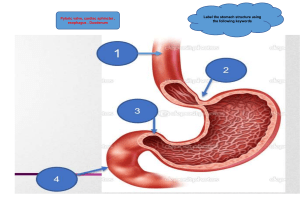
Anatomy & Physiology Cardiac System Med Surg: Cardiac Blood flow of the heart 1. Deoxygenated blood gets “vacuumed” back to the vena cava (superior and inferior vena cava) 2. Right Atria - Tricuspid Valve - Right Ventricle. 3. Through the pulmonary valve & pulmonary arteries into the lungs to drop off CO2 & pick up O2 (oxygen) in the capillaries. 4. This oxygenated blood is then pumped through the pulmonary veins. 5. Left Atrium - Mitral Valve (bicuspid valve) - Left Ventricle • Side note: Left ventricle is the “BIG momma pumper” pumping oxygen rich blood OUT to the body = cardiac OUTput 6. Left Ventricle pumps O2 rich blood through the aortic valve & then finally 7. The Aorta & out to the body via the “Arteries = pump аway”. Anatomy of the heart Cone shaped organ located in the mediastinal space. The pericardial sac encases the heart and protects it, lubricates and holds 5-20 ml of pericardial fluid. This has two layers. • the parietal pericardium which is the outer membrane. • the visceral pericardium is the inner membrane attached to the heart. Consists of 3 layers • Epicardium: outermost layer of the heart. • Myocardium: middle layer of the heart, the contracting muscle. • Endocardium: innermost layer of the heart, lines the inner chambers and the valves. Function of circulation Delivers 02, nutrients, hormones and antibodies to organs, tissues and cells. Removes the end product of cellular metabolism Function of the heart Pumps oxygenated blood into the arterial system to supply capillaries and tissue. Pumps oxygen poor blood from the venous system through the lungs to be reoxygenated. Pulmonary Valve 4 valves Two atrioventricular valves that close at the beginning of ventricular contraction. They prevent blood from flowing back into the atria. • Tricuspid valve: on the right side of the heart. • Bicuspid valve: on the left side of the heart. Two semilunar valves that prevent blood from flowing back into the ventricles during relaxation. • Pulmonic semilunar valve: between the right ventricle and pulmonary artery. • Aortic semilunar valve: between the ventricle and the aorta. Coronary arteries • Right main coronary artery: supplies the right atrium and ventricle, the inferior left ventricle, posterior septal wall, 1SA and AV nodes. • Left main coronary artery: consists of two main branches left anterior descending which supplies blood to the left ventricle and the ventricular septum and circumflex arteries which supply blood to the left atrium and the lateral/posterior aspects of the left ventricle. RA LA valve valve Aortic Valve RV LV 4 chambers • Right atrium: carries deoxygenated blood from the body via superior and inferior vena cava. • Right ventricle: carries blood from the right atrium and pumps it into the lungs through the pulmonary artery. • Left atrium: carries oxygenated blood from the pulmonary veins. • Left ventricle: carries oxygenated blood from the left atrium and pumps it into the systemic circuit through the aorta. Electrical conduction: • SA node: pacemaker of the heart and initiates contraction at 60-100 BPM. • AV: receives impulses from the SA node initiates and sustains impulses at 40-60 BPM. • Bundle of His: continuation of the AV node and branches into the the bundle branches which terminate in the purkinje fibers. • Purkinje fibers: network of conducting strands beneath the ventricular endocardium. They can act as a pacemaker when the SA and AV fail as pacemakers. They can sustain at 20-40 BPM. Hypertension Med Surg: Cardiac Pathophysiology Numbers to know: Hypertension is chronic high blood pressure, which if not treated can cause damage to organs from all that high pounding pressure • Brain - CVA (stroke risk!) NCLEX TIP • Heart - MI (heart attack) & HF (heart failure) • Kidney - CKD (Renal failure) • Blood vessels - Atherosclerosis (scared arteries) • Eyes - Blindness (Retinopathy NCLEX TIP MEMORY TRICK Systolic/Diastolic ‘’San/Diego’’ Squeeze/Decompress STAGE 2: 140/90 (or more) “NORMAL BP” STAGE 1: 130-139/80-89 ELEVATED: 120-129/80 OVER (or less) 140/90 NORMAL: 120/80 (or less) Signs & Symptoms