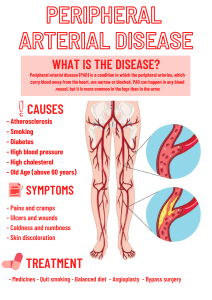
Altered Peripheral Tissue Perfusion Overall purpose This instructional unit focuses on patients with Peripheral Vascular Disease: arterial and venous. The Nursing Process and Readiness for Practice Framework will be used as the approach for patient care. His study guide 1. What lifestyle changes? (BIG) 2. Physical symptoms of PAD 3. Medications for PAD → And things you won’t see but will see for venous things. 4. What diagnostics things for PAD Peripheral Artery Disease - Involves progressive narrowing and degeneration of arteries of upper and lower extremities - Atherosclerosis is leading cause in majority of cases, which why it is closely tied to CAD. - Patients with PAD are more likely to have coronary artery disease and/or cerebral artery disease - Remember, this is an arterial disease, not a venous disease → with venous return insufficiency diseases fluid overload is a common major difference which often requires diuretics (review from earlier semesters). - Think of how they’re have all sorts of obstructions caused by malformations in their arterial system → inhibiting blood flow to their lower extremities. “Piping is broken or rotting” Pathogenesis of Atherosclerosis From the textbook: Pathogenesis of atherosclerosis. A, Damaged endothelium; can cause weaking of the artery itself... B, Fatty streak and lipid core formation. C, Fibrous plaque covers the lipid core. D, Complicated lesion: Plaque rupture with thrombus formation. 1 - Notice how these are related to lifestyle, and how we need to educate on the changes. - People who quit smoking that had had Berger’s started to do better, while those who continued needed amputations. - Complicated lesions can be caused by cancer - Progressive narrowing and degeneration of arteries in the lower (predominantly) and upper extremities. - When talking about aneurysms, the most common ones are below your renal arteries, aka abdominal aortic aneurysms (AAA) PAD - Peripheral artery disease (PAD) may affect - Iliac artery - Femoral artery - Popliteal artery - Tibial artery - Peroneal artery Common Sites of Atherosclerotic Lesions - A lot of the arteries we’ll be talking about are the ones below the renal artery and that feed into calf, gluteal, femoral, and upper leg. - Most patients come into the clinical due to intermittent claudication. - Some patients can show issues with the tibial arteries, perineal, posterior tibial. Etiology - Typically appears at ages in sixth to eighth decades of life - Largely underdiagnosed - Risk factors: - Smoking - Elevated C-reactive protein (CRP) - Changed by cessation - Uncontrolled hypertension - Diabetes - Family history - Can control it better with diet and - Very good chance you’ll develop it. insulin. - Increasing age - Hyperlipidemia - Obesity - Controlled with better diet and - Sedentary lifestyle medications. - Stress → take a good look at what is modifiable with diet and lifestyle changes 2 Case Study - B.D., a 62-year-old man, complains of pain in his lower legs when walking his dog. - Pain is relieved with rest. - Has pain on exertion = intermittent claudication; a classic sign of PAD. - When not relieved with rest, it is more severe/critical. - Primary care, outpatient situation. - He has a history of hypertension and hyperlipidemia. - He smokes one pack of cigarettes per day. Clinical Manifestations - Classic symptom of PAD – intermittent claudication - Ischemic muscle pain that is caused by a constant level of exercise that is resolved in 10 minutes or less with rest. - Reproducible - Pipe dream: have pt walk for 30 minutes, take a break, and see how long it takes for pain to solve - Actual situation: Tell patient to walk for however long it takes for their legs to hurt, once they do have them rest, and time how long for symptoms to subside. Then try doing more exercise, repeat. See if it happens in a cyclical fashion. - Paresthesia – from poor blood supply - Numbness or tingling in the toes or feet - May get ulcers at the very tips of their toes, or between their toes, that are not going to heal well (d/t poor perfusion). - Produces loss of pressure and deep pain sensations - Injuries often go unnoticed by patient because they can’t feel sensation well. - Nerves end up dying because they are not getting enough blood supply d/t the poor arterial perfusion. - Thin, shiny, and taut (tight) skin → versus the edematous PVD with weeping skin - Loss of hair on the lower legs - Diminished or absent pedal, popliteal, or femoral pulses - Pallor of foot with leg elevation - Will become paler in color as we lay the patient flat. - When legs are down, the blood is able to flow easier due to gravity, so they will be more red. → Reactive hyperemia of foot with dependent position - Pain at rest - As PAD progresses, they get into critical limb ischemia territory. - Occurs in feet or toes - Aggravated by limb elevation - Because having more trouble to oxygenate as leg height ↑ - Occurs from insufficient blood flow - Occurs more often at night - Some people like to sleep sitting up in their chairs because of this. 3 → This is also true with venous