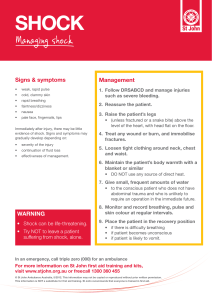
Shock, Sepsis, and Multiple Organ Dysfunction Syndrome Nurse sarah professor Shock • Characterized by decreased tissue perfusion and impaired cellular metabolism • Imbalance of O2 supply and demand • Continuous demand for O2 and nutrient supply at cellular level • Low supply of O2 and nutrition leads to cell necrosis, organ damage, and failure. • Metabolic and hemodynamic instability • Drop in blood pressure! • DON’T MATTER WHAT TYPE OF SHOCK, BP WILL BE LOW Classification of shock 1. Cardiogenic Shock (weak heart) – MI. Cardiomyopathy 1. Cause of the shock is cardio related 2. Heart cannot pump enough blood to meet body perfusion 3. Why: filling/ contraction dysfunction 4. Volume is not an issue 5. Pumping issue to maintain cardiac output 2. Hypovolemic Shock (fluid loss) – Hemorrhage 1. Low blood volume causes low bp • Blood loss • Vomiting ect 3. Distribution Shock: vasodilation (video on pp) • Neurogenic Shock – Spinal Cord Injury (SCI) 1. Sympathetic tone is lose cause vasodilation and hypertension • Anaphylactic Shock – insect bites, anesthetics, vaccines, contrast media, snake venom • Septic Shock – PNA, Peritonitis, Cholangitis 1. Systemic cytokine release 4. Obstructive Shock – Cardiac tamponade, Pneumothorax, SVC Syndrome Stages of shock (ICPR) 1. Initial Stage Occurs at cellular level and is usually not clinically apparent Metabolism changes at cellular level from aerobic to anaerobic, causing lactic acid buildup Cell switches from aerobic to anaerobic metabolism, producing lactic acid s/s (are subtle) lactic acid build up (> 4mmol/l) decreased cardiac output 2. Compensatory Stage Classic sign of shock: drop in BP Elevated lactic acid Decreased cardiac output Body activates neural, hormonal, and biochemical compensatory mechanisms to overcome the increasing consequences of anaerobic metabolism and to maintain homeostasis body will try to compensate and will release biochemical hormones to increase tissue perfusion (norepi and epi vasoconstriction) perfusion from nonvital organs move to more vital organs arterial pressure decreases and a decrease in hydrostatic pressure hydrostatic pressure: amount of pressure that blood exerts in capillary wall. Fluid moves from interstitial space to intravascular space, increasing venous blood return to heart Kidneys activate renin angiotensin system (RAS) Renin stimulates angiotensin 1 to angiotensin 2 (vasoconstrictor) Increases CO and Perfusion to cell and helps with venous return Adrenal cortex senses angiotensin 2 and releases aldosterone Aldosterone retains sodium and water Urine will have high osmolality, body will release ADH in response to aldosterone to retain fluid Gi system Skin Lungs Low perfusion Low perfusion Low perfusion Decreased peristalsis Cool, moist pale Decrease O2 level Increase rr 3. Progressive Stage (body system failure) I. Body can no longer compensate and body system are failing II. Progressing to Multi organ dysfunction syndrome / death III. No more compensation drop in Cardiac output drop in tissue perfusion drop in O2 cells die (hypoxic injury) capillary permeability increases drop in bp fluid spills into interstitial space causing edema IV. Presentation Neuro Lungs Heart Map < 60 ards Cells not being perfused muscle die Neuro changes: slow speech, Edema in lungs crackles AMI confusion, agitation, decreased reaction Respiratory failure (mechanical Dysrhythmia (vtach vfib) ventilation) Kidney Gut liver Renal failure Loses protective chemicals DIC Decreased urine output Ulcers, gi bleeding ^ bun, creat, Patients must be moved to the intensive care unit (ICU) for advanced monitoring and treatment Cardiovascular system is profoundly affected Anasarca – diffused profound edema Sustained hypoperfusion results in weak peripheral pulses, and ischemia of the distal extremities eventually occurs Pulmonary system is often the first system to display signs of critical dysfunction GI system is also affected by prolonged decreased tissue perfusion Effect of prolonged hypoperfusion on the kidneys is renal tubular ischemia 4. Refractory Stage (unmanageable) Final stage of shock Decreased perfusion from peripheral