Examination: been linked to a higher incidence of recurrence ● and rectal prolapse, in which a portion of the Monitor the patient closely in the recovery room. ● IV fluid should be rectum protrudes from the monitored if working well anus, and enough fluids. compared to hemorrhoidectomy. ● (Hemorrhoids - Diagnosis and Treatment - Mayo Give medications as indicated. ● Clinic, 2021). Provide a warm sitz bath as appropriate. ● Cleanse the rectal area with mild soap and water or 275 wipes after each stool and provide skin care. ● Encourage patient to move around to prevent breathing and circulation problems. VII. SURGICAL MANAGEMENT PROCEDURE Hemorrhoidectomy RATIONALE NURSING RESPONSIBILITIES Surgery to remove hemorrhoids Before is called the hemorrhoidectomy. Procedure/Examination: The doctor makes small cuts around the anus to slice them away. You may anesthesia (the get ● local Assess patient discomfort operated on is numb, and you're associated awake hemorrhoids, relaxed) the presence of hemorrhoids, area being though for or or pain with diet, fluid general anesthesia (you're put intake, and presence of to sleep). Hemorrhoidectomy is constipation. often an outpatient procedure, ● Instruct patient and/or and you can usually go home family regarding causes of the same day (Khatri, 2022). hemorrhoids, methods of avoiding hemorrhoids, and Procedure for Prolapse PPH is also called a stapled and Hemorrhoids hemorrhoidectomy. The doctor (PPH)/Hemorrhoid will use a stapler-like device to stapling reposition the hemorrhoids and cut off their blood supply. treatments that can be performed. ● Instruct patient family regarding and/or all procedures required. Without blood, they'll eventually shrivel and die. It can treat 276 hemorrhoids that have and Instruct patient and/or have not prolapsed, or slipped family in comfort measures down out of the anus (Khatri, to use with the presence of 2022). hemorrhoids. Hemorrhoidal Artery Hemorrhoidal Artery Ligation Ligation and Recto and Recto Anal Repair (HAL- Anal Repair (HAL- RAR) is a new procedure in RAR) ● which a miniature Doppler During Procedure/Examination: ● sensor is inserted in the anus to to surgeon hemorrhoids. can arteries The pinpoint supplying ● are no reduced After longer the Procedure/Examination: ● Monitor the patient closely in the recovery room. ● noticeable. The procedure is IV fluid should be monitored if working well effective and virtually painless (Khatri, 2022). Ensure the IV fluids given to the patient. almost immediately and within weeks, the time the the off to cut the blood supply. The are for anesthesia started. the hemorrhoids and can tie them hemorrhoids Note surgery and the general detect the arteries supplying blood the and enough fluids. ● Give medications as indicated. ● Provide a warm sitz bath as appropriate. ● Cleanse the rectal area with mild soap and water or wipes after each stool and provide skin care. ● Encourage patient to move around to prevent breathing and circulation problems. 277 VIII. NURSING MANAGEMENT NURSING DIAGNOSIS GOAL Acute Pain related to difficulty After nursing 1. Examine the patient in defecation as evidenced by intervention, the patient will be for headaches, sore a pain scale of 7/10 and able to report decreased rectal throats, swelling pain as evidenced by a pain malaise scale of 1/10 and shows weakness, improvement in comfort. spasms, Rationale: 1 hour of INTERVENTION If a hemorrhoid forms a clot, overall or bodily muscle and soreness. the person may experience R: pain when they sit down, elevated defecate, urinate, or walk. frequently the root cause of According headaches, to Caruso, S. Inflammation or an temperature is sore throat, malaise, muscle (2021), acute pain can start general slowly or suddenly. A painful pains, sensory symptoms may indicate acute and emotional experience is what is referred and pain. These pain caused by hemorrhoids. to as acute pain, where most of the time, it is connected to 2. Examine the patient's tissue damage in the body. vital signs The muscles that open and deviations close the anus may stop baselines. for from hemorrhoids from receiving R: The autonomic response to blood pain (strangulated hemorrhoid). The hemorrhoid usually causes an increase in vital signs. tissues could die as a result. If this occurs, they will have 3. Administer analgesics, severe rectal pain and can as ordered. notice blood and pus at the R: Analgesics are a anus. pharmacologic treatment for 278 pain and discomfort that reduces brain prostaglandin production. If the pain is intolerable, analgesics are beneficial. 