insufficiency as well d/t fluid overload from right side of heart (which a lot of the time comes from CHF), and this impacts their lungs once they lay flat. - When assessing B.D., you find that his feet are pale and cool to touch. - This represents poor perfusion - He has diminished pedal and posterior tibial pulses and decreased sensation. - If pedal pulses are absent, use a doppler. - It is possible that he has some form of circulation down in his ankle area d/t collateral circulation. - He has a small open area on the lateral side of his left ankle. - Probably not healing well? → Patients who had chronic PAD and took too long to see MD may have enough collateral circulation (micro growths) of arteries feeding their lower extremities; but these don’t last long. Critical Limb Ischemia (CLI) - Characterized by: - Pain that doesn’t get relieved by rest. - Chronic ischemic rest pain lasting more than 2 weeks - Get worst ulcers: arterial leg ulcers that can be gangrenous - typically end up with amputations once gangrenous. → WANT TO CATCH THIS EARLY Complications → More at risk for infections because their tissue is starting to die. - Atrophy of skin and underlying muscles - Tissue necrosis - Delayed healing - Arterial ulcers - Wound infection - Nonhealing arterial ulcers and gangrene are most serious complications - Can spread and become a septic infection. - May result in amputation - If adequate blood flow is not restored - If severe infection occurs → Which ultimately makes them less ambulatory → decondition further because they aren’t going to exercise → no microcirculation created. Diagnostic Studies - Doppler ultrasound; especially if you can’t palpate anything. - Segmental blood pressure - A means of comparing blood pressure measurements using a Doppler device in the upper thigh, above and below the knee, at the ankle, and on the arm to determine any constriction in blood flow. - Ankle-brachial index (ABI) – huge with PAD - The ratio and difference of a blood pressure done at our arms and ankles. - Done using a hand-held Doppler 4 - Angiography and magnetic resonance angiography - Go into the arteries and take a look - Angiography or arteriography is a medical imaging technique used to visualize the inside, or lumen, of blood vessels and organs of the body, with particular interest in the arteries, veins, and the heart chambers. - We try to stay noninvasive, but if there is pain not relieved at rest, they may go to a cath lab and do an angiography. - Duplex imaging - Bidirectional, color Doppler Interprofessional Care - Risk Factor Modification - Tobacco cessation - How long have you been smoking? What can we do to help you stop smoking (e.g. patches, supplement with something else [soda, m&ms, peanuts], Wellbutrin). - Glycosylated hemoglobin <7.0% for diabetics; help them get good glucose control. Glucose tears up vessels. - Aggressive treatment of hyperlipidemia – get them on statins - Even if they have a good LDL value but Dx with PAD and have a high risk factor for worsening, they will be given aggressive statin medication to prevent any other complications. - e.g. Simvastatin. - BP maintained <140/90 - Hard crowd to get them to do that, because when they start to walk they’re in pain. May need to get them on a pain medication regimen if they have poor pain tolerance. - There is a specific physical therapy for these pts: Vascular Physical Therapy. - Focus on how long they can walk per day and increase it every day. Goal: increase collateral circulation. 5 Drug Therapy - ACE inhibitors – ‘prils’ - It will help increase walking distance, thus help their PT regimen. - As well as help with blood flow. - Ramipril (Altace) ↓ Cardiovascular morbidity ↑ ABI ↓ Mortality ↑ Walking distance ↑ Peripheral blood flow - Antiplatelet agents - Aspirin – 81mg - Clopidogrel (Plavix) – 75mg → Want to make the platelets slippery and easier to flow because arteries are narrowing. Otherwise, platelets might start clumping/sticking up together. - Drugs prescribed for treatment of intermittent claudication - Cilostazol (Pletal) – CONTRAINDICATED WITH HF - Inhibits platelet aggregation - ↑ Vasodilation - Adversely can lower ejection fraction (why not given with HF) - People with CAD may have HF, or it can lead to HF. - Pentoxifylline (Trental) - Improves deformability of RBCs and WBCs - Decreases fibrinogen concentration, platelet adhesiveness, and blood viscosity - By making the blood cells more flexible. Helps with red blood cell “flow” - Lowers blood viscosity; helps with blood flow with pt at risk for clots or with 90% narrowing of arteries. Makes the cell more flexible and squishy? Case Study B.D. is ordered the following drugs: Aspirin 81 mg daily Simvastatin (Zocor) 10 mg hs - We have cholesterol surges while we sleep. Ramipril (Altace) 2.5 mg daily Pentoxifylline (Trental) 400 mg tid → There is no diuretics here or anticoagulants (“it would do nothing in this case”). Exercise Therapy - Note: they are challenging patients to work with because they are in pain; thus we need to push them onto a medication regimen pair with physical therapy. → If they’re working with a vascular surgeon, they may know a vascular PT. - Try to connect with a vascular team, the cities are going to be most common. - Exercise improves oxygen extraction in legs and skeletal metabolism - Walking is most effective exercise for individuals with claudication - 30 to 45 minutes daily, 3 times/week - Walking can help create collateral vessel circulation which can help to prevent lack of circulation leading to CLI and other ischemic leg issues. - Need walking for the impact, gravity on ground sort of thing. 