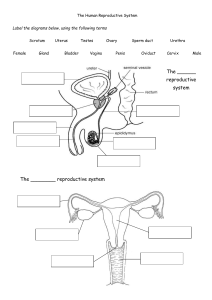
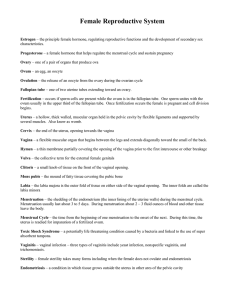
CLASS 10 BIOLOGY (22-23 SESSION) LESSON 10 REPRODUCTIVE SYSTEM Solutions to the Exercise questions of Reproductive System by BYJUS is provided in the link given below: https://byjus.com/icse-selina-solution-concise-biology-class-10-chapter-13-the-reproductive-system/ Video links: https://youtu.be/D-gPmMCOKeg https://youtu.be/bOHu9AI9OQE • • What is reproduction? Reproduction is the process of producing new individuals by an organism of the same kind which in turn can repeat the process. Types: Asexual, Sexual. M ALE REPRODUCTIVE SYSTEM Also called the male uro-genitalsystem as sperms and urine have a common passage from urethra which is called penis. A) PRIMARY REPRODUCTIVE ORGANS: TESTES (singular testis) 1. Paired, oval organs, situated outside abdominal cavity in loose sacs called scrotum/ scrotal sacs. • 2. Testes descend into scrotum through the inguinal canal a little before birth as scrotum has a lower temperature than abdominal cavity which is suitable for production and maturation of sperms by testes. 3. Each testis divided into 200-350 lobules. Each lobule has 2 parts: a) Seminiferous tubules- produces sperms by a process called spermatogenesis (gametogenesis in general). b) Interstitial cells of Leydig- producing male hormone testosterone. This hormone helps in sperm maturation, growth and development of male reproductive organs, development of male secondary sexual characteristics. Note: 1.Testes are considered as endocrine tissue as it has endocrine function of secreting the hormone testosterone and also non-endocrine function of spermatogenesis (producing sperms). 2. Hernia- a condition in which the intestine bulges into the scrotum through the inguinal canal due to pressure exerted by abdomen usually after any surgical procedure. B) ACCESSORY REPRODUCTIVE ORGANS: 1) DUCTS: From the testes, the sperms move through a system of ducts to finally reach the urethra. Testes→ Rete testis (network of tubules)→ Vasa efferentia (12-14 ducts)→Epididymis→ Vas deferens (sperm duct)→ Urethra Epididymis- highly coiled duct, begins from the upper part of testis, traverses along its back and joins the vas defenens. Its function is storage and maturation of sperms. Vas deferens- travels up from the testes through the inguinal canal into the abdominal cavity, loops over the ureters and opens into the urethra. Its function is to transfer sperms from epididymis to urethra. 2) ACCESSORY GLANDS: a) Seminal vesicle: paired, located between urinary bladder and rectum. Each gives out a duct that joins the vas deferens to form a 2cm long ejaculatory duct before opening into the urethra. Produces a secretion for providing a medium for transportation of sperms. b) Prostate gland: single, bilobed, surrounding the urethra at the base of the bladder. Produces an alkaline secretion to neutralize the acidic environment of the female reproductive tract. c) Bulbo-urethral gland/ Cowper’s gland: Paired, located below the prostate gland. Its secretion lubricates the penis. Note: Semen- an alkaline, milky and sugary fluid which is a mixture of sperms and secretions of the accessory glands. Alkaline nature neutralizes the acidic environment of the female tract so that sperms can survive. Sugar present provides energy for the movement of sperms. 3) SUPPORTIVE STRUCTURE: PENIS: Cylindrical, highly vascular, made of erectile tissue, becomes rigid and erect under sexual stimulation. Serves as a passage for both sperms and urine. STRUCTURE OF SPERM Head: contains a specialized lysosome that secretes an enzyme called hyaluronidase for dissolving the outer membrane of ovum for easy penetration by the sperm. Also contains a nucleus. Midpiece: contains mitochondria that gives energy to the sperm for locomotion. Also has centrioles. Tail: helps in propagation of the sperm along its course. ______________________•____________________ FEM ALE REPRODUCTIVE SYSTEM A) PRIMARY REPRODUCTIVE ORGANS: OVARIES 1. Paired, oval bodies, located one on either side of the uterus in the pelvic cavity of female. 2. Only one matured egg is produced by each ovary alternately every month. 3. Consists of ovarian follicles at various stages of maturity like primary, secondary etc. 4. A fully matured ovarian follicle is called Graafian follicle containing a matured ovum. 5. Ovary produces ova (singular ovum) by a process called oogenesis. 6. Graafian follicle secretes a hormone called oestrogen. 7. It ruptures to release the matured ovum which penetrates the ovarian wall and lies outside in the pelvic cavity/ abdominal cavity. This process is called ovulation. 8. The remainings of the Graafian follicle transform into an yellow mass of endocrine tissue called corpus luteum. 9. Corpus luteum secretes the hormones Oestrogen, progesterone and relaxin. Note: Ovary can be called as endocrine tissue as it has endocrine function of producing hormones as well as non-endocrine function of producing ova by oogenesis. Ovulation is the release of mature ovum from the ovary into the pelvic cavity by the rupture of the Graafian follicle. B) ACCESSORY REPRODUCTIVE ORGANS: 1. Oviducts: ➢ Also called as Fallopian tubes, paired, originating one from each ovary. ➢ Carries the ovum from the ovary to the uterus. ➢ Oviduct has inner lining of ciliated epithelium, fluid current and shows peristalsis of the muscles in its wall. All these help in movement of ovum along the oviduct. 2. Uterus: Hollow, pear-shaped organ situated in the pelvic cavity between urinary bladder and rectum. It has 3 parts- upper dome-shaped head called fundus, body and a lower narrowed part called cervix. Its walls have 3 layers of muscles. From outside inwards these are- perimetrium, myometrium and innermost endometrium. 3. Vagina: ✓ Muscular tube, serving as lower end of the birth canal. ✓ Receives the penis during copulation. 