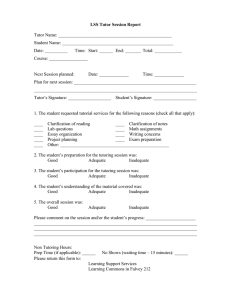
Standard Symbols for Genogram Family Coping Index 1.Physical Independence 1- Family failing entirely to provide personal care to its members: No competence 3- Family providing partially the needs of its members or proving care for some members but not for others: Incomplete Independence. 5- All family members receiving necessary care to maintain health and personal hygiene: Complete Independence 2. Therapeutic Competence (Management of prescribed drugs diet, exercises, procedures, using appliances etc.) 1- Family either not carrying out procedures prescribed or doing it unsafe: No competence. 3- Family carrying out some but not all of the treatments: Moderately Competence. 5- Family able to demonstrate that they can carry out the prescribed procedures safely and efficiently: Complete Competence. 3. Knowledge of Health Conditions: 1- Totally uninformed about the condition or misinformed: -unsatisfactory knowledge. 3- Has some knowledge of the disease or condition but has not grasped the underlying principles: - Satisfactory Knowledge. 5- Knows the salient facts about the disease well enough to take necessary action at proper time: - Good Knowledge. 4. Application of Principles of General Hygiene: (Maintaining family nutrition, securing adequate rest and relaxation for family members carrying out accepted preventive measures such as immunization etc.,) 1- Family diet grossly inadequate or unbalanced, necessary immunizations not secured for children, house dirty, food handled in an unsanitary way: - No Application. 3- Failing to apply some general principle of hygiene for instance secure initial immunizations but not boosters or some but not all available immunization: - Moderate Application. 5- Household runs smoothly, family meals well selected, habits to sleep and rest adequate to needs: -Complete Application. 5. Health Attitude: 1- Family resents and resists all health care, has no confidence in doctors uses patent medicines: - Unsatisfactory Attitude 3- Accepts health care to some degree, but with reservations. Ex: - Accept need for medical care for illness but not preventive measures: - Satisfactory Attitude. 5- Understands and recognizes need for medical care in illness and for usual preventive services: - Good Attitude. 6. Emotional Competence: (Maturity and integrity with which the members of family are able to meet the usual stresses and problems of life) 1- Family does not face realities, assume moribund patient will get well: - No Competence. 3- Family members usually do fairly well but one or more members evidence lack of security or maturity: -Moderate Competence. 5- All members of the family able to maintain a reasonable degree of emotional calm, face up to illness realistically and hopefully: -Complete Competence. 7. Family living: 1- Family consists of a group of individuals indifferent or hostile to one another or strongly dominated and controlled by a single-family member, no control of children: - Unsatisfactory 3- Family gets along but has habits or customs that interfere with their effectiveness or coherence as a family: -Satisfactory. 5- Family cohesive does things together each members acts for the good of the family as whole children respect parents and vice versa: - Good 8. Physical Environment: 1- House in poor condition, unsafe, unscreened, poorly ventilated neighborhood deteriorated, no playing space except streets: - Unsatisfactory environment. 3- House need some repair or painting but fundamentally sounds: - Satisfactory environment. 5- House in good repair, provides for privacy for members and is free of accident and best hazards: - Good environment. 9. Use of Community facilities: (The wisdom with which they use available community recourses for health, education and welfare. This would include the way, in which they use services of private physicians, clinics, emergency, rooms, hospitals, schools, churches etc.,) 1- Family has obvious and serious social needs, but has not sought or found any help for them: - No usage 3- Family knows about or uses some but not all of the available community resources that they need: - moderate usage 5- Family using the facilities they need appropriately and promptly know when and whom to call for help: - complete usage Criteria for Prioritization of Health Problems 1. NATURE OF THE PROBLEM (Weight: 1) Health Deficit Health Threat Foreseeable Crisis 3 2 1 2. MODIFIABILITY OF THE PROBLEM – Probability of success in minimizing, alleviating or totally eradicating the problem through intervention (Weight: 2) Easily modifiable 2 Partially modifiable Not modifiable 1 0 3. PREVENTIVE POTENTIAL - Nature and magnitude of future problems that can be minimized or totally prevented if intervention is done on the problem under consideration (Weight: 1) High Moderate Low 3 2 0 4. SALIANCE OF THE PROBLEM - Family’s perception and evaluation of the problem in terms of seriousness and urgency of attention needed (most important) (Weight: 1) A serious problem, immediate attention needed A problem, but not needing immediate attention Not a felt need / problem Scoring: 2 1 0 1. Decide on a score for each of the criteria. 