6 - There is a strong link that people don’t need invasive surgery (stenting with interventional radiology) as long as they do medication with a walking regimen. - Outcome was basically the same. Nutritional Therapy - BMI < 25 kg/m2 - Waist circumference <40 inches for men and <35 inches for women - Recommend reduced calories and salt for obese or overweight persons - Really want to reduce fat as well. - Salt increases fluid intake in people’s bodies - Take away: may want to include a dietician; they may be put on a cardiac diet. Maybe vegan. Interprofessional Care: Leg With Critical Limb Ischemia (point of almost no return) - Goal: create new blood flow again by revascularizing. - Revascularization via bypass surgery - Utilizing grafts to reestablish blood flow in blocked / narrow vessels [usually grafted from leg / arm / chest] - Percutaneous transluminal angioplasty (PTA) - Balloon tipped catheter which places a stent - IV prostanoids (iloprost [Ventavis]) - Med that improves blood flow by relaxing blood vessels, especially in the lungs, which is one reason this is readily used for Pulmonary Arterial Hypertension. It is a vasodilator and can be given multiple ways including nebulized for direct effect in lungs. - Spinal cord stimulation - SCS improves micro blood flow, can diminish ischemic pain, and may reduce potential for amputations in patients with PAD. - Angiogenesis / stem cell therapy - If a CLI patient cannot be revasc’d, interventions do not work, and / or cannot be subjected to PTA, angiogenesis can be attempted. Angiogenesis is growth and creation of blood vessels from an existing concentration of blood vessels, another name common for this is Stem Cell Therapy. - The basic goal for Critical Limb Ischemia is create blood flow to the distal blood vessels with angioplasty or through revascularization, but if that cannot be achieve, or if a patient is too high risk for procedures other methods can be utilized. For the most part with CLI (Critical Limb Ischemia) they will do conservative treatment - Conservative Treatment – try to stay away from surgical interventions. - Protect from trauma (e.g. numbness → trauma) - One prevention is to wear shoes, watch where you’re walking; to avoid bumping into or stepping onto things. - Decrease ischemic pain - Pain medications - Prevent/control infection – abx? - Improve arterial perfusion - prevented by medications and walking 7 B.D. returns for follow-up in 3 months. His BP and lipid levels are stabilizing, but he complains of increasing leg pain at rest. His physician determines that it is time to consider an intervention to improve his circulation. - He may be heading towards CLI, so this is when we consider invasive procedures. Interventional Radiology Procedures - Indications - Intermittent claudication symptoms become incapacitating - Pain at rest - Ulceration or gangrene severe enough to threaten viability of the limb - If became septic that will kill him real quick. - Interprofessional Care Surgical Therapy - Most common surgical approach: bypass grafts - Peripheral artery bypass surgery with autogenous vein or synthetic graft to bypass blood around the lesion - PTA with stenting may also be used in combination with bypass surgery - Go into the are where narrowing is present and open a balloon up there. Do some “roto routing”, dissolving some of the clots or whatever the formation is and pull it out. Nursing Management: Nursing Assessment - Past health history - Diabetes mellitus - Hyperlipidemia - Smoking - Obesity - Hypertension - Exercise intolerance - Loss of hair on legs and feet; shiny and pale - No circulation to feed the hair follicles. - Decreased or absent peripheral pulses - May still have sensation and some function with little bloody supply, but this is do to collateral circulation. - Intermittent claudication Nursing Management Planning - Overall goals for patient with PAD - Adequate tissue perfusion - Get them involved with exercise. - Relief of pain - Increased exercise tolerance - Do a lot of cheerleading for these patients. - Intact, healthy skin on extremities - Prevention of pressure injuries and infection - Increased knowledge of disease and treatment plan 8 Nursing Management Nursing Implementation - Health Promotion - Identification of at-risk patients - Specific recommendations for individual factors such as diabetes - Diet modification - If they need help with controlling diabetes have them meet a diabetes educator. - Proper care of feet - If they have foot problems you can connect them with a podiatrist. - Avoidance of injuries - If they have numbness or tingling, they