Surra & Babesiosis in Ruminants: Diseases, Treatment, Prevention
advertisement

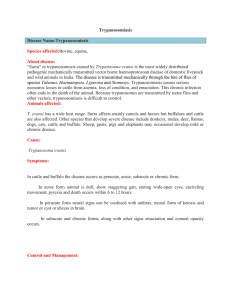
MODULE 4: COMMON RICKETTSIAL AND PROTOZOAN DISEASES IN RUMINANTS Surra • Etiology: Trypanosoma evansi • Epidemiology: o Transmitted by biting flies such as Tabanus, Stomoxys o Transmission is probably resulting from interrupted feedings o A few wild animals are susceptible to infection and may serve as reservoirs Epidemiology • Hosts • • • • • • • Pathogenic in most domesticated animals and some wild animals Domesticated animals: Horses, mules, donkeys, cattle, buffalo, camels (dromedary and Bactrian), llamas, pigs, sheep, goats, dogs and cats Most important single cause of morbidity and mortality in camels Wild animals: deer, capybara (reservoir host) and other species New world camelids in South America are experimentally susceptible but natural disease has not been reported despite presence in cattle and horses Reservoir hosts to camels and horses: cattle, buffalo, capybara, and vampire bat Rats and mice are highly susceptible as experimental hosts for detecting subclinical (nonpatent) infections Surra • Transmission • Direct life cycle with no intermediate host • Agent is transmitted from animal to animal mechanically by hematophagous flies, including Tabanus spp. and Musca spp. • Also Lyperosia, Stomoxys and Atylotus genera. • Tabanids (horse flies) are the most significant vectors • Vampire bats in South and Central America are hosts, reservoirs and vectors of T. evansi; they transmit T. evansi mechanically in their saliva, and may develop high parasitaemia which may kill the bat. • Recovered bats serve as carriers • Carnivores may become infected after ingesting infected meat • Transmission in milk and during coitus has been documented Surra • Sources of infection • Blood from infected animals • occasionally meat and milk • T. evansi frequently localises extravascularly in tissues including the central nervous system Surra • Occurrence • T. evansi has a wide distribution in Asia, North Africa (extending into tsetse areas with T. brucei infections) and Central and South America. • The main host species varies with the geographical region. • Horses are most often affected in South America; horses, mules, buffalo, and deer in China (People’s Rep. of); horses, cattle, and buffalo in SouthEast Asia; and camels in the Middle East and Africa. Surra: Diagnosis • Clinical diagnosis • Morbidity and Mortality: Camels living in northeastern Africa may have infection rates of 20–70%. • Case fatality rate in untreated horses and camels is nearly 100%. • Surra in cattle and buffalo tends to be chronic with a much lower CFR. • Animals subjected to stress, like malnutrition, pregnancy, and physical labour, are more susceptible to disease. • often rapidly fatal in camels and horses, but may also be fatal in buffalo, cattle, llama and dogs, however these host species may develop mild or subclinical infections. • Nervous signs are common in horses. • Dogs may also have nervous signs that resemble rabies. • Infections in deer are usually chronic with oedema, anaemia, emaciation and nervous signs. • Clinical signs are suggestive but diagnosis must be confirmed by a laboratory. Surra • Pathogenesis o Metacyclic trypanosomes inoculated into the skin of animals during a blood meal by vectors o Trypanosomes grow for a few days and cause localized swellings o Trypanosomes enter lymph nodes -→ bloodstream (divide) o Immune response of animals result in production of immune complexes that cause inflammation, which contributes to the signs and lesions of the disease o Antibodies against the surface-coat glycoproteins kill the trypanosomes, however, trypanosomes have multiple genes that code for different surfacecoat glycoproteins that are not vulnerable to the immune response (this phenomenon is called antigenic variation). This results in persistence of the organism. Surra: Clinical Diagnosis • Fever, directly associated with parasitaemia – recurrent episodes occur during the course of disease • Progressive anaemia, weight loss and icterus • Progressive weakness and lethargy • Oedematous swellings of the lower parts of the body: legs, briskets and abdomen (gravity dependent) • Urticarial plaques in the skin • Petechial haemorrhages of the serous membranes (eyelids, nostrils and anus) • Abortions reported in buffaloes and camels • Immunodeficiency • Death may occur in 2 weeks to 4 months, chronic infections may last up to 2 years Weight loss and testicular oedema; Source: hindawi.com • T. evansi in a blood smear Source: visavet.es Surra • Serological tests • Indirect immunofluorescent antibody test: useful when screening s small number of samples • Antibody detection ELISA: very useful for large-scale surveys o ELISA using variable surface glycoproteins from a T. evansi RoTat 