NO SYMPTOMS = Silent KILLER A –Achy head (Headache) NCLEX TIP B –Blurred vision (retinopathy) C –Chest pain (angina) SEVERE: HTN Crisis OVER 180/120 Immediate Action: • B - Beta blockers “Blocks Beats” • C - CCBs “C Calms the heart” • D - Dilators (Vasodilators) “Nitro = Pillow” • E - Emergency to ICU! OH LORDY! LOW: 90/60 (or less) Labs BNP - B-type Natriuretic Peptides • 100 & Less = Normal • 300+ Mild • 600+ Moderate • 900+ SEVERE Cholesterol Panel • Total Cholesterol = 200 • Triglycerides = 150 • LDL = Under 100 • HDL = OVER 40 NOTE: All should be low, except the HDL “Happy - keep them HIGH” Imaging • Echocardiogram measure Ejection fraction (blood pumped out of heart) 55 - 70% = normal Less than 40% = Heart Failure • ECG & EKG - Tall R peaks from the high pumps • Side note: 3 BP measurements - 1 week apart, confirms diagnosis Pharmacology Blood Pressure Lowering Drugs ABCD A –Ace inhibitors -pril Lisinopril B Education DIET LOW SCC (Sodium, Calories, Cholesterol) REDUCE ALCOHOL & CAFFEINE C EXERCISE: WALKING (30 min. x 5 days/wk) D STOP SMOKING & ALCOHOL STRESS REDUCTION D Causes SODA S –Stress, Smoking, Sedentary Lifestyle O–Obesity, Oral Contraceptives (birth control) D–Diet (High sodium & cholesterol) Diseases DM, Renal disease, HF, Hyperlipidemia (Over 200) A–African men & Age (old) A–Angioedema C–Cough E–E+ imbalances (LOW sodium, HIGH potassium) ARBS “-sartan” Losartan –Beta blockers (slows HR) “-lol” Atenalol Blocks Beats Caution: 4 B’s Bradycardia (60 or Less) Bottomed out BP (80/60) Breathing problems (COPD, Asthma) Blood sugar masking (diabetics) –Calcium channel blockers Calms heart, Controls BP Niphedipine, Cardizem, Verapamil –Diuretics D–Drains Fluid “Diurese” K+ Wasting–Furosemide & HCT (caution: Low K+, Eat fruits & green leafy) K+ Sparing–Spironolactone (avoid Salt Substitues) –Dilators (vasodilators) (Relieves Pressure) Nitroglycerin = Pillow (rest & relaxed heart) Caution: No Viagra = DEATH AC Anti-Clogging of the arteries A –Antiplatelet (Anti Clumping) C A–ASA C–Clopidogrel Caution: Bleeding –Cholesterol Lowering Lovastatin “stay clean” Caution: Liver Toxic, NO grapefruit MI, Angina, CAD Med Surg: Cardiac Pathophysiology Diagnostics 1st–EKG (Any chest pain or MI symptoms) Myocardial Infarction (MI) the heart muscles DIE “necrosis” from lack of oxygen. This occurs when there is a blockage of the coronary arteries, the “O2 tubes” feeding the heart oxygen. Signs & Symptoms O2 PAIN–Jaw, back, mid back/shoulder pain, heartburn (epigastric), Substernal Key words = priority: “Sudden” “Crushing” “radiating” NCLEX TIP SOB “dyspnea” “labored breathing” NAUSEA Vomiting “Abdominal pain” SWEATING “Diaphoresis” PALE COOL SKIN “dusky” ANXIETY NormalNormal ST elevation ST elevation ST Depression Causes SODDA S–Stress, Smoking, Stimulants (caffeine, amphetamines) O–Obesity–(BMI over 25) D–Diabetes & HTN (over 140/90) D–Diet (high cholesterol) animal fats A–African American males & Age (over 50) *Men more than women Progression CAM C–CAD “coronary artery disease” A–ACS “acute coronary syndrome” Angina - Stable “Safer”- relieved w/rest Angina - Unstable “Unsafe” - Unrelieved M–MI (heart die) Patient Education DRESS D–Diet low (sodium & fluids (2g/2L per day) Prevent HF Heart Failure=Heavy Fluid Report "New, Rapid" Weight Gain-Water Gain! R–Reduce Stress, Alcohol, Caffeine, Cholesterol (animal fats) E–Exercise (30 min x 5 days/wk) S–Smoking Cessation S–Sex (2 flights of stairs with NO SOB) NCLEX TIP *AVOID NSAIDS (naproxen, ibuprofens) = increases CLOT risk! Treatment: Pharmacology AC–Anti Clogging of Arteries A–Antiplatelet HOLD if: Platelets 50K or LESS “below 50 gets risky” (not INR, not aPTT) A–ASA C–Clopidogrel C–Cholesterol Lowering “-Statin” Lovastatin “stay clean” CAUTION: NO grapefruit Liver Toxic–report “clay colored stools” Muscle pain (Rhabdomyolysis risk) Late night–take at dinner 2nd–LABS T–Troponin (Over 0.5 ng/mL) T–Trauma (ONLY indicator of MI) Other labs: Crp, Ckmb, Myoglobin, CRP (inflammation) Treatment: Pharmacology DURING–Any Chest Pain O–Oxygen A–Asa N–Nitro–under tongue x 3 Max M–Morphine - Any pain after = MI (injury) AFTER–MI Clot Stabilization: Heparin: prevents CLOT growth (NOT dissolve only t-PA) PTT: 46 - 70 “3 x MAX” Antidote: Protamine Sulfate Memory Trick: “HaPTT” frog Heart Rest: B–Beta Blockers (-lol) Atenolol Blocks both BP & HR (Lol = Low BP & HR) CAUTION: B–Bad for Heart Failure patients (CHF) B–Bradycardia (60 or Less) & BP low (HR LESS than 60) B–Breathing Problems “wheezing” (Asthma, COPD) B–Blood sugar masking “hides s/s” (Diabetics) C–Calcium Channel Blockers Calms BP & HR-(AVOID Low Hr & BP) (Nifedipine, Diltiazem, Verapamil) -dipine “declined BP & HR” -zem “zen yoga for heart” -amil “chill heart” D–Dilators (vasOdilators = O2 to heart) Nitroprusside (only for HTN crisis) & Isosorbide Nitro “Pillow for heart” NO viagra “-afil” Sildenafil = DEATH! Nitro drip: STOP if Systolic BP below 90 or 30 mmHg Drop SE: HA is Common + SLOW Positions changes “syncope” t DISCHARGE–GOING HOME CHOLESTEROL PANEL C-CLOGGED ARTERIES (risk) 200 or Less-Total Cholesterol 150 or Less-Triglycerides 100 or Less-LDL 40 or More = HDL Heart Rest: 1st choice A–Ace (-pril) Lisonopril “chill pril” 2nd choice A–ARBs (-sartan) Losartan “relax man” Antihypertensive (BP ONLY) *HOLD: Low BP (not HR) Precautions: A–Avoid Pregnancy A–Angioedema “thick tongue” (Airway Risk) *only Ace NCLEX TIP C–Cough *only Ace Creatinine (Kidney) (normal: 0.9 -1.2) *only Ace E–Elevated K+ (normal 3.5-5.0) NCLEX TIP AVOID Salt Substitues + Green Leafy veggies • 1st–Cardiac Monitor • High Potassium = High Pump • Monitor: muscle cramps, spasms, peaked T waves, ST changes MI, Angina, CAD II Med Surg: Cardiac Cath Lab C–Contrast = Kills Kidneys “Angioplasty, Angiogram, CABG” A–Allergy to Iodine (warm flushing normal) B–Bleeding–direct manual pressure (above site) NO=heparin, warfarin, ASA, clopidogrel C–Creatinine “Kidney” (normal: 0.9 - 1.2) REPORT: Creatinine Over 1.3 & Urine below 30 ml/hr STOP Metformin 48 hrs (before/after) C–Can’t feel pulses (Pulses = Perfusion O2) Diminished pulses (4-12 hrs post-procedure) MAX PRIOITY: Non palpable pedal pulse AFTER = CALL HCP (Dr.) Key words: “cool leg, pulse non palpable, present only with doppler US. Complications After MI ACUTE: (weeks after) Cardiogenic Shock (severe hypotension) V fib/V tach (no pulse) = DEADLY Defibrillate=Don’t have a pulse Cardioversion=Count a pulse *synchronize* CHRONIC: (lifetime) Heart failure “Heavy Fluid” Rapid weight gain (Water Gain), Worsening crackles (fluid in lungs “pulmonary, edema”) Sudden edema (JVD, peripheral edema “+1 pitting”) #1 Priority–IV Diuretics–Furosemide, Bumetanide “dried” (NOT isosorbide) NitrOglycerin O2 to Heart NO viagra “-afil” Sildenafil = DEATH! NORMAL ADVERSE EFFECT: HA=Normal Side Effect Hypotension=Adverse effect (need slow position changes) PILL (or spray) Nitro Patch (Transdermal nitro patch) S–Stable Angina S–Safe Angina S–Stops when activity STOPS (Stress Induced) *Take Before strenuous activity GOAL: NO chest pain=Daily activities “comb hair, fix hair, get dressed, make up, making bed etc.” TAKING MED: CALL 911: PAIN 5 min. After 1st dose. 3 doses max x 5 min apart NO SWALLOW–SL under STORAGE: NO LIGHT–NO HEAT NOT: pill box, car, plastic bag, pocket YES: purse ok *Replace every 6 months U–Unstable Angina U–Unsafe Angina U–Unrelieved with rest /Unpredictable (anytime) 1 x daily NOT PRN 1 patch at a time NOT 2 patches YES Shower is ok LOCATION: Rotate locations Daily “Clean, Dry, shaven area” teach patient to wash hands after application Upper Body (subclavian, arm, upper chest) NOT: hairy, scarred, burned, callous NOT BROKEN SKIN *TEST TIP: Patch fall off? (Over 1 hour ago) Take nitro (pill/spray) New patch can take 40–60 min. *Nurses wear gloves! Will cause MAJOR HA if it comes into contact with skin! 0.4 mg MI, Angina, CAD III Med Surg: Cardiac Anticoagulants (clot prevention) Bleed Risk (Patient Education) Antiplatelets (LESS potent) ASA & Clopidogrel Platelets LESS than 50k = RISKY (Normal: 150–400k) NOT INR or PTT Anticoagulants (MOST potent) Warfarin = INR “warINR” Range: 2.5–3.5 (3 x MAX range) Antidote: Vitamin K (green leafy veggies) *NOT K+ = potassium* Heparin (Enoxaparin) = aPTT “HaPTT” frog Partial Thromboplastin Range: 46–70 (3 x MAX range) Antidote: Protamine Sulfate NO peptic ulcers (or active bleeds) NO Rugs/dim halls (well-lit halls) NO razors, hard brushing, constipation NO NSAIDS like naproxen/ ibuprofen NO EGGO vitamins E–E Echinacea, Vitamin A G–Gingko, Garlic, Ginseng O–Omega 3 MYOCARDIAL INFARCTION Treatment (+) Positive Troponin = Heart Attack (MI) PRIORITY: REMOVE THE CLOT! CLOT BUSTER “Thrombolytics, Fibrinolytics” “CATH LAB” OR SURGERY “PCI” -graphy, -plasty BEFORE NPO 6 - 12 hrs AFTER NO heavy lifting–lie flat NO Baths–Shower ok (dont soak) Infected Incision “red, warm, drainage” t-PA: Alteplase, Streptokinase (Allergy risk) Dissolves Clot ONLY (heparin does NOT) BLEED RISK 8 hour duration NO injections (IV, SQ, IM, ABG) NOT via central lines (CVC) ONLY “compressible site” (IV, PICC) NOT FOR: Active Bleeds: Peptic Ulcers (but menstruation is safe) History: Arteriovenous malformations Intracranial “Cerebral” hemmorhage Hypoglycemia (relative contraindication) Hypertension (over 180/110) TEST TIP STRESS TEST Non MI (non priority) • Spot the Narrowing TREADMILL STRESS TEST STOP test: chest pain ST elevation NormalNormal CHEMICAL: NUCLEAR PHARMACOLOGICAL STRESS TEST 24–48 hours BEFORE NO Cigarettes, Caffeine (tea, soda, coffee) *NO DECAF NO Meds: Nitro, Beta Blocker, Theophylline (stimulant) NPO (nothing oral) 4 hrs before/after ST elevation ST elevation Heart Failure Med Surg: Cardiac Patho The heart fails to maintain adequate cardiac output (oxygenated blood pumped OUT to the body) due to impaired pumping ability. MEMORY TRICKS • HF - Heart Failure (failure to pump blood forward) • HF - Heavy Fluid (backs up in lungs / body) Weight Gain = Water Gain Signs & Symptoms R - RIGHT Sided HF R - ROCKS BODY with fluid • Peripheral Edema • Weight Gain = Water Gain • JVD (big neck veins) • Abdominal Growth - Ascites (fluid in abdomen) - Hepatomegaly (big liver) - Splenomegaly (big spleen) L - LEFT sided HF L - LUNG fluid • Pulmonary Edema • Crackles in lungs “Rales that don't clear with a cough” • Pink Frothy “blood tinged” sputum • Orthopnea - difficulty breathing when lying flat Causes R - RIGHT-Sided HF L-LEFT sided HF • HTN (high BP) • Pulmonary HTN • Stiff “fibrotic” lungs • Left-sided HF can cause Right HF Weak heart = weak pump • After a heart attack (MI myocardial infarction) • Ischemic heart disease low oxygen to heart muscles (CAD, ACS) 3 Common EXAM Questions: Patient with heart failure who is constipated! What would the nurse recommend? Which food item should the heart failure patient avoid? Select all that apply. 1. Walking 1. Chips - NO SODIUM! 2. Increase fiber 2. Fruits 3. Stool Softeners 3. Veggies 4. Drink extra water - NO! 4. Grilled chicken & fries - NO! 5. Canned beans - NO! 6. Bread A client with chronic heart failure took cold medicine for her flu. She presents with new productive cough with pink frothy sputum and worsening crackles. What action should the nurse take first? 1. Assess lung sounds 2. Give bumetanide IV Push - YES 3. Notify the HCP 4. Clock out for lunch Look for KEY WORDS “New, sudden, worsening, rapid symptoms” # 1 Action is Furosemide = “Body Dried” Risk Factors 1. Hypertension (high BP) is the #1 risk factor 2. Atrial fibrillation & other dysrhythmias 3. Mitral valve regurgitation 4. Cardiomyopathy Diagnostic tests • Labs: BNP (brain type natriuretic peptides) Memory trick: B - Broken ventricles Over 900+ = SEVERE HEART FAILURE • Echocardiogram measures Ejection Fraction (blood pumped out of heart) 55 - 70% = normal 40% or LESS = BAD (heart failure) • Hemodynamic Monitoring “Swanz Ganz” (Pulmonary Artery catheter) Over 8 = is NOT GREAT! (normal: 2 - 8 mmHg) Priority Interventions For Pulmonary Edema Crisis (lung fluid) KEY WORDS “New, sudden, worsening, rapid symptoms” # 1 Action is Furosemide = “Body Dried” • H - HOB 45 degree or higher (Semi-fowler’s, High fowler’s, orthopneic position) • O - Oxygen • P - Push Furosemide + Morphine, Positive inotropes • E - End sodium & fluids (Sodium Swells the body) NO drinking fluids + STOP IV fluids Heart Failure II Pharmacology & Care Pharmacology Lisinopril • Losartan A – ACTS on BP only (not HR) A – ACE (-pril) Lisinopril “chill pril” 1st choice A – ARBS (-sartan) Losartan “relax man” 2nd choice Atenolol A–Avoid Pregnancy A–Angioedema (Airway Risk) *only Ace C–Cough *only Ace E–Elevated K+ (normal 3.5-5.0) Nifedipine, Cardizem, Verapamil B – BETA BLOCKERS (-lol) AtenoLOL “LOL = LOW” Cardiac Glycoside Nitroglycerin Potassium Wasting & Sparing Milrinone *inotropic drug-LAST LINE therapy-palliative care Blocks both BP & HR (AVOID Low HR & BP) Caution: HOLD IF: B–Bradycardia (LESS than 60) & BP low (90/60) only hold if the patient is in an acute exacerbation of CHF B–Breathing problems “wheezing” (Asthma, COPD) B–Bad for Heart Failure patients B–Blood sugar masking “hides S/S” (Diabetics) C – CALCIUM CHANNEL BLOCKERS Nursing Care & Interventions DRBEDSS LOW Sodium & Fluid (2L + 2g or LESS/day) (Change positions slowly!) (Should NOT be increasing) (with pillows) High Fowlers (3lbs/day or 5 lbs/7 days = Worsening!) (2 flights of stairs with NO SOB) ‘’TED hose’’ (decreases blood pooling, Remove daily) Calms BP & HR (AVOID Low HR & BP) (Nifedipine) -dipine “declined BP & HR -amlodipine “chill heart” D – DIURETICS Drain Fluid D–Drains Fluid “Diurese” “Dried” K+ Wasting–Furosemide & Hydrochlorothiazide (caution: Low K+, Eat melons, banana & green leafy veg) K+ Sparing–Spironolactone “Spares potassium” (AVOID Salt Substitues, melons & green leafy veg) D – DILATORS (Vasodilators) Nitroglycerin, Isosorbide Nitroglycerin “Nitro = Pillow for heart” Caution: NO Viagra “-afil” Sildenafil = DEATH! Nitro drip: STOP = Systolic BP below 90 or 30 mmHg Drop Adverse effect: HA= side effect Low BP= adverse effect (SLOW position changes) D – DIGOXIN (Inotropic) NO OTC meds (Cough or Flu, Antacids or NSAIDS) NCLEX TIP NO Canned or packaged foods (chips, sauces, meats, cheeses, wine) NEVER massage calves (CHF patients) NCLEX TIP Digs for a DEEP contraction Increased contractility Apical Pulse x 1 minute Toxicity (over 2.0) Vision changes, N/V TEST TIP Potassium 3.5 or less (higher r/t toxicity) Peripheral Vascular Med Surg: Cardiac NARROW PVD | VEIN NARROW PAD | ARTERY Signs & Symptoms Signs & Symptoms VEINY ARTS V VOLUMPTUOUS PULSES - Warm legs E EDEMA (blood pooling) I IRREGULAR SHAPE SORES (Exotic pools) N NO SHARP PAIN (Dull pain) Y YELLOW & BROWN ANKLES A ABSENT PULSES, Absent Hair (Shiny) = Cool legs R ROUND, RED SORES (blood pooling) T TOES & FEET PALE or BLACK “Eschar” S SHARP CALF PAIN (intermittent Claudication) E - Exercise • E-Elevation (recliner chair) Patient Education Positioning PVD VEINS = ELEVATE (Vacuum) Positioning PVD & PAD C–Constriction AVOID C–Cross legs C–Constrictive clothing C–Cigarettes C–Caffeine C–Cold Temperatures T–Toenails trimmed ONLY by Dr. NCLEX TIP PAD ARTERIES = HANG (Away) DVT, RAYNAUD’S & BUERGER’S DVT - Deep Vein Thrombosis Treatments Pathophysiology CLOT in a deep vein DURING CLOT-DV D Don’t Walk (bed rest) V Venous return (eleVate) Signs & Symptoms CHANT COWS C CALF PAIN & CRAMPING O ONE-SIDED SWELLING (Unilateral) W WARM & RED (Blood pooling) S SOB & CHEST PAIN = PE! (Call Doctor) AFTER CLOT C Calf Exercise & Isometrics H Hydration NCLEX TIP A Ambulation N NO long sitting (Car, Airplane, Bedrest) T Ted & SCDs (AFTER CLOT resolved) Raynaud’s & Buerger’s Disease Signs & Symptoms R–RAYNAUD’S • R–RING FINGER B–BUERGER’S • B–BLACK FINGERS & TOES Valve disorder Med Surg: Cardiac Pathophysiology Mitral valve Aortic valve Mechanical valves The heart is like a 4 bedroom suite. The valves are like doors & the chambers are like rooms. If valves have trouble closing it can result in black flow of blood & insufficient blood flow to the body. Stenosis: stiff, narrowed, hard valves Regurgitation: Return of blood or backflow of blood as the valve does not completely close. Main Types • Aortic Stenosis • Aortic Regurgitation • Mitral Stenosis • Mitral Regurgitation Causes Pharmacology Anything that can damage the heart! • Congenital heart disease (pre-term babies) • Cardiomyopathy - a disease of the heart muscle • Heart Attack - damaged heart muscles • Infection: • Rheumatic fever - ruins the heart • Endocarditis - infection in the heart • Anticoagulants: Heparin & Warfarin • Antiplatelet: Aspirin & Clopidogrel • Nitroglycerin for chest pain Signs & Symptoms Think LOW oxygen from LOW heart pumps. Regurgitation • Aortic Tachycardia, dyspnea, fatigue • Mitral Edema, pleural effusion, enlarged organs & ascites Stenosis • Aortic Angina, sys. murmur, syncope, fatigue, orthopnea • Mitral Cyanosis, activity intolerance, diastolic murmur, s/s of right ventricular failure, clear lung sounds Surgeries • Valve replacement - Warfarin therapy life long • Balloon valvuloplasty - Stenosis Patient Education • AVOID dental procedures for 6 months after surgery & take antibiotics before dental exams. • Warfarin (anticoagulant) • Life long drug with “routine blood tests” • 2.5 - 3.5 INR (for valve replacements) • Even intake of Green leafy veggies (vitamin K) NOT increased & NOT decreased intake - nice & even • Bleeding precautions • NO brushing teeth too hard • NO shaving - only electric shaver • NO throw rugs & always well lit halls Endocarditis / Pericarditis Med Surg: Cardiac ENDOCARDITIS Causes • Dirty Needles • Dental visits • Heart Surgery: Valve replacements & CABG • Untreated Strep Throat Pathophysiology Inflammation INside the heart • Infective = bacteria (mold on heart valves) • Noninfective = No bacteria (only inflammation) Heart valves can’t close fully Less cardiac output = Less oxygen OUT Treatment Signs & Symptoms • • Antibiotics • Valve repair or Replacement C - Clots in the heart & brain • Risk for stroke CVA - monitor for “agitation” “change in level of consciousness” NCLEX TIP • Splinter hemorrhages (clots under fingernails) L - Lung fluid (crackles) • O - Overheated (fever) • T - Too little Oxygen (low cardiac output) • • Clubbing fingers *Roth spots, Osler’s nodes, Janeway lesions (body’s immune response) PERICARDITIS Acute MI AUTOIMMUNE DISORDERS INFECTION RENAL FAILURE Uremia (High BUN) ORAL CARE brush 2x day NO FLOSSING LET ALL PROVIDERS KNOW DENTAL VISITS OR SURGERY ADHERENCE • Precordial chest pain • Elevated WBC (over 10,000) • C-reactive protein • Cardiac Tamponade 1. JVD 2. Muffled heart sounds 3. Pulsus paradoxus (drop in sys. BP by 10 mmHg) Inflammation OUTside the heart (heart gets compressed & can’t pump) Less cardiac OUTput = Less oxygen OUT HEART ATTACK MONITOR Signs & Symptoms + Labs Pathophysiology Causes Education Treatment • NSAIDS (indomethacin) • Steroids (prednisone) • Pericardiocentesis (needle in the heart) used to drain any fluid or blood in the heart sac. Cardiomyopathy Med Surg: Cardiac Pathophysiology • Dilated Cardiomyopathy: Think “Distended heart muscles”, clients present with fibrosis (stiff hard muscles) of the myocardium and endocardium, dilated chambers, making it hard for the heart to pump out oxygen rich blood. DILATED RESTRICTIVE HYPERTROPHIC Distended heart muscle “Rock hard’’ heart muscle Huge trophy-like heart muscle • Restrictive Cardiomyopathy: Think “Rockhard heart muscles”, so the heart cannot RE-fill with REstrictive cardiomyopathy, emboli (blood clots) are common. • Hypertrophic Cardiomyopathy: Think “Huge Trophy like heart muscles” in the middle septum which can obstruct the aorta block ing all oxygenated blood out to the body - very deadly! Obstructive = blocks the aortic valve Non-obstructive = does not block Pharmacology Labs & Diagnostics • Chest X-ray & MRI • Echocardiogram measures Ejection Fraction (blood pumped out of heart) 55 - 70% = normal 40% or LESS = BAD (heart failure) • Angiography Highlights the coronary arteries to see blockages & rule out ischemic heart disease (low oxygen to heart muscles) • BNP “B-type or Brain Natriuretic Peptides” Breaking & Stretching of ventricles All problems lead to LESS cardiac output meaning LESS oxygen rich blood OUT to the body. Causes NCLEX TIP • Hypertrophic = genetics ONLY NCLEX TIP • Dilated & Restrictive • Genetics • Damage to the heart = radiation Signs & Symptoms • Low oxygen • Restlessness, agitation, altered level of consciousness NCLEX TIP • syncope, dizzy + fatigue • Heart failure signs • Left-sided = lung fluid • Right-sided = rocks the body with fluid (edema, ascites, JVD) Dilated cardiomyopathy • S3 murmur • Cardiomegaly (dilated