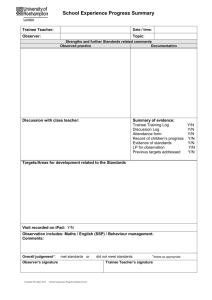
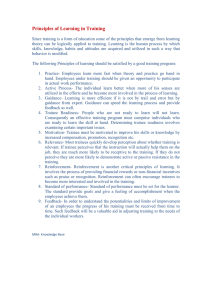
Northamptonshire diabetic eye screening service Training Programme for slit lamp bio microscopy examiner ( A) Purpose: To set up a clear, structured and repeatable training pathway for staff to learn the new skill of being able to use a slit lamp. The training plan is split into 3 segments; Introduction Training Assessment process Each section is divided into smaller steps and if at any point the training supervisor feels the trainee needs more time on a particular step or needs to go back to one or more steps, the plan can be paused and then restarted once the training supervisor is happy for the trainee to progress forwards. The aim of this plan is to be able to train a staff member who has little or no previous experience of working with a slit lamp. The outcome will be that staff is able to run slit lamp bio microscopy clinics with no supervision, whilst also achieving high standards set by both our local diabetic eye screening programme DESP and the National DESP team. This plan assumes the trainee has prior experience of digital retinal photography in addition to primary and secondary grading to National DESP grading standards. Introduction Step 1 A meeting will be arranged with the nominated training supervisor generally the Clinical lead or Consultant ophthalmologist who will talk to the trainee about the training supervisors expectations, the standards they want to see them achieve and maintain, the timescale of their training period and how they will be assessed. Step 2 The Senior Retinal Screener Grader (who are also Slit lamp bio microscopy graders) will do the initial training on how to use a slit lamp. They will cover the basics, like: How to set up the slit lamp How to focus the slit lamp ( using the focus arm) Explain what each button, nob and lever does on the slit lamp. Go through all the different lenses available, explaining how they differ from one another and when to use which one( in particular the 78D and 90) Go through the different lights available on the slit lamp and explain which is used when (narrow beam, wide beam, bright light, dull light, blue light, etc) Showing how drawing the retina as you are viewing it can help show colleagues and assessors where you have seen lesions. It is important that they understand that images are flipped and they are able to show this when recording what they see. Describing where to instruct the patient to fixate in order to view the necessary areas of the retina for grading. Training Step 3 Observer slit lamp clinic with a medical retina consultant, watch what they do, how they assess patients using the slit lamp, how they interact with the patients, what they ask the patient and if they use other information to help them grade that patient. Step 4 Then ask to see a clinician patient before or after they see them while being supervised by the clinician for advice while they kept their confidence up and become accustomed to slit lamp clinics Step 5 The training supervisor will do a training session and catch up with the trainee and assess how they are progressing and if they are ready for the next step The training supervisor should go through the differences in grading between 2D images and slit lamp. They should explain the differences in grading for maculopathy and go through how to assess for oedema and which tools are useful for this. Desired outcome: To know the differences between grading from an image and grading from slit lamp in real time and to understand different definitions concerning grading for maculopathy. Also be aware that slit lamp is less sensitive when grading for micro aneurysms and should be clear differences between IRMA and new vessels. The trainee should be able to explain different parts of the slit lamp and functionality of each part. Step 6 Then when the trainee is comfortable with the slit lamp, focus should be to understand and identify normal lids, conjunctiva and cornea and identify any abnormality. The trainee should get feedback from the clinician. The emphasis should be on making sure the trainee is able to identify the normal structures and can pick up any abnormality easily. Step 7 Focus at this stage should be on the examination of anterior segment, identification of cataract/ Pseudophakia, anterior capsule and posterior capsular opacity. Step 8 Focus at this stage should be on examination of the retina with 90 D or 78 D lens in a systemic manner starting with disc, vessels, 4 quadrants and macula. The trainee should be able to identify the normal structures and identify any abnormality. The trainee should get feedback from the clinician. When the trainee feel comfortable using the slit lamp, interacting with patients and asking them where to look, then they should progress into giving a grade and outcome for each patient they see. The trainee should be able to discuss their findings with the clinicians and should be capable of describing where and what they have seen. Step 9: Interpreting OCT images The training supervisor should explain how to interpret the OCT images and identify the macular pathology. Desired outcome: To know when it is suitable / appropriate to request OCT images. To know what to look out for, when looking at OCT images. The trainee should be able to discuss their findings with the clinicians and should be capable of describing where and what they have seen. When the trainee feels confident in their ability, they should organise a meeting with the training supervisor. Training supervisor should gather feedback from all the clinicians they have worked beside the trainee and talk to the trainee about any areas that they may need to work on. If the training supervisor is happy with the trainee’s ability they should progress to step 10, if there are areas that training supervisor feels needs to be addressed go back to step which needs to be addressed. Assessment Process Step 10 Trainee’s final assessment will include level 1 assessment, level 2A and Level 2B assessments followed by competency sign off sheet. The trainee will have to see anywhere between 15 and 30 patients with the training supervisor. The training supervisor will be having the final say whether the trainee is capable or not. Outcomes: The training supervisor passes the trainees who can then start running their own slit lamp bio microscopy clinics. The training supervisor identifies small areas that need improving. Trainee will go back to the desired step requiring improvement, but they will not have to do step 10 again. The training supervisor identifies serious concerns about trainee’s ability. The training supervisor should decide which steps trainee should go back to (1, 2, 3 etc.). If the training supervisor or the trainee, themselves feel they will never be able to perform Slit Lamp Grading to the standards required then the trainee should be taken off the training programme. Estimated total training time 18 months to 24 months