vasoconstriction and decreased CO exacerbate anaerobic metabolism Patient demonstrates profound hypotension and hypoxemia • SIRS, SEPIS, SEPTIC SHOCK, MODS SIRS • • • • • • • Systemic Inflammatory Response Syndrome (SIRS) • Inflammation all over the body, causing systemic inflammation. • Most common is sepsis • Main treatment will be antibiotic systemic inflammatory response to a variety of insults, including infection inflammation in organs remote from the initial insult characterizes SIRS • usually distal injury then spreads to rest of body Causes: • Burns, crush injuries, surgical procedures • Abscess formation • Ischemic or necrotic tissue: Pancreatitis, vascular disease, • Microbial invasion: Bacteria (main cause), viruses (rarely), fungi (rarely), parasites Sepsis pathophysiology map When there is an infection in the body, the immune system releases cytokines to fight infection • Cytokines can cause vasodilation (explains low bp in septic shock) • Large amounts of cytokines cause blood to clot • • • • Platelets and clotting factors decrease What 2 things drops bp in septic shock? • vasodilation and increased cap permeability • Administer pressors • 4 processes that causes decreased o2 delivery to body? peripheral vasodilation, increased permeability, micro emboli, Stages of shock 1. Initial Stage Occurs at cellular level and is usually not clinically apparent Metabolism changes at cellular level from aerobic to anaerobic, causing lactic acid buildup 2. Compensatory Stage Body activates neural, hormonal, and biochemical compensatory mechanisms to overcome the increasing consequences of anaerobic metabolism and to maintain homeostasis Classic sign of shock: drop in BP 3. Progressive Stage Patients must be moved to the intensive care unit (ICU) for advanced monitoring and treatment Cardiovascular system is profoundly affected Anasarca – diffused profound edema Sustained hypoperfusion results in weak peripheral pulses, and ischemia of the distal extremities eventually occurs Pulmonary system is often the first system to display signs of critical dysfunction GI system is also affected by prolonged decreased tissue perfusion Effect of prolonged hypoperfusion on the kidneys is renal tubular ischemia • 4. Refractory Stage Final stage of shock Decreased perfusion from peripheral vasoconstriction and decreased CO exacerbate anaerobic metabolism Patient demonstrates profound hypotension and hypoxemia Clinical manifestations • Organ System • Signs and Symptoms • Cardiovascular • • • • • ↓/↑ Temperature (high or low in sepsis, swinging of temp) Myocardial dysfunction (drop in by, low CO, ect) Biventricular dilation (sluggish blood flow creates dilation in ventricles) ↓ Ejection fraction (measures strength of Heart muscle via echo) weak (60-70%) • • • • • • Hyperventilation Crackles Respiratory alkalosis → respiratory acidosis Hypoxemia (low o2 in blood) Respiratory failure ARDS • Respiratory • Pulmonary hypertension • Renal • ↓ Urine output • Neurologic • • • Alteration in mental status (e.g., confusion) Agitation Coma (late) • G.I. • • GI bleeding Paralytic ileus • sepsusvDiagnostic Markers • • • • • • • • • ↑/↓ WBC, ↓ Platelets, ↑ Lactate, ↑ Blood glucose (cortisol helps wbc, but also increases bgc) ↑ Procalcitonin (released in tissue injury or infection) ↑ Urine specific gravity 1.005 to 1.030 (normal specific gravity) 1.001 after drinking excessive amounts of water (diluted) More than 1.030 after avoiding fluids (concentrated) ↓ Urine Na+ Positive blood cultures (48 to 72 hrs) • • Complete blood count( must know) • • Parameter • Unit of Measurement • WBC • K/UL • Hemoglobin • • Hematocrit • Normal Value g/dL • • • 4.0-10.0 In sepsis < 4 or > 10 12.0-16.0 • % • 37-47 Platelets • x 10 / L • 150,000-400,000 • WBC • K/UL • 4.0-10. • Hemoglobin • g/dL • 12.0-16.0 • Basal metabolic panel • • Parameter Normal Value • Glucose • 65-100 mg/dl • CO2 • 22-26 mEq/L • AGAP • 3-10 mEq/L • BUN (break down body products) • Creatinine • • • 8-25 mg/dl In sepsis it goes up 0.8-1.4 mg/dl • Sodium • 135-145 mEq/L • Potassium • 3.5-5.0 mEql/L • Chloride • 97-110 mEq/L • • Specific tests • Parameter • Normal Value • Lactic acid • • 0.5-2.0 mEq/L