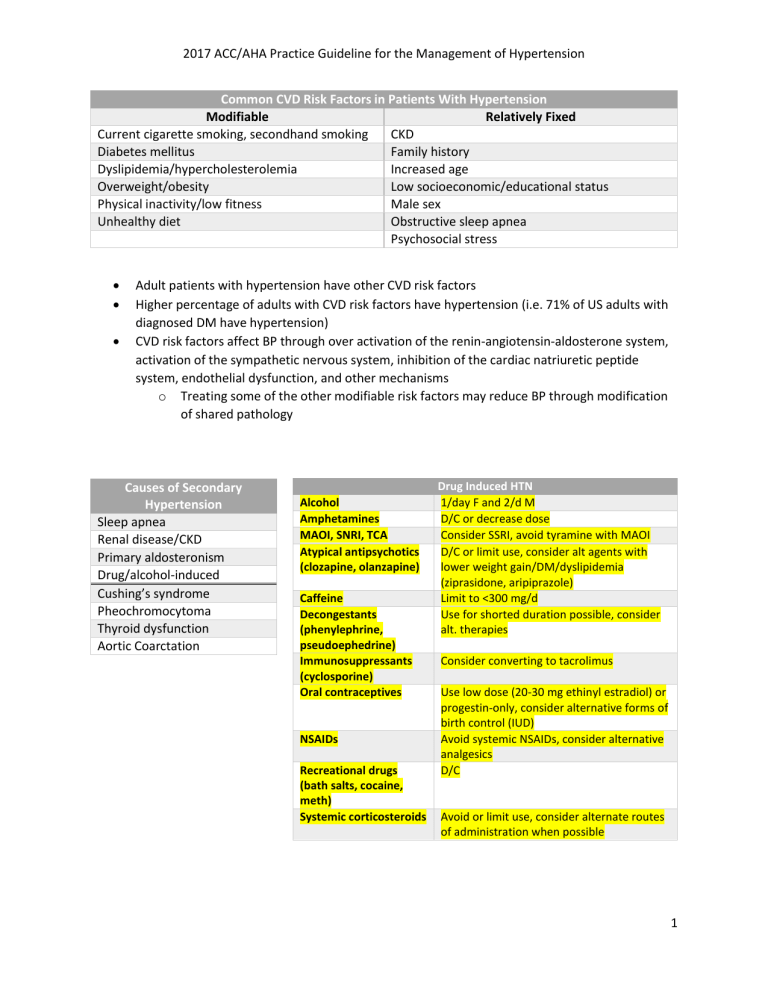
2017 ACC/AHA Practice Guideline for the Management of Hypertension Common CVD Risk Factors in Patients With Hypertension Modifiable Relatively Fixed Current cigarette smoking, secondhand smoking CKD Diabetes mellitus Family history Dyslipidemia/hypercholesterolemia Increased age Overweight/obesity Low socioeconomic/educational status Physical inactivity/low fitness Male sex Unhealthy diet Obstructive sleep apnea Psychosocial stress Adult patients with hypertension have other CVD risk factors Higher percentage of adults with CVD risk factors have hypertension (i.e. 71% of US adults with diagnosed DM have hypertension) CVD risk factors affect BP through over activation of the renin-angiotensin-aldosterone system, activation of the sympathetic nervous system, inhibition of the cardiac natriuretic peptide system, endothelial dysfunction, and other mechanisms o Treating some of the other modifiable risk factors may reduce BP through modification of shared pathology Causes of Secondary Hypertension Sleep apnea Renal disease/CKD Primary aldosteronism Drug/alcohol-induced Cushing’s syndrome Pheochromocytoma Thyroid dysfunction Aortic Coarctation Alcohol Amphetamines MAOI, SNRI, TCA Atypical antipsychotics (clozapine, olanzapine) Caffeine Decongestants (phenylephrine, pseudoephedrine) Immunosuppressants (cyclosporine) Oral contraceptives NSAIDs Recreational drugs (bath salts, cocaine, meth) Systemic corticosteroids Drug Induced HTN 1/day F and 2/d M D/C or decrease dose Consider SSRI, avoid tyramine with MAOI D/C or limit use, consider alt agents with lower weight gain/DM/dyslipidemia (ziprasidone, aripiprazole) Limit to <300 mg/d Use for shorted duration possible, consider alt. therapies Consider converting to tacrolimus Use low dose (20-30 mg ethinyl estradiol) or progestin-only, consider alternative forms of birth control (IUD) Avoid systemic NSAIDs, consider alternative analgesics D/C Avoid or limit use, consider alternate routes of administration when possible 1 2017 ACC/AHA Practice Guideline for the Management of Hypertension Step 1: Properly prepare the patient Step 2: Use proper technique for BP measurements Step 3: Take the proper measurements needed for diagnosis and treatment of elevated BP/hypertension Step 4: Properly document accurate BP readings Step 5: Average the readings Step 6: Provide BP readings to patient Accurate Blood Pressure Measurement 1. Have the patient relax, sitting in a chair (feet on floor, back supported) for >5 min. 2. The patient should avoid caffeine, exercise, and smoking for at least 30 min before measurement. 3. Ensure patient has emptied his/her bladder. 4. Neither the patient nor the observer should talk during the rest period or during the measurement. 5. Remove all clothing covering the location of cuff placement. 6. Measurements made while the patient is sitting or lying on an examining table do not fulfill these criteria. 1. Use a BP measurement device that has been validated, and ensure that the device is calibrated periodically. 