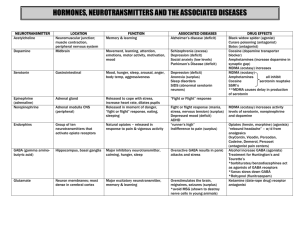
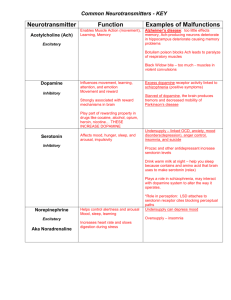
The Role of Neurotransmitter Imbalances in Abnormal Behavior and Mental Health. I. Neurotransmitter Imbalances and Abnormal Behavior a) The impact of serotonin imbalances on abnormal behavior. Serotonin, also known as the "feel-good" neurotransmitter, plays a vital role in mood regulation, sleeping habits, and appetite. Imbalances in serotonin levels have been linked to various abnormal behaviors, particularly those related to mood disorders (Ressler and Nemeroff, 2000). For example, major depressive disorder (MDD) has an associated etiology with reduced serotonin activity in the brain (Albert et al., 2019). Serotonin regulates the brain's response to emotional stimuli, and therefore, low levels of this neurotransmitter can lead to persistent feelings of sadness, emptiness, and worthlessness, characterizing depression (Shevchuk, 2008). Moreover, serotonin imbalances also play a part in anxiety disorders. The amygdala, a brain region responsible for processing emotions, receives inputs from serotonin neurons. Hence, low serotonin activity in the amygdala may result in heightened fear responses and exaggerated anxiety reactions to stressors. Disorders such as generalized anxiety disorder and social anxiety disorder have been linked to dysregulation in serotonin levels (Albert et al., 2019). b) The impact of dopamine imbalances on abnormal behavior Dopamine is related to the reward system of the brain, encouraging activities that result in pleasure and satisfaction. Dopamine imbalances have been linked to a variety of aberrant behaviors, including addiction, attention deficit hyperactivity disorder (ADHD), and schizophrenia (Blum et al., 2022). Substances such as narcotics or alcohol may trigger an increase in dopamine release, resulting in a powerful reinforcing mechanism. Individuals may get addicted to these substances over time as their brains relate them with emotions of pleasure and reward (Fiorillo et al., 2018). Similarly, dopamine imbalances can support behavioral addictions such as gambling or gaming. In the case of ADHD, reduced dopamine activity in the prefrontal cortex is thought to affect attention, impulse control, and working memory (Fiorillo et al., 2018). This can lead to symptoms such as difficulty in staying focused, impulsivity, and hyperactivity. Schizophrenia, a serious psychological disorder, has also been attributed to dopamine signaling abnormalities. According to the dopamine hypothesis, an excess of dopamine in certain parts of the brain, particularly the mesolimbic pathway, contributes to positive symptoms of schizophrenia such as delusions and hallucinations (Howes & Kapur, 2009). Negative symptoms and cognitive deficiencies in schizophrenia, on the other hand, may be caused by decreased dopaminergic activity in other brain regions, such as the prefrontal cortex. c) The role of gamma-aminobutyric acid (GABA) in abnormal behavior. GABA is the primary inhibitory neurotransmitter in the brain, performing an essential role in preserving a balance between excitation and inhibition. GABA levels that are outside of balance have been associated to a variety of aberrant behaviors, including anxiety disorders, epilepsy, and insomnia (Gasmi et al., 2022). GABA's inhibitory properties help moderate the brain's response to fear-inducing events in anxiety disorders. Reduced GABA activity can result in a hyperactive amygdala, which leads to increased anxiety in response to stimuli (Gupta et al., 2020). Benzodiazepines, which increase GABA activity, are often used to promote relaxation and lessen anxiety symptoms in the treatment of anxiety disorders. GABA imbalances have also been linked to epilepsy, a neurological condition marked by recurring seizures. GABAergic transmission is critical in preventing abnormal neuronal excitation, and a lack of GABA can result in seizure activity (Treiman, 2001). On the other hand, GABA abnormalities have also been related to insomnia, a sleep disease characterized by difficulty sleeping or staying asleep. GABAergic transmission is required for promoting restful sleep by decreasing brain activity. Reduced GABA levels may result in hyperarousal and difficulty falling asleep (Treiman, 2001). II. Neurotransmitter Imbalances and Mental Health Problems a) Depression and neurotransmitter imbalances Depression is a complex mental health illness marked by persistent poor mood, lack of enthusiasm or enjoyment in activities, and a sense of worthlessness or guilt. To explain the function of neurotransmitter imbalances in depression, the monoamine hypothesis has long been looked at. According to this theory, serotonin, norepinephrine, and dopamine imbalances lead to the onset of depression (Zakaria et al., 2022). Antidepressants, including selective serotonin reuptake inhibitors (SSRIs), are designed to boost serotonin levels in the brain in such a situation. By blocking serotonin reuptake, SSRIs increase its availability in synapses, potentially relieving depressive symptoms. Furthermore, norepinephrine regulates attention, motivation, and arousal, where as abnormalities in this neurotransmitter may contribute to the loss of energy and motivation that is frequent in depression (Arias et al., 2021). b) Anxiety disorders and neurotransmitter dysregulation Anxiety disorders are a type