In sepsis, goes up > 4 • Procalcitonin • <0.5µg/L • Troponin • 0-0.4 ng/ml • CK-MB • 30-225 U/L • • • Coagulation profile • Parameter • Normal Value • • • PT (Prothrombin Time) How long it takes blood to clot Checks level of clotting factors • 11-15 secs • INR (International Normalized Ratio) • 0.9-1.1 • • PTT (Partial Thromboplastin Time) Factors 2,9,7,12 • 25-.37 secs • Fibrinogen (fibrin, clotting factor) • 200-400 mg/dl • FDP (Fibrinogen Degradation Products) determines coagulopathy • • <10 mg/L • Clinical condition: diagnostic criteria know distinction and how to manage • Clinical Condition • • SIRS Usually infection is present (any form) first, followed by sepsis • • • • • • Tachycardia >90 bpm Tachypnea >20 breaths/min or PCO2 <32 mmHg (due to tachypnea) Hyperthermia >38C or Hypothermia <36C’ 36-38* 96.8-100.4 Cbc, (high or low wbc, low platelets, high bun and creatinine, high lactic acid) Procalcitonin, lactic acid • Sepsis (any 2 or more of SIRS) • • • • • • • • Tachycardia >90 bpm Tachypnea >20 breaths/min or PCO2 <32 mmHg Hyperthermia >38C or Hypothermia <36C’ ^ 2 of 3 PLUS below Leukocytosis >12,000 cells/mm3 or Leukopenia <4,000 cells/mm3 or >10% immature cells (bands) labs to confirm sepsis cbc , lactic acid , procalcitonin, coag profile, chest xray Important to catch infection and intervene as early as possible • Severe Sepsis (+ organ dysfunction, hypoperfusion, hypotension) • • • • • • S/s of sepis PLUS elevated lactic acid (^), procalcitonin (^) impaired perfusion to organs, oliguria, changes on LOC • • Septic Shock Important characteristic is low bp • • Severe hypotension despite adequate fluid resuscitation, with impaired organ perfusion txt if bp drops initial fluid resus (ns bolus 30 cc/kg if bp keeps dropping give vasopressin, or pheno or • MODS (70-80% mortality rate) • ARDS, Hyperdynamic or Hypodynamic Cardiac function, DIC, Renal Failure, Liver failure, CNS Ischemia, Metabolic Acidosis Once a patient enters mods, there is no going back RECAP: diagnostics • Blood Works CBC CMP Lactic acid Procalcitonin Urinalysis Culture and Sensitivity (Blood, Urine, Wound, etc) Pan culture (multiple cultures) CXR Common cause of sepsis is pneumonia • • • Management • • • • • • • • Fluid Resuscitation: is the corner stone for fluid resus Cornerstone of therapy for septic, hypovolemic, and anaphylactic shock • Low fluids for cardiogenic and or neurogenic shock Ideal choice of fluid for resuscitation remains controversial. • NS 0.9% is most often used in the initial resuscitation (fluid volume replacement) • Half NS (0.45%) Large volume resuscitation with: • Saline – can lead to hyperchloremic metabolic acidosis (isotonic crystalloid) • 30cc per kg MAIN FLUID RESUS • Lactated (lactic acid) Ringer’s solution – may cause serum lactate levels to increase • CONTAINS NA, K, CHLORIDE, CALCIUM AND LACTATE Fluid responsiveness is determined by clinical assessment • Fluid challenge, normal saline is given first and lactic acid is given, goal is to see lactic acid is improving • Normal lactic is less than 2.0 Two major complications of large amounts of fluids • Hypothermia and coagulopathy BOLUS MIGHT NOT CORRECT ISSUES, FOLLOW BOLUS BY VASOPRESSOR Sympathomimetic Drugs (vasoactive meds) • Effects are mediated through their binding to a- or b-adrenergic receptors • Vasopressor drugs – drugs that cause peripheral vasoconstriction • Can increase SVR (BLOOD VESSEL IS DIALTED OF CONSTRICTED) , further risking tissue perfusion • 770-1500 • DILATED, CONSTRICTED • Goal is to achieve and maintain a MAP of greater than 65mmHg • MORE SENSATIVE INDICATOR OF PRESSURE • NORMAL IS 65-100 • Continuously monitor end-organ perfusion and serum lactate levels to ensure that tissue perfusion is adequate Drug therapy (medications are given via central line) • DRUG • MECHANISM OF ACTION • NURSING IMPLICATIONS • Norepinephrine • • • (Levophed) Hypotension and normal hr Low bp and norm hr • • • • • • Phenylephrine • (Neosynephrine) Hypotension and tachycardia ok Low bp and ^ hr Vasopressin VASOP ISADH Hypotension and tachycardia ok Drug of choice for septic shock • • • • β1-Adrenergic agonist (cardiac stimulation)affects hr α-Adrenergic agonist (peripheral vasoconstriction) ↑ BP, MAP, CVP, PAWP, SVR ↑/↓ CO (effect will vasoconstrict, TOO much constriction will decrease cardiac output Affects hr • α-Adrenergic agonist (peripheral vasoconstriction) ↑ HR, BP, SVR ↑/↓ CO Does not affect hr • • Antidiuretic hormone (vasoconstriction) • DOESNT AFFECT HR • Nonadrenergic vasoconstrictor • ↑ MAP • ↑ Urine output (?) • Administration via central line is recommended (infiltration leads to tissue sloughing). Can give if hypotensive and tachycardic • May be administered with together with norepinephrine if needed • Infusions are not titrated. Monitor hemodynamic pressures and urine output. IT’S THE DRUG OF CHOICE BECAUSE ITS VASOCONSTRICS, RETAINS WATER FROM KIDNEYS AND DOES NOT AFFECT HEART Can give if hypotensive and tachycardic Low bp and ^ hr • Hydrocortisone To lower anti-inflammatory -DECADONE - DEXAMETHASONE - Methylprednisolone Central line is required (infiltration leads to tissue sloughing). • Monitor for dysrhythmias • DO NOT give if tachycardic • Decreases inflammation, reverses increased capillary permeability • DECREASE INFLAMMITORY RESPONSE OF CYTOKINES • ↑ BP, HR • Monitor for hypokalemia, hyperglycemia. • ATC administration • Consider use as continuous infusion. Tidbips: stabilize pt (fix bp), draw blood culture THEN admin antibiotics Vanco is given because it’s a broad spectrum atb Central venous access devices (slide 21) (look into picc line nursing) Overview Catheters placed in large blood vessels (subclavian vein,internal jugular vein, femoral vein, etc) • Advantages • Reduce need for multiple venipuncture • Infusion of fluids and medications • Administration of vesicant (irritating)drugs, blood products, total parenteral nutrition, hemodynamic monitoring (cvp), etc. • Vesicant drugs: vanco, norepi, phenylephrine • Major Disadvantage • Central Line Associated Bacterial Systemic Infection (CLABSI) • Aseptic technique Central Venous Catheters • • • Rests in SVC if inserted through subclavian or jugular vein • Femoral vein sometime accessed Can single, double, triple or quad lumens MD order required for use by nursing Peripherally Inserted Central Catheter (PICC) • • Rests in SVC inserted into a vein (cephalic, median, brachial vein) in the arm • For patients who needs vascular access for 1 week to 6 months (sometimes longer) • Can single, double, triple lumens • MD order required for use by nursing • management Treatment of Infection • Broad spectrum antibiotics initially • Vanco • Targeted antibiotic administration based on offending organism • If hemodynamically stable, aggressive surgery is recommended to remove necrotic tissue that can provide a culture medium for microorganisms • Cannot send unstable patient to sx • Aggressive pulmonary management can reduce the risk of infection • Strict asepsis can decrease infections related to intraarterial lines, endotracheal tubes, indwelling urinary catheters, IV lines, and other invasive devices or procedures. MANAGEMENT • • Maintenance of Tissue Oxygenation • Hypoxemia frequently occurs in patients with SIRS and MODS • Interventions that decrease O2 demand and increase O2 delivery are essential • Sedation, mechanical ventilation, analgesia and rest may decrease O2 demand • Sedate the patient to redirect o2 demand to organs • Propofol Neurologic Status • Orientation and level of consciousness using valid tool, at least 1 to 2 hours • Neuro checks q1-2 hrs • • • • Best indicator of blood flow • Be aware of the clinical manifestations • (e.g. changes in behavior, hyper-alertness, blurred vision, confusion, paresthesia) • Orient the patient to person, place, time and events on a regular basis Respiratory Status • Ensure adequate oxygenation, detect complications early, and provide data regarding the patient’s acid-base status • Monitor rate, depth, and rhythm of respirations as frequently as every 15 to 30 minutes • Increased heart rate and depth provide information regarding the patient’s attempt to correct metabolic acidosis • Assess breath sounds every 1 to 2 hours a needed • Use pulse oximetry to continuously monitor O2 saturation • Arterial blood gases (ABGs) provide definitive information on ventilation