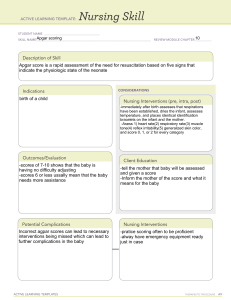
Maternal Final Exam Blueprint Chapter 12: Process of Birth 4 Stage of True Labor: -“bloody show” mucus & blood -Water breaking: Amniotic Sac Rupture -True labor contraction Increased frequency (regular & rhythmic) Increased intensity & duration -Cervix (dilation) how wide is the cervix? Goal = 10cm! means baby is ready to come out! -Effacement = cervix gets thinner & shorter (Elastic cervix) (0-100%) -Braxton Hicks Contractions = FALSE LABOR CONTRACTIONS disappear with walking or position changes, No dilation of cervix decrease in intensity with ambulation True Labor – Pain does not decrease with reset Contractions: -regular (increasing frequency, duration, & intensity) -stronger, last longer, frequent -felt in lower back, radiates to abdomen -walking = increasing intensity -continue despite comfort measure False Labor – Pain alleviated with rest or changing position Contractions: -painless, irregular, intermediate -decrease in frequency, duration, & intensity with walking/position changes -felt lower back/abdomen -often stop with sleep/comfort Cervix: -progressive change in dilation & effacement -moves to anterior position -bloody show Cervix: -no significant change in dilation or effacement -often remains posterior position -no significant bloody show Fetus: -presenting part is not engaged in pelvis Fetus: -presenting part engages in pelvis Back pain “back labor” Occiput posterior position Interventions: 1. Apply counterpressure to sacrum during contractions 2. Reposition mom on hands & knees with birth ball & encourage to change position every 30-60 mins. Characteristics of a contraction: -Assess uterine contraction by palpation (place hand over fundus) -Frequency = beginning of one contraction to beginning of next (in minutes) -Duration = time between beginning of contraction to end of same (in seconds) -Intensity = strength of contraction at it’s peak mild: slightly tense like pressing your nose moderate: firm like pressing finger to chin strong: rigid, like pressing finger to forehead Stages of Labor 1st stage of labor: (longest stage, lasts up to 20 hours) (beginning of regular contractions or ROM to 10cm/100%) Latent phase – cervix becomes soft & thin as it gets ready to open up (dilate) for your baby to be born. For this to happen, you’ll start having contractions: 0-3cm dilated (frequency 3-5 mins, duration 30-45 secs) Active phase – 4-7cm dilated, frequency 3-5 mins, duration 40-70 secs, STRONG Transition phase – 8-10cm dilated, frequency 2-3mins, duration 45-90 secs Interventions: -emotional support -breathing techniques -10cm dilated- document FHR every 15 mins -AVOID pushing until 10cm, fully dilated (risk for cervical swelling & lacerations) 2nd stage of labor: 10cm to delivery, full dilation contractions 1-2mins (delivery of baby) Interventions: -cervix must be 100% effaced & 10cm dilated -signs: increase in contractions & urge to push during labor Ferguson reflex: spontaneous urge to push during labor occurs when presenting part of fetus reaches pelvic floor -positioning of mother = PRIORITY, high fowlers, lithotomy, side lying -push properly, avoid holding breath or tightening abdomen -push when feeling the urge, breathe in deep -breathe out slowly through mouth, keep mouth open while pushing down -assessments: FHR, frequency & duration of contractions, uterine tone 3rd stage of labor: delivery of neonate to delivery of placenta High risk for: -infection: If placenta parts are not fully removed -uterine inversion: pulling on cord -severe hemorrhaging: bleeding, decreasing BP, Tachycardia -Pitocin (oxytocin) to prevent hemorrhage 4th stage of labor: recovery, bonding -skin to skin & breastfeeding -infection: temp over 100.7 -hemorrhage: peri pads (fully saturated in less than 1hr) hypotension, tachcardia Interventions: -Fundus check FIRST! Soft & boggy= massage until firm -Void or use catheter -Pitocin (oxytocin): IV or IM, control bleeding after childbirth -Breastfeeding: stimulates release of natural oxytocin Normal fundus= firm, midline, level with umbilicus Not normal= displaced fundus above umbilicus or to one side, bladder distention -Intervention Void every 2-3 hours (bedpan preferred) Lochia Assessment = discharge after birth -Lochia Rubra= bright redflow (3-4 days) small clots NORMAL -Lochia Serosa= pink/brown (4-10 days) NORMAL -Lochia Alba= white/yellow (10-28 days) NORMAL NOT NORMAL = large clots, malodorous “foul odor”, excessive bleeding Check under patient for pooled lochia Interventions for infants who are SGA: -support