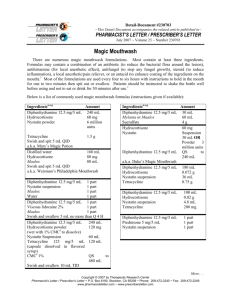
PL Detail-Document #301105 −This Detail-Document accompanies the related article published in− PHARMACIST’S LETTER / PRESCRIBER’S LETTER November 2014 Magic Mouthwash Recipes Ingredients1-11,a-e Amount Diphenhydramine 12.5 mg/5 mL 240 mL Hydrocortisone 60 mg Nystatin powder 6 million units Tetracycline 1.5 g Swish and spit 5 mL QID. a.k.a. Mary’s Magic Potion Ingredients1-11,a-e Hydrocortisone Nystatin Diphenhydramine 12.5 mg/5 mL a.k.a. Duke’s Magic Mouthwash4 Amount 60 mg Suspension 30 mL OR Powder 3 million units QS 240 mL Distilled water 160 mL Hydrocortisone 80 mg Maalox 80 mL Swish and spit 5 mL QID. a.k.a. Weisman’s Philadelphia Mouthwash Diphenhydramine 12.5 mg/5 mL Hydrocortisone Nystatin suspension Tetracycline Diphenhydramine 12.5 mg/5 mL Nystatin suspension Maalox Water Diphenhydramine 12.5 mg/5 mL Hydrocortisone Nystatin suspension Tetracycline 100 mL 0.02 g 4.8 mL 200 mg Diphenhydramine 12.5 mg/5 mL Prednisone 5 mg/5 mL Nystatin suspension 1 part 1 part 1 part Nystatin Susp. 100,000 U/mL Lidocaine Viscous 2% Distilled Water Crystal Light-Raspberry with Aspartame crystals8 83.3 mL 83.3 mL 83.3 mL 0.47 g 1 part 1 part 1 part 1 part Diphenhydramine 12.5 mg/5 mL 1 part Viscous lidocaine 2% 1 part Maalox 1 part Swish and swallow 5 mL no more than Q4H. OR For radiation oncology mucositis; palliative care: Swish, hold, and spit or swallow 30 mL Q2H.1 Diphenhydramine 12.5 mg/5 mL 240 mL Hydrocortisone powder 120 mg (wet with 1% CMCf to dissolve) Nystatin Suspension 60 mL Tetracycline 125 mg/5 mL 120 mL (capsule dissolved in flavored syrup) CMCf 1% QS 480 mL Swish and swallow 10 mL TID. Diphenhydramine 12.5 mg/5 mL Mylanta or Maalox Sucralfate Swish and spit or swallow 5 mL meals and PRN.6 30 mL 60 mL 4g TID before 180 mL 0.072 g 36 mL 0.75 g Cherry-flavored Kool-Aid mixed 100 mL with 2000 mL distilled water (sugar-free) Viscous lidocaine 2% 100 mL Nystatin suspension 100 mL Swish and spit or swallow 15 mL QID. OR For radiation oncology mucositis; palliative care: Swish, hold, and spit or swallow 30 mL Q4H.1 a.k.a. Koolstat More. . . Copyright © 2014 by Therapeutic Research Center 3120 W. March Lane, Stockton, CA 95219 ~ Phone: 209-472-2240 ~ Fax: 209-472-2249 www.PharmacistsLetter.com ~ www.PrescribersLetter.com ~ www.PharmacyTechniciansLetter.com (PL Detail-Document #301105: Page 2 of 3) Ingredients1-11,a-e Amount Hydrocortisone 100 mg/2 mL 12 mL (Solu-Cortef) Nystatin suspension 7.2 mL Tetracycline 125 mg/5 mL 12 mL (capsule dissolved in syrup) Diphenhydramine 12.5 mg /5 mL 150 mL Swish and swallow 10 mL QID. Viscous lidocaine 2% Hydrocortisone 100 mg/2 mL (Solu-Cortef) Nystatin suspension Mouth rinse Do not swallow. 250 mL 1g 150 mL QS 500 mL Diphenhydramine 12.5 mg /5 mL Dexamethasone 4 mg/mL injection Nystatin suspension Distilled water QS to 200 mL8 Swish and Spit 5 mL QID. 120 mL 0.56 mL 40 mL Viscous lidocaine 2% Cherry flavored Kool-Aid mixed with 1500 mL of sterile water for irrigation (sugar-free) 2000 mL QS 3400 mL Diphenhydramine 12.5 mg/5 mL Prednisone 5 mg/5 mL Nystatin suspension 1 part 1 part 1 part Viscous lidocaine 2% 80 mL Mylanta 80 mL Diphenhydramine 12.5 mg/5 mL 80 mL Nystatin suspension 80 mL Prednisolone 15 mg/5 mL 80 mL Distilled water 80 mL Swish, gargle, and spit 5 mL to 10 mL Q6H PRN. May be swallowed if esophageal involvement.10 Viscous lidocaine 2% 150 mL Diphenhydramine 12.5 mg/5 mL 20 mL Hydrocortisone (Solu-Cortef) 100 mg Tetracycline 2 grams Nystatin suspension 20 mL Swish, hold, and swallow 15 to 30 mL Q4-6H.1 a.k.a. Mile’s Solution Ingredients1-11,a-e Amount Viscous lidocaine 2% 30 mL Maalox 60 mL Diphenhydramine 12.5 mg/5 mL 30 mL Carafate 1 g/10 mL 40 mL Swish, gargle, and spit 5 mL to 10 mL Q6H PRN. May swallow if esophageal involvement.10 Dexamethasone 0.5 mg/5 mL 100 mL Diphenhydramine 12.5 mg/5 mL 100 mL Nystatin suspension 60 mL Tetracycline 1500 mg Swish, gargle, and spit 5 mL to 10 mL Q6H PRN. May swallow if esophageal involvement.10 