and oxygenation status and acid-base balance • Maintaining patent airway and monitoring for ventilator-related complications are critical • VAP bundle (vent associated pneumo) Gastrointestinal Status • Auscultate bowel sounds at least every 4 hours • Absence can be paralytic illeus • Monitor for abdominal distention • If nasogastric tube is present, measure drainage and check for occult blood • Assess readiness for gastric feeding • Check stools for occult blood Nutritional Therapy • Protein-calorie malnutrition is one of the main manifestations of hypermetabolism in shock • Nutrition is vital to reducing mortality • Enteral nutrition should be started within 24 hours (ideally) • High doses use of vasopressor/s, hold-off feeding • • • • Wake the pt up (lower sedation) RASS (usually -2) • • • High vasopressor >10 mc. Can cause vasoconstriction in intestine as well, impairing absorption • Trophic feeding – (trickle feed) defined as slow drip of small amounts of enteral nutrition (e.g. 10mL/hr) • If pt have been npo >3days stomach is sluggish, you want to start slow feeding • Parenteral nutrition is used only if enteral feedings are contraindicated Ambulatory Care • Rehabilitation of the patient who has experienced critical illness requires: • Correction of the precipitating cause • Prevention or early treatment of complications • Teaching focused on disease management or prevention of recurrence based on the initial cause of shock • Continue to monitor the patient for indications of complications throughout the recovery period • Patients recovering from shock often require diverse services after discharge. These can include: • Admission to transitional care units • Rehabilitation centers • Home health care agencies • Start planning for safe transition from hospital to home Support of Failing Organs • Support of any failing organ is a primary goal of therapy • ARDS – requires aggressive O2 therapy and mechanical ventilation • DIC – should be treated appropriately (e.g. blood products) • Disseminated I coagulation, systemic clotting • Coag profile can test for DIC • Within coag profile: pt/ptt/Inr/fdp • Renal failure – may require dialysis. Continuous renal therapy is better tolerated than hemodialysis, especially in a patient with hemodynamic instability • Most damaged organ in sepsis • It is important to maintain communication between the health care team and the patient’s caregiver regarding realistic goals • Withdrawal of life support and starting end-of-life care may be the best options for the patient Cardiogenic shock • • • Occurs when either systolic or diastolic dysfunction of the heart’s pumping action results in reduced cardiac output • Ejection fraction will be low Mortality rate approach 60% Decreased filling of the heart results in decreased stroke volume weak heart low blood flow poor perfusion cell death Clinical presentation: • Similar with acute decompensated heart failure • Tachycardia, Hypotension • Pulse pressure narrow • Tachypnea, crackles on auscultation of breath sounds • Increase in pulmonary artery wedge pressure (PAWP), stroke volume variation (SVV), and pulmonary vascular resistance • Signs of peripheral hypoperfusion (e.g. cyanosis, pallor, diaphoresis, weak peripheral pulses, cool and clammy skin, delayed capillary refill) are seen • Decreased renal flow • Anxiety, confusion, and agitation may develop • Clue: Recent cardiac intervention or pre-existing cardiac condition • • • • Cardiogenic shock Drug management • DRUG • MECHANISM OF ACTION • NURSING IMPLICATIONS • Dobutamine • • ↑ Myocardial contractility ↓ Ventricular filling pressures ↓ SVR, PAWP ↑ CO, stroke volume, CVP ↑/↓ HR • Administration via central line is recommended (infiltration leads to tissue sloughing). Do not administer in same line with NaHCO3. tachydysrhythmias develop. • • • • • • • • Dopamine Epinephrine (Adrenaline) Drug of choice for anaphylactic shock • • • • • • ↑ Myocardial contractility ↑ Automaticity ↑ HR, CO ↑ BP, ↑ MAP ↑ MVO2 Can cause progressive vasoconstriction at high doses • Low doses: β-Adrenergic agonist (cardiac stimulation, bronchodilation, peripheral vasodilation) • ↑ HR, contractility, CO ↓ SVR • High doses: α-Adrenergic agonist (peripheral vasoconstriction) • ↑ Stroke volume, SVR • ↑ Systolic/↓ diastolic BP, widened pulse pressure • ↑ CVP, PAWP • • • Administration via central line is recommended (infiltration leads to tissue sloughing). Do not give in same line with NaHCO3. Monitor for tachydysrhythmias. • Monitor for HR >110 beats/min. • Monitor for dyspnea, pulmonary edema. Monitor for chest pain, dysrhythmias Monitor for renal failure secondary to ischemia. • Intra-aortic Balloon Pump • • • • • • • • IABP provides temporary circulatory assistance to sick heart by reducing afterload (reduces pressure against L ventricle (via reduction in systolic pressure) and augmenting the aortic diastolic pressure. • Improve coronary blood flow. Consists of a sausage-shaped balloon, a pump that inflates and deflates the balloon, a control panel for synchronizing the balloon inflation to the cardiac cycle, and fail-safe features Balloon is inserted percutaneously(under skin) into the femoral artery → descending thoracic aorta just below the left subclavian artery and above the renal arteries X-ray confirms the position. Pneumatic device fills the balloon with helium at the start of diastole (immediately after aortic valve closure) and deflates it just before the next systole. • During diastole balloon inflates ECG is the trigger used to start deflation on the upstroke of the R wave (of the QRS) and inflation on the T wave Known as counterpulsation because the timing of balloon inflation is opposite to ventricular contraction. • Deflates during systole Timing • 1:1 • 1:2 • 1:3 Indications for IABP • Refractory unstable angina (when drugs have failed) • Short-term bridge to heart transplantation • Acute myocardial infarction with any of the following:† • Ventricular aneurysm accompanied by ventricular dysrhythmias • Acute ventricular septal defect • Acute mitral valve dysfunction • • • Cardiogenic shock Refractory chest pain with or without ventricular dysrhythmias Preoperative, intraoperative, and postoperative cardiac surgery (e.g., prophylaxis before surgery, failure to wean from cardiopulmonary bypass, left ventricular failure after cardiopulmonary bypass) • High-risk interventional cardiology procedures Irreversible brain damage Major coagulopathy (e.g., disseminated intravascular coagulation (DIC) Terminal or untreatable diseases of any major organ system • Liver, kidney failure ect ect Abdominal aortic and thoracic aneurysms Moderate to severe aortic insufficiency • Leaky aortic valve Generalized peripheral vascular disease (e.g., aortoiliac disease) Complications of IABP (slides 43/44) • • • • • • • • Potential Complications • Nursing Interventions • Thromboembolism caused by trauma, balloon obstruction of blood flow distal to catheter • Give prophylactic heparin therapy (if ordered). Evaluate pulses, urine output, and level of consciousness at least every hour. Check circulation, sensation, and movement in both legs at least every hour. • • • Hematologic complications caused by platelet aggregation along the balloon (thrombocytopenia) • • Monitor coagulation profiles, hematocrit, and platelet count. • Hemorrhage from insertion site • Check site for bleeding at least every hour. Monitor vital signs for signs of hypovolemia with each check. • • • • • • • • Balloon leak or rupture • Cardiogenic shock VAD management (slide 44) Intra-Aortic Balloon Pump Cardiogenic shock VAD management Impella • Prepare for emergent removal and possible reinsertion. Anaphylactic shock • An acute, life-threatening hypersensitivity (allergic) reaction to a sensitizing substance • The reaction quickly causes massive vasodilation, release of vasoactive mediators, and an increase in capillary permeability • Can lead to respiratory distress due to laryngeal edema or severe bronchospasm, and circulatory failure from the massive vasodilation • Sudden onset of symptoms including: • Dizziness • Chest pain • Incontinence • Swelling of the lips and tongue • Wheezing • Stridor • Skin changes including flushing, pruritus, urticaria, and angioedema • Patient may be anxious and confused • management • IM epinephrine is the first drug of choice – it