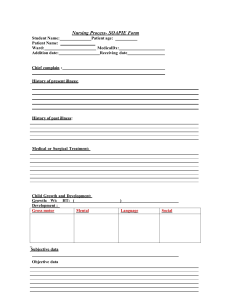
Exam 1 Study Guide Potter & Perry Chapter 2: Health and Wellness - Health: is a state of being influenced by a persons value, personality and lifestyle. Physical mental well-being and not merely absence of disease - Illness: is a state in which a persons physical, emotional, intellectual, social, developmental, or spiritual function is diminished or impaired compared with previous experience (many people find health within illness) - Wellness: is an active process of becoming aware of and making choices toward a healthy and fulfilling life. Wellness is more than being free of illness, it is a dynamic process of change and growth… a state of physical, mental, and social well-being, and not merely the absence of disease or infirmity - Acute illness: is usually short term. The symptoms appear abruptly, are intense, and often subside after a relatively short period - Chronic illness: usually last longer than 6 months - Prevention care/ Health promotion: activities to help individuals change their lifestyle to move toward a state of optimal health (a balance of emotional, local etc) 1. Primary Prevention(true prevention): prevention of the initial occurrence of a disease or an injury (programs to prevent smoking, vaccines, immunization programs, organization programs) its goal is to reduce the incidence of disease, providing intervention such as health education ** Don't have the disease 2. Secondary Prevention: early identification with prompt intervention to prevent or limit disability (early mammograms, diabetes screening) any kind of SCREENING; focuses on on preventing the spread of disease, illness, or infection once it occurs, treat people who have new cases of a disease or identify people who have been exposed to a disease but do not have the disease yet 3. Tertiary Prevention: assistance to halt further disease progress and to meet ones potential and maximum quality of life (already have disease tries to minimize it) modification helps try to manage the disease, already have it, focuses on reducing complications of long-term disease and disabilities through treatment and rehabilitation - Risk factors for diseases: is any attribute, quality, trait or environmental condition that increases vulnerability of an individual, community, or population to an illness or accident. Risk factors do not cause disease or accidents, but they increase the chance that an individual, community, or population will experience a particular disease or accident. You asses for risk factors to identify a patients health status. People can modify some risk factors such as dietary choices, whereas other risk factors such as genetics or age are nonmodifiable. - Nonmodifiable risk factors: risk factors such as age, gender, genetics and family history cannot be changed. Use your knowledge of nonmobifiable risk factors to provide secondary prevention. Ex: children are at risk of accidental deaths due to drowning, risk for asthma is higher in boys than girls - Modifiable risk factors: some risk factors such as life style practices and health-related behaviors can be modified. Ex: overeating or poor nutrition, insufficient sleep or poor hygiene. Also what can put people at risk is drug abuse, tabbaco, and activities that involve drinking alcohol or texting while driving - Environment: the environment is affected by physical, chemical, biological, social and psychosocial factors. Environment includes physical space in which we live, the water, soil, air and food that is around us and the biological, chemical, and radiological exposure we experience Chapter 3: Health Care delivery System - Primary health care (health promotion: level of prevention delivered in preventive and primary care settings such as schools, physicians offices, outpatient clinics, occupational health settings, and nursing centers): Ex: diagnosis and treatment of common illnesses, ongoing management of chronic health problems. prenatal care, well-baby care, family planning, and patient center medical home - Secondary health care (acute care): traditional reason people use health care services such as a hospital is to diagnose and treat illness. When the nature of the severity of a condition makes primary care insufficient, secondary and tertiary often become necessary. Secondary health care is provided by a specialist or agency on referral by a primary health care provider. It requires more specialized knowledge, skill, or equipment than the primary care physician or nurse practitioner can provide. Ex: urgent or emergency care; acute medical-surgical care: ambulatory, hospitals; radiological procedures - Tertiary health care: is specialized consultative care, usually provided on referral from secondary medical personnel. However, change in medical cost reimbursement, improved technology and less invasive treatment have often made secondary and tertiary care available at the primary care level. Ex: high specialized: intensive care inpatient psychiatric facilities; speciality care (such as neurology, cardiology, rheumatology, dermatology, oncology) Chapter 9: Nursing Process: - ADPIE: - Examples of assessment diagnosis, planning and intervention & evaluation Assessment: - Subjective data: patient information, are patients verbal description of their health problems, such as feelings and fear, anxiety, fatigue, physical discomfort or stress; only patients provided subject data - Objective data: physical examination findings- measurement, observation; diagnostic and laboratory data; are observed measurements of a patients healths status. Inspection of condition of a wound or observation of a patients posture and gait are examples of objective data. Ex Fahrenheit, Celsius, thermometer, centimeters etc - Assessment techniques: - Inspection: Inspect the body system using vision smell and hearing asses normal conditions and deviations. Asses color, size, location, movement, texture, symmetry, odor, and sound as you asses each body system - Auscultation: involves listening for various lung, heart, and bowel sounds with a stethoscope - Palpation: requires you to touch the patient with different parts of your hand, using varying degrees and pressure. Wear gloves when palpating mucous membranes or areas in contact with body fluids. Palpate tender areas last - Percussion: involves taping fingers or hands quickly and sharply against