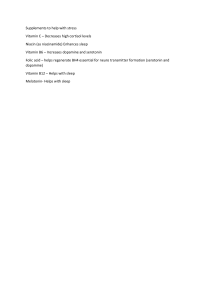
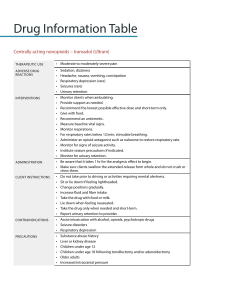
Anxiety and Depression Depression: Definition: (DSM-5) o > 5 of the following in the same 2 week period Depressed mood nearly every day Diminished pleasure in most/all activities on most days Significant weight loss or gain OR increased or decreased appetite Insomnia or hypersomnia nearly every day Psychomotor agitation or retardation on most days Fatigue or loss of energy on most days Feeling worthless or inappropriate guilt most days Decreased concentration or indecisiveness most days Recurrent thoughts of death Symptoms: SIGECAPS o Decreased sleep o Decreased interest o Increased guilt o Decreased energy o Decreased concentration o Increased or decreased appetite o Decreased psychomotor o Increased suicide Pathophysiology: Four proposed mechanisms o Biogenic amine hypothesis depression linked to a deficiency of catecholamines (NE, serotonin, dopamine) o Desensitization hypothesis acute increased in neurotransmitters may cause adaptive changes in receptor sensitivity o Dysregulation hypothesis possible impairment of neurotransmitter systems in one or more regulatory or homeostatic brain mechanisms o Dopaminergic hypothesis decreased dopaminergic neurotransmission may play a role in depressive symptoms Antidepressants: all carry a BBW for increased risk of suicide 1st line SSRIs, SNRIs, Bupropion, Mirtazepine SSRIs Fluoxetine, Sertraline, Paroxetine, Citalopram, Escitalopram, Fluvoxamine o MOA inhibit the reuptake of serotonin from the synaptic cleft o AE GI upset, CNS effects, sexual dysfunction, serotonin syndrome, hyponatremia o Contraindicated with Linezolid, IV methylene blue, and MAOIs (current or within 2 weeks) SNRIs Duloxetine, Venlafaxine, Desvenlafaxine, Milnacipran, Levomilnacipran o MAOIs inhibits reuptake of serotonin and norepinephrine from the synaptic cleft o AE GI upset, CNS effects, sexual dysfunction, serotonin syndrome, SIADH o Contraindicated with Linezolid, IV methylene blue, and MAOIs (current or within 2 weeks) Mixed Serotonin Modulators Vortioxetine (Trintellix), Vilazodone (Viibryd) Norepinephrine Dopamine Reuptake Inhibitor (DNRI) Bupropion o MOA inhibits reuptake of NE and dopamine o AE anxiety, insomnia, headache, nausea, tremor, weight loss, dry mouth, seizures (dosedependent) o Contraindicated with Linezolid, IV methylene blue, and MAOIs (current or within 2 weeks), seizure history, eating disorders, abrupt alcohol or sedative Tetracyclic Mirtazapine o Inhibits alpha-2 receptors on pre-synaptic neuron to increase release of serotonin and NE o SE sedation, increased appetite, weight gain, dizziness, HLD/HTGD o Contraindicated with Linezolid, IV methylene blue, and MAOIs (current or within 2 weeks) TCAs Amitriptyline, Nortriptyline, Imipramine, Desipramine, Doxepin, Amoxapine, Clomipramine o Block serotonin and NE reuptake o AE they have TONS; that is why they are not first line agents o Contraindications acute/recent MI, history of prolonged QTc, narrow angle glaucoma, tachycardia, Linezolid, IV methylene blue o Think TCAs Tremor, CV effects, Anticholinergic effects, Sedation/Seizures MAOIs Isocarboxazid, Phenelzine, Selegiline, Moclobemide o MOA irreversibly inhibit monoamine oxidase; increases NE, serotonin, and dopamine within neuronal synapse o AE way too many to type. o Contraindications cerebrovascular disease, hepatic impairment, uncontrolled HTN, Linezolid, IV methylene blue Side effects of antidepressants: o Suicidal thoughts Seen in teens and young adults Increase in energy without resolution of depression Greatest risk in first few weeks o Sexual dysfunction common with all BUT Bupropion o HA/N/V Caused by the increase in serotonin Should resolve as depression resolves Serotonin Syndrome: Signs and symptoms: o Tachycardia, HTN o Mydriasis o Hyperreflexia, clonus, tremor o Diaphoresis, vomiting, diarrhea o Agitation, altered mental status Management: o DC offending agent o Supportive care o Benzodiazepine for agitation Duration of Treatment: 1st episode 6-12 months 2nd episode 3 years once remission is reached > 3 episodes indefinite treatment Increase Suicide Monitoring in: Treatment initiation Dose increases Younger patients Barriers to ALL Behavioral Health Treatment: Stigma, cost, and disjointed health care delivery systems Diagnosis of Both: Medical diagnosis consists of objective information and presenting symptoms Behavioral diagnosis is mostly subjective and relies on symptoms and assessment measures from patient and family Lots of diagnosis or risk assessment comes from questionnaires in the outpatient setting o PHQ-2 o PHQ-9 o HAM-D o BDI o GDS o QIDS o WHO-5 Well Being Index All diagnoses will refer back to the DSM-5 Criteria (addressed earlier) Anxiety: Persistent, excessive, uncontrollable and unrealistic worry about everyday things Diagnostic Criteria: Excessive anxiety/worry lasting for > 6 months that is difficult to control Presence of > 3 symptoms for > 1 month: o Restlessness, feeling keyed up, or on edge o Easily fatigues o Difficulty concentrating or mind going blank o Irritability o Muscle tension o Sleep disturbances Significant distress of functional impairment Risk Factors: Women > men Stress Medications Medical conditions Non-Pharmacological Interventions: Exercise Psychotherapy Relaxation/Meditation therapy Pharmacotherapy Options: SSRI or SNRI first line Benzodiazepine or Atypical Buspirone second line Antihistamine Hydroxyzine Other Antipsychotics, Pregabalin adjunctive Benzodiazepines: MOA increase GABA receptor activity AE CNS depression, DC syndrome Contraindicated SA history, respiratory disorders, pregnancy/lactation/labor, significant hepatic disease Good for acute management, adjunctive with initiation of antidepressant May contribute to depressive symptoms In geriatric patients, prefer LOT (Lorazepam, Oxazepam, Temazepam) Buspirone: MOA partial serotonin agonist Efficacious but inferior to benzo Non-addictive and well-tolerated No immediate anxiolytic effect Hydroxyzine: MOA histamine and serotonin receptor antagonist Anticholinergic and antihistaminic side effects Active metabolite is cetirizine Onset of action is within 30 minutes Pregabalin: MOA binds voltage-gated calcium channels Good for acute management with anxiolytic effects similar to benzos Potential alternative to long-term benzo Potential for abuse/dependence Second Generation Antipsychotics: MOA partial serotonin agonist Augmentation therapy for refractory disease, psychosis, or severe agitation Olanzapine, Risperidone, and Quetiapine have the most evidence for support