4. Vulva: External female genitalia corresponding to penis in males. Note: Puberty is the period during which reproductive organs of humans mature and they become capable of reproduction. The course and fate of the egg/ovum inside the female’s body since its production can be outlined as follows: Ovulation→ Fertilisation→ Implantation→ Gestation→ Parturition These events will be now briefly discussed: A matured ovum is released from the ovary by ovulation as already defined. It will be soon picked up by finger-like projections surrounding the mouth of the oviducal funnel (expanded anterior end of oviduct/Fallopian tube) called fimbriae. If the ovum meets a sperm in the oviduct, then fertilization occurs in the oviduct. Fertilisation is defined as the fusion of sperm and ovum to form a zygote. The zygote divides by mitosis to form a solid ball of cells called morula, which further divides to form a hollow ball of cells called blastocyst. By this time, it has already reached the uterus. The blastocyst fixes itself to the endometrium (innermost muscle wall) of the uterus. The fixation of the blastocyst to the endometrium of the uterus 7-8 days after fertilization is called implantation. This is done to obtain required nutrition from the mother by the developing embryo. When the embryo is 8 weeks old, it is called the foetus. It needs food and oxygen, it also needs to eliminate nitrogenous wastes. This work is done through the placenta. The placenta is a disc-like structure attached to the wall of uterus. It is formed by 2 sets of villi (finger-like projections)- one set formed by uterine wall and the other set formed by a membrane covering the embryo called allantois. The 2 sets of villi interlock but never fuse. There is never any mixing of foetal blood and maternal blood. A cord or rope-like structure connects the placenta with the abdomen of the foetus. This blood-vascular connection between the mother and the foetus is called umbilical cord. Functions of placenta: 1. Tranfers nutrients from mother to foetus. 2. Tranfers wastes from foetus to mother. 3. Acts as a barrier against microbes which might enter from maternal to foetal blood. 4. Acts as an endocrine gland- secretes hormones oestrogen, progesterone and relaxin which were so long secreted from corpus luteum. After pregnancy, this work is done by the placenta. The full term development of the embryo inside the mother’s uterus for a period of 280 days is called gestation. During this gestation period, the embryo develops many coverings around itself called extra-embryonic membranes like amnion, chorion, allantois. The amnion develops around the embryo and encloses a fluid called amniotic fluid in which the foetus remains floating. Functions of amniotic fluid to be studied from the book directly. The act of expulsion of the full term foetus from the uterus of the mother at the end of gestation is called parturition. ROLE OF HORMONES IN REPRODUCTION PITUITARY HORMONES: 1. Follicle-stimulating hormone (FSH)→ helps in development of ovarian follicles from primary to secondary to Graafian follicle. These follicles start secreting oestrogen. 2. Luteinising hormone (LH)→ helps in growth and development of corpus luteum. The latter secretes oestrogen, progesterone and relaxin. OVARIAN HORMONES: 1. Oestrogen-stimulates growth of uterus, vagina, mammary glands, and also development of secondary sexual characteristics. 3. Progesterone- prepares the uterus for implantation, growth and development of foetus. So it is called the “pregnancy hormone”. 4. Relaxin- Relaxes/dilates the uterine cervix during childbirth. NOTE: ➢ IDENTICAL/ MONOZYGOTIC TWINS: Forms when a single fertilized egg splits into two parts, they share a common placenta, usually of the same sex but may be different, each part grows as a separate individual. ➢ NON-IDENTICAL/ DIZYGOTIC/FRATERNAL TWINS: If 2 ova are released by the same or different ovaries at the same time and are fertilized by two different sperms, then two individuals are formed, they have their own placenta, may or may not be of the same sex. MENSTRUAL CYCLE A cyclical event that occurs in females during the reproductive period of 13 to 45-50 years. Here, there is a periodical shedding of blood alongwith unfertilized ovum after every 28 days. Menarche- onset of menstrual cycle in a young female at about 13 years. Menopause- permanent stoppage of menstruation. The menstrual cycle is a series of changes in the endometrium of a non-pregnant female that prepares the lining of the uterus to receive a fertilized egg. Note: Along with changes in the uterine wall, changes also occur in the ovary during this cycle. These changes are influenced by pituitary and ovarian hormones. It can be divided into 4 phases: 1. Menstrual phase- day 1 to 5, characterized by shedding of endometrial lining and elimination of blood, mucous, wornout epithelial cells and unfertilised ovum. Ovary starts developing a new follicle. Low level of Oestrogen and FSH secretion. 2. Follicular phase- day 6 to 13, endometrium starts to thicken and develop more blood vessels, ovarian follicle matures to form Graafian follicle, FSH and oestrogen secretions rise to a peak. 3. Ovulatory phase- day 13 or 14, ovulation occurs by rupture of the Graafian follicle. LH secretion suddenly rises. Oestrogen falls temporarily. 4. Luteal phase- corpus luteum develops due to high levels of LH. Both oestrogen and progesterone level rise considerably. Note: If the ovum is not fertilized, it disintegrates , corpus luteum stops producing progesterone. The endometrium is shed and a menstrual cycle begins. If the ovum is fertilized, the corpus luteum persists and secretes hormones till the placenta is formed. The uterus is maintained in a state suitable for implantation. Video courtesy: SHIKSHA HOUSE