2. Support the patient’s arm (eg, resting on a desk). 3. Position the middle of the cuff on the patient’s upper arm at the level of the right atrium (the midpoint of the sternum). 4. Use the correct cuff size, such that the bladder encircles 80% of the arm, and note if a larger- or smaller-than-normal cuff size is used. 5. Either the stethoscope diaphragm or bell may be used for auscultatory readings. 1. At the first visit, record BP in both arms. Use the arm that gives the higher reading for subsequent readings. 2. Separate repeated measurements by 1–2 min. 3. For auscultatory determinations, use a palpated estimate of radial pulse obliteration pressure to estimate SBP. Inflate the cuff 20–30 mm Hg above this level for an auscultatory determination of the BP level. 4. For auscultatory readings, deflate the cuff pressure 2 mm Hg per second, and listen for Korotkoff sounds. 1. Record SBP and DBP. If using the auscultatory technique, record SBP and DBP as onset of the first Korotkoff sound and disappearance of all Korotkoff sounds, respectively, using the nearest even number. 2. Note the time of most recent BP medication taken before measurements. Use an average of ≥2 readings obtained on ≥2 occasions to estimate the individual’s level of BP. Provide patients the SBP/DBP readings both verbally and in writing. Out-of-Office Blood Pressure Measurements Recommended to confirm HTN diagnosis and to titrate medications Training should occur for home blood pressure monitoring(HBPM) o Automated devices, appropriate cuff size o Remain still, avoid smoking, caffeine, exercise for 30m prior; feet on the floor; keep arm supported on flat surface 2 2017 ACC/AHA Practice Guideline for the Management of Hypertension o Take at least 2 readings 1 min apart before taking medications and in the evening before dinner o Optimally measure daily o Record all readings Ambulatory blood pressure monitoring (ABPM) is preferred method for out-of-office measurements o Monitors usually programmed to obtain readings every 15-30m during the day and every 15m-1h during the night o Can determine the nocturnal “dipping” of blood pressure and daily/nighttime patterns o Machine may be reimbursable to patients with suspected white-coat HTN and masked HTN White-coat HTN - office BP elevated (>130/80 and <160/100) but daytime ABPM or HBPM is not Masked HTN – office BP 120-129/<80 but ABPM or HBPM >130/80 Clinic 120/80 130/80 140/90 160/100 Corresponding SBP/DBP Values for Measurement Kinds HBPM Daytime ABPM Nighttime ABPM 120/80 120/80 100/65 130/80 130/80 110/65 135/85 135/85 120/70 145/90 145/90 140/85 Category Normal Elevated Hypertension Stage 1 Stage 2 Hypertensive Crisis Hypertensive Emergency Population Uncomplicated HTN Diabetes CKD Older Adults Blood Pressure Classification SBP (mmHg) < 120 And 120 – 129 And 24-hour ABPM 115/75 125/75 130/80 145/90 DBP (mmHg) < 80 < 80 130 – 139 Or 80 – 89 ≥ 140 Or ≥ 90 > 180 And/or > 120 Hypertensive crisis + evidence of acute target organ damage Blood Pressure Goals Across Guidelines ACC/AHA Other Guideline