heart) Restrictive Cardiomyopathy • (same general low oxygen & HF) Hypertrophic Cardiomyopathy • Typically asymptomatic (no s/s) until heavy exercise & then the child DIES! NCLEX TIP BNP ELEVATED 100 OR LESS - NORMAL HOLD MED IF: 1. Apical Pulse 60 2. Potassium (K+) 3.5 (Risk for Dig Toxicity) 3. Digoxin Toxicity OVER 2.0 101-299+ MILD ELEVATION 300+ MILD HF 600+ MODERATE HF 900+ SEVERE HF Vision Changes, N/V, Fatigue ‘’dizzy’’ Education Side note: Hypertrophic Cardiomyopathy • B - Beta blockers • C - Calcium channel blockers NO DDD • D - Dilators • D - Digoxin • D - Diuretics NO strenuous activity! This can block the aorta. Cardiac Tamponade Med Surg: Cardiac Pathophysiology COMPRESSION OF THE HEART caused by fluid collecting in the pericardial sac. (weaker pump = less cardiac output) This is a medical emergency as fluid or blood fills the pericardial sac, compressing the heart so that it cannot fill & pump! The result is a dramatic drop in blood pressure that can kill the client. MEMORY TRICK • C - Cardiac Tamponade • C - Compression on the heart • C - Critical client! Causes ACUTE TRAUMA: (Stabbing or MVA) CHRONIC: Pericarditis Treatments PERICARDIOCENTESIS 1. CARDIAC MONITOR 2. CATHETER ATTACHED to drainage system 3. ASSESS DRAINAGE (Type & speed of drainage) Signs & Symptoms BECKS TRIAD BEC B • Big Jugular Veins Distension (JVD) E • Extreme Low BP (Hypotension) C • Can’t hear heart sounds (muffled) PULSE PARADOXES Systolic drop of 10 mmHg (120/80 to 110/80) ECG QRS complexes (short & uneven height) Heart Sounds & 5 EKG Lead Placement Heart Sounds Memory Trick APETM “All Pigs Eat Too Much” PULMONIC (2nd Intercostal Space L Sternal Border) AORTIC (2 Intercostal Space R Sternal Border) A - Aortic P - Pulomonic E - Erb’s point T - Tricuspid M - Mitral nd TRICUSPID (3nd or 4th Intercostal Space L Sternal Border) ERB’S POINT (3rd Intercostal Space L Sternal Border) MITRAL (5th Intercostal Space Midclavicular Line) 5 EKG Lead Placement QRS Complex R Memory Trick P PR Segment PR Interval Q ST Segment White on Right Smoke over Fire Brown in the Middle Grass under sky (white) T S QT Interval Proper 12-Lead Placement for Left Side of Chest v1 4th intercostal space to the right of the sternum v2 4th intercostal space to the left of the sternum v3 directly between the leads V2 & V4 v4 5th intercostal space at midclavicular line v5 level with V4 at left anterior axillary line v6 level with V5 at left midaxilary line (directly under the midpoint of the armpit) v4R 5th intercostal space, right midclavicular line v1 v4R v2 v 3 v4 v5 v6 5 Step EKG INTERPRETATION Heart rate Rhythm P wave PR interval (in seconds) QRS (in seconds) 60 -100/min Regular Present before each QRS, identical P/QRS ratio 1:1 0.10 - 0.20 (<5 small squares) Normal shape < 0.12 8 x 10 = 80 Heart Rate 1. Normal Sinus Rhythm Rate - 60 -100 count the peaks - we have 8 here multiply by 10 = 80 beats! 1 2 3 4 5 6 7 8 Rhythm 2. Rhythm - R peaks are evenly spaced apart. To quickly measure this simply grab some paper & mark 2 R peaks then just march it out. The R peaks should be even every time. R R R-R int. R R R R P Wave R 3. P wave - which is our atria contracting is it present? & does it have its buddy QRS? we need a P with QRS every time P T Q PR interval (in seconds) P R P PR int. R-R int. 5 mm 0.2 sec PR ST seg. seg. P PR int. T Q S QRS int. ST int. QT int. 0.5 mV 5 mm 0.2 sec QRS (in seconds) 5. QRS - Ventricles contracting Is it present, upright & TIGHT? Should NOT be wide, should only be 3 boxes - .12 seconds here. T Q S 0.5 mV 4. PR interval - basically measures the time it takes between atrial contractions & ventricular contractions should be 5 mini boxes or less - or .10 - 2.0 seconds here. R S R 9 ECG Strips on the NCLEX 1. Normal sinus rhythm Treatment: None - continue to monitor Causes: Being healthy Memory tricks Normal beat - evenly spaced 2. Bradycardia BRADY Bunch old TV show (slow times) <60 Treatment: Atropine ONLY if symptomatic showing low perfusion (pale, cool, clammy) Causes: ATROPINE Vagal maneuver (bearing down), Memory tricks meds (CCB, Beta Blockers) BRADYcardia Below 60/min 3. Ventricular