a. Elixirs containing alcohol can cause stinging. Consider using injectable or powder formulation, crushing tablets, or opening capsules in place of elixir formulation to avoid stinging. b. Some U.S. clinicians have found the new formulation of Kaopectate (i.e., containing bismuth) to solidify over a short period of time when mixed with other ingredients. U.S. clinicians should consider this potential problem if utilizing recipes which use Kaopectate in place of Maalox. Canadian Kaopectate formulation does not contain bismuth. c. Nystatin has not been shown to be effective in treating oral fungal infection associated with oral mucositis.11 d. The use of corticosteroids, such as hydrocortisone or dexamethasone, has not been adequately studied to recommend its inclusion in magic mouthwash.11 e. In general, per USP standards, oral mixtures containing water should have an expiration not longer than two weeks (refrigerated) and mucosal mixtures containing water should have an expiration of not longer than 30 days (room temp).12 f. CMC=Carboxymethylcellulose. Users of this PL Detail-Document are cautioned to use their own professional judgment and consult any other necessary or appropriate sources prior to making clinical judgments based on the content of this document. Our editors have researched the information with input from experts, government agencies, and national organizations. Information and internet links in this article were current as of the date of publication.. More. . . Copyright © 2014 by Therapeutic Research Center 3120 W. March Lane, Stockton, CA 95219 ~ Phone: 209-472-2240 ~ Fax: 209-472-2249 www.PharmacistsLetter.com ~ www.PrescribersLetter.com ~ www.PharmacyTechniciansLetter.com (PL Detail-Document #301105: Page 3 of 3) Project Leaders in preparation of this PL DetailDocument: Wan-Chih Tom, Pharm.D. (Original November 2009 version); Stacy A. Hester, R.Ph., BCPS, Assistant Editor (November 2014 update) References 1. 2. 3. 4. 5. The Erie St. Clair Palliative Care Management Tool. January 2007. http://palliativecareswo.ca/PalliativeCareManagme nTool_v3.2.pdf. (Accessed October 14, 2014). Anon. Slang terms and jargon can cause medication errors. Drugs & Therapy Bulletin. Shands at the University of Florida. November/December 2005. Volume 19, Number 10. http://professionals.ufhealth.org/files/2011/11/1005drugs-therapy-bulletin.pdf. (Accessed October 14, 2014). Bulletin Board of Oral Pathology. University at Buffalo. 2007. North Carolina Board of Pharmacy. http://www.ncbop.org/faqs/Pharmacist/faq_DukesM agicMouthwash.htm. (Accessed October 14, 2014). Hodgins C, Mosley M, Pola-Strowd M. Recommendations for the diagnosis and management of recurrent aphthous stomatitis. 2003. University of Texas at Austin, School of Nursing. 6. Tarascon Pharmacopoeia. 2009 Library Edition. Ed. In Chief: Richard J. Hamilton. Jones & Bartlett. Sudbury, MA:164. 7. Department of Pharmacy Services. Mount Sinai Hospital. Toronto, Ontario MSG 1XS. October 2009. 8. Toronto Sunnybrook Regional Cancer Centre Pharmacy. Toronto, Ontario M4N 3M5. October 2009. 9. Drug Information and Research Centre. Ontario Pharmacist’s Association. October 2009. 10. Randy Otterholt, DDS General Dentistry. http://www.drotterholt.com/magicmouthwash.html. (Accessed October 14, 2014). 11. Chan A, Ignoffo RJ. Survey of topical oral solutions for the treatment of chemo-induced oral mucositis. J Oncol Pharm Pract 2005;11:139-43. 