Recommendations < 130 / 80 < 130 / 80 ADA 2023 < 130 / 80 < 130 / 80 KDIGO 2021 < 120 SBP < 130 SBP ACP/AAFP 2017 General: < 150 SBP Stroke/TIA or high CV risk: < 140 SBP 3 2017 ACC/AHA Practice Guideline for the Management of Hypertension Non-Pharmacologic Treatment Treatment Weight loss DASH diet Dietary Sodium Dietary Potassium Aerobic exercise Dynamic resistance exercise Alcohol Intervention Goal: IBW; expect 1 mmHg reduction for every 1-kg lost Fruits, vegetables, wholegrains, low-fat dairy with reduced saturated and trans fats Goal: < 1500 mg/d (aim for < 1000) Goal: 3500 – 5000 mg/d 90 – 150 min/wk of 65 – 75% heart rate reserve 90 – 150 min/wk: 6 exercises at 50 – 80% 1 rep max, 3 exercises/sets with 10 reps/set M < 2; F < 1 Pharmacologic Treatment Stage 1 HTN (clinical ASCVD, 10-yr ASCVD risk > 10%, DM, CKD) Monotherapy Stage 2 HTN BP > 20/10 above goal combination therapy with 2 first-line agents 4 2017 ACC/AHA Practice Guideline for the Management of Hypertension Initial Medication Selection: First line therapies: General: Thiazide diuretics, CCB, ACE, ARB - ALLHAT: chlorthalidone, amlodipine, lisinopril no difference found in primary outcome (CVD death, nonfatal MI); chlorthalidone showed CVD benefit compared to amlodipine, lisinopril - ACCOMPLISH – benazepril/amlodipine significantly decreased primary (CV death, nonfatal MI) and secondary outcomes African American patients (w/o HF or CKD): thiazide, CCB - lower RAAS efficacy (lower circulating renin concentrations) Comorbidity specific (below) *most patients will require 2 or more medications to achieve their BP goal Recommended therapy for comorbid conditions & Special Populations Diabetes AND CKD - Albuminuria: ACE or ARB - ≥ 300 mg/d or mg/g albumin-creatinine ratio or equivalent - No albuminuria: thiazide, CCB, ACE, ARB - Kidney transplant: CCB - AVOID: non-DHP CCB HFrEF - carvedilol, metoprolol XR, bisoprolol (GDMT BB), ACE, ARB, ARNI, mineral corticoid RA, diuretics - AVOID: non-DHP CCB HFpEF - diuretic (initiate first to control volume overload), BB, ACE, ARB Stable Ischemic Heart Disease (SIHD) - ACE, ARB, BB (continue x3 year if has MI or ACS) - CCB (esp. if angina and uncontrolled HTN), thiazide or MRA can be added PRN - AVOID ISA BB Secondary Stroke Prevention - thiazide, ACE, ARB; combination thiazide + ACE A fib - ARB Aortic disease - BB PREGNANCY - Methyldopa, nifedipine, labetalol - CI : ACE, ARB, renin inhibitors - GOAL: < 120 – 160 / 80 – 105 (American College of Ob and Gyn) Resistant Hypertension - ≥ 130 / 80 despite concurrent use of 3 antihypertensives from different classes (including long acting CCB, RAAS blocker and diuretic at max tolerated doses) 5 2017 ACC/AHA Practice Guideline for the Management of Hypertension - drug-induced, nonadherence, volume overload, co-morbid conditions, secondary THN cause - optimizing drug regimens (in order) - substitute thiazide diuretic for loop diuretics - add MRA - add BB - add hydralazine - sub minoxidil for hydralazine FRIST LINE DRUGS (ACE, ARB, thiazide, CCB) Benazepril Captopril