parts of the patient body to help locate organ borders, identify organ shape and position and determine if an organ is solid or filled with fluid or gas Chapter 10: Communication: - Therapeutic communication techniques: an interactive dynamic process involving verbal and nonverbal exchange between a nurse and patient, you develop a relationship with the patient to meet health related goals. A therapeutic relationship requires you to help a patient clarify needs and goals, solve problems and cope with situational maturational crises. Also help them explore meaning of their illness experience and sort our response to stressful situations to increase coping skills. Creating a therapeutic environment depends on your ability to communicate, provide comfort, and help patients meet their needs. Comforting strategies include gentle humor, physical comfort measures, emotional supportive statements, and therapeutic touches. Aim to listen carefully to what a patient says and pay attention to unspoken messages. Respond with empathy and attentiveness to the patient physical and emotional needs. Convey care whether you are completing you assesent, provide technical care, or respond to nurse call system. - Communication zones: - Intimate: 0- 18 in; holding an infant, patient assessment, bathing, dressing, changing dressing - Personal: 18in- 4 ft; sitting at bedside, teaching individual, changing of shift into - Social: 4 ft- 12 ft; sitting at head of a conference, making rounds with MD or HCP - Public: 12 ft and greater; speaking at community forum, lecturing to class of students - Communication techniques: Clarifying, focusing, listening, summarizing Chapter 17: Medication Administration: - Administering Mediaction: - Prescribers role: uses various formats when ordering medication, uses written and electric format. If necessary verbal orders such as telephone orders, must be counter signed within 24 hours - Types of orders - Standing: continue to administer until discontinued (antibiotics) - prn: only when needed (Tylenol for headaches) - Single one time: single dose usually the now order, one dose - STAT: up to one hour to give a STAT medication - Now: you have a little more time than STAT - Prescription: order and prescription is the same, prescription are written for patients who take medication outside the health care facility - Pharmacist role: prepare and distribute medication, are responsible for filling prescriptions accurately and ensuring the prescription are valid - 6 Rights of Medication Administration: 1. The right medication(be familiar with the medication being prescribed) 2. The right dose (weight, standard adult) 3. The right patient (name, date of birth)4. The right route 5. The right time 6. The right documentation (adverse effects) - Nursing Process and Medication Administration: - Know the patients history*** ask about allergies, medications including over the counter meds, and diet - Patients perspective: current condition, attitude about medication use, knowledge and understanding of medication use, learning needs, and expectation - Routes of Administration: - Oral (enteral:administration via human GI tract) PO, SL (sublingual/mucus membrane, under tongue) - Parenteral: drug administration outside of the GI tract (IV: intravenous, IM: intramuscular, SC: subcutaneous, fat/tissue) - Topical: creams, patch, ointment, gel - Intraocular: eye drops - Intraotic: ear drops (pull out and down for peds, out and up for adults)** Chapter 21: Cultural diversity: - Cultural sensitive care - Communication with diverse cultures - Dietary differences - Pain expression Chapter 23: Growth & Development - Play activities for different age groups - Infant play develops motor skills - Preschooler imagination is active - Safety - Toddlers safety is a huge concern as they begin to explore the world homes must be - “childproof” - Preschool children will begin to tell you how they feel and what they want - School-age students parents must educate them regarding safety issues. Accidents can occur participating in sports. Prevention of drowning, fires, burns, and other injuries; firearm safety and interacting with adults including strangers should be covered - Adolescent: substance abuse, suicide, sexual experimentation (STIs, HIV, AIDs), motor vehicle accidents, homicides and eating disorder - Young adults: self examination, routine mammography, violence, alcohol and drug consumption - Types of play: parallel: children are adjacent to each other, but do not try to influence the others behavior, play alone, but are interested in what other children are doing, solitary: independent, when the child is alone and maintain focus on its activity and is uninterested in what others are doing (2-3 years), associative: a group of children participate in similar or identical activities without formal organization or group interaction(ex two or more children playing with blocks building the same thing talking to each other but not working together, cooperative: involves the division of effort to reach a common goal, everyone wins - Reducing fears of hospitalization for different age groups - Toddlers if hospitalized need their parents present and familiar items around then to ease anxiety - Preschooler when hospitalized, it is important for the parents to be present to reduce child fear, let hospitalized children touch and play with medical equipment as appropriate - School age if hospitalized this age group can describe their pain and tell you how they feel - Adolescents when hospitalized feel their independence is restricted by all the rules and regulations Chapter 25: Family context in nursing: - Health and Illness within the family: Hockenberry (Wong) Chapter 2: Social cultural and religious influence on child health promotion: Chapter 3: Family influences on child health promotion: Chapter 12: Health promotion of the toddler and family: - Ritualization - Safety - Sleep patterns - Play activities - Gross motor, fine motor, cognitive development - Nutrition Chapter 13: Health promotion of the preschooler and family - Fears of this age group - Safety - Sleep patterns - Play activities - Gross motor, fine motor, cognitive development - Nutrition Hunt Chapter 1-3 - Definition of community - Current nursing practice trends and nursing interventions - Prevention of disease and injury in community based nursing health promotions