Fibrillation (V Fib) Treatment: 1. V Fib - Defib #1 Defibrillation immediately Stop CPR to do it & before drugs! *NO synchronization needed 2. Drugs: LAP - Lidocaine, Memory tricks Fib is flopping- squiggly line 4. Ventricular Tachycardia (V Tach) Amiodarone, Procainamide Causes: Untreated V Tach, Post MI, Causes: Post MI, Hypoxia, Treatment: 1. Early Defibrillation! NCLEX TIP V Tach Tombstone pattern A LIDOCAINE P PROCAINAMIDE AMIODARONE E+ imbalance, proarrhythmic meds Low potassium, Low magnesium Memory tricks L Apply defibrillator pads Call out & look for everyone to be CLEAR! Shock & IMMEDIATELY continue chest compressions 2. When to Shock? NCLEX TIP V Tach with No pulse = Defibrillation V Tach with Pulse = Cardioversion Memory tricks C C - Count a pulse C - Cardiovert *Synchronize First & Sedation D D - Dead - NO PULSE D - DEFIB!! *NO Synchronize D - Don't wait 9 ECG Strips on the NCLEX II 5. Atrial Fibrillation (A Fib) Digoxin Causes: Valvular disease, Heart failure, Pulm. HTN, A COPD, after heart surg. Treatment: 1. Cardioversion (after TTE to rule out clots) *Push Synch 2. Digoxin - Deep Contraction Check ATP Before giving: A - Apical pulse 60 T - Toxicity (Max 2.0 range) visual disturbances, T Max 2.0 60 40 kg P N/V, Anorexia Memory tricks No P wave = Fibrillation FloPPing 6. Atrial Flutter (A Flutter) P - Potassium below 3.5 - HIGHER risk for toxicity < 3.5 3. Anticoagulants: Warfarin (monitor INR, Vit. K antidote, moderate green leafy veggies) Potassium K+ Causes: Valvular disease, Heart failure, Pulm. HTN, COPD, after heart surg. Treatment: 1. Cardioversion (after TTE to rule out clots) *Push Synch 2. Digoxin - Deep Contraction Check ATP Before giving: A - Apical pulse 60 T - Toxicity (Max 2.0 range) visual disturbances, N/V, Anorexia Memory tricks A FluTTer = sawTooTh P - Potassium below 3.5 - HIGHER risk for toxicity 3. Anticoagulants: Warfarin (monitor INR, Vit. Max 2.0 40 kg < 3.5 K Potasssium K+ KAPLAN Causes: Stimulants, Strenuous exercise, hypoxia, heart disease Super Fast = Supraventricular 60 K antidote, moderate green leafy veggies) 7. SVT - Supraventricular Tachycardia Memory tricks DIGOXIN Treatment: 1. Vagal Maneuver (bear down like having a bowel movement, ice cold stimulation) 2. Adenosine - RAPID PUSH & flush with NS - HR may stop Which medication should be held 48-hours prior to an elective cardioversion for SVT? Digoxin due to increased ventricular irritability Client with SVT has the following assessment data: HR 200, BP 78/40, RR 30 Priority action: Synchronized cardioversion PRIORITY 3. Cardioversion - *Push Synch 8. Torsades de Pointes Memory tricks M Magnesium Causes: Post MI, Hypoxia, Low magnesium Treatment: Magnesium Sulfate NCLEX TIP Memory tricks Tornado Pointes Magnesium Mg+ M Mellows out the heart 9 ECG Strips on the NCLEX III 9. Asystole - Flatline Epinephrine, Atropine & CPR *NO Defibrillation (NO shock) NCLEX TIP Memory tricks Assist Fully! … patient is flatlined R R PP Q P Q S NCLEX Key Terms R PP Q S S 1. P wave = Atrial rhythm Asystole 4. “Bizarre” - Tachycardia “Lack of QRS complexes” Answer: Asystole Q S 3. V Tach Ventricular Tachycardia “Bizarre rhythm with wide QRS complex” Answer: Ventricular Tachycardia Question: R 3. Question: 2. QRS wave - Ventricular rhythm 5. “Sawtooth” - Atrial Flutter “Wide bizarre QRS complexes” Answer: V Tach 3. “Chaotic or unorganized” - Fibrillation Question: A FluTTer = sawTooTh “Chaotic rhythm with no P waves” Answer: Atrial Fibrillation Atrial Flutter “CHAOTIC rhythm without QRS complexes” Answer: Ventricular Fibrillation Atrial Fibrillation If you know these, you will pass the NCLEX! NCLEX TIP Normal sinus rhythm Bradycardia Ventricular Fibrillation (V Fib) Ventricular Tachycardia (V Tach) Atrial Fibrillation (A Fib) Atrial Flutter (A Flutter) Torsades de Pointes Asystole - flatline 3. SVT - Supraventricular Tachycardia EKG Quick view 9 strips to know for the Nclex Normal sinus rhythm Bradycardia Ventricular Fibrillation (V Fib) Ventricular Tachycardia (V Tach) Atrial Fibrillation (A Fib) Atrial Flutter (A Flutter) SVT - Supraventricular Tachycardia Torsades de Pointes Asystole - flatline