4. Provide a relaxing and peaceful environment for the patient. R: This method decreases stimulation that may aggravate discomfort. 5. Give the patient a warm sitz bath. R: Warmth induces vasodilation, which relieves hemorrhoids' discomfort. 6. For the treatment of hemorrhoids, apply topical ointments or use a suppository. R: Topical ointments and suppositories can help relieve the pain and discomfort of hemorrhoids. 7. Educate the patient or significant other about breathing, relaxation, meditation, massage, and other 279 nonpharmacologic interventions. R: This strategy helps patients focus less on pain. These techniques will change the patient's perception of pain and may improve discomfort the they are experiencing. Impaired Skin Integrity related to After 8 hours of nursing 1. Assess the patient for hemorrhoidal intervention, the patient will be the presence surgery and procedures as able to maintain intact skin hemorrhoids, evidenced by swelling and with no signs and symptoms discomfort disruption of skin layers from of associated the incision site rectal prolapse and bleeding of or pain with hemorrhoids, diet, fluid intake, and presence Rationale: The of constipation. skin is the body's R: Provides baseline outermost line of protection, information as to the type of preventing hemorrhoids germs penetrating disease. and Cuts, from (external or spreading internal), degree of venous abrasions, thrombosis, and presence of ulcers, incisions, and wounds complications, damage the skin, allowing bleeding, and risk factors that germs to enter and cause preclude infections. Even after having hemorrhoids hemorrhoids initiation removed, the patient may still feel like they including the of patient to a from enable care plan appropriate for the patient. have hemorrhoids in the skin tags that surround the anal area. This includes some 2. Assess impaired the site of tissue post-operative swelling, which 280 will go away over time. Some integrity may be brought on by tissue condition. that was removed not during completely surgery. and its R: Redness, swelling, pain, burning, and itching are Impairment of the skin can be indications of due surgical and body’s on the system response to localized patient. Although it has the tissue trauma or impaired highest tissue integrity. to certain procedures done likelihood complications, of immune surgical hemorrhoidectomy is the most successful the inflammation treatment 3. Assess for the characteristics of the hemorrhoids. wound, including color, size (length, width, depth), drainage, and odor. R: These findings will give information on the extent of the impaired tissue integrity or injury. Pale tissue color is a sign of decreased oxygenation. An odor may result from the presence of infection on the site; it may also be coming from necrotic tissue. Serous exudate from a wound is a normal part of inflammation and must be differentiated from pus or purulent discharge present in the infection. 281 4. Provide tissue care as needed. R: Each type of wound is best treated based on its etiology. Skin wounds may be covered with wet or dry dressings, topical creams or lubricants, hydrocolloid dressings (e.g., DuoDerm), or permeable vapormembrane dressings such as Tegaderm. 5. Keep a sterile dressing technique during wound care. R: A sterile technique reduces the risk of infection in impaired tissue integrity. This involves the use of a sterile procedure field, sterile gloves, sterile supplies and dressing, and sterile instruments 6. Monitor patient’s continence status and minimize exposure of skin impairment site and other areas to moisture from incontinence, perspiration, or wound drainage. 282 R: Prevents exposure to chemicals in urine and stool that can strip or erode the skin causing further impaired tissue integrity. 7. Administer antibiotics as ordered. R: Although intravenous antibiotics may be indicated, wound infections managed well may and be more efficiently with topical agents. 8. Tell the avoid patient rubbing scratching. to and Provide gloves or clip the nails if necessary. R: Rubbing and scratching can cause further injury and delay healing. 9. Discuss the relationship between adequate nutrition consisting of fluids, protein, vitamins B and C, iron, and calories. R: Nutrition plays a vital role in maintaining intact skin and in promoting wound healing. 283 10. Instruct patient, significant others, and family in the proper care of the wound, including handwashing, wound cleansing, dressing changes, and application of topical medications). R: Accurate information increases the patient’s ability to manage therapy independently and reduces the risk of infection. 