12. Chapter 795 Pharmaceutical Compounding-Nonsterile Preparations. The United States Pharmacopeia and The National Formulary (USPNF). http://www.usp.org/sites/default/files/usp_pdf/EN/gc 795.pdf. (Accessed October 14, 2014). Cite this document as follows: PL Detail-Document, Magic Mouthwash Recipes. Letter/Prescriber’s Letter. November 2014. Pharmacist’s Evidence and Recommendations You Can Trust… 3120 West March Lane, Stockton, CA 95219 ~ TEL (209) 472-2240 ~ FAX (209) 472-2249 Copyright 2014 by Therapeutic Research Center Subscribers to the Letter can get PL Detail-Documents, like this one, on any topic covered in any issue by going to www.PharmacistsLetter.com, www.PrescribersLetter.com, or www.PharmacyTechniciansLetter.com PL Detail-Document #301105 −This PL Detail-Document gives subscribers additional insight related to the Recommendations published in− PHARMACIST’S LETTER / PRESCRIBER’S LETTER November 2014 Prevention and Treatment of Oral Mucositis Oral mucositis is mucosal ulceration caused by chemotherapy or radiation treatment. Mucositis can affect not only the mouth, but also the pharyngeal, laryngeal, and esophageal areas.1 Mucositis is usually very painful and can be slow to heal.1-3 It can reduce an individual’s ability to tolerate cancer treatment, maintain nutritional intake (e.g., drink, eat, swallow), or speak.1,4 Treatment guidelines have been developed for prevention and treatment of oral mucositis by the Multinational Association of Supportive Care in Cancer (MASCC)/International Society of Oral Oncology (ISOO) (http://www.mascc.org/assets/Guidelines-Tools/mascc%20isoo%20mucositis%20guidelines%20summary%201feb2014.pdf). The National Cancer Institute (NCI) also provides recommendations (http://www.cancer.gov/cancertopics/pdq/supportivecare/oralcomplications /HealthProfessional/page5) as does the National Comprehensive Cancer Network (NCCN, http://www.nccn.org/JNCCN/PDF/mucositis_2008.pdf). Stomatitis is a term that is sometimes used interchangeably with mucositis, but is actually more general and describes any inflammatory condition of oral tissue.2 Canker sores are also different from oral mucositis. Their cause is unclear but they tend to be recurrent and triggered by factors such as smoking, stress, etc. For more info on treatment of canker sores, go to our PL Detail-Document, Treatment of Canker Sores. The following chart lists commonly asked questions about the treatment of oral mucositis. Keep in mind that the effectiveness of interventions may depend on factors such as treatments and the type of cancer being treated. QUESTION How can oral mucositis be prevented? ANSWER What nondrug therapies can be recommended for patients with oral mucositis? Proper oral hygiene can help minimize severity of oral mucositis.1,2 Holding ice chips in the mouth, or cryotherapy, during treatment may help prevent mucositis in some situations.1,3,12 Oral zinc supplements may be helpful in some patients.1 Rx palifermin (Kepivance) is FDA- and Health Canada-approved for prevention of oral mucositis in certain oncology patients.1,2 It can reduce severity and duration of mucositis.5 Maintain proper oral hygiene, such as brushing the teeth with a soft-bristle toothbrush and flossing with gentle irrigation using a water flosser on a low setting.1,5 Avoid irritating foods or beverages (e.g., dry, salty, acidic, hard, hot).5 Rinsing frequently, such as every four hours or between medicated mouth rinse doses, with a bland solution, such as one teaspoon of table salt in 32 oz. (1 L) of water (to make 0.9% sodium chloride) with or without one to two tablespoons of sodium bicarbonate, can be tried.1,2,5,12 This mixture can be used at room temperature or refrigerated. The patient should rinse and swish then spit.2 (Note that experts suggest that patients who use well water make their salt solution with bottled water instead.) More. . . Copyright © 2014 by Therapeutic Research Center 3120 W. March Lane, Stockton, CA 95219 ~ Phone: 209-472-2240 ~ Fax: 209-472-2249 www.PharmacistsLetter.com ~ www.PrescribersLetter.com ~ www.PharmacyTechniciansLetter.com (PL Detail-Document #301105: Page 2 of 5) QUESTION What are some commercially available treatments for oral mucositis? ANSWER What are some common ingredients of compounded “magic mouthwash”? What is the rationale for these? How effective is magic mouthwash? Continued An OTC antacid liquid (e.g., Amphojel) or film-forming agent (e.g., Zilactin) can be tried.2 Rx oral protectants (e.g., Episil, Gelclair [alcohol-free], and MuGard-all