respiratory efforts (suction, maintain airway) -prevent cold stress by providing neural thermal environment, isolette or radiant heat warmer may be needed) -initiate early feedings because SGA babies require more frequent feedings (administers parenteral nutrition if necessary) -maintain hydration, conserve energy level, prevent skin breakdown, protect from infection Interventions for infants who are LGA: Prior to delivery: -prepare for vacuum assist or c-section -prepare to place client in McRoberts’ position (lithotomy with legs flexed to chest) -prepare to supply suprapubic pressure to aid in delivery of anterior shoulder -assess newborn for trauma After delivery: -early and frequent heel sticks for blood glucose -initiate early feedings or IV therapy to maintain normal glucose levels -administer surfactants by endotracheal tube if needed 5 P’s of Labor Passageway- “Pelvis” Birth Canal -Presentation: what part of baby is presenting: head, chin, shoulder, breech -Lie: what is baby in relation to mother: transverse, parallel/longitudinal -Attitude: baby’s head: flexion, extension = bad! -High risk c-section: transverse, sideways, oblique, angle Passenger- Placenta and Fetus -fetal station = degree of fetal descent into pelvis Position (fetal positions) GOOD POSITION ROA – right occiput anterior LOA – left occiput anterior BAD POSITION – makes labor worse & long, back labor OP – occiput posterior OT – occiput transverse -Breech presentations: complete, frank, footling Interventionsexternal cephalic version, c-section Power- strength of contractions, contractions to OPEN cervix -frequency (how often – mins) 2-3mins apart -duration (how long – secs) 60 secs between contractions -Intensity (how strong) increase closer to delivery Psychological- emotional status of mother during birth, cultural considerations Fetal Station Station -1 to -5 = baby’s head ABOVE mom’s ischial spine (deeper inside pelvis) Station 0 = Baby’s head is level with mom’s ischial spine, engaged & ready for labor Station 1 - 5 = Baby’s head is coming out! “crowning” start pushing Chapter 13: Pain management during birth Pain control -monitor for nonverbal signs of ineffective coping with labor (panic, anxiety, squirming movements) -breathing techniques, imagery, massage: sacral counterpressure, effleurage Sedatives: Barbitrates – phenobarbital *caution: respiratory depression, (do not give if birth anticipated 12-24 hours) Opiods: Butorphanol, Nalbuphine, Meperidine -Only give opiods during contractions, after cervix 4cm dilated or it will slow labor *Have naloxone ready (antidote) -If given to mother too close to time of delivery, can cause respiratory depression in neonate Epidural Anesthesia -blocks sensation from waist down, umbilicus to legs -given after 4cm dilated *caution: maternal hypotension, fetal bradycardia, low platelet count (norm=150k-400k) Spinal Anesthesia -used for C section -100% loss of motor movement & sensation Interventions: epidural & spinal block -IV fluids to help counteract side effects of maternal hypotension -Turn mother to left lateral position & increase IV fluid rate Pudendal Nerve Block -perineum, vulva, rectum (lower part of the perimeum) -can be given quickly when birth is imminent -does not relieve contraction pain -mother still feels pressure Perineum Care -apply ice packs to the perineum to reduce pain/edema and prevent hematoma formation -after voiding, use squeeze bottle with warm water to clean are & pat dry -use sitz bath several times daily for 15-20 mins -witch hazel pads can reduce pain and swelling associated with hemorrhoids -increase fluid & fiber intake to prevent constipation Endometritis -most common postpartum infection, inflammation & infection of the uterus -S&S: fever, suprapubic pain and tenderness, excessive/malodorous lochia, tachy, hypotension -give IV/oral antibiotics & monitor for complications (sepsis, necrotizing fasciitis) Postpartum hemorrhage -S&S: saturating pad <15min, soft/boggy uterus, large blood clots, constant blood flow from vagina, signs of hypovolemic shock (tachy, hypotension, cool/clammy skin) -Interventions: firmly massage fundus, administer O2, IV fluids, blood products as ordered, elevate patient’s legs Non pharmacological pain management -does not slow, no side effects, may be the only realistic option in advanced rapid labor Techniques: -relaxation -sensory: aromatherapy, breathing techniques, imagery, music, focal points, subdued lighting -cutaneous simulation: touch & massage, walking, rocking, sacral counter pressure, position changes, application