causes peripheral vasoconstriction and bronchodilation and opposes the effect of histamine • Diphenhydramine and ranitidine (Zantac) are given as adjunctive therapies to block the ongoing release of histamine from the allergic reaction • Maintaining a patent airway is important because the patient can quickly develop airway compromise from laryngeal edema or bronchoconstriction • Nebulized bronchodilators are highly effective • Aerosolized epinephrine can also be used to treat laryngeal edema • Endotracheal intubation or cricothyroidotomy may be necessary to secure and maintain a patent airway • Hypotension • Aggressive fluid resuscitation, usually with crystalloids is necessary • IV corticosteroids may be helpful if significant hypotension persists after 1 to 2 hours of aggressive therapy Neurogenic shock • A hemodynamic phenomenon that can occur within 30 minutes of a spinal cord injury and can last up to 6 weeks • Generally associated with a cervical or high thoracic injury • Spinal anesthesia can block transmission of impulses from the SNS • Depression of the vasomotor center of the medulla from drugs also can decrease the vasoconstrictor tone of the peripheral blood vessels • Clinical manifestations: • Hypotension (brainstem is damaged) • Bradycardia (different from other shocks) • Patient may not be able to regulate body temperature • Skin is warm due to massive vasodilation • management • Treatment of neurogenic shock is based on the cause • Place them on inotropes , no fluid bolus • Promote spinal stability (e.g. spinal precautions, cervical stabilization with a collar) are initially used • Treatment of the hypotension and bradycardia is essential to prevent further spinal cord damage • Vasopressors (e.g. phenylephrine) to maintain BP and organ perfusion • Bradycardia may be treated with atropine • Infuse fluids cautiously as the cause of the hypotension is not related to fluid loss • The patient with a spinal cord injury also needs to be monitored for hypothermia caused by hypothalamic dysfunction Obstructive shock • • • • Develops when a physical obstruction to blood flow occurs with a decreased CO Can be caused by restricted diastolic filling of the right ventricle from compression Abdominal compartment syndrome – increased abdominal pressures compress the inferior vena cava, thus decreasing venous return to the heart • Patients experience a decreased CO, increase afterload, and variable left ventricular filling pressures • Other clinical signs: jugular venous distention and pulsus paradoxus • Rapid assessment and treatment are important to prevent further hemodynamic compromise and possibly cardiac arrest management • Early recognition and treatment to relieve or manage the obstruction • Pericardial tamponade, tension pneumothorax and hemopneumothorax • Mechanical decompression may be done by needle or tube insertion • Pulmonary embolism • May require thrombolytic therapy • Superior vena cava syndrome – a compression or obstruction of the outflow tract of the mediastinum • May be treated by radiation, debulking, or removal of the mass or cause • Decompressive laparotomy may be indicated or abdominal compartment syndrome Hypovolemic shock • • Occurs after loss of intravascular fluid volume Absolute hypovolemia – results when fluid is lost through: • Hemorrhage • Gastrointestinal (GI) loss (e.g. vomiting, diarrhea) • Fistula drainage • Diabetes insipidus • • • Diuresis Relative hypovolemia – fluid volume moves out of the vascular space into the extravascular space. • Called third spacing Management focuses on stopping the loss of fluid and restoring the circulating volume • Fluid resuscitation is calculated using a 3:1 rule (3mL of isotonic crystalloid for every 1mL of estimated blood loss) • • • • • • • • YouTube. Retrieved from https://www.youtube.com/watch?v=yl6R_3Jrs_s YouTube. Retrieved from https://www.youtube.com/watch?v=WueGqL58tlo YouTube. Retrieved from https://www.youtube.com/watch?v=GhWB7T5QxMI YouTube. Retrieved from https://www.youtube.com/watch?v=ZBMhi5HrS2s YouTube. Retrieved from https://www.youtube.com/watch?v=EFnUaYRAdro YouTube. Retrieved from https://www.youtube.com/watch?v=vJ_anWmQbUM