1.2 clone successfully differentiated T. evansi from T. brucei. • Card agglutination test: also makes use of T. evansi RoTat 1.2 clone • Latex agglutination test: currently under evaluation Surra • Lesions • • • • • • Post-mortem lesions are nonspecific and may include: emaciation of the carcass anaemia petechial haemorrhages on some internal organs hydrothorax and ascites enlarged lymph nodes and spleen • Differential diagnosis • Horses: African horse sickness, equine viral arteritis, equine infectious anaemia, chronic parasitism, dourine • Camels: tsetse-transmitted trypanosomosis, anthrax, chronic parasitism • Cattle: babesiosis, anaplasmosis, theileriosis (East Coast Fever), haemorrhagic septicaemia, anthrax, chronic parasitism, malnutrition • Dogs: rabies if neurological signs Treatment • Suramin – 10 mg/kg bw IV, repeated 1 week later • Quinapyramine sulfate – 3 mg/kg – dose divided between 2 or more sites • Isometamidium chloride – 0.25 to 2 mg/kg IM • Melarsen oxide Prevention • Prevention relies on the ff: • identification and treatment of infected horses • Appropriate vector control • Hygiene • Repeated treatment with suramin, quinapyramine, and isometamidium chloride has been suggested Babesiosis • a tick-borne, malaria-like illness caused by species of the intraerythrocytic protozoan Babesia • Transmitted by ticks • Worldwide distribution Source: en.wikipedia.org Babesiosis: Transmission & Epidemiology • Main vectors: one-host Boophilus spp ticks, in which transmission occurs transovarially • In ticks, the blood stages of the parasite are ingested during engorgement and undergo life cycles in the replete female, eggs, and subsequent parasitic stages • Transmission to the host occurs when larvae (in the case of B. bovis) or nymphs and adults (in the case of B. bigemina) feed Source: semanticscholar.org Source: link.springer.com Babesiosis: Transmission & Epidemiology • In endemic areas, two features are important in determining the risk of clinical disease: 1) calves have a degree of immunity that persists for approx 6 mos, and 2) animals that recover from Babesia infections are immune for life. Thus at high levels of tick transmission, all newborn calves will become infected with Babesia by 6 mo of age, show few if any clinical signs, and subsequently be immune. Babesiosis: Transmission & Epidemiology • Situations that could upset endemic stability: o Either natural (e.g. climatic) or artificial (e.g. acaricide treatment) reduction in tick numbers to levels in which tick transmission of Babesia in calves is insufficient to ensure all are infected during this critical early period o Introduction of susceptible cattle to endemic areas o Incursion of Babesia-infected ticks into previously tick-free areas Babesiosis: Symptoms • BB is predominantly observed in adult cattle • Infected animals develop a life-long immunity against re-infection with the same species and some cross-protection is evident in B. bigemina-immune animals against subsequent B. bovis infections. • B. bovis Conditions are often more severe than other strains. • High fever • Parasitaemia (percentage of infected erythrocytes) - maximum parasitaemia is often less than one per cent. • Neurologic signs such as incoordination, teeth grinding and mania. Some cattle may be found on the ground with the involuntary movements of the legs. When the nervous symptoms of cerebral babesiosis develop, the outcome is almost always fatal. • Dark coloured urine • Anorexia • B. bigeminaFever • Anorexia • Animals likely to separate from herd, be weak, depressed and reluctant to move • Haemoglobinuria and anaemia • Dark coloured urine • Central nervous system (CNS) signs are uncommon • Lesions • In B. bigemina parasitaemia often exceeds 10 per cent and may be as high as 30 per cent. Source: obhiro.ac.jp Post-mortem findings of bovine babesiosis caused by Babesia bigemina. Enlarged urinary bladder containing dark-colored urine (A), kidney degeneration (B), lung edema (C), jaundice of the liver (D), intra-erythrocytic merozoites on a Giemsa-stained blood smear (E) Source: researchgate.net Babesiosis: Treatment • Mild cases may recover without treatment. • Sick animals can be treated with an antiparasitic drug. Treatment is most likely to be successful if the disease is diagnosed early; it may fail if the animal has been weakened by anemia. • Imidocarb has been reported to protect animals from disease but immunity can develop. There are also concerns with regard to residues in milk and meat. • In some cases, blood transfusions and other supportive therapy should be considered. Babesiosis: Prevention • Effective control of tick fevers has been achieved by a combination of measures directed at both the disease and the tick vector. Tick control by acaracide dipping is widely used in endemic areas. • Dipping may be done