of hot or cold -mental stimulation Chapter 14: Intrapartum Fetal Surveillance Fetal Heart Monitoring Normal = 110 – 160bpm -External = point of maximal pulse baby’s HR can be heard the loudest -Cephalic = lower abdomen replacement -Breech = higher abdomen placement -Contraction monitor sensor = high up on abdomen -Internal fetal monitor = high risk pregnancy, not affected by movement (better readings) Absent variability not jiggly = NOT good Minimal variability flatter line, that looks “sleepy & sad” *Moderate variability normal & desired finding Marked variability jagged jiggles = STRESSED baby Accelerations = temporary increase in FHR, indicates great oxygenation for baby “happy little mountains” Decelerations = dips from baseline Early decelerations = excellent! Shallow, bowl shaped dips that mirror moms contractions, indicates head compression Variable decelerations = very bad! “sharp v-dips” indicates cord compression Interventions: reposition client from side to side or into knee-chest position, discontinue oxytocin if being infused, administer oxygen by mask 8-10L/min, perform or assist with vaginal exam, assist with amnioinfusion if prescribed. Late decelerations = BAD! Indicates decreased oxygen (hypoxia) placental insufficiency Interventions: place client in side lying position; insert an IV catheter if not placed & increase rate of IV fluid administration, discontinue oxytocin if being infused, administer terbutaline & oxygen by mask 8-10L/min, elevate legs, notify provider, prepare for an assisted vaginal birth or c-section. -Sinusoidal FHR = repetitive, wave-like fluctuations (hills) with no variability & no response to contractions -Tachysystole complication = over 5 contractions in 10 minutes What is amnioinfusion? Installation of sterile saline into amniotic cavity to refill lost fluid -report immediately if indications of overfilling -uterine resting tone that increases to 45mm Hg How do you auscultate leopold’s maneuver? -consist of performing external palpitations of the maternal uterus through the abdominal wall to determine the number of fetuses, presenting part, degree of descent, and location of the fetus’ part -performed on patient who is in labor & determines fetus is in RSA position = BREECH Chapter 15: Nursing Care During Labor & Birth -Therapeutic communication with mother while in birth -Review nursing responsibility during admissions -Assessment to maternal and fetus Dilation = the opening of the cervix, the entrance to the uterus, measured from 1-10cm. Effacement = Thinning of the cervix, measured from 0-100%. Station = measurement of fetal descent in centimeters with station 0 being at the level of an imaginary line at the level of ischial spines, minus stations superior to the ischial spines, and plus stations inferior to the ischial spines (-3 to 3+) Chapter 16: Intrapartum complications What is chorioamnionitis? Bacterial infection that occurs before or during labor. The name refers to the membranes surrounding the fetus: the “chorion” (outer membrane) and “amnion” (fluid filled sac). The condition occurs when bacteria infect the chorion, amnion, and amniotic fluid around the fetus. Abnormalities that may result in dysfunctional labor or risk for preterm labor Infections of the urinary tract or vagina, HIV, active herpes infection, or chorioamnionitis Previous preterm birth Multifetal pregnancy Oligohydramnios (too little amniotic fluid) causes poor fetal lung development Polyhydramnios (too much amniotic fluid) fetal is not swallowing Advanced maternal age Smoking, substance use, violence/abuse, history of multiple miscarriages/abortions Diabetes mellitus, chronic hypertension, preeclampsia, lack of prenatal care Placenta previa/abruptio, premature rupture of membranes Uterine abnormalities, second trimester bleeding, low pregnancy weight, congenital anomaly Prolapsed umbilical cord- Umbilical cord is displaced, proceeding the presenting part of the fetus, or protruding through the cervix. S&S: -patient reports she feels something coming through vagina -visualization or palpation of the umbilical cord protruding from introitus -FHR monitoring shows variable or prolonged deceleration -excessive fetal activity followed by c-section of movement, suggestive of severe fetal hypoxia Interventions: -call for assistance immediately -notify HCP -use a sterile gloved hand, insert two fingers into the vagina and apply finger pressure on either side of the cord to the fetal presenting part to elevate it off the cord. Meconium-stained amniotic fluidS&S: -amniotic fluid varies