Enalapril Fosinopril Lisinopril Quinapril Ramipril ACE INHIBITORS Usual Dose Range (mg/d) 10–40 12.5–150 5–40 10–40 10–40 10–80 2.5–20 Daily Frequency 1 or 2 2 or 3 1 or 2 1 1 1 or 2 1 or 2 MOA – inhibit conversion of angiotensin I to II (angiotensin II = vasoconstrictor) Do not use in combination with ARB or direct renin inhibitor (aliskiren) (hyperkalemia risk) DDI – NSAIDs o NSAIDs constrict afferent arteriole (PG dilates), ACE/ARB dilate (ANGII constrict)efferent arteriole together filtrate does not stay in the glomerulus to be filtered when administered concomitantly DDI – may increase lithium concentrations Nephroprotective o To much circulating renin increased angiotensin II increased vasoconstriction of efferent arteriole increased glomerular pressure and damage 36h Entresto washout Benign increase in SCr (20-30% acceptable) Hyperkalemia Angioedema (less with ARBs) Cough (increased bradykinin) CI: bilateral renal artery stenosis, AKI, pregnancy (teratogenic), Hx angioedema (BBW) Ok in gout (lipid and uric acid neutral) 6 2017 ACC/AHA Practice Guideline for the Management of Hypertension Candesartan Irbesartan Losartan Olmesartan Telmisartan Valsartan ANGIOTENSIN II RECEPTOR BLOCKERS (ARB) Usual Dose Range (mg/d) Daily Frequency 8–32 1 150–300 1 50–100 1 or 2 20–40 1 20–80 1 80–320 1 MOA – selectively antagonize angiotensin II AT1 receptors Do not use in combination with ACE or direct renin inhibitor (aliskiren) (hyperkalemia risk) Olmesartan – diarrhea causing weight loss Benign increase in SCr (20-30%) acceptable Hyperkalemia Angioedema o Less than ACE o 6 week washout if angioedema with ACE before starting ARB o Normal transition = 36 h washout CI: bilateral renal artery stenosis, AKI, pregnancy (teratogenic), Hx angioedema with ARB DIHYDROPYRIDINE CALCIUM CHANNEL BLOCKERS Usual Dose Range (mg/d) Daily Frequency Amlodipine 2.5–10 1 Felodipine 2.5–10 1 Nicardipine SR 60–120 2 Nifedipine LA 30–90 1 MOA – inhibits smooth muscle calcium channels (more in vasculature than myocardium) AVOID in patients with HErEF (can use amlodipine or felodipine if required) Nicardipine XR – ghost tablet, preferred formulation (IR profound SE) Dose-related pedal/peripheral edema (more common in women) Headache, flushing, Reflex tachycardia (vasodilatory SE) Gingival hyperplasia Orthostasis Greater benefit in the African American population than RAAS inhibitors/BB Can be used in Raynaud syndrome CI: Nicardipine in aortic stenosis DDI: grapefruit (3A4) Clevidipine (IV) o Increases TG (2kcal/mL) o 3A4 DDI o CI: soy/egg allergy 7 2017 ACC/AHA Practice Guideline for the Management of Hypertension THIAZIDE/THIAZIDE-LIKE DIURETICS Usual Dose Range (mg/d) Chlorthalidone 12.5–25 Hydrochlorothiazide 25–50 Indapamide 1.25–2.5 Metolazone 2.5–5 Daily Frequency 1 1 1 1 MOA – inhibits Na/Cl reabsorption in the distal convoluted tubule Chlorthalidone currently preferred to HCTZ (longer t1/2 and proven to decrease CV death (ALLHAT)) HYPO – K, Na, Mg HYPER – Ca, BG, UA, TG/LDL CI: Anuria, sulfa Not effective with GFR < 30 CAUTION: gout