really need to wear protective shoes all the time. They won’t feel sharp sides of a table, they can break their toe - Acute Care - Frequently monitor after surgery, and compare both sides while wanting to see improvement. - Skin color and temperature - Is pallor decreasing, warm to touch, etc. - Capillary refill getter better? - Presence of peripheral pulses distal to the operative site present? - Sensation and movement of extremity improving? - May not get sensation back immediately. When people re-perfuse after having a long history of arterial damage, their leg may feel like it’s on fire. Indicating that the blood is returning and working on all the damaged tissue (nerves, arteries, etc.). They will need some pain control. Say someone’s right leg was balloon stented and blood flow returned, the left leg is going to be worked on later. The leg that was revascularized and now has fluid/blood flow going into it, is going to take blood from the other (left) leg, causing more pain for the left one. So whichever side you revascularize if they both had the same issue will kind of steal the blood from it Will need to have the other surgery soon afterwards because patient will report increasing pain. Can’t do both at the same time, that’ll cause them to be bed bound for a while. Buerger’s Disease (“Thromboangiitis Obliterans” TAO) - RARE! - No atherosclerosis - Young men (< 45 yo) - Inflammatory disorder - Smoking – cigarettes or marijuana - No build up in the arteries - Something in smoking that is causing - Small to medium sized arteries and veins the immune system to respond. of upper and lower extremities - Poor oral care – periodontal infections - Occasionally, arthritis at wrists or knees develops before blood vessels become blocked. - These patients have auto-amputation issues. → So what should we tell our patients with confirmed Buerger’s disease about methods to prevent complications? - Preventative lifestyle choices 9 - Acute phase - There is such profound inflammation causing they arteries in the hands and feet to close and the blood begins to clot (where blood can pool, things clot) -These clots obstruct blood flow; can get bad enough that it will lead to amputations and chronic phase… - Chronic phase - Thrombosis and fibrosis cause tissue ischemia. Cause necrosis and autoamputations. - Symptoms - Intermittent claudication - Rest with pain - Ischemic ulcerations - Skin signs – color, temperature, paresthesia, superficial vein thrombosis and cold sensitivity - Cold or temperature fluctuations (hot-cold sensitivity), where this is a bit more pale and numbness. Diagnosis - Ultrasound – blood vessels narrowing - Angiography – visualize the inside of blood vessels - Patient drinks/takes a fluid containing a high radiological isotope that lights up when using an x-ray scan or radiological scan once absorbed into blood stream. See pictures above. - May see blockages/narrowing due to less blood flow to an area - May see corkscrewing or spiraling pattern of arteries around a blockage. - This is a pattern of regrowth (collateral circulation). - Looking more for microclot formations on images, micro circulation. To r/o atherosclerosis you have to look at history and see if there are hyperlipidemia/fat deposits. - You can see difference between narrowing and clots. Buerger’s Treatment - Preventative: - Stop smoking - Keep walking - Definitive treatment - Avoid trauma to extremity - Avoid cold if sensitive - Antibiotics and wound care - Meds – Goal: try to get more blood flow, stop the clot formation; then stop pain. - Calcium channel blockers - Cilostazol - NOT IF THAT HAVE ANY HF - Sildenafil (Viagra) - Vasodilate - Iloprost – most promising - Helps with constricted blood vessels. - Aspirin? - Amputation if necessary 10 - Sympathectomy - A lumbar sympathectomy can reduce pain and help heal ischemic ulcers of the lower limbs in the patients with Buerger’s disease which can help dilate small blood vessels to help blood flow. - Can cauterize nerve ending to help reduce ulcers Raynaud’s Phenomenon - Episodic vasospastic disorder of small arteries, most often in fingers and toes (can be seen in nose too). - Have “cold spells” - Face very sensitive to environments. - Women – 15-40 higher prevalence - May occur with other diseases – lupus, RA, scleroderma - Vibrating machinery - Found easily in people who work on a production line. - “I was working, but all of a sudden I couldn’t feel my fingers and I got really cold” - Can become apparent when emotionally upset - Cold environments - Really easy to detect in colder areas - Get irregularly cold and irregularly sensitive to it. - Heavy metal exposure - Hyperhomocyteinemia – seen in many degenerative diseases, mostly treated with vitamin B supplements - Strong genetic link to this. “Does your family have Raynauds?” - Vitamin B issues. - Potentially genetically linked Raynauds - symptoms - Vasospasm induced color changes to distal extremities – vasospasms are causing the arteries to close a little bit as well as a reaction to the cold - Fingers, nose, ears, and toes! - From white, mottled to blue/black - Look like frost