as frequently as every 4-6 weeks in heavily infested areas. The occurrence of resistance of ticks, chemical residues in cattle and environmental concerns over the continued use of insecticides has led to use of integrated strategies for tick control. • Babesiosis vaccines are readily available and are highly effective. Antitick vaccines are also available in some countries and can be used as part of an integrated program for the control of ticks. • Babesiosis can be eradicated by eliminating the host tick(s) Anaplasmosis • A disease of ruminants caused by obligate intraerythrocyte parasites of the order Rickettsiaeles, Anaplasma • Cattle, sheep, goats, deer, antelope, giraffes, and buffalo may be infected • Bovine anaplasmosis is of economic importance in the cattle industry Anaplasmosis: Etiology • Clinical bovine anaplasmosis is usually caused by A. marginale • Cattle are also infected with A. caudatum (may result in severe disease) and A. centrale (mild disease) • A. ovis (mild to severe disease): sheep, deer, and goats Source: en.wikipedia.org Anaplasmosis: Transmission & Epidemiology • Anaplasmosis is not contagious • Most transmission occurs via numerous species of tick vectors • Boophilus species are major vectors • After feeding on an infected animal, intrastadial or trans-stadial transmission may occur • Transovarian transmission may also occur (rare) • Transplacental transmission is usually associated with acute infection of the dam in the second or third trimester of gestation • May also spread through the use of contaminated needles or dehorning or other surgical instruments • There is a strong correlation between age of cattle and severity of disease. Calves are much more resistant to the disease than older cattle • After recovery from the acute phase of infection, cattle remain chronically infected carriers of the parasite and immune to further clinical disease. However, these chronically infected cattle may relapse to anaplasmosis when immunosuppressed (e.g. by corticosteroids), when infected by other parasites, or after splenectomy. • Carriers serve as a reservoir for further transmission Source: intechopen.com Anaplasmosis: Clinical Findings • Anaplasmosis is characterized by progressive anemia due to extravascular destruction of infected and uninfected erythrocytes • The prepatent period of A. marginale is directly related to the infective dose and typically ranges from 2 to 8 weeks • Parasitemia approximately doubles every 24 hr during the exponential growth phase • Generally, 10-30% of the erythrocytes are infected at peak parasitemia • Erythrocyte count, PCV, and haemoglobin values are all severely reduced • Macrocytic anemia with circulating reticulocytes may be present late in the disease • Acute infection: o Rapid loss of condition o Drop in milk production o Inappetence, loss of coordination, breathlessness when exerted, and a rapid bounding pulse are usually evident in the late stages o Urine may be brown (but myoblobinuria does not occur) Anaplasmosis: Clinical Findings o o o o Transient febrile response Paleness and then yellowing of the mucous membrane Abortion may occur in pregnant cows Surviving cattle convalesce over several weeks (during which hematologic parameters gradually return to normal) Anaplasmosis: Lesions • • • • • • • Carcasses are generally markedly anemic and jaundiced Blood is thin and watery Spleen is characteristically enlarged and soft, with prominent follicles Liver may be mottled and yellow-orange Gallbladder is often distended and contains thick brown or green bile Hepatic and mediastinal lymph nodes appear brown Epicardial and pericardial petechiae and ecchymoses are often present Anaplasmosis: Diagnosis • Microscopical examination of Giemsa-stained thin and thick blood films • Chronically infected carriers may be identified by serologic testing • complement fixation • card agglutination tests Anaplasmosis: Treatment • Tetracyclines and imidocarb • Prompt administration of tetracycline, chlortetracycline, or oxytetracycline in the early stages of acute disease (e.g., PCV >15%) usually ensures survival o Commonly used treatment: single IM injection of long-acting oxytetracycline (20 mg/kg) • Blood transfusion to partially restore the PCV greatly improves the survival rate of more severely affected cattle • The carrier state may be eliminated by administration of a long-acting oxytetracycline (20 mg/kg, IM), at least two injections with a 1-wk interval • Imidocarb o Efficacious against A. marginale as a single injection o Elimination of the carrier state: requires higher repeated doses of imidocarb (e.g., 5 mg/kg, IM or SC, two injections of the dihydrochloride salt 2 wks apart) Anaplasmosis: Prevention • Vaccination • Sustained stringent control or elimination of the arthropod vectors may be a viable control strategy