11. Educate the patient on the need to notify the physician or nurse. R: This is to prevent further impaired tissue integrity complications. Constipation related to low After nursing 1. Assess the patient's residue diet as evidenced by intervention, the patient will be bowel habits, lifestyle, the passage of hard-formed able to establish and maintain capacity to detect a stool passage of soft, formed stool defecation at a frequency perceived as severe hemorrhoids, normal by the patient. and history Rationale: Constipation typically 8 hours of urge, of constipation. happens when waste or stool R: This intervention aids in passes too slowly through the determining an efficient bowel digestive tract or cannot be regimen, impairment, and the 284 efficiently evacuated from the need for support. As a result of rectum, which may result in poor digestion, Gl function the stool becoming hard and may dry. is impairment caused by muscle constipated, patients are more weakness and immobility may prone to push forcefully when result in reduced abdominal defecating. As a result, the peristalsis rectum and anus veins could identifying get larger. These protruding defecate. When a person suffer. and the Functional trouble need to veins are called hemorrhoids. Hemorrhoids and constipation 2. Examine the patient's may get worse if the patient stool frequency, will not consume enough fiber. features, flatulence, stomach pain or distension, and stool straining. R: Constipation can be caused by aging factors such as diminished rectal compliance, discomfort, and impaired rectal sensation. 3. Thoroughly observe the patient's nutrition and fluid intake. R: Sufficient amounts of fiber and roughage produce bulk, and at least 2 L of liquids per day is beneficial in preventing hard stools. 285 4. Examine the bowel sounds for presence and quality. R: Atypical sounds, including high-pitched tinkles, indicate difficulties such as ileus. 5. Assess the patient for complaints of abdominal discomfort and distention. R: Gas, abdominal distention, or ileus could all contribute to constipation. Impaired digestion can cause intestinal distention and, in severe cases, Can result in ileus due to a lack of peristalsis. 6. Keep an eye on the patient's mental state, syncope, heart palpitations, and any transient attacks. doctor ischemic Inform if the these symptoms develop. R: Excessive straining may severely affect arterial circulation, resulting in heart, cerebral, or peripheral ischemia. 286 7. Examine the patient for rectal bleeding. R: Extreme straining can result in hemorrhoids, rectal prolapse, or anal perforations, all of which cause damage to the tissue and bleeding 8. As needed, administer bulk stool softeners, laxatives, suppositories, or enemas. R: These medications help stimulate stool evacuation. 9. Advise the patient to consume high-fiber foods such as wholegrain cereals, bread, and fresh fruits. R: This intervention enhances peristalsis and aids in elimination 10. Monitor the patient's medication that may predispose them to be constipated. R: Some medications are known to cause constipation include analgesics, 287 anesthetics, anticholinergics, and diuretics. 11. Educate the patient in activity or routines for the exercise appropriate disease process. R: Activity peristalsis and enhances defecation Exercises serve to strengthen the stomach muscles, which helps with bowel movement. IX. LITERATURE Hemorrhoids: A range of treatments Bora & Gorgun (2020) Hemorrhoids: A range of treatments. Retrieved on February 20, 2023, from: https://www.ccjm.org/content/86/9/612 Hemorrhoids accounted for more than 3.5 million US outpatient visits in 2010, and they were the third leading cause of hospital admissions related to gastrointestinal disease. In choosing the treatment for hemorrhoids, one should consider the disease grade and severity, its impact on the quality of life, the degree of pain it causes, the patient’s likelihood of adhering to treatment, and the patient’s personal preference. Treatments can be grouped in 3 categories: conservative, office-based, and surgical. Conservative measures are aimed at softening the stool, relieving pain, and correcting bad toileting habits. In most cases, the primary precipitating factor is lifestyle, and unless patients change it, they are more likely to have recurrent symptoms in the long term. Officebased treatments rubber band ligation, infrared photocoagulation, and sclero-therapy are commonly used for grade