U.S. only) may be more convenient than OTC products.2 However, they can cost $100/week or more.5 Commercial kits for compounding “magic mouthwash” are available in the U.S. These include: o First-Mouthwash BLM (diphenhydramine, lidocaine, aluminum/magnesium hydroxide) o First-BXN Mouthwash (diphenhydramine, lidocaine, nystatin) o First-Duke’s Mouthwash (diphenhydramine, hydrocortisone, nystatin) o First-Mary’s Mouthwash (diphenhydramine, hydrocortisone, nystatin, tetracycline) Magic mouthwash kits might be easier to e-prescribe and bill for than compounded products. However, kits are typically about three times more expensive than mixing the mouthwash from scratch using individual ingredients (approximately $25 to $40 vs $5 to $15), and kits only come in specific combinations and concentrations.6 The logic behind “magic mouthwash” is to combine ingredients with different mechanisms of action.5 There are numerous magic mouthwash formulations. Most have at least three ingredients. Recipes may contain a combination of an antibiotic (to reduce the bacterial flora around the lesion), antihistamine (for local anesthetic effect), antifungal (to stop any fungal growth), steroid (to reduce inflammation), a local anesthetic/pain reliever, or an antacid (to enhance coating of the ingredients on the mouth).7 Common ingredients of magic mouthwash recipes include viscous lidocaine, diphenhydramine, milk of magnesia, kaolin with pectin, and aluminum/magnesium hydroxide.2 The most popular magic mouthwash formulation includes viscous lidocaine and diphenhydramine plus aluminum/magnesium hydroxide to help ingredients coat the mouth. There is a lack of controlled studies to evaluate the efficacy of the many different magic mouthwash recipes. Whether one recipe is more effective than another is unknown.8,12 The 2004 guidelines for the treatment of oral mucositis suggest that magic mouthwashes (with various combinations of viscous lidocaine, benzocaine, milk of magnesia, kaolin-pectin, chlorhexidine, or diphenhydramine) are no better than normal saline solution in pain relief.9 In addition, a Cochrane review found magic mouthwash (containing lidocaine, diphenhydramine, and aluminum hydroxide) to be ineffective in shortening the healing time of oral mucositis related to cancer therapies.10 There is also concern about the absorption of anesthetics such as lidocaine when used on damaged mucosa.9 Although frequently used as an ingredient of magic mouthwash, nystatin has not been shown to be effective in treating oral fungal infection associated with mucositis.7 It is also suggested that the high sugar content of nystatin suspension may feed the fungus.8 Corticosteroids have not been studied adequately to be recommended as an ingredient of magic mouthwash, and More. . . Copyright © 2014 by Therapeutic Research Center 3120 W. March Lane, Stockton, CA 95219 ~ Phone: 209-472-2240 ~ Fax: 209-472-2249 www.PharmacistsLetter.com ~ www.PrescribersLetter.com ~ www.PharmacyTechniciansLetter.com (PL Detail-Document #301105: Page 3 of 5) QUESTION ANSWER continued How effective is magic mouthwash? Where can I find recipes for magic mouthwash? What are some tips for compounding magic mouthwash? What are some tips for billing compounded magic mouthwash products? Continued there’s concern that long-term use may lead to oral candidiasis. Despite the lack of evidence that magic mouthwashes work in decreasing the pain associated with chemotherapy/radiation-induced mucositis, canker sores, or other oral pain conditions, many patients and prescribers continue to use them. There is a need to standardize the ingredients used to compound magic mouthwash in order to fully evaluate efficacy. We have a number of different recipes in our PL Chart, Magic Mouthwash Recipes. Most formulations are used every four to six hours with instructions to hold in the mouth for one to two minutes then spit out or swallow. (Those with lidocaine should be spit out.)12 Patients should be instructed