of mental illness characterized by extreme worry, nervousness, and apprehension. Anxiety disorders are directly linked to neurotransmitter dysregulation, particularly affecting GABA, serotonin, and norepinephrine (Slee. 2022). As previously stated, GABA plays a crucial role in regulating excessive neuronal activation, and this helps in the regulation of anxiety reactions. Reduced GABA activity in the brain can lead to increased excitability, which can contribute to anxiety disorders (Gupta et al., 2020). Due to its involvement in moderating responses to fear, serotonin, which is also involved in mood regulation, is linked to anxiety. A serotonin imbalance can cause an excessive and uncontrollable reaction to perceived threats. Norepinephrine participates in the fight-or-flight response and helps to activate the physiological stress response. Increased norepinephrine levels may lead to increased alertness and a state of perpetual focus, which are symptoms of certain anxiety disorders (Stein et al., 2021). c) Schizophrenia and dopamine dysregulation Schizophrenia is another devastating mental illness that affects how people regulate their thoughts, emotions, and perceive reality. One of the primary hypotheses in understanding the neurochemical foundation of schizophrenia is dopamine dysregulation (Pan, 2022). According to Howes and Kapur (2009), the dopamine hypothesis proposes that a surplus of dopamine in particular parts of the brain, particularly the mesolimbic pathway, leads to the positive symptoms of schizophrenia. Positive symptoms are experiences or behaviors that are not present in healthy people but are present in people suffering from schizophrenia, such as hallucinations and delusions. On the other hand, negative symptoms and cognitive deficiencies in schizophrenia, may be connected with decreased dopamine activity in other brain regions, such as the prefrontal cortex. These regions are in charge of executive activities including decision-making processes, planning, and working memory. Reduced dopamine levels in these areas can cause cognitive deficits and information processing concerns (Howes and Kapur, 2009). III. Conclusion Neurotransmitter abnormalities play an important role in the development and maintenance of aberrant behavior and contribute significantly to various mental health issues. The complicated interplay of serotonin, dopamine, GABA, and other neurotransmitters impacts many aspects of cognitive function, behavior, and emotional regulation. Recognizing the role of neurotransmitter imbalances in abnormal behavior and mental health facilitates the development of targeted therapeutic interventions that specialize in restoring balance and improving the quality of life of individuals affected by such disorders. List of References Albert, P. R., Le François, B., & Vahid-Ansari, F. (2019). Genetic, epigenetic and posttranscriptional mechanisms for treatment of major depression: the 5-HT1A receptor gene as a paradigm. Journal of psychiatry and neuroscience, 44(3), 164-176. Arias, H. R., Targowska-Duda, K. M., García-Colunga, J., & Ortells, M. O. (2021). Is the antidepressant activity of selective serotonin reuptake inhibitors mediated by nicotinic acetylcholine receptors?. Molecules, 26(8), 2149. Blum, K., Dennen, C. A., Elman, I., Bowirrat, A., Thanos, P. K., Badgaiyan, R. D., ... & Gold, M. S. (2022). Should reward deficiency syndrome (RDS) be considered an umbrella disorder for mental illness and associated genetic and epigenetic induced dysregulation of brain reward circuitry?. Journal of Personalized Medicine, 12(10), 1719. Fiorillo, C. D., Tobler, P. N., & Schultz, W. (2018). Discrete coding of reward probability and uncertainty by dopamine neurons. Science, 299(5614), 1898-1902. Gasmi, A., Nasreen, A., Menzel, A., Gasmi Benahmed, A., Pivina, L., Noor, S., ... & Bjørklund, G. (2022). Neurotransmitters Regulation and Food Intake: The Role of Dietary Sources in Neurotransmission. Molecules, 28(1), 210. Gupta, D., Radhakrishnan, M., & Chadda, R. K. (2020). Gamma-aminobutyric acid and glutamate in anxiety and depression: A focus on GABA-ergic and glutamatergic interplay. Indian Journal of Psychiatry, 62(1), S50-S56. Howes, O. D., & Kapur, S. (2009). The dopamine hypothesis of schizophrenia: Version III—the final common pathway. Schizophrenia Bulletin, 35(3), 549-562. Pan, J. (2022, July). An overview of Schizophrenia treatment options. In AIP Conference Proceedings (Vol. 2511, No. 1). AIP Publishing. Ressler, K. J., & Nemeroff, C. B. (2000). Role of serotonergic and noradrenergic systems in the pathophysiology of depression and anxiety disorders. Depression and anxiety, 12(S1), 2-19. Shevchuk, N. A. (2008). Adapted cold shower as a potential treatment for depression. Medical hypotheses, 70(5), 995-1001. Slee, A. (2022). Generalised Anxiety Disorder: Incidence and Drug Treatment (Doctoral dissertation, UCL (University College London)). Stein, D. J., Craske, M. G., Rothbaum, B. O., Chamberlain, S. R., Fineberg, N. A., Choi, K. W., & Maj, M. (2021). The clinical characterization of the adult patient with an anxiety or related disorder aimed at personalization of management. World Psychiatry, 20(3), 336-356. Zakaria, F. H., Samhani, I., Mustafa, M. Z., & Shafin, N. (2022). Pathophysiology of Depression: Stingless Bee Honey Promising as an Antidepressant. Molecules, 27(16), 5091.