in color; black to greenish, yellow or brown, through meconium-stained amniotic fluid is often green criteria for evaluation of meconium-stained amniotic fluid : -often in breech position, and might not indicate fetal hypoxia -no changes in FHR -stained fluid accompanied by variable or late decelerations in FHR Interventions: -document color and consistency of stained amniotic fluid -gather equipment for neonatal resuscitation -assess neonatal respiratory efforts, muscle tone & HR -suction mouth and nose using bulb syringe (HR should be >100 bpm) -suction below the vocal cords using an endotracheal tube before spontaneous breaths occur if reparation are depressed and HR <100bpm. Fetal distress- FHR is <110/min or >160/min, FHR shows decreased or no variability and there is fetal hyperactivity or no fetal activity. S&S: -nonreassuring FHR pattern with decreased or no variability Interventions: -monitor vitals & FHR -position the patient in a left side-lying reclining position with legs elevated -administer 8-10L/min of oxygen through face mask -discontinue oxytocin if being administered -increase IV fluid rate to treat hypotension if indicated -prepare for an emergency c-section Chapter 17: Postpartum adaptations & nursing care Postpartum baby blues: -10 days or less & resolve on it’s own -crying & sadness but don’t know why -fatigue & exhaustion Postpartum depression: -2 weeks or more -onset within 4 weeks after delivery -anxiety, panic, overwhelmed, stressed -persistent sadness & mood swings -loss of interest, decreased appetite, insomnia Interventions = longer maternity leave, depression therapy, meds, follow up Postpartum psychosis: MOST SEVERE -within 2-3 weeks of delivery -confusion, hallucinations, paranoid -high risk harm to self & baby ASK SIMPLE QUESTIONS! -Have you felt depressed/hopeless over last 2 weeks? -Do you still enjoy same things? Fetal Demise: still born infant who has dies before or during delivery -allow parents to stay with baby as long as they want -ask parents if they would like to help bathe infant -encourage parents & family to hold infant -offer to obtain handprints, footprints, & photo of infant Postpartum assessment normal findings: -after birth, fundus should be firm, midline, at the level of the umbilicus -at 12 hours, fundus is 1cm ABOVE umbilicus -fundus descends 1-2cm every 24 hours -at day 6, fundus is ½ way between umbilicus & symphysis pubis BUBBLE HERV B- Breast U- Uterus (fundal height, uterine placement & consistency) B- Bowel & GI function B- Bladder Function L- Lochia (color, odor, consistency, and amount) E- Episiotomy H- Hemorrhoids E- Emotions R- Rubella (prevent pregnancy at least 1 month after receiving) V- Vaccines Postpartum discharge teaching: -Perineal Care: clean front to back with warm water after each BM/void -remove and apply perineal pads from front to back -Activity: c-section- postpone abdominal exercises/heavy lifting -Kegel exercises -no driving for the first 2 weeks -sexual activity can resume by the 2nd-4th week after birth, when bleeding has stopped, or perineum has healed -avoid sex until vaginal discharge is white: lochia alba & episiotomy is healed -use OTC lubricants during sex -ovulation may occur 4 weeks after delivery, before menses returns -use contraception (condoms) immediately Chapter 18: Postpartum Maternal Complications Vaginal birth- loss of more than 500mL of blood Cesarean birth- loss of 1,000mL or more of blood Risk factors- uterine atony, complications during pregnancy, administration of magnesium sulfate therapy during labor, lacerations & hematomas, inversion of uterus, retained placental fragments Expected findings- increase of change in lochial pattern, uterine atony, blood clots larger than a quarter, perineal pad saturation in 15 mins or less, constant oozing, trickling, or frank flow of bright red blood from the vagina, tachycardia & hypotension, skin pale, cool, clammy with loss of turgor and pale mucous membranes, oliguria Lab tests- Hgb, Hct, coagulation profile (PT), bloodtype & crossmatch Complications- hypovolemic shock, anemia Nursing Care- monitor vital signs, assess for source of bleeding, assess fundus for height, firmness, and position. If uterus is boggy, massage fundus to increase muscle contraction, assess bladder for distention: insert an indwelling urinary catheter to assess the client’s kidney function and obtain an accurate measurement of urinary output Medications-Oxytocin (Pitocin) promotes uterine contractions -Methylergonovine (Methergine) assess uterine tone & vaginal bleeding, prevention & treatment of postpartum hemorrhage -DO NOT administer to clients who have hypertension -Misoprostol (Cytotec) Chapter 19: Normal Newborn Process of Adaptation: APGAR SCORE -done at 1 minute after birth & 5 mins after delivery -may be reassessed at 10 minutes if score less than 7 **7 or LESS = REASSESS** A- Appearance (skin color) P- Pulse (heart rate) G- Grimace (reaction & reflex) A- Activity (muscle tone) R- Respiratory effort 0 points 1 point Blue/pale color Blue arms/legs (acrocyanosis) & pink body Absent Less than 100/min Absent Grimace 2 points Completely pink Over 100/min Cry & pull away Limp Absent Minor flexion Weak cry Active flexion & extension Strong cry Interventions based on score 0-3 = severe distress Resuscitate fully 4-6 = moderate distress Some resuscitation (oxygen, suction, stimulate, rub back/feet) 7-10 = Adequate Provide post delivery care Chapter 20: Assessment of Newborn: Phase 1: Stabilization Phase 2: Infant physical exam Phase 3: Routine care **Immediately after delivery dry & cover infant with a warm sterile blanket Vital Signs: -Assessed every 30 mins after birth for 2 hours, then every 4-8 hours -HR: (resting not crying) 110-160bpm, assess for apical pulse for full 1 minute, pull bell of stethoscope at 4th intercostal space- left midclavicular line -Blood Glucose: 40-60, encourage breastfeeding -Respirations: 30-60 -Temperature: (axillary) 97.7-99.5F or 36.5-37.2C NO RECTAL TEMP!! -Blood Pressure: 73/55 -Length: 18-22inch -Weight: 5.5-9.5lb NORMAL = newborn weight loss first 3-4 days 5-6%. Report if weight loss over 7% New Ballard Scale -Posture: fully extended = premature, fully flexed = mature -Square window: measures wrist flexibility >90 degree angle = premature 0 degree angle = mature -Popliteal angle: extended baby’s knee. Big angle (180) = premature small angle (90) = mature -Scarf sign: cross body’s arm over chest. Little to no resistance = premature resistance = mature -Heel to ear: reach baby’s heel to ear. Little to no resistance = premature resistance = mature -Arm recoil: no recoil = premature full recoil = mature -Skin texture: sticky transparent = premature leathery & wrinkled = mature -Lanugo: none = very premature present = premature mostly bald = mature -Plantar surface creases: absent = premature creases over entire sole = mature -Breast tissue: imperceptible = premature full areola with 5-10mm bud = mature -Eye opening, ear cartilage: lids focused and no recoil of pinna = premature eyes open and pinna recoils when folded = mature -Genitalia flat smooth scrotum or prominent clitoris with flat labia = premature pendulous testes with rugae or labia major covering labia minora & clitoris = mature Infant Reflexes -Tonic neck: head turned to one side, arm and leg on that side extended -Babinski: stroke outer edge of foot, toes fan up and out -Stepping: elicit by touching infant’s on flat surface -Sucking/rooting: elicit by stroking cheek, infant will turn to that side -Palmar grasp: elicit by stroking object in baby’s palm, infant will grasp -Plantar grasp: elicit by touching sole of foot, infant curls toes -Moro reflex: infant’s response to lack of support (falling) arms & legs extend & fingers form a C Newborn Medications -Erythromycin Optic Ointment: prevents infections/blindness, give in lower conjunctival sac, within 1-2 hours of birth -Vitamin K: prevent hemorrhage, give in thighs (vastus lateralis) -Hepatitis B: get informed consent, do not give in same thigh as vit K, give within 24hrs Circumcised & Uncircumcised -petroleum jelly application at diaper changes -normal healing = yellow exudate after first day -no bathing until circumcision has healed -clean with warm water without soap, avoid alcohol based wipes Signs to report: -bleeding exceeding the size of a quarter -dry diaper or no voiding 6-8hrs after circumcision Chapter 21: Care of Normal Newborn: Crying -newborns cry when they are hungry, overstimulated, wet, cold, hot, tired, bored, or need to be burped -don’t feed every time they cry, this leads to overeating causing stomachs and diarrhea Sleep -sleep 16-19hr/day -supine sleeping position decreases risk for infant death syndrome Oral/nasal suctioning -compress bulb before inserting into side of mouth -aspirate side of the mouth first and then one nostril followed by the second nostril -avoid center of the mouth because that can stimulate gag reflex Bathing -performed 2-3x/week using mild soap (water only for eyes) -bathing by immersion is not done until the cord has fallen off an circumcision has healed -sponge baths: wash area