not to eat or drink for 30 minutes after use.7 Focal application should be used when possible, instead of widespread topical administration.2 When compounding these mixtures, try to avoid using elixir formulations as the alcohol content can cause stinging. Consider injectable or bulk powder formulations, crushed tablets, or opened capsules if needed. In some cases injectable formulations are used in place of elixirs. Some U.S. clinicians have found the new formulation of Kaopectate (i.e., containing bismuth) to solidify over a short period of time when mixed with other ingredients. U.S. clinicians should consider this potential problem if utilizing recipes which use Kaopectate in the place of Maalox. Canadian Kaopectate formulation does not contain bismuth. The combination of lidocaine and sucralfate in magic mouthwash may not be compatible in some recipes. Some clinicians report the formation of a thick gel when the two ingredients are mixed. Prior to dispensing magic mouthwash, pharmacists should verify the formula and patient allergies. Patients should be counseled regarding the proper use of magic mouthwash (e.g., to shake well before use, hold in mouth for a minute or two, whether to swallow or not, etc). Billing for magic mouthwash is not straightforward and varies among different pharmacies. There is no single NDC number that can be used to bill for magic mouthwash mixed from individual ingredients. In addition, some of the ingredients used in the magic mouthwash are OTC products, which may not be covered by some insurances. Some pharmacists are left with the option of billing for a single prescription ingredient used for the compound and for the full bottle used since billing a partial bottle is not allowed by insurance companies. Some pharmacists have the patient pay cash. In some cases, the dispensing software allows the pharmacist to enter each ingredient used and the cost of each ingredient for billing. In other cases, pharmacists may choose to bill each ingredient separately as separate prescriptions. The magic mouthwash compounding kits each come with a single unique NDC number accounting for all the ingredients, which can make billing less complicated in some cases. It may be easier to compound with these kits More. . . Copyright © 2014 by Therapeutic Research Center 3120 W. March Lane, Stockton, CA 95219 ~ Phone: 209-472-2240 ~ Fax: 209-472-2249 www.PharmacistsLetter.com ~ www.PrescribersLetter.com ~ www.PharmacyTechniciansLetter.com (PL Detail-Document #301105: Page 4 of 5) QUESTION ANSWER continued What are some tips for billing compounded magic mouthwash products? than having to measure and mix each individual ingredient. These compounding kits have also gone through stability testing and have specified stability duration for an expiration date. Lastly, these mouthwashes have added flavors and may be better tasting than mouthwashes compounded from scratch. Check insurance coverage before assembling the kit. Medicare and Medicaid coverage may be spotty because these are compounding kits, not approved drug products. However, some managed plans may still cover the kits. Prescribers should specify mouthwash kits by brand name or specify the magic mouthwash formula. What beyond-use date should be assigned to compounded magic mouthwash products? Beyond-use dates of these mixtures can vary depending on the ingredients and their individual expiration dates. In general, per USP standards, if a mixture contains water and is a mucosal liquid, the beyond-use date should not be longer than 30 days (room temperature).7,11 Oral mixtures containing water should have an expiration not longer than two weeks (refrigerated).11 How should pain from oral mucositis be managed? Start with topical anesthetics such as topical lidocaine, 0.5% doxepin mouth rinse, or diphenhydramine mouth rinse.1,2 Keep in mind most magic mouthwash recipes contain a topical anesthetic. If topical anesthetics don’t provide relief, consider opioids such