I, II, and III hemorrhoids that have not responded to conservative management. The primary goal of these treatments is to decrease blood flow into the hemorrhoidal sac. Although nonsurgical treatments have substantially improved, surgery is the 288 most effective and strongly recommended treatment for patients with high-grade internal hemorrhoids (grades III and IV), external and mixed hemorrhoids, and recurrent hemorrhoids. The most popular surgical options are open or closed hemorrhoidectomy, stapled hemorrhoidopexy, and Doppler-guided hemorrhoidal artery ligation. “PNR-Bleed” classification and Hemorrhoid Severity Score a novel attempt at classifying the hemorrhoids Kahn, Chowdri, et al. (2020) “PNR-Bleed” classification and Hemorrhoid Severity Score a novel attempt at classifying the hemorrhoids Retrieved on February 20, 2023, from: https://jcol.elsevier.es/en-pnr-bleed-classification-hemorrhoid-severity-scorea-articuloS2237936320300423 Hemorrhoids are generally classified on the basis of their location and degree of prolapse. To describe the hemorrhoidal disease more vividly, they devised the “PNR-Bleed” (or PNRBooking) classification system. They classified hemorrhoids based on the four main characteristics of the hemorrhoidal disease i.e. the degree of hemorrhoidal Prolapse (P), Number (N) of the primary hemorrhoidal columns involved, Relation (R) of the hemorrhoidal tissue to dentate line and the amount of Bleeding (B) from it. All the four components in this classification system are graded into five grades ranging from 1 to 5. Based on this “PNR-Bleed” classification, They introduced another concept of scoring the severity of hemorrhoids. In this article, they refer to this scoring system for hemorrhoids as the Hemorrhoid Severity Score (HSS) which is the total score obtained by the sum of the numerical grades of all four characteristics of hemorrhoids in “PNR-Bleed” classification. This new “PNR-Bleed” system of classifying the hemorrhoids and calculation of HSS seems to be more comprehensive, detailed, more objective and easily reproducible. This new classification of hemorrhoids may provide a new dimension of research for the management of hemorrhoidal disease. Midwifery Care for Mothers with Hemorrhoids Sujawaty, Tompunuh, et al, (2023) Midwifery Care for Mothers with Hemorrhoids. Retrieved on February 20, 2023, from: https://www.aisyah.journalpress.id/index.php/jika/article/view/812 Women die from complications during pregnancy, childbirth and the puerperium. It was found that respondents suffered from grade IV hemorrhoids where in most cases pregnant women with grade IV hemorrhoids would have section caesarea surgery to reduce pressure pain when 289 the mother pushes. In pregnancy, due to the influence of increased sex hormones and increased blood volume, causing dilation of the veins in the rectal area. The increase in the hormone progesterone in pregnant women will cause peristalsis of the digestive tract to slow down and the muscles to relax, as well as relaxation of the anorectal venous valves, which will result in constipation which will aggravate the venous system. Likewise, due to the suppression of the fetus in the uterus on the veins in the pelvic area will result in damming. Coupled with straining to defecate that often occurs in pregnant women because constipation will cause hemorrhoidal prolapse. Hemorrhoids that do not because complaints do not require special treatment, except for the preventive measures mentioned. After delivery, uncomplicated hemorrhoids will shrink on their own. Hemorrhoids can be prevented by drinking enough water, eating lots of vegetables, and lots of fruits, so that the stool does not harden. Hemorrhoids are not too dangerous, both for the mother and the fetus, but when the doctor has entered the fourth degree, it is more advisable to do a cesarean section to reduce pressure pain when the mother pushes. 290 X. REFERENCES Acetaminophen (Tylenol) Nursing Considerations & Patient Teachings. (2023, January 12). NurseTogether. https://www.nursetogether.com/acetaminophen-nursing- considerations/ Acetaminophen: Generic, Uses, Side Effects, Dosages, Interactions, Warnings. (2022, October 11). RxList. https://www.rxlist.com/consumer_acetaminophen_tylenol/drugscondition.htm Ambardekar, N. (2022, September 18). GERD. WebMD. Retrieved January 13, 2023, from https://www.webmd.com/heartburn-gerd/guide/reflux-disease-gerd-1 Analgesics: Uses, treatment, risks. (2021, March 22). Cleveland Clinic. Retrieved February 26, 2023, from https://my.clevelandclinic.org/health/drugs/21483-analgesics Aspirin: Generic, Uses, Side Effects, Dosages, Interactions & Warnings. (2021b, August 9). RxList. https://www.rxlist.com/consumer_aspirin/drugs-condition.htm Basson M. (2022) Ulcerative Colitis. Retrieved on February 9, 2023 from https://emedicine.medscape.com/article/183084-overview Bakshis, B. (2021, May 10). 