around cord, move from cleanest to dirtiest (starting with eyes, face, head, proceed to chest, arms legs, lastly the groin area). -test water with elbow before proceeding -expose only the part of the body part that is being bathed to prevent heat loss -wash uncircumcised penis with soap and water -wash circumcised penis with ONLY warm water until it has healed Feeding -at least 6 wet diapers a day (report less than 6 diapers a day or poor feeding) -at least 3 BM/day, less for formula fed infants -first 3 months, newborn requires 110kcal/day -requires 9g/day of protein from birth to 6mos of age - breastfeed every 2-3hrs awake newborn every 3hrs to feed during the day Cord Care -keep cord DRY -keep top of diaper folded underneath cord -sponge baths only until cord falls off (10-14 days after birth) -report a cord that is moist, red, has foul odor, and purulent drainage Clothing -too many layers of clothing or blankets can make newborn too hot -wash clothes separately with hot water & mild detergent -dress newborns as parents would dress themselves What to report -temp over 100.4 or less than 97.9 -poor feeding, frequent vomiting, decreased urination, jaundice, cyanosis, lethargy -labored breathing with flared nostrils or absence of breathing with greater than 15 secs Thermoregulation – balance between heat loss & heat production Types of heat loss: -Conduction: heat loss from direct contact with cooler surface (stethoscope, scale) -Convection: heat loss from cooler environmental air (fan, air conditioning vent) -Evaporation: heat loss when surface liquid is converted to vapor (bathing) -Radiation: heat loss from close proximity to cooler surface (windows) Interventions: dry newborn immediately after birth & bathing, swaddle & place hat on infant, encourage skin to skin contact with mother, use protective cover over scale, keep cribs away from ac, windows, or drafty areas. Infant safety Home safety: place newborn on back while sleeping -mattress should be firm, never put pillows/bumper pads/toys/loose blankets in crib -bassinet/crib should be placed on an inner wall, not next to a window (prevents stress by radiation) -nothing should be placed around infants neck -all visitors mush wash hands before handling infant -no smoking around the baby Car safety: placed in the back seat – rear facing until age 2. Chapter 22: Infant Feeding Breastfeeding benefits: -what is it? prolactin & oxytocin inside of the breast making the mik -reduces risk of infection -promotes rapid brain growth due to large amounts of lactose -provides protein & nitrogen for neurological cell building & improves the newborn’s ability to regulate calcium & phosphorus levels -contains electrolytes & minerals -easy for newborn to digest -promotes maternal-infant bonding -reduces incidence of sudden infant death syndrome, allergies, & childhood obesity During breastfeeding = need a good latch!! -baby’s mouth open covering areola & nipple -ensure bottom of areola is in baby’s mouth, nipple up against roof of mouth -baby’s tongue against bottom of areola, reposition baby’s latch always use 1 finger to break suction first Bad latch -shallow latch, only tip of nipple in baby’s mouth, causes less milk flow, nipple soreness, cracking, bleeding For sore nipples: -allow nipples to air dry by applying breast milk to sore nipples -lanolin cream, nip defense After breastfeeding: -FULLY empty breasts with each feeding, use breast pump if needed (helps mom increase milk supply & helps prevent breast engorgement -Initially feed every 1-3hrs, 8-12x/day *AVOID alcohol during breastfeeding (wait 2 hours or more) -analgesics immediately after breastfeeding Education for mothers: -encourage fluid intake for adequate milk production -wear supportive bra -report to HCP for signs of mastitis: flu like symptoms, fever, muscle aches, unilateral breast swelling, pain, inflammation, redness, warmth, edema blocked milk duct Before breastfeeding apply warm compress to breasts to open milk ducts & prevent blockage After breastfeeding apply cold compress Interventions for breast engorgement -feed or pump more regularly -recognize feeding cues from baby: rooting reflex, suckling motion, hand to mouth movements -use chilled fresh cabbage leaves on breasts throughout the day -warm compress or warm shower before -apply breast milk to sore nipples and allow to air dry after feeding Formula -wash the top of formula can before opening -refrigerate unused formula & discard after 48hrs -throw away leftover formula after feeding -boil or wash in a dishwasher, bottles/nips/cups -before feeding, warm formula & test temperature on inner wrist, should be lukewarm -NEVER over dilute or over concentrate the formula, never microwave Chapter 23: High Risk Newborn Complications- Gestational Age & Development: & Chapter 24: Acquired & Congenital Conditions Hyperbilirubinemia -Increased bilirubin in the blood resulting in jaundice, due to infant’s immature liver function -Usually begins on day 2-4 & resolves in 2 weeks, it NEVER occurs in first 24hrs -yellowish hues, face or eyes (sclera), trunk/extremities -drowsiness, high pitched cry, poor feeding -presence of cephalhematoma Treatment = Phototherapy (Baby is placed under UV lights or special light-producing blanket) -Interventions: -place baby under light wearing just a diaper -protect baby’s eyes with mask -turn baby frequently every 2 hours -monitor baby’s temperature -monitor for dehydration, weight, urine output (weigh diaper) -dehydration risk = give fluids every 2 hours -do not apply lotion on baby -check bilirubin levels every 6-12 hours -possible side effect is a rash “bronze baby syndrome” Hypoglycemia -serum glucose less than 40, poor feeding, jitterness, sweating, irritability, lethargy, high pitched/weak cry Interventions: breastfeed or provide frequent feedings, monitor blood glucose levels closely with heel sticks, keep warm Hypothermia (cold stress) -altered mental status “irritability or lethargy” -bradycardia, tachypnea, hypoxia -hypoglycemia & feed intolerance -hypotonia, weak suck & cry, no shivering ability Interventions: skin to skin contact, dry newborn immediately & place hat, provide care under radiant warmers, use prewarmed incubator when transporting Hypoxia (Respiratory Distress) -pathologic apnea, intercostal retractions, central cyanosis, nasal flaring, grunting, wheezing -fluid/mucus obstruction = dry, stimulate, suction -prematurity = support ventilation, give betamethasone -cardiac defect = monitor & surgery -admit to NICU for stabilization -Diagnostic: Silverman Anderson Index Necrotizing Enterocolitis -life threatening inflammation of the intestines, leading to necrosis -S&S: poor feeding, lethargy, vomiting, abdominal distention, bloody stoold Interventions: daily abdominal girth measurements, maintain fluid/nutrition, monitor labs/xray, prepare for surgery Failure to Thrive -inadequate caloric intake (socioeconomic) -S&S: signs of malnutrition, developmental delays, no eye contact Interventions: observe the child feeding, monitor type/quantity of food, monitor child’s response/positioning, monitor parent/child interaction, develop structured routine, assess parenting skill Fetal Alcohol Syndrome -intellectual disability developmental delay, hypotonia (weak muscle tone), poor sucking reflex & feeding, minimal response to stimuli, abnormal palmar creases, distinct facial characteristics Interventions: educate mother on no alcohol, monitor newborns response to feeding & weight gain pattern Neonatal Abstinence Syndrome -multisystem infant disorder due to maternal use of drugs (especially opioids) during pregnancy -within 24-72 hours after birth -S&S: high pitched cry/shrill cry, tremors, fever, diaphoresis, frequent sneezing/yawning, diarrhea Interventions: seizure precautions, decrease environmental stimuli, swaddle & gently rock, side lying position for feeding, small frequent feedings, skin protectants, perform Finnegan NAS screening every 3 hours Sepsis Neonatorum -Infection involving the bloodstream of an infant <28 days old -S&S: HR/temp/blood glucose instability, vomiting/diarrhea, sunken fontanelles, irritability Interventions: assess infection risks, IV antibiotics, draw labs, alert provider to early s&s of sepsis, obtain specimens for culture (blood, urine) as ordered Sudden Infant Death Syndrome -unexpected death of an infant less than 1yr old Education: -place infant in supine position during sleep, in sleep sack -breastfeed, up to date vaccinations, smoke free environment -provide firm sleep surface, avoid sleeping with infant, no bumper pads Neonatal Resuscitation Program -place newborn on warmer in sniffing position “appropriate for ventilating) -suction airway, dry, & stimulate for 30 secs -If HR 60-100 positive pressure ventilation -If HR below 60 epinephrine, chest compression, 30 secs after quality PPV Infant CPR 2 techniques -pointer & middle finger in sternum -2 thumbs in middle of sternum, below nipple line 1. Brachial pulse for 10 seconds 2. Call 9-1-1 3. 2 mins of CPR 100-120 compressions per minute Single rescuer: 30:2 Two rescuers: 15:2 4.Retrieve AED after 2 mins of CPR