bite. - Rubor when blood flow is restored - Throbbing, aching pain, tingling and swelling in the hyperemic phase - Similar to a pt getting revascularized once blood started flowing again. - Once blood starts flowing again, we Raynaud’s patient to seek worth - Risk factors increasing episodes include - Emotional upset - Cold exposure - Tobacco use - Caffeine use 11 Raynauds - treatment - Loose warm clothing in layers - Avoid temperature extremes - Protect from being cold - Try their best not to be exposed to the cold. - Stop all vasoconstrictors – tobacco, caffeine, cocaine, amphetamines, pseudoephedrine (nasal sprays) - Stress management - Don’t panic when cold, just seek warmth. - ↑A lot of these are lifestyle changes↑ - Drug therapies - Calcium channel blockers – promote vasodilation - Critical ischemia – iloprost, bosentan (look up) - If they’re to the point of having actual frostbite, they may need some debridement or amputation; then they may need something like iloprost. Iloprost is heavy duty stuff. - Sympathectomy in severe cases – decreases ability to sweat, blush, or react to cold as much. Permanent, last resort. - Considered a last-ditch effort Aortic Aneurysm - Permanent, localized outpouching or dilation of the vessel wall. - Dilated segment of an artery caused by weakness and stretching of the arterial wall - Dissection is a tear - Most common site: Aorta; Most common type is Abdominal Aortic Aneurysm (AAA) - It’s going to be below the renal arteries. - Risk factors: - Age (>50 yo) - History of CAD - Obesity - Male - HTN - White and Native - Tobacco use - Previous stroke Americans higher risk Etiology - Mostly in the abdominal aorta (3/4), below the renal arteries - Because there is less elastin and the tissues are not that strong in this area; causing them to pouch more. - May involve aortic arch or thoracic areas (1/4) - If involved, first indication is confusion; vessels going into the brain get blocked off, causing blood supply issue - Incidence increases with age - Men greater than women - The greater the size of the aneurysm the greater chance for rupture - Abdominal aorta size greater than 3 cm = aneurysm - Extremely serious: people can bleed out super quickly. - Strong genetic link with connective tissue diseases. - Marfan’s Syndrome (breakdown of - Polycystic kidney disease vascular elastic tissue) - Coarctation of the aorta - Ehlers-Danlos syndrome (collagen - Bicuspid aortic valve defect) 12 - Acquired - Atherosclerosis - Trauma - E.g.: in a MVA and patient hit the steering wheel hard. Their heart smashes against the front of their chest, causing some tearing in the aorta. - Infections – syphilis, polyarteritis Classifications - By location - Aortic, thoracic, abdominal - By etiology - Atherosclerotic, syphilitic, hypertensive (common) - By appearance - True – A true aneurysm is one in which the wall (intima, media and adventitia) of the artery forms the aneurysm, with at least 1 vessel layer still intact. True aneurysms are subdivided into fusiform and saccular. - Fusiform – all the way around the artery; circumferential and relatively uniform in shape. - Saccular – outpouching in only one plane; pouchlike - False – pseudoaneurysm – pouching of one layer of disruption - Disruption of all arterial walls held together by bleeding that is contained by surrounding anatomic structures. - Part of the wall starts to peel back/break down; seen usually with pts with longstanding HTN issues. - Usually from trauma, infection, graft surgery (at the site of the graft-to-artery anastomosis), or leakage after cath lab procedure; E.g. femoral artery catheter or balloon pump is lodged incorrectly, or the stent ends up tearing. A, True fusiform abdominal aortic aneurysm. B, True saccular aortic aneurysm. C, False aneurysm, or pseudoaneurysm. D, Aortic dissection. → Aortic dissection is misnamed “dissecting aneurysm.” It is not a type of aneurysm. Results from the creation of a false lumen between the intima (inner lining) and the media (middle layer) of arterial wall. Aortic dissection is classified based on the location of the dissection and duration of onset. Signs and Symptoms of Aneurysm - Thoracic – often asymptomatic and less common - Chest pain - Pressure on associated anatomy may produce symptoms - Hoarseness, dysphagia, increased JVD, edema of face/arms. - Remember with tamponade: when there’s pressure against the heart, the heart can’t pump effectively. - When the thoracic aneurysm is really big, it will push up against neighboring organs and create pressure against the heart. - May hear a bruit upon cardiac auscultation with muffled heart noises. 