6 Signs You May Have a Stomach Ulcer. Digestive Health. https://www.healthgrades.com/right-care/digestive-health/6-signs-you-may-have-astomach-ulcer Belleza, M., & R.N. (2018, December 6). Gastroesophageal Reflux: Study Guide for Nurses. Retrieved from Nurseslabs website: https://nurseslabs.com/gastroesophagealreflux/#medical_management Boakye-Yiadom, M., Kumadoh, D., Adase, E., & Woode, E. (2021). Medicinal Plants with Prospective Benefits in the Management of Peptic Ulcer Diseases in Ghana. BioMed Research International, 2021, 1–14. https://doi.org/10.1155/2021/5574041 Caio, G., Lungaro, L., Caputo, F., Zoli, E., Giancola, F., Chiarioni, G., De Giorgio, R., & Zoli, G. (2021). Nutritional Treatment in Crohn’s Disease. Nutrients, 13(5), 1628. https://doi.org/10.3390/nu13051628 Calixtro, L. (2020). Hemorrhoidectomy. studylib.net. Retrieved February 13, 2023, from https://studylib.net/doc/25510915/hemorrhoidectomy 291 Carter, A. (2022) What to know about Calcium Blockers. Retrieved February 26, 2023 from https://www.medicalnewstoday.com/articles/h2-blockers Chron's and Colities Canada. (2019). GAS AND BLOATING. SYMPTOMS MANAGEMENT. https://crohnsandcolitis.ca/About-Crohn-s-Colitis/IBDJourney/Symptom-Management/Gas-and-Bloating Cleveland Clinic (n.d) Digital Rectal exam. Retrieved on February 26, 2023 from https://my.clevelandclinic.org/health/diagnostics/24212-digital-rectal-exam Cleveland Clinic. (2020, April 23). Ulcerative Colitis: Symptoms, Treatment & Living With It & Diagnosis. Retrieved February 24, 2023, from https://my.clevelandclinic.org/health/diseases/10351-ulcerative-colitis#management-andtreatment Cleveland Clinic. (2020, April 26) Stomach Flu (Gastroenteritis) : Symptoms, Causes &. Diagnosis .Retrieved February 19, 2023, from https://my.clevelandclinic.org/health/diseases/12418-gastroenteritis Corticosteroids. (2020, January 20). Cleveland Clinic. Retrieved February 26, 2023, from https://my.clevelandclinic.org/health/drugs/4812-corticosteroids crohn’scolitisfoundation.org. (2022). Ulcerative Colitis Treatment Options. Crohn’s & Colitis Foundation. Retrieved February 25, 2023, from https://www.crohnscolitisfoundation.org/what-is-ulcerative-colitis/treatment-options Creaky Joints Org. (2020). Crohn’s Disease Symptoms You Should Never Ignore. https://creakyjoints.org/education/crohns-disease/symptoms/ Dickson, D. (2022). A new device is helping treat acid reflux and Heartburn ahead of the holidays. 25 News KXXV and KRHD. Retrieved from www.kxxv.com/brazos/a-newdevice-is-helping-treat-acid-reflux-and-heartburn-ahead-of-the-holidays Differences in Small & Large Intestines | Children’s Pittsburgh. (n.d.). Children'S Hospital of Pittsburgh. https://www.chp.edu/our-services/transplant/intestine/education/about- small-large-intestines Difficulty Swallowing (Dysphagia). (2023). Endoscopy Center of Red Bank. https://endoscopycenterofredbank.com/condition/difficulty-swallowing-dysphagia DiGiacinto, J. (2021, October 20). Everything you need to know about acid reflux and GERD. Healthline. Retrieved February 13, 2023, from https://www.healthline.com/health/gerd Frcr, A. N. K. M. F. F. (n.d.). Ulcerative Colitis Imaging: Practice Essentials, Radiography, Computed Tomography. https://emedicine.medscape.com/article/375166-overview 292 Gastroesophageal_reflux_laryngitis. (2020). University of Mississippi Medical Center. Retrieved February 13, 2023, from https://www.umc.edu/Healthcare/ENT/PatientHandouts/Adult/Voice_Swallowing/Gastroesophageal_Reflux_Laryngitis.html GERD (chronic acid reflux): Symptoms, treatment, & causes. (2019, December 6). Cleveland Clinic. Retrieved February 13, 2023, from https://my.clevelandclinic.org/health/diseases/17019-gerd-or-acid-reflux-or-heartburnoverview Digestive Health Associates Endoscopy. (2020, Ocotober 19). Signs of a Stomach Ulcer. Gastroenterology Conditions. https://www.dhaendoscopy.com/blog/post/signs-of-astomach-ulcer.html Golen, T. (2022) Could Stress be Making Acid Reflux Worse? Retrieved February 26, 2023 from https://www.health.harvard.edu/diseases-and-conditions/could-stress-be-making- my-acid-refluxworse#:~:text=Emotional%20stress%20can%20increase%20acid%20production%20in% 20the,up%20from%20the%20stomach%20and%20into%20the%20esophagus. Hamza, Z. (2022). Two