2. Divide the score by the highest possible score and multiply by the weight: (score/highest score) x weight. 3. Sum up the scores for all the criteria. The highest score is 5 (equal to total weight). Typology of Nursing Problems *** First Level Assessment *** I. Presence of Wellness Condition A. Potential for Enhanced Capability for/ B. Readiness for Enhanced Capability for: Healthy lifestyle (e.g. nutrition/diet, exercise/activity) Healthy maintenance/health management Parenting Breastfeeding Spiritual well-being Others. Specify. II. Presence of Health Threats A. B. C. D. Presence of risk factors of specific diseases (e.g. lifestyle diseases, metabolic syndrome) Threat of cross infection from communicable disease case Family size beyond what family resources can adequately provide Accident hazards, specify: Broken chairs Pointed /sharp objects, poisons and medicines improperly kept Fire hazards Fall hazards Others specify. E. Faulty/unhealthful nutritional/eating habits or feeding techniques/practices. Specify: Inadequate food intake both in quality and quantity Excessive intake of certain nutrients Faulty eating habits Ineffective breastfeeding Faulty feeding techniques F. Stress Provoking Factors. Specify: Strained marital relationship Strained parent-sibling relationship Interpersonal conflicts between family members Care-giving burden G. Poor Home/Environmental Condition/Sanitation. Specify: Inadequate living space Lack of food storage facilities Polluted water supply Presence of breeding or resting sights of vectors of diseases Improper garbage/refuse disposal Unsanitary waste disposal Improper drainage system Poor lightning and ventilation Noise pollution Air pollution H. Unsanitary Food Handling and Preparation I. Unhealthy Lifestyle and Personal Habits/Practices. Specify: Alcohol drinking Cigarette/tobacco smoking Walking barefooted or inadequate footwear Eating raw meat or fish Poor personal hygiene Self medication/substance abuse Sexual promiscuity Engaging in dangerous sports Inadequate rest or sleep Lack of /inadequate exercise/physical activity Lack of/relaxation activities Non use of self-protection measures (e.g. non use of bed nets in malaria and filariasis endemic areas). J. Inherent Personal Characteristics (e.g. poor impulse control) K. Health History, which may Participate/Induce the Occurrence of Health Deficit, (e.g. previous history of difficult labor L. Inappropriate Role Assumption (e.g. child assuming mother’s role, father not assuming his role) M. Lack of Immunization/Inadequate Immunization Status Specially of Children N. Family Disunity, e.g.: Self-oriented behavior of member(s) Unresolved conflicts of member(s) Intolerable disagreement O. Others. Specify._________ III. Presence of health deficits (Instances of failure in health maintenance) A. Illness state, regardless of whether it is diagnosed or undiagnosed by medical practitioner. B. Failure to thrive/develop according to normal rat C. Disability (whether congenital or arising from illness; transient/temporary (e.g. aphasia or temporary paralysis after a CVA) or permanent (e.g. leg amputation secondary to diabetes, blindness from measles, lameness from polio) IV. Presence of stress points/foreseeable crisis situations (Anticipated periods of unusual demand on the individual or family in terms of adjustment/family resources) A. Marriage B. Pregnancy, labor, puerperium C. Parenthood D. Additional member (e.g. newborn, lodger) E. Abortion F. Entrance at school G. Adolescence H. Divorce or separation I. Menopause J. Loss of job K. Hospitalization of a family member L. Death of a member M. Resettlement in a new community N. Illegitimacy O. Others, specify. ***Second-Level Assessment*** I. Inability to recognize the presence of the condition or problem due to A. Lack of or inadequate knowledge B. Denial about its existence or severity as a result of fear of consequences of diagnosis of problem, specifically: Social-stigma, loss of respect of peer/significant others Economic/cost implications Physical consequences Emotional/psychological issues/concerns C. Attitude/Philosophy in life, which hinders recognition/acceptance of a problem D. Others. Specify. II. Inability to make decisions with respect to