as an alcohol-free morphine solution to swish and swallow, transdermal fentanyl, PCA morphine, etc.1,2,5 What treatments for oral mucositis should actually be avoided? Avoid sucralfate or chlorhexidine, because they aren’t likely to help.1,3,4 Also avoid alcohol-based mouth rinses, which can increase pain.12 Avoid using hydrogen peroxide solutions (e.g., 3% hydrogen peroxide diluted 1:1 with water or normal saline) for more than two days. These may help remove oral debris, but longer periods of use can slow healing.2 Users of this PL Detail-Document are cautioned to use their own professional judgment and consult any other necessary or appropriate sources prior to making clinical judgments based on the content of this document. Our editors have researched the information with input from experts, government agencies, and national organizations. Information and internet links in this article were current as of the date of publication. More. . . Copyright © 2014 by Therapeutic Research Center 3120 W. March Lane, Stockton, CA 95219 ~ Phone: 209-472-2240 ~ Fax: 209-472-2249 www.PharmacistsLetter.com ~ www.PrescribersLetter.com ~ www.PharmacyTechniciansLetter.com (PL Detail-Document #301105: Page 5 of 5) Project Leader in preparation of this PL DetailDocument: Stacy A. Hester, R.Ph., BCPS, Assistant Editor References 1. 2. 3. 4. 5. 6. Lalla RV, Bowen J, Barasch A, et al. MASCC/ISOO clinical practice guidelines for the management of mucositis secondary to cancer therapy. Cancer 2014;120:1453-61. NCI. Oral mucositis. http://www.cancer.gov/cancertopics/pdq/supportivec are/oralcomplications/HealthProfessional/page5. (Accessed October 8, 2014). Worthington HV, Clarkson JE, Bryan G, et al. Interventions for preventing oral mucositis for patients with cancer receiving treatment (Review). Cochrane Database Syst Rev 2011;(4):CD000978. Clarkson JE, Worthington HV, Furness S, et al. Interventions for treating oral mucositis for patients with cancer receiving treatment. Cochrane Database Syst Rev 2010;(4):CD001973. Negrin RS, Bedard J, Toljanic JA. Oral toxicity associated with chemotherapy. Last updated September 12, 2014. In UpToDate, Basow DS (ed), UpToDate, Waltham, MA 02013. Cutis Pharmaceuticals. http://www.cutispharma.com. (Accessed October 9, 2014). 7. Chan A, Ignoffo RJ. Survey of topical oral solutions for the treatment of chemo-induced oral mucositis. J Oncol Pharm Pract 2005;11:139-43. 8. Dodd MJ, Dibble SL, Miaskowski C, et al. Randomized clinical trial of the effectiveness of 3 commonly used mouthwashes to treat chemotherapy-induced mucositis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000;90:39-47. 9. Rubenstein EB, Peterson DE, Schubert M, et al. Clinical practice guidelines for the prevention and treatment of cancer therapy-induced oral and gastrointestinal mucositis. Cancer 2004;100(9 Suppl):2026-46. 10. Clarkson JE, Worthington HV, Eden OB. Interventions for treating oral mucositis for patients with cancer receiving treatment. Cochrane Database Syst Rev 2007;(2):CD001973. 11. <795> Pharmaceutical Compounding--Nonsterile Preparations. The United States Pharmacopeia and The National Formulary (USP-NF). http://www.usp.org/sites/default/files/usp_pdf/EN/gc7 95.pdf. (Accessed October 9, 2014). 12. Bensinger W, Schubert M, Ang K, et al. NCCN task force report: prevention and management of mucositis in cancer care. January 2008. http://www.nccn.org/JNCCN/PDF/mucositis_2008.pd f. (Accessed October 10, 2014). Cite this document as follows: PL Detail-Document, Prevention and Treatment of Oral Mucositis. Pharmacist’s Letter/Prescriber’s Letter. November 2014. Evidence and Recommendations You Can Trust… 3120 West March Lane, Stockton, CA 95219 ~ TEL (209) 472-2240 ~ FAX (209) 472-2249 Copyright 2014 by Therapeutic Research Center Subscribers to the Letter can get PL Detail-Documents, like this one, on any topic covered in any issue by going to www.PharmacistsLetter.com, www.PrescribersLetter.com, or www.PharmacyTechniciansLetter.com