surgeries for chronic GERD yield similar long-term outcomes. Medical News. Retrieved from https://www.medpagetoday.com/gastroenterology/gerd/98325 Healthline (2018) Coffee Vs. Tea for GERD. Retrieved February 26, 2023 from https://www.healthline.com/health/gerd/coffee-tea Heartburn, Acid Reflux, or GERD: Whatâs the Difference? | Pfizer. (2023). https://www.pfizer.com/news/articles/heartburn_acid_reflux_or_gerd_what_s_the_differe nce Hemorrhoids - Diagnosis and treatment - Mayo Clinic. (2021, May 12). https://www.mayoclinic.org/diseases-conditions/hemorrhoids/diagnosis-treatment/drc20360280 Hollman, J. (2022) Hiatal Hernia and GERD: Symptoms, Treatment and Prevention. Retrieved February 26, 2023 from https://easyhealthoptions.com/hiatal-hernia-gerdsymptoms-treatment-prevention/ https://www.webmd.com/ibd-crohns-disease/ulcerative-colitis/surgery-ulcerative-colitis John Hopkins Medicine (2023) anoscopy and high resolution anoscopy. Retrieved on February 26, 2023 from https://www.hopkinsmedicine.org/health/treatment-tests-andtherapies/anoscopy-high-resolution-anoscopy 293 Jones, G. L. (2019, October). Abdominal X-ray - Abnormalities. Radiology Masterclass. Retrieved February 25, 2023, from https://www.radiologymasterclass.co.uk/gallery/abdo/abdominal_xray/ulcerative_colitis Kamada, T., Satoh, K., Itoh, T., Ito, M., Iwamoto, J., Okimoto, T., Kanno, T., Sugimoto, M., Chiba, T., Nomura, S., Mieda, M., Hiraishi, H., Yoshino, J., Takagi, A., Watanabe, S., & Koike, K. (2021). Evidence-based clinical practice guidelines for peptic ulcer disease 2020. Journal of Gastroenterology, 56(4), 303–322. https://doi.org/10.1007/s00535-021-017690 Khatri, M. (2022, November 27). Surgery for Ulcerative Colitis. WebMD. Retrieved February 24, 2023, from Khatri, M. (2022, September 18). Hemorrhoid Surgery. WebMD. Retrieved February 13, 2023, from https://www.webmd.com/digestive-disorders/surgery-treat-hemorrhoids Kizior, R. J. (2019). Saunders Nursing Drug Handbook, 2020. S.L.: Elsevier Saunders. Kizior, R. J. (2019). Saunders Nursing Drug Handbook, 2020. S.L.: Elsevier Saunders. Kizior, R. J., & Hodgson, K. (2021). Saunders Nursing Drug Handbook 2022. Elsevier Gezondheidszorg. Li, X., Wei, X., Sun, Y., Du, J., Li, X., Xun, Z., & Li, Y. C. (2019). High-fat diet promotes experimental colitis by inducing oxidative stress in the colon. American Journal of Physiology. Gastrointestinal and Liver Physiology, 317(4), G453–G462. https://doi.org/10.1152/ajpgi.00103.2019 Manuelpillai, C., MD. (2018, March 4). 6 Reasons You Are Regurgitating and How to Stop It | Buoy. https://www.buoyhealth.com/learn/regurgitation Martin, P. (2019, March 2). Fecal Analysis (Stool Analysis). Nurseslabs. Retrieved February 13, 2023, from https://nurseslabs.com/fecal-analysis-stool- analysis/#nursing_responsibility_for_stool_analysis Martin, P. (2022, March 7). Colonoscopy. Nurseslabs. Retrieved February 13, 2023, from https://nurseslabs.com/colonoscopy/#nursing_responsibilities Mayo Clinic. (2020, October 13). Crohn’s disease - Symptoms and causes. Retrieved from Mayo Clinic website: https://www.mayoclinic.org/diseases-conditions/crohns- disease/symptoms-causes/syc-20353304 Mayo Clinic. (2023). Gastroesophageal reflux disease (GERD) - Diagnosis and treatment - Mayo Clinic. Retrieved from www.mayoclinic.org website: https://www.mayoclinic.org/diseases-conditions/gerd/diagnosis-treatment/drc20361959#:~:text=Endoscopy- 294 Mayo Clinic. (2023). Gastroesophageal reflux disease (GERD) - Diagnosis and treatment - Mayo Clinic. Retrieved from www.mayoclinic.org website: https://www.mayoclinic.org/diseases-conditions/gerd/diagnosis-treatment/drc20361959#:~:text=EndoscopyMayo Clinic. (2022, June 11). Peptic ulcer. Disease and Conditions. https://www.mayoclinic.org/diseases-conditions/peptic-ulcer/symptoms-causes/syc20354223 Medication Options for Ulcerative Colitis. (2022.). Crohn’s & Colitis Foundation. https://www.crohnscolitisfoundation.org/what-is-ulcerative-colitis/medication MedlinePlus. (2018). Esomeprazole: MedlinePlus Drug Information. Retrieved from Medlineplus.gov website: https://medlineplus.gov/druginfo/meds/a699054.html MedlinePlus. (2018). Esomeprazole: MedlinePlus Drug Information. Retrieved from Medlineplus.gov website: https://medlineplus.gov/druginfo/meds/a699054.html MedlinePlus. (2022, January 15).Ondansetron . Retrieved February 19, 2023, from https://medlineplus.gov/druginfo/meds/a601209.html Medscape. (2021). Ampicillin (Rx). Retrieved last March 19, 2023 from: https://reference.medscape.com/drug/ampi- omnipen-ampicillin-342475 Meima - Van Praag, E. M., Buskens, C. J., Hompes, R., & Bemelman, W. A. (2021). Surgical management of Crohn’s disease: a state of the art review. International Journal of Colorectal Disease, 36(6), 1133–1145. https://doi.org/10.1007/s00384021-03857-2 Miller, J. (2021) What are the Exercises that should be Avoided by People with GERD? Retrieved February 26, 2023 from https://livehealthy.chron.com/exercises-Shouldavoided-people-gerd-1251.htm MIMS. (2023). Kremil-S Advance. Retrieved February 13, 2023, from Mims.com website: https://www.mims.com/philippines/drug/info/kremil-s%20advance/indications MIMS. (2023). Kremil-S Advance. Retrieved February 13, 2023, from Mims.com website: https://www.mims.com/philippines/drug/info/kremil-s%20advance/indications Mouth anatomy. (2023, January 5). Britannica. Retrieved February 13, 2023, from https://www.britannica.com/science/mouth-anatomy N. (2020, December 5). SIGMOIDOSCOPY - nurseinfo. Nurseinfo -. https://nurseinfo.in/sigmoidoscopy/ 295 NCI dictionary of cancer terms. (2020). National Cancer Institute. Retrieved February 13, 2023, from https://www.cancer.gov/publications/dictionaries/cancer-terms/def/digestivesystem NonSteroidal Anti-Inflammatory drugs (NSAIDs). (2020, January 25). Cleveland Clinic. Retrieved February 26, 2023, from https://my.clevelandclinic.org/health/drugs/11086-nonsteroidal-anti-inflammatory-medicines-nsaids Osborne, H. (2022, July 12). Imaging techniques for UC diagnosis. https://www.medicalnewstoday.com/articles/ulcerative-colitis-x-ray#ct-scan Padua D. (2022) Can ulcerative colitis cause Nausea? Retrieved on February 13, 2023 from https://www.healthcentral.com/article/ulcerative-colitis-nausea Pathak, N. (2021, March 8). Ulcerative Colitis Treatment. WebMD. Retrieved February 25, 2023, from https://www.webmd.com/ibd-crohns-disease/ulcerative-colitis/digestive- diseases-ulcerative-colitis-treatment Pathak, N. (2021, September 16). What Is a Peptic Ulcer? Digestive Disorders. https://www.webmd.com/digestive-disorders/peptic-ulcer-overview Petagna, L., Antonelli, A., Ganini, C., Bellato, V., Campanelli, Divizia, A., Franceschilli, M., Guida, A. M., Ingallinella, S., & Montagnese, F. (2020, November 07). Pathophysiology of Crohn’s disease inflammation and recurrence. Biological Direct. Phillips, Q. (2021, July 30). What’s a Sigmoidoscopy? All About Testing and Diagnosis. EverydayHealth.com. Phillips, M. M., & Dugdale, D. C. (2022, May 4). Bloody or tarry stools. https://www.mountsinai.org/health-library/symptoms/bloody-or-tarry-stools Prima Medicine. (2021). 5 Signs You May Have an Ulcer. Prima Medicine. https://www.everydayhealth.com/ulcerative-colitis/sigmoidoscopy/ Phn, A. C. R. B. (2023, January 23). Peptic Ulcer Disease Nursing Diagnosis and Nursing Care Plans. NurseStudy.Net. https://nursestudy.net/peptic-ulcer-disease-nursing- diagnosis/ Roda, G., Chien Ng, S., Kotze, P. G., Argollo, M., Panaccione, R., Spinelli, A., Kaser, A., Biroulet, L. P., & Danese, S. (2020, April 02). Crohn’s disease. Nature Reviews Disease Primers. https://www.nature.com/articles/s41572-020-0156-2 R.N., M. B. (2019, May 13). Antacids Nursing Pharmacology Study Guide. Nurseslabs. Retrieved from https://nurseslabs.com/antacids/#antacids_generic_and_brand_names R.N., M. B. (2019, May 13). Antacids Nursing Pharmacology Study Guide. Nurseslabs. Retrieved from https://nurseslabs.com/antacids/#antacids_generic_and_brand_names 296 Rath, L. (2022). Crohn’s Disease and Oral Contraceptives: What to Know. Retrieved February 23, 2023, from WebMD website: https://www.webmd.com/ibd-crohns- disease/crohns-disease/crohns-disease-oralcontraceptives#:~:text=Research%20has%20shown%20that%20combination RegisteredNursing.org Staff Writers. (2022, August 28). Medication Administration: NCLEX-RN. Retrieved February 24, 2023, from https://www.registerednursing.org/nclex/medication-administration/ RNpedia. (2021). Ampicillin Nursing Considerations & Management. Retrieved lastMarch 19, 2023 from: https://www.rnpedia.com/nursing-notes/pharmacology-drug-study- notes/ampicillin/ Robinson, E. (2019. New research could change how clinicians diagnose, treat Unmanaged Heartburn. OHSU News. Retrieved from https://news.ohsu.edu/2019/10/23/new-research-could-change-how-clinicians-diagnosetreat-unmanaged-heartburn Roth, E. (2019, March 8). Acid Reflux and Nausea. Healthline. https://www.healthline.com/health/gerd/nausea Sang, J.K., (2019) Gender Specific Differences in Prevalence and Risk Factors for GastroEsophageal Reflux Disease. Retrieved February 26, 2023 from https://pubmed.ncbi.nlm.nih.gov/31144481/ Schere, E. (2022) How Common is GERD. Retrieved February 26, 2023 from https://health.howstuffworks.com/diseases-conditions/digestive/how-common-is-g erd.htm Skidmore-Roth, L. (2021). Mosby’s 2021 nursing drug reference. St. Louis, Missouri: Mosby. Skidmore-Roth, L. (2021). Mosby’s 2021 nursing drug reference. St. Louis, Missouri: Mosby. Smith L. (2021) 4 Types of Ulcerative Colitis, According to a Gastroenterologist. Retrieved on February 9, 2023 from https://www.goodrx.com/conditions/ulcerative-colitis/ulcerativecolitis-types Sleiman, J., El Ouali, S., Qazi, T., Cohen, B., Steele, S. R., Baker, M. E., & Rieder, F. (2020). Prevention and Treatment of Stricturing Crohn’s Disease – Perspectives and Challenges. Expert Review of Gastroenterology &Amp; Hepatology, 15(4), 401–411. https://doi.org/10.1080/17474124.2021.1854732 297 Stuart, C. C. (2019, February 20). Treating constipation in Crohn's disease. Medical News Today. https://www.medicalnewstoday.com/articles/324502 Surgery for Ulcerative Colitis. (n.d.). Crohn’s & Colitis Foundation. https://www.crohnscolitisfoundation.org/what-is-ulcerativecolitis/surgery#:~:text=The%20standard%20surgical%20procedure%20to,used%20to%2 0treat%20ulcerative%20colitis. Swiner, C. (2022, January 31). Gastroesophageal reflux disease (GERD). WebMD. Retrieved February 13, 2023, from https://www.webmd.com/heartburn-gerd/refluxdisease Taylor, C., Nall, R., & Meixner, M. (n.d.). Gastroenteritis and Stool Culture: Why It's Needed and How It Helps. Healthline. Retrieved February 19, 2023, from https://www.healthline.com/health/gastroenteritis-stool-culture#about-a-stool-culture Temple Health Org. (2023). Symptoms. https://www.templehealth.org/services/conditions/crohns-disease/symptoms The Editors of Encyclopaedia Britannica. (2023, January 5). Mouth | Definition, Anatomy, & Function. Encyclopedia Britannica. https://www.britannica.com/science/mouth-anatomy Tresca, A. (2021). Understanding what ulcerative colitis is and how it develops. Very Well Health. Retrieved on February 13, 2023 from https://www.verywellhealth.com/ulcerativecolitis-pathophysiology- 5208723 Ulcerative Colitis Diagnosis and Testing. (n.d.-b). Crohn’s & Colitis Foundation. https://www.crohnscolitisfoundation.org/what-is-ulcerative-colitis/diagnosis-testing University of Illinois. (2019, March 15). Ampicillin, Oral Capsule. Retrieved last March 19, 2023 from: https://www.healthline.com/health/ampicillin-oral-capsule#other-warnings Vera, M. (2023, January 16). Aspirin nursing considerations and patient teaching [Drug guide]. Nurseslabs. Retrieved February 26, 2023, from https://nurseslabs.com/aspirinnursing-considerations-and-patient-teaching-drug-guide Warf, K. (2022, April 28). 7 Tips to Stop a GERD Cough. Ear, Nose, and Throat Center. https://www.ent-center.com/7-tips-to-stop-a-gerd-cough/ Watson S. (2021) Ulcerative colitis and weight loss. Retrieved on February 13, 2023 from https://www.healthline.com/health/ulcerative-colitis/weight-loss-faqs-answered Watson, S. (2022, June 29). Crohn’s Disease: The Effects of Smoking. Retrieved from WebMD website: https://www.webmd.com/ibd-crohns-disease/crohns-disease/smokingaffect-crohns-disease 298 Wayne, G. (2023, January 23). Acetaminophen nursing considerations & patient teaching [drug guide]. Nurseslabs. Retrieved February 26, 2023, from https://nurseslabs.com/acetaminophen-nursing-considerations-and-patient-teachingdrug-guide/ WebMD. (2022). Crohn’s Disease Overview. Retrieved from WebMD website: https://www.webmd.com/ibd-crohns-disease/crohns-disease/digestive-diseases-crohnsdisease WebMD. (2022). Drugs & Medications. Retrieved from www.webmd.com website: https://www.webmd.com/drugs/2/drug-5035-250/famotidine-oral/famotidine-10-mgoral/details WebMD. (2022). Drugs & Medications. Retrieved from www.webmd.com website: https://www.webmd.com/drugs/2/drug-5035-250/famotidine-oral/famotidine-10-mgoral/details Winsborough, H. (2022). NSAIDs and Crohn’s Disease. Retrieved from WebMD website: https://www.webmd.com/ibd-crohns-disease/crohns-disease/crohns-disease-andnsaids#:~:text=The%20American%20College%20of%20Gastroenterology Wint C. (2021) Why do I have tenesmus. Retrieved on February 13, 2023 from https://www.healthline.com/health/tenesmus Yen, H., Wu, P. Y., Chen, M., Lin, W., Tsai, C., & Lin, K. (2021). Current Status and Future Perspective of Artificial Intelligence in the Management of Peptic Ulcer Bleeding: A Review of Recent Literature. Journal https://doi.org/10.3390/jcm10163527 of Clinical Medicine, [Original 10(16), 3527. source: https://studycrumb.com/alphabetizer] 299