13 - If caught early enough, normally do conservative treatment with thoracic. - Abdominal - May mimic back pain, kidney/ flank pain, epigastric pain, constipation - Often found on routine exam - X-ray - See an outpouching - Pulsating mass to the left of umbilicus - Bruit may be auscultated; a turbulence of fluid splashing against the vessel wall that sounds like a whooshing noise. - Will be located in the upper quadrants of your abdomen. - No deep palpation if you hear bruit! It may be almost to the point of a rupture. - These types of patients need to get imaging Case Study E.O., a 74-year-old woman, comes to the ED with deep chest pain radiating throughout the chest to the back. - This could be a heart attack. So we need to r/o MI with EKGs She reports that she smoked 1 pack of cigarettes/day for 20 years, quitting 5 years ago. She weighs 212 lb. Complications - Rupture! - If they have a micro rupture or a pseudoaneurysm with a diesstion (and just a little bit of the layer of the arterial wall is open) and there is a seeping of blood, you will see back or flank ecchymosis; similar to Turner’s sign. - AAA – into retroperitoneal space - Back pain - Back or flank ecchymosis – Grey Turner’s sign (see pancreatitis) - Thoracic or abdominal – >90% will not survive the rupture – depends upon how fast the leak is – see shock lecture from 75B Diagnosis - Physical Exam (no deep palpation) - X-rays – often incidental CXR, abdominal x-ray - EKG – if due to chest pain and occlusion of coronary arteries - Cardiac labs, cardiac enzymes, etc. - May clue us into what potential arteries are involved. - Echocardiogram - CT – most accurate – but dangerous! If ruptures! - Dangerous d/t the contrast; they put in a lot of fluid with a lot of force. - Angiography – to map and size the system, as well as look at the inside of the arterial walls. 14 Case Study Based on E.O.’s symptoms, which type of aneurysm would you suspect? Sounds like thoracic (not epigastric or abdominal issues) What are the immediate concerns for her? We’re worried about hemorrhaging, as well as her blood pressure (we don’t want to cause an ↑ in pressure due to anxiety, so keep in mind to keep it under control) while trying to rule out diagnosis. E.O. has an ECG in the ED that rules out an acute MI. Chest x-ray is suspicious for thoracic aneurysm. She is now scheduled to go to radiology for CT scan of her chest. Treatment - If it is a small aneurysm - Nothing – prevent rupture - Modify risk factors – what are those? - Get blood pressure under control; n - Control their hyperlipidemia - Cessation of smoking - Annual monitoring of size – patients will often know - Greater than 5.5 cm = may consider surgical repair; OR if it’s a genetic disorder, expands too rapidly, becomes symptomatic, or risk of rupture is high. - Can be elective or emergent → Emergent when someone is highly symptomatic, e.g. having a ton of pain, bruising, shows that some dissection is starting to occur, arterial wall layers are super thin => ↑ risk of rupture. - If elective will have time to correct electrolyte, hydration, coagulations and hematology Case Study E.O. returns from CT scan with a diagnosis of a thoracic aortic aneurysm measuring 5.2 cm. A surgical consult is ordered and E.O. is scheduled for surgery in the next hour. Open vs. Endovascular repair - Open - Large abdominal incision - Cross clamp the aorta - Insert synthetic graft or a stent - Close the native wall by stitching back around. → These patients are not going to get the correct perfusion when aorta is being worked on. They’re at really high risk of clotting during this surgery. - Endovascular - Minimally invasive procedure - Go through the femoral artert - Need to have good iliofemoral arteries for access 15 - Endograft inserted and deployed (complex surgical-grade malleable fabric) → Can be really dirty going through this way (high risk of infection). They need to be carefully monitored afterwards, as well as have a pressure clamp on their leg wrapped really tightly for an hour. High risk for throwing clots. Postoperative complications - Endoleak – most common, when blood leaks back into the aneurysm sac after an endovasc procedure. Can cause: - Aneurysm above or below the graft → Blood can seep in and get past the wall of the stent and cause another dissection. - Stent was either not placed perfectly or occluding enough, and blood begins to pool and form clots around it, which puts more pressure on the side of the aorta → pouch more, and get a worsening dissection. - Dissection - Graft thrombosis - Renal artery occlusion - Infection - Stent migration and occlusion - Hematoma - Acute myocardial infarction (AMI) - Sexual dysfunction - Renal failure - Spinal cord ischemia with paralysis - Bowel and bladder incontinence Abdominal Compartment Syndrome - Emergency repair of ruptured AAA - Intraabdominal hypertension can happen with this emergency repairs. - Decreases blood flow to the viscera - Decreased end organ perfusion - Multisystem organ failure – see shock lecture - 25% occurrence in open AAA - 70% mortality - ICU patient! - Measure intraabdominal pressures – through transducer in foley or direct - Blood transfusions too. → Reason why watching and waiting is preferred. They will have a better quality of life this way instead of surgery after surgery. Super high risk. Nursing Management Assessment - Thorough history and physical exam - Watch for signs of cardiac, pulmonary, cerebral, and lower extremity vascular problems - Cerebral: altered mental statys - Cardiac: bad perfusion, abnormal sounds, new rhythms - Pulmonary: trouble breathing, back up of fluids - Lower