or DM Osteoporosis protective (prevents urine Ca loss) OTHER AGENTS NON-DIHYDROPYRIDINE CALCIUM CHANNEL BLOCKERS Usual Dose Range (mg/d) Daily Frequency Diltiazem ER 120–360 1 Verapamil IR 120–360 3 Verapamil SR 120–360 1 or 2 Verapamil-delayed onset ER 100–300 1 (in the evening) MOA – more inhibition of calcium channels in myocardium/conduction tissue than vasculature smooth muscle Useful in patients with concomitant A Fib May be useful in migraine prophylaxis AVOID in patients with HErEF 3A4CYP INHIBITOR and SUBSTRATE o DDI - statins Bradycardia Heart/AV block Constipation Gingival hyperplasia CI: heart/AV block; sick sinus syndrome Caution: concomitant BB (increased risk of heart/AV block and bradycardia) 8 2017 ACC/AHA Practice Guideline for the Management of Hypertension Bumetanide Furosemide Torsemide Conversion Daily Frequency 2 2 1 PO 1 mg 40 mg 20 mg IV 1 mg 20 mg - MOA – inhibit the reabsorption of Na and Cl in the ascending loop of Henle and distal tubule Preferred diuretics in persons with symptomatic HF Preferred over thiazides in persons with moderate-severe CKD (GFR < 30) Bumetanide - myalgias HYPO – Ca, K, Mg, Na HYPER – BG, UA, TG Dehydration Ototoxic Orthostasis CI: Anuria Ethacrynic acid if sulfa allergy Amiloride Triamterene LOOP DIURETICS Usual Dose Range (mg/d) 0.5–2 20–80 5–10 POTASSIUM-SPARING DIURETICS Usual Dose Range (mg/d) Daily Frequency 5–10 1 or 2 50–100 1 or 2 MOA – interferes with K/Na exchange in the distal convoluted tubule ( decrease in water reabsorption and increases potassium retention) Used in combination with thiazide in patients with hypokalemia on thiazide monotherapy o Minimally effective as an antihypertensive as monotherapy HYPER – K, BG, UA AVOID: GFR < 45 CI: Anuria, hyperkalemia, severe renal or hepatic disease 9 2017 ACC/AHA Practice Guideline for the Management of Hypertension Eplerenone Spironolactone ALDOSTERONE ANTAGONISTS Usual Dose Range (mg/d) 50–100 25–100 MOA – antagonize specific aldosterone receptors ( decreased Na and water reabsorption and increased potassium retention) Preferred in primary aldosteronism and resistant HTN (add-on) Eplerenone often requires BID dosing for adequate BP control Hyperkalemia; greater risk if with an ACE; D/C if K > 5.5 Gynecomastia, impotence (spironolactone) Hirsutism (eplerenone – lower binding affinity for progesterone/androgen receptors, increased for MRA) CI: GFR < 30, Anuria, SCr > 2 for F and SCr > 2.5 M Atenolol Bisoprolol Metoprolol tartrate Metoprolol succinate Daily Frequency 1 or 2 1 BETA BLOCKERS Usual Dose Range (mg/d) 25–100 2.5–10 100–200 50–200 Daily Frequency 2 1 2 1 Not first line unless HF or ischemic heart disease Bradycardia Caution: bronchospastic disease, Raynaud’s disease Carvedilol – edema, weight gain Exercise intolerance Sexual dysfunction Fatigue Depression Cold extremities Metoprolol IV: PO 1:2.5 May mask symptoms of hypoglycemia Metoprolol XL, carvedilol – take with food, 2D6 substrates CI: AV block/dysfunction, decompensated HF, severe bronchospastic disease CI: carvedilol in severe