taking appropriate health action due to: A. Failure to comprehend the nature/magnitude of the problem/condition B. Low salience of the problem/condition C. Feeling of confusion, helplessness and/or resignation brought about by perceive magnitude/severity of the situation or problem, i.e. failure to breakdown problems into manageable units of attack. D. Lack of/inadequate knowledge/insight as to alternative courses of action open to them E. Inability to decide which action to take from among a list of alternatives F. Conflicting opinions among family members/significant others regarding action to take. G. Lack of/inadequate knowledge of community resources for care H. Fear of consequences of action, specifically: Social consequences Economic consequences Physical consequences Emotional/psychological consequences I. Negative attitude towards the health condition or problem-by negative attitude is meant one that interferes with rational decision-making. J. In accessibility of appropriate resources for care, specifically: Physical Inaccessibility Costs constraints or economic/financial inaccessibility K. Lack of trust/confidence in the health personnel/agenc L. Misconceptions or erroneous information about proposed course(s) of action M. Others. Specify. III. Inability to provide adequate nursing care to the sick, disabled, dependent or vulnerable/at risk member of the family due to: A. Lack of/inadequate knowledge about the disease/health condition (nature, severity, complications, prognosis and management) B. Lack of/inadequate knowledge about child development and car C. Lack of/inadequate knowledge of the nature or extent of nursing care needed D. Lack of the necessary facilities, equipment and supplies of care E. Lack of/inadequate knowledge or skill in carrying out the necessary intervention or treatment/procedure of care (i.e. complex therapeutic regimen or healthy lifestyle program). F. Inadequate family resources of care specifically: Absence of responsible member Financial constraints Limitation of luck/lack of physical resources G. Significant persons unexpressed feelings (e.g. hostility/anger, guilt, fear/anxiety, despair, rejection) which his/her capacities to provide care. H. Philosophy in life which negates/hinder caring for the sick, disabled, dependent, vulnerable/at risk membe I. Member’s preoccupation with on concerns/interests J. Prolonged disease or disabilities, which exhaust supportive capacity of family members. K. Altered role performance, specify: Role denials or ambivalence Role strain Role dissatisfaction Role conflict Role confusion Role overload L. Others. Specify. IV. Inability to provide a home environment conducive to health maintenance and personal development due to: A. Inadequate family resources specifically: Financial constraints/limited financial resources Limited physical resources-e.i. lack of space to construct facility B. Failure to see benefits (specifically long-term ones) of investments in home environment improvement C. Lack of/inadequate knowledge of importance of hygiene and sanitation D. Lack of/inadequate knowledge of preventive measures E. Lack of skill in carrying out measures to improve home environment F. Ineffective communication pattern within the family G. Lack of supportive relationship among family members H. Negative attitudes/philosophy in life which is not conducive to health maintenance and personal development I. Lack of/inadequate competencies in relating to each other for mutual growth and maturation (e.g. reduced ability to meet the physical and psychological needs of other members as a result of family’s preoccupation with current problem or condition. J. Others specify._________ V. Failure to utilize community resources for health care due to: A. Lack of/inadequate knowledge of community resources for health care B. Failure to perceive the benefits of health care/services C. Lack of trust/confidence in the agency/personnel D. Previous unpleasant experience with health worker E. Fear of consequences of action (preventive, diagnostic, therapeutic, rehabilitative) specifically: Physical/psychological consequences Financial consequences Social consequences F. Unavailability of required care/services G. Inaccessibility of required services due to: Cost constrains Physical inaccessibility H. Lack of or inadequate family resources, specifically: Manpower resources, e.g. baby sitter Financial resources, cost of medicines prescribe I. Feeling of alienation to/lack of support from the community, e.g. stigma due to mental illness, AIDS, etc J. Negative attitude/ philosophy in life which hinders effective/maximum utilization of community resources for health care K. Others, specify __________