extremity vascular problems: numbness, tingling, color, temperature 16 - Find out when it was first detected, how bad it was, so we can establish baseline data to compare postoperatively - If worst, surgery was not a success. → Want the pulses of these types of patients, especially after revascularization, to have pulses of a 1 or 2 (basic pulses). You DO NOT want bounding (+3), indicates pressure maldistribution. Case Study E.O.’s assessment findings include Alert and oriented to person and place; but disoriented to time BP 158/98 (elevated), P 92, R 22 (minutely elevated) Verbalizes pain at 6 on 0-10 scale Bilateral pedal pulses audible by Doppler → Doesn’t look like she is doing so well. What else are we worried about? Worried about clots, but don’t want to put them on anticoagulants before a procedure. - Note quality and character of peripheral pulses and neurologic status - Mark/document pedal pulse sites and any skin lesions on lower extremities before surgery Nursing Management Planning - Overall goals include - Normal tissue perfusion - Intact motor and sensory function - No complications related to surgical repair Nursing Management Nursing Implementation - Health promotion - Alert for opportunities to teach health promotion to patients and their caregivers - Teach how to make modifications (change their diet, quit smoking, etc.) - Encourage patient to reduce cardiovascular risk factors - Schedule follow up appointments to help ensure graft patency after surgery - Imaging, someone responsible for tracking them Case Study E.O.’s daughter is called and arrives in the E.D. Her daughter is very anxious and has many questions regarding the impending surgery. E.O.’s surgery goes well and she arrives in ICU. What are your priorities in monitoring her in the immediate postoperative period? Pulses, all the basic assessments (CSM checks, cap refill, doppler q hour), titrate vasopressors, - Acute Intervention - Postop - Will be in ICU, do assessments q4. - Titrate vasopressors, want mean arterial pressure of 60 – 70 (normal is 60 – 100) in order to keep pressure system low.* 17 - Peripheral perfusion status - Pulse assessment - Mark pulse locations with felt-tip pen - Extremity assessment - Temperature, color, capillary refill time, sensation, and movement of extremities - May need to use a Doppler to assess - Renal perfusion status; make sure we didn’t damage the renal artery system/kidneys. - Urinary output - CVP/PA pressure - Fluid intake - Blood urea nitrogen/creatinine - Daily weight Graft patency* - When aneurysms do need to be surgically maintained or grafted, maintain graft patency during acute care. - An adequate BP is important to maintain graft patency. Prolonged low BP may result in graft thrombosis. Give IV fluids and blood components as ordered to maintain adequate blood flow. Monitor CVP or PA pressures and urine output hourly in the immediate postoperative period to assess the patient’s hydration and perfusion status - Avoid severe hypertension, which may stress the arterial anastomoses, resulting in leakage of blood or rupture at the suture lines. Drug therapy with IV diuretics (e.g., furosemide) or IV antihypertensive agents (e.g., labetalol, metoprolol, hydralazine, sodium nitroprusside [Nipride]) may be indicated. - Ambulatory and home care - Encourage patient to express concerns, that we are available for questions. - Vascular follow up appointments. - Instruct patient to gradually increase activities - No heavy lifting, no marathons, no aggressive gardening, no 18 holes of golfing. - Teach about signs and symptoms of complications - Infection (feverish, sweaty, HR) - Neurovascular changes (for family/caretakers) Nursing Management Evaluation - Expected outcomes - Patent arterial graft with adequate distal perfusion - Adequate urine output - No signs of infection 18 Aortic Dissection - Often misnamed “dissecting aneurysm” - Not a type of aneurysm, it is a pseudoaneurysm. - Result of a false lumen through which blood flows - Classified by location and duration of onset - Type A dissection affects the ascending aorta and arch, requiring emergency surgery. - Type B dissection begins in the descending aorta, allowing for potential conservative management. - We also describe dissections as acute (first 14 days), subacute (14 to 90 days), or chronic (greater than 90 days) based on symptom onset. - An area that is created and torn, which starts to pouch out a false lumen to which blood flows in and gets trapped. Etiology and Pathophysiology - Due to degeneration of the elastic fibers in the arterial wall - Chronic hypertension hastens the process - Tear in inner layer allows blood to “track” between inner and middle layer - Depends on location of intimal tear and extent of dissection Clinical Manifestations - Pain characterized as - Sudden, severe pain in anterior part of chest, or intrascapular pain radiating down spine to abdomen or legs - Described as “sharp” and “worst ever” - May mimic that of MI - Need an X-ray imagine as well as an EKG to r/o MI - Cardiovascular, neurologic, and respiratory signs may be present - If aortic arch involved - And impacts coronary artery (not enough blood flow), neurologic deficiencies may be present (people may seem confused) - Cardiac tamponade (if they have some pouching that is near the heart, creating pressure). - Severe, life-threatening complication - Occurs when blood escapes from dissection into pericardial sac - This can constrict heart; may need cardiac chest tube. - Clinical manifestations include - Hypotension - Muffled heart sounds - Narrowed pulse pressure - Pulsus paradoxus - Distended neck veins - Aorta may rupture - Results in exsanguination and death - Hemorrhage may occur in mediastinal, pleural, or abdominal cavities 19 - Occlusion of arterial supply to vital organs - If you’re going to bleed out, you won’t have arterial supply to other areas od the body. Diagnostic Studies - ECG to rule out MI - Chest x-ray - 3-D CT scan; without contrast - Transesophageal echocardiography - MRI - No MRI if the person is unstable Collaborative Care - Initial goal is to take the pressure of the dissection. - ↓ BP and myocardial contractility to diminish pulsatile forces within aorta - Drug therapy - IV β-adrenergic blocker - Esmolol (Brevibloc) - Other antihypertensive agents - Calcium channel blockers - Nitroprusside - Angiotensin-converting enzyme inhibitors - Morphine - If they’re trouble breathing and their blood pressure can sustain it/ (From slide: Would you want to give anticoagulation to prevent clots? Think about this…) Nursing Management - Preoperative - Semi-Fowler’s position - Maintaining a quiet environment - Anxiety and pain management - Opioids and tranquilizers as ordered - Continuous IV administration of antihypertensive agents - Continuous ECG and intraarterial pressure monitoring in the ICU - Observation of changes in quality of peripheral pulses - Frequent vital signs - Postoperative - See aneurysm postop care (discussed earlier) - Discharge teaching - Therapeutic regimen - Antihypertensive drugs and side effects - If pain returns or symptoms progress, instruct patient to seek immediate help Chronic Venous Insufficiency (CVI) and Venous Leg Ulcers - CVI—abnormalities of venous system include edema, skin changes (follicle death, skin can be translucent because bound by so much fluid), and venous leg ulcers (seen where we a dependent, e.g. when sleeping it will be on the back of the foot, sometimes on top of the foot) - Mepilex with some triad, creams, etc. A lot of serous fluid seeps out. - Etiology and Pathophysiology - Primary varicose veins and PTS 20 - Ambulatory venous hypertension - Serous fluid and RBC leak results in edema and chronic inflammatory changes - Hemosiderin—brown skin discoloration - Skin is hard, thick, and contracted Clinical Manifestations and Complications - Lower leg — brown, leathery, and edematous - Eczema with itching and scratching (Table 37-1) - Venous ulcers → - Pain especially with dependent position, challenging for these people to sleep. - Risk of infection - Their tissues start to get disintegrate because they aren’t getting any perfusion; high risk of infection. - Compression for healing and prevention of recurrence - Stockings, bandages, IPCs, wraps, Mediplexes, etc. to help return some of that fluid back to their heart. Crucial for them to be on diuretics, otherwise wounds will get weepy and it’ll just slough off. - Teach proper fit and application - Assess for PAD prior to compression - Major difference: there is no fluid component. It is arterial, not venous. - Think of venous as a fluid reservoir; if reservoir isn’t working, it is going to leak towards the path of least resistance (in the case of a body, it’ll go to be bottom). If they lay, it’ll go to hollow cavities (e.g. lungs) - Activity guidelines and limb positioning - Avoid prolonged sitting or standing - Positional: if they lay down, they feel like they’re choking on their own fluid and can’t breathe. - Affected by gravity a lot. - Elevate legs above heart - Daily walking - Have less pain when they are walking (challenging for them to sit idly). - Going to have paresthesia, numbness, tingling - Avoid trauma - At high risk for amputation, d/t ulcers → gangrene/necrosis. - Daily foot and leg care - May also diabetic, so they will be followed by podiatry. - Wound care and dressings — moist environment; lots of seepage. - Challenging: really need to get the venous issue under control with diuretics while being on a cardiac diet - Nutrition — adequate protein, vitamins A and C, zinc; cardiac diet - Diabetics — normal blood glucose levels - Monitor for infection - Debridement, excision, antibiotics - Drug therapy — pentoxifylline or micronized flavonoid fraction - Pentoxifylline – help RBCs make it to the area they want to go to by being flexible. 21 - MPFF - improves venous tone and lymphatic drainage, and reduces capillary hyperpermeability by protecting the microcirculation from inflammatory processes. - Potential requirement for diuretics - In order to get fluids under control - Need to make sure her BP is okay for this. - Other: skin replacement (e.g., grafts) - Daily moisturizing - Super necessary, even if skin sloughs off onto your gloves. 22