hepatic impairment Warning: carvedilol – intraoperative floppy iris syndrome (cataract surgery) Cautions: asthma or COPD (especially non-selective; use cardio-selective agents) TAPER over 2 weeks to discontinue 10 2017 ACC/AHA Practice Guideline for the Management of Hypertension Cardio-selective (Beta 1) Alpha, non-selective beta Cardio-non-selective (beta 1 and 2) Atenolol Metoprolol Bisoprolol Nebivolol Renally cleared Succinate preferred in HFrEF Preferred in HFrEF Nitric oxide inhibition/vasodilatory no sexual dysfunction Esmolol Carvedilol Labetalol Propranolol Nadolol Sotalol Timolol Pindolol Preferred in HFrEF ISA, generally avoid DIRECT RENIN INHIBITORS Aliskiren Daily Frequency 150–300 1 MOA – directly inhibits renin High fat meals decrease absorption Unknown efficacy in renal insufficiency (excluded group in trials) hyperkalemia CI: pregnancy, in combinations with ACE or ARB (hyperkalemia increase), bilateral renal artery stenosis Doxazosin Prazosin Terazosin Usual Dose Range (mg/d) Alpha-1 blockers Usual Dose Range (mg/d) 1–16 2–20 1–20 Daily Frequency 1 2 or 3 1 or 2 MOA – antagonize peripheral alpha-1 adrenergic receptors Can be used in BPH (second line antihypertensive in patients with concomitant BPH) Dizziness and orthostasis BEER’s List Crosses BBB Start low and titrate Consider taking at bedtime (1st dose orthostasis) 11 2017 ACC/AHA Practice Guideline for the Management of Hypertension Clonidine oral Clonidine patch Methyldopa Guanfacine Daily Frequency 2 1 weekly 2 1 MOA – agonize alpha-2 in the brain ( decreased sympathetic output from vasomotor center and increased vagal tone) o Also works in the periphery ( decreased sympathetic tone = decreased HR, CO, total peripheral resistance) Generally reserved last line for HTN due to significant CNS SE (especially in elderly) Guanfacine is alpha-2a selective o ADHD Do NOT abruptly D/C (rebound hypertension) – esp. clonidine Methyldopa – DOC HTN in pregnancy Beneficial for hypertensive urgency Anticholinergic SE Dizziness and orthostasis Drowsiness Dry mouth BEER’s List Rare hepatitis (methyldopa) Avoid in PT with HF Hydralazine Minoxidil CENTRAL ALPHA-2 AGONISTS Usual Dose Range (mg/d) 0.1–0.8 0.1–0.3 250–1000 0.5–2 DIRECT VASODILATORS Usual Dose Range (mg/d) 100–200 5–100 Daily Frequency 2 or 3 1-3 Hydralazine – tachycardia (use with BB), DILI, fluid retention (use with loop diuretic), HA Minoxidil – fluid retention, pericardial effusion (use with loop diuretic), hirsutism BEER’s List 12 2017 ACC/AHA Practice Guideline for the Management of Hypertension HYPERTENSIVE CRISISES Crisis/urgency: > 180 / 120 o Usually do not require hospitalization o Should receive immediate combination oral therapy Captopril, clonidine, and labetalol o Decrease SBP by no more than 25% in the 1st hour then decrease to < 160 / 100 within the next 2-6 hours Emergency: > 180 / 20 with signs of target end organ damage o Requires hospitalization IV antihypertensives Nicardipine, clevidipine, sodium